Chapter 53 Orbitozygomatic Infratemporal Approach to Parasellar Meningiomas
Lesions located high in the parasellar region and the interpeduncular fossa are challenging and often difficult to approach, as a result of both the deep position and the surrounding vital structures that obscure the view. In 1977, we developed a new surgical approach, the orbitozygomatic infratemporal approach,1 consisting of an orbitozygomatic osteotomy, a fronto-temporo-orbital craniotomy, and removal of the posterolateral wall of the orbital bone and major sphenoid wing lateral to the foramen spinosum. This approach provides a good exposure of the infratemporal fossa, permits access obliquely upward to the parasellar region and the interpeduncular fossa, and permits safe manipulation of parasellar and interpeduncular lesions via the shortest distance.2–4
Operative Technique
A bicoronal scalp incision is made to gain sufficient exposure of the zygomatic arch and superior and lateral orbital margins, starting at the inferior end of the base of the earlobe, running along the anterior margin of the ear cartilage, extending upward and forward, and running within the hairline to a level 3 cm above the upper margin of the contralateral zygomatic arch. The superficial layer of deep temporal fascia is incised and reflected with the skin flap to avoid the injury of the frontal branch of the facial nerve. The skin flap is reflected farther anteriorly with the frontal pericranium to expose the orbitozygomatic complex, cutting the supraorbital notch for the preservation of the right supraorbital nerve.5,6 To preserve the temporal and zygomatic branches of the facial nerve, the fascia covering the temporomandibular joint capsule is carefully pulled away, and the periosteum covering the outer surface of the zygomatic arch is incised vertically just in front of the tuberculum articulare. The entire outer surface of the zygomatic arch from its frontal process to its-pedicle is then fully exposed subperiosteally. The superior and lateral orbital margins are then exposed, maintaining continuity of the pericranium and the periorbita. The superior and lateral periorbita are separated from the superior and lateral posterior walls of the orbit.
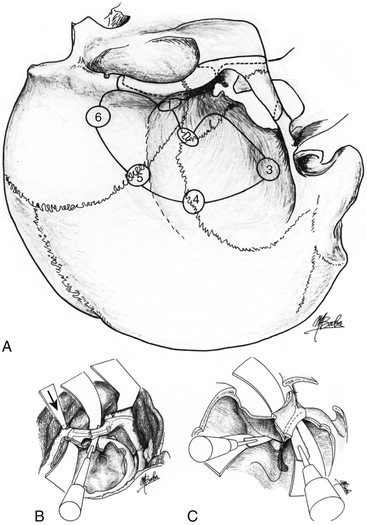
Multiple burr holes are made, the first of which, in the lateral frontal bone just behind the frontal process of the zygomatic bone, is the key burr hole. The second burr hole is at the pterion, the third in the temporal bone just above the pedicle of the zygomatic process, the fourth in the squamous suture about 3 cm above the zygomatic arch, the fifth in the coronal suture about 6 cm above the zygomatic arch, and the sixth in the frontal bone 3 cm above the orbital ridge (Fig. 53-1). The anterior and posterior ends of the zygomatic arch are then cut using a sagittal saw, and it is retracted downward hinged on the masseter muscle.
The second, third, fourth, fifth, and sixth burr holes are then connected with a craniotome (see Fig. 53-1). Using a reciprocating saw, osteotomy of the lateral and superior walls of the orbit is performed from the inferior orbital fissure. The orbital content is protected by a spatula during this osteotomy. The frontotemporal bone flap and the orbitozygomatic flap are kept in saline solution containing an antibiotic. While protecting the periorbita and the dura mater with self-retaining retractors with spatulas, the remaining major sphenoid wing lateral to the foramen spinosum, forming the posterolateral orbital wall and the anterolateral part of the middle fossa, and the posterior portion of the orbital roof lateral to the superior orbital fissure, are divided, using either a sagittal saw or small chisel (see Fig. 53-1). The remaining medial part of the minor sphenoid wing is then partially removed with an air drill and a bone rongeur. The bone fragments are kept in the saline solution to be replaced at the end of the procedure.
The exposed frontotemporal dura mater is opened in semicircular fashion, from the medial superior orbital margin to the midportion of the inferior temporal region. Alternatively, in a combined orbitozygomatic epidural and subdural approach,7–9 an inverted T-shaped dural incision is made along the sylvian fissure to the superior surface of the optic nerve sheath forward with a short vertical incision at the distal sylvian fissure. The orbital contents are retracted medially downward by retracting the anterior dural fringe forward.
The operative microscope is now introduced, and either a trans-sylvian approach or a subtemporal approach can be taken with minimal retraction of the brain. In the trans-sylvian approach, the sylvian fissure is widely opened, with preservation of the bridging veins coming from the tip of the temporal lobe. The parasellar region as well as the interpeduncular fossa can be reached at a short distance through the space formed via this approach.
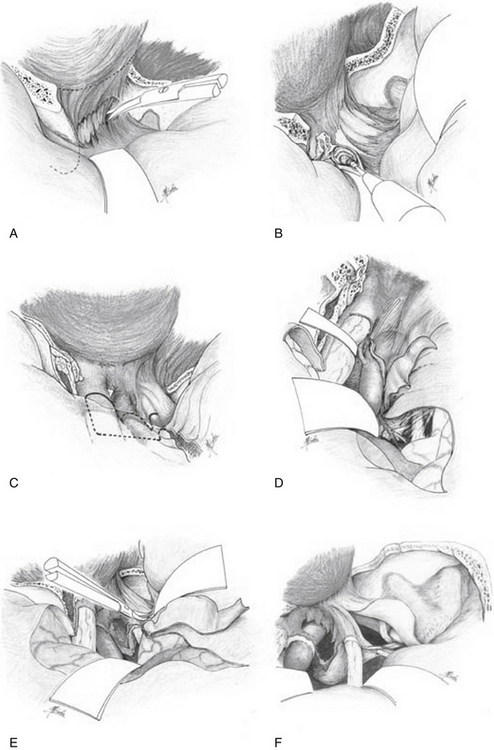
When the tumor is invading the cavernous sinus (CS),5 the CS is explored by a combined orbitozygomatic infratemporal epidural and subdural approach, which has been described elsewhere.7–9 The periosteal reflection, which is continuous with the periorbita, is divided at the superior and inferior margins of the superior orbital fissure by sharp dissection using either microscissors or a knife; then the temporal dura propria, forming the superficial layer of the CS, can be separated from the content of the superior orbital fissure (Fig. 53-2A). The lateral part of the anterior clinoid process is shelled out, leaving a thin layer of its cortical bone. The optic canal is then opened along its length. The cortical bone of the anterior clinoid process and the optic strut are removed by a bone-cutting forceps and a small diamond drill (Fig. 53-2B). The dural incision passes along the sylvian fissure to the superior surface of the optic nerve sheath forward, and then turns laterally at a right angle (Fig. 53-2C). It passes backward at a right angle and runs along the medial part of the distal carotid ring, then along the carotid artery 2 mm away from the artery (Fig. 53-2D). Opening of the medial triangle (Hakuba’s triangle, which is a triangle in the subdural space) starts from the distal ring along the medial side of the triangle to the posterior clinoid process and turns laterally at a right angle along the posterior side of this triangle to the dural entrance of the third cranial nerve. The lateral dural fringe of the medial triangle is elevated. Then the remaining outer layer of the CS is separated farther backward from the inner layer of the lateral wall of the CS consisting of the nerve sheaths of the third through fifth cranial nerves (Fig. 53-2E), and the entire CS is unveiled (Fig. 53-2F). Bleeding from the CS is easily controlled by elevating the head side of the table, and the opened venous pathway in the CS is immediately sealed off by insertion of either a fibrinogen-soaked oxidized cellulose sponge or a collagen sponge into the CS, and a bipolar coagulation. Because the intracavernous internal carotid artery (ICA) has its own dural sheath,10 the plane between the ICA and the tumor is usually found relatively easily, and the tumor is freed from the ICA if it is not invasive. When the artery is torn during dissection, 8-0 monofilament nylon interrupted sutures are applied while trapping this segment of the artery between two temporary clips at both C3 and either C5 or the intrapetrous portions of the ICA, with intravenous administration of barbiturates for brain protection8 (pentobarbital 4 mg/kg as the initial dose, followed by 2 mg/kg/hr).
Closure of the Opened Paranasal Sinus and Dural Defect
Summary of Cases
Between 1977 and 2009, 181 cases were treated using the orbitozygomatic approach either alone or combined with other approaches, such as the oticocondylar approach11 or transpetrosal approach.7 These cases included 44 parasellar meningiomas, 24 pituitary adenomas, 26 basilar tip aneurysms, 12 trigeminal neurinomas, 19 chordomas, 11 internal carotid aneurysms, 21 craniopharyngiomas, 3 CS cavernomas, and 21 other lesions (Table 53-1). Of 44 parasellar meningiomas, 19 patients were men and 25 women. Ages ranged from 35 to 76 years (mean of 57.2 years). Total removal of the tumor was accomplished in 32 cases, subtotal removal in 8, and partial removal in 4. Postoperative bacterial meningitis and either an epidural or a subdural hematoma was seen in three cases, wound infection in two, and pneumonia in one. In the cases of the tumors involving the CS, impairment of extraocular movement was seen postoperatively in five cases, trigeminal nerve injury in four, and ipsilateral blindness in two. There was no mortality, but four patients developed disturbance of their conscious level (severely disabled in one case and moderately disabled in three). The operative results were classified as follows: excellent, when the patients have no neurologic deficit; good, when the patients have normal activity in daily life with minor neurologic dysfunction; fair, when the patients are moderately disabled but independent with major neurologic deficit; and poor, when the patients are severely disabled and totally dependent. The operative results were excellent in 23 patients and good in 17 patients (Table 53-2). Three of the remaining four patients were fair postoperatively as a result of bacterial meningitis in one; hypothalamic damage, which had been seen preoperatively, in one; and a combined epidural and subdural hematoma in one. The last one was poor because of a postoperative epidural hematoma. Two representative cases are described briefly.
Table 53-1 Summary of Cases Accessed with Orbitozygomatic Approach
| Pathology | No. of Cases |
|---|---|
| Parasellar meningioma | 44 |
| Pituitary adenoma | 24 |
| Basilar tip aneurysm | 26 |
| Trigeminal neurinoma | 12 |
| Chordoma | 19 |
| Craniopharyngioma | 21 |
| IC aneurysm | 11 |
| CS cavernoma | 3 |
| Others | 21 |
| Total | 181 |
CS, cavernous sinus; IC, internal carotid.
Table 53-2 Surgical Outcome of 44 Parasellar Meningiomas Removed by Orbitozygomatic Approach
| Grade | No. of Cases |
|---|---|
| Excellent | 23 |
| Good | 17 |
| Fair | 3 |
| Poor | 1 |
Case Report 1
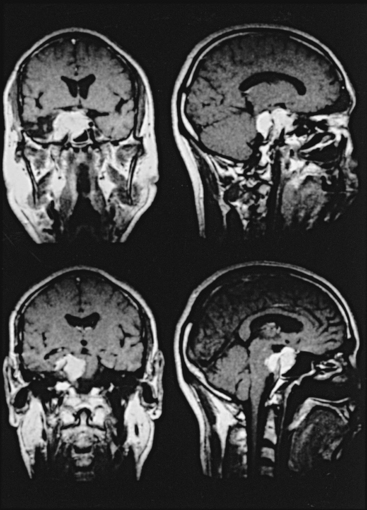
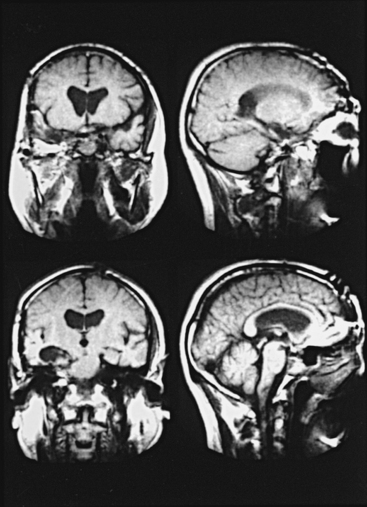
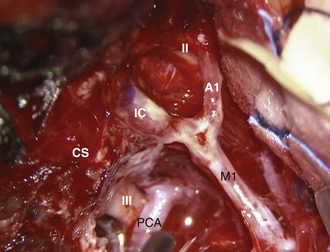
The right orbitozygomatic infratemporal approach with a combined epidural and subdural (medial triangle) approach was used on a 57-year-old, right-handed man with a large right parasellar meningioma who had total ophthalmoplegia after partial removal of the tumor in the past (Fig. 53-3). A large tumor occupied the entire CS with encasement of the intracavernous segment of the right ICA. The tumor extended backward subdurally behind the upper clivus with marked compression of the pons and extended inferiorly into the right sphenoid sinus. All the cranial nerves were encased and invaded by the tumor in the CS and had to be sacrificed and removed with the tumor. The intracavernous ICA was carefully dissected out and preserved. The upper basilar artery and its tributaries, which were displaced backward and partially encased, were also well preserved, with total removal of the tumor (Fig. 53-4). The patient had moderate left hemiparesis, which lasted 2 weeks postoperatively; he was neurologically intact except for permanent total ophthalmoplegia at 4 months.
Case Report 2
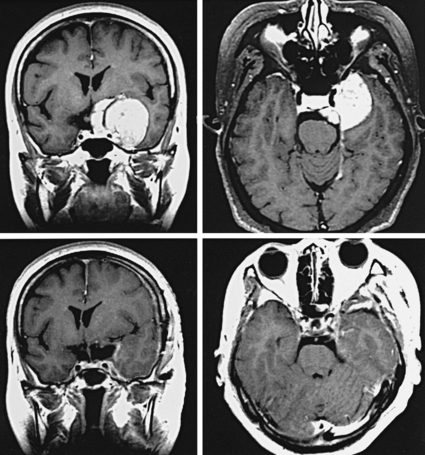
A 57-year-old woman presented with progressive visual deterioration of the left eye. Radiologic study showed a large left parasellar meningioma (Fig. 53-5). A left orbitozygomatic approach was used for total removal of the tumor. The tumor was engulfing the ICA, but it could be easily separated from it because of the presence of arachnoid space between the artery and the tumor. The tumor extended into the left optic canal and compressed the optic nerve. The canal was opened for excision of that part of the tumor. The anterior part of the lateral wall of the CS was invaded by the tumor, but intracavernous structures were not involved by the tumor. The pituitary stalk was shifted and flattened by the tumor. All these structures were preserved, and total removal of the tumor was achieved (Fig. 53-6 see also Fig. 53-5). Postoperatively the patient showed mild left oculomotor palsy, which improved gradually.
Discussion
Radical removal of parasellar meningiomas usually involves difficult surgical procedures.12 With the orbitozygomatic infratemporal approach, the working distance to the lesions in the parasellar region and the interpeduncular fossa is about 3 cm shorter and the angle to the lesions about 1 to 3 cm lower than with either the pterional or the subtemporal approach. With the combined orbitozygomatic infratemporal epidural and medial triangle approach, the intracanalicular portion of the optic nerve is well exposed, so that much more space can be obtained between the optic nerve and the carotid artery. With this combined approach, the parasellar region, including the CS, and the interpeduncular fossa can be accessed in the shortest possible distance with minimal retraction of the temporal lobe.2–4 Manipulation of the vital structures is much easier and safer, even with large parasellar meningiomas, than with the conventional operative approaches.
In the orbitozygomatic infratemporal approach, wide exposure of the parasellar lesions can be obtained exclusively by aggressive posterior temporal lobe retraction, which may be at risk of temporal lobe contusion. Surgical strategy should consider the preoperative imaging study of the venous system. The contusion is avoidable by preservation of temporal venous drainage. In the cases of parasellar meningiomas invading the medial sphenoid ridge, the sphenoparietal sinus is usually occluded by tumor and collateral flow via cortical veins is well developed, so that safe posterior temporal lobe retraction is possible after transecting the sylvian vein at its orifice to the sphenoparietal sinus. If the sphenoparietal sinus is patent, an extradural orbitozygomatic approach should be taken for preservation of the venous drainage of the sylvian vein to the pterygoid venous plexus. Peeling off of the temporal dura propria from the inner layer of medial wall of the cavernous sinus is feasible down to the dural entrance of the trochlear nerve.13 In cases of retrochiasmatic parasellar meningioma in which either the superficial or deep sylvian vein is draining directly into the CS without efficient transcortical collateral circulation, the orbitozygomatic approach risks its damage. In such cases, we select the combined anterior and posterior transpetrosal approach.
The petrosal portion of the ICA, 1 cm long, is epidurally exposed with removal of the petrosal apex at the posterior portion of the trigeminal impression medial to the great petrosal nerve groove by using an air drill. Therefore, when parasellar tumors extend into the CS, the intracavernous portion of the procedure is performed relatively safely while trapping the intracavernous portion of the ICA between its petrosal and C3 portions if necessary.14 Because the petrosal bone is removed, both medial to the petrosal ICA and anterior to the internal auditory meatus and cochlea, a transzygomatic preauricular transpetrosal approach9 can be readily carried out. Therefore, parasellar tumors extending into the posterior fossa can be totally removed at one stage with this combined epidural and subdural approach.
To preserve the peripheral facial nerve in such low craniotomies, it is necessary to know its topographic anatomy.15 After exiting from the stylomastoid foramen, the facial nerve crosses the posterior margin of the mandible about 2 cm below the inferior base of the earlobe and enters the parotid gland from behind, where it is situated between the superficial and deep portions of the gland. The branches leave the gland at its superior, anterior, and inferior borders, forming a pattern of rami located superficial to Bichat’s fat pad and underneath the facial muscles, entering them from their deep surface. The temporal and zygomatic rami cross the zygomatic arch about 2 cm anterior to the anterior margin of the external auditory canal. Therefore, it is safe to make the skin incision along the anterior margin of the ear cartilage. The temporal and zygomatic rami of the ipsilateral facial nerve are usually well preserved by elevating the superficial temporal fascia together with the skin flap and subperiosteally dissecting the zygomatic arch and zygomatic bone.
Ammirati M., Spallone A., Ma J., et al. An anatomical study of the temporal branch of the facial nerve. Neurosurgery. 1993;33:1038-1043.
Bruder N., Ravussin P., Young W.L., et al. Anesthesia for surgery of intracranial aneurysms. Ann Fr Anesth Reanim. 1994;13:209-220.
Chanda A., Nanda A. Anatomical study of the orbitozygomatic transsellar-transcavernous-transclinoidal approach to the basilar artery bifurcation. J Neurosurg. 2002;97:151-160.
Day J.D. Cranial base surgical techniques for large sphenocavernous meningiomas [technical note]. Neurosurgery. 2000;46:754-759.
Hakuba A. Surgical approaches to the cavernous sinus via the medial triangle: report of an aneurysm at the C4–C5 junction of the internal carotid artery [Japanese]. Geka Shinryo. 1965;26:1385-1390.
Hakuba A., Liu S.S., Nishimura S. The orbitozygomatic infratemporal approach: a new surgical technique. Surg Neurol. 1986;26:271-276.
Hakuba A., Matsuoka Y., Suzuki T., et al. Direct approaches to vascular lesions in the cavernous sinus via the medial triangle. In: Dolenc V.V., editor. The Cavernous Sinus. New York: Springer-Verlag; 1987:272-284.
Hakuba A., Tanaka K., Suzuki T., et al. A combined orbitozygomatic infratemporal epidural and subdural approach for lesions involving the entire cavernous sinus. J Neurosurg. 1989;71:699-704.
Lemole G.M.Jr., Henn J.S., Zabramski J.M., et al. Modifications to the orbitozygomatic approach [technical note]. J Neurosurg. 2003;99:924-930.
Millesi H.. Extratemporal surgery of the facial nerve—palliative surgery, Krayenbuhl H., et al, editors, Advances and Technical Standards in Neurosurgery, Vienna, Springer-Verlag, 1980;Vol 8:180-308.
Ohata K., Baba M. Orbitozygomatic infratemporal approach. In: Hakuba A., editor. Surgical Anatomy of the Skull Base. Tokyo: Miwa Shoten; 1996:1-35.
Ohata K., Baba M. Otico-condylar approach. In: Hakuba A., editor. Surgical Anatomy of the Skull Base. Tokyo: Miwa Shoten; 1996:37-75.
Ohata K., Hakuba A., Branco S.J. Development of the meninges: Application to microneurosurgery [Japanese]. In: Ishii R., editor. Surgical Anatomy for Microneurosurgery. Tokyo: SIMED Publications; 1997:58-64.
Sindou M.P. Working area and angle of attack in three cranial base approaches: pterional, orbitozygomatic, and maxillary extension of the orbitozygomatic approach. Neurosurgery. 2002;51:1526-1527.
Takami T., Ohata K., Nishikawa M., et al. Transposition of the oculomotor nerve for resection of a midbrain cavernoma [technical note]. J Neurosurg. 2003;98:913-916.
1. Hakuba A., Liu S.S., Nishimura S. The orbitozygomatic infratemporal approach: a new surgical technique. Surg Neurol. 1986;26:271-276.
2. Chanda A., Nanda A. Anatomical study of the orbitozygomatic transsellar-transcavernous-transclinoidal approach to the basilar artery bifurcation. J Neurosurg. 2002;97:151-160.
3. Lemole G.M.Jr., Henn J.S., Zabramski J.M., et al. Modifications to the orbitozygomatic approach [technical note]. J Neurosurg. 2003;99:924-930.
4. Sindou M.P. Working area and angle of attack in three cranial base approaches: pterional, orbitozygomatic, and maxillary extension of the orbitozygomatic approach. Neurosurgery. 2002;51:1526-1527.
5. Ammirati M., Spallone A., Ma J., et al. An anatomical study of the temporal branch of the facial nerve. Neurosurgery. 1993;33:1038-1043.
6. Ohata K., Baba M. Orbitozygomatic infratemporal approach. In: Hakuba A., editor. Surgical Anatomy of the Skull Base. Tokyo: Miwa Shoten; 1996:1-35.
7. Hakuba A. Surgical approaches to the cavernous sinus via the medial triangle: report of an aneurysm at the C4–C5 junction of the internal carotid artery [Japanese]. Geka Shinryo. 1965;26:1385-1390.
8. Hakuba A., Matsuoka Y., Suzuki T., et al. Direct approaches to vascular lesions in the cavernous sinus via the medial triangle. In: Dolenc V.V., editor. The Cavernous Sinus. New York: Springer-Verlag; 1987:272-284.
9. Hakuba A., Tanaka K., Suzuki T., et al. A combined orbitozygomatic infratemporal epidural and subdural approach for lesions involving the entire cavernous sinus. J Neurosurg. 1989;71:699-704.
10. Ohata K., Hakuba A., Branco S.J. Development of the meninges: application to microneurosurgery [Japanese]. In: Ishii R., editor. Surgical Anatomy for Microneurosurgery. Tokyo: SIMED Publications; 1997:58-64.
11. Ohata K., Baba M. Otico-condylar approach. In: Hakuba A., editor. Surgical Anatomy of the Skull Base. Tokyo: Miwa Shoten; 1996:37-75.
12. Day J.D. Cranial base surgical techniques for large sphenocavernous meningiomas [technical note]. Neurosurgery. 2000;46:754-759.
13. Takami T., Ohata K., Nishikawa M., et al. Transposition of the oculomotor nerve for resection of a midbrain cavernoma [technical note]. J Neurosurg. 2003;98:913-916.
14. Bruder N., Ravussin P., Young W.L., et al. Anesthesia for surgery of intracranial aneurysms. Ann Fr Anesth Reanim. 1994;13:209-220.
15. Millesi H.. Extratemporal surgery of the facial nerve—palliative surgery, Krayenbuhl H., et al, editors, Advances and Technical Standards in Neurosurgery, Vienna, Springer-Verlag, 1980;Vol 8:180-308.