Chapter 105 Optimal Procedures for Retinal Detachment Repair
![]() For additional online content visit http://www.expertconsult.com
For additional online content visit http://www.expertconsult.com
Introduction
About a century ago, rhegmatogenous retinal detachment (RRD) was essentially untreatable. A survey of ophthalmologists, carried out in 1912, estimated the success rate of therapy to be 1 in 1000.1 Many treatments were attempted, ranging from draining subretinal fluid to injections of mercury salts around the eye, but without success. Jules Gonin was the first to realize that curing RRD required prevention of recruitment of subretinal fluid through retinal breaks. His introduction of thermocautery immediately raised the success rate to about 1 in 2, a landmark achievement.2 The etiology of RRD is now better understood, and most surgeons agree that retinal breaks should be first closed, and then permanently sealed with retinopexy. However, despite this agreement, there is still enormous variation between surgeons in their choice of procedure for particular detachments.3 This chapter aims to examine those procedures, and assist the reader in choosing between them, for eyes with noncomplex RRD.
Round hole retinal detachment
Introduction
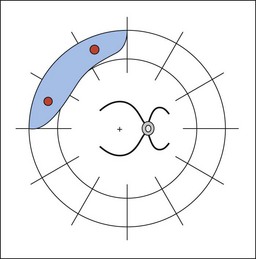
In eyes with round hole retinal detachment, the causative breaks are small round holes, often associated with lattice degeneration. Patients affected are typically young, low myopes, presenting with blurring of vision and a visual field defect. Some patients are asymptomatic and picked up on routine examination (Figs 105.1, 105.2). Round hole detachments are relatively uncommon, and in a large series of RRD reported by Tillery and Lucier, only 2.8% of cases were found to be secondary to round holes.4 Other series have reported a higher frequency, with 13.9% being reported by Morse and Scheie,5 and 21% in a series from Japan.6 An important clinical finding in these patients, is that the posterior hyaloid is usually attached. For example, in a large series of 110 round hole detachments requiring treatment, only eight (7%) of the eyes had a detached vitreous, and in these cases, the associated clinical findings suggested that the retinal detachment predated the posterior vitreous detachment (PVD).7
Natural history
Much of our understanding of the natural history of round hole detachments comes from the painstaking work of Norman Byer. In a long-term follow-up of patients with asymptomatic retinal lesions, there were 17 eyes with 18 areas of round hole retinal detachment.8 The majority (75%) of the patients were followed-up for more than 5 years, and some for up to 12 years. There was no change in 13 of the 18 areas of detachment, and only a minor change in three areas (18%). In a later report, Byer reported on 19 eyes with up to 33 years of follow-up.9 There were 22 areas of subclinical detachment in the 19 eyes, seven of which showed some form of progression, and only two of which required treatment, which was successful in both. Therefore, it can be stated that none of the patients in this series lost vision as a result of the initial decision to defer surgery.
A common misconception is that a pigment line, or “tide mark” or “demarcation line” posterior to the area of detachment will prevent progression. This is not the case, though such a line does imply stability of the extent of the detachment for at least some months. Benson studied 66 retinal detachments with demarcation lines (a subset of a larger series all requiring surgery), 20 of which were detected on routine examination. Most of these patients were young (median age 33), and had detachments secondary to round holes. The demarcation line had failed to prevent progression in 51 of the 66 cases.10
Brod et al. observed 28 patients (31 eyes) for 0.5–12.1 years (a mean follow-up of 3.4 years). The patients’ age range was 17–82 years, with a mean of 49 years. The majority of eyes were myopic, with 76% of patients having refractive errors of −2 diopters or more. A demarcation line was present in 23 eyes (74%). Only one patient progressed to develop symptoms with associated detachment of the macula, and reduction of visual acuity to 20/30, 3.3 years later. Vision returned to 20/20 following successful surgery. Another patient developed a new detachment from a subsequent PVD and a retinal “U” (“horseshoe”) tear.11
Jarrett reported on 16 patients with retinal detachments in whom surgery was delayed or did not occur. Eleven of these patients had round holes or dialyses. Eight patients had buckling surgery up to 8 years after detection, the delay being for a variety of reasons, including reluctance on behalf of asymptomatic patients to undergo eye surgery. Seven eyes progressed, but only one patient who delayed surgery presented later with a detached macula.12
Treatment
Laser demarcation
The extent of detached retina can be limited by creating a surrounding adhesion between the retina and the retinal pigment epithelium (RPE). This is the principle of retinopexy, and is widely used to treat retinal tears. The principle can also be applied to wider areas of detachment with a view to limiting progression.13 Such treatment of course does nothing to resolve an existing detachment, so this choice of management effectively “writes off” the detached area of retina. This is appropriate in patients with asymptomatic retinal detachments, or those with very minimal symptoms.
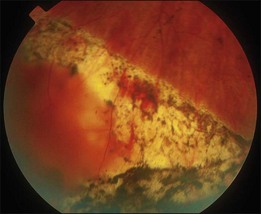
The aim of demarcation treatment is to create a band of effective chorioretinal adhesion, which completely surrounds the area of detachment. This generally means applying treatment from ora to ora, just posterior to the fluid (Fig. 105.3). Although cryotherapy could be used, laser photocoagulation is preferred as it causes less tissue damage, and less inflammatory reaction to the external eye. There is evidence that an adhesion stronger than normal appears within 24 hours of the application of treatment,14 but maximum strength is achieved between 3 and 14 days later.15 Therefore, laser demarcation is not suitable for rapidly progressive detachments.
There is only a limited amount of experience in the literature to assess the long-term value of this treatment. Okun et al. discussed demarcation in 1968. The authors treated 48 eyes, and 42 (88%) were stable after 0.5–6 years follow-up. Of the remaining six eyes, three developed additional areas of detachment from new breaks, and three were judged at the time of laser to need surgical treatment.16 Treplin presented a series of four cases from Tasmania, explaining; “Any Tasmanian presentation is in single figures, as there are not very many Tasmanians.” In one case with an extensive area of detachment, laser failed to prevent progression.17
Gratton treated 42 phakic patients with limited retinal detachments and attached maculae. Most patients (54%) were myopes. Follow-up was for 1–4 years, during which time only one case progressed. In this patient, surgery was successful in reattaching the retina with no visual loss or complications.18
Vrabec and Baumal treated 34 eyes with a variety of retinal detachments, all with attached maculae. They used the indirect laser ophthalmoscope to produce three confluent rows of retinopexy extending posteriorly to the fluid from ora to ora. All eyes were stabilized except one, in which inadequate laser had been applied because of the proximity of the posterior pole.19
Scleral buckling
The primary success rate of scleral buckling in round hole detachments is very high, but there is a risk of ocular morbidity. Tillery and Lucier reported results of buckling surgery in cases with detachments secondary to round holes in lattice (some of whom were asymptomatic). The reattachment rate with scleral buckling was 98%. However, 15% had worse vision postoperatively, and the proportion of eyes with worse post-operative vision in the subgroup of those eyes with 20/40 or better preoperatively, was 31%.20 Greven et al. reported results of 28 eyes of 27 patients with subclinical detachments. In 16 eyes (57%), the detachment was detected on a routine examination, and in eight patients, the fellow eye had a previous symptomatic detachment. All eyes were treated with segmental scleral buckling, and two were encircled. The initial reattachment rate was 100%, but one eye developed another retinal detachment associated with new breaks after 14 months. One eye lost vision from 20/20 to 20/30 “without obvious cause,” but no mention was made of any other complications.21
Ung et al. from Cambridge reported excellent results from scleral buckling in a large series of retinal detachments secondary to round holes. All but one of 110 detachments were repaired with a single procedure, a success rate of 99%.7
Detachment due to retinal dialyses
Introduction
A retinal dialysis is a tear of the retina from its insertion at the ora serrata.22 Some dialyses are secondary to trauma, and are most commonly found in the inferotemporal quadrant.23 Non-traumatic idiopathic dialyses also occur, and tend to be bilateral and inferotemporal,22,24 and some such cases may be inherited.25 In a large series of 1601 retinal detachments, 71 (4.4%) were found to be secondary to a retinal dialysis.26 The majority of patients were young (mean age 30), and there was a male to female preponderance of 1.3 : 1. Only 70% of patients gave a history of trauma. The vitreous is attached in the vast majority of cases. In Bonnet’s series, a PVD was only found in 1 of 48 cases (2.1%).27
Natural history
There is often a long interval between the creation of the dialysis, and the development of a symptomatic retinal detachment. In the series of traumatic retinal detachments described by Cox et al., the time from trauma to retinal detachment was up to 40 years, though in 80% of cases, was less than 2 years.28 In another series of 50 patients, 41% of the detachments due to traumatic dialysis were diagnosed more than 1 year after injury.29 The progression of the detachment can be slow, and this may be related to the lack of vitreous detachment. If the detachment is not detected until the macula becomes involved, then the final visual acuity can be compromised. In Ross’s series, 84% of eyes had detached maculae prior to surgery.29 In a report on patients with traumatic retinal detachments from Northern Ireland, patients with delayed diagnosis were found to have a less favorable visual outcome than those who were diagnosed within 6 weeks of the trauma.30
Conservative management
The considerations and options for management of patients with limited detachment secondary to dialysis are identical to those for patients with round hole detachments. Cases with signs of chronicity, such as tidemarks and retinal cysts, have probably been stable for some time, consequently with a relatively low risk of progression. In one series of 71 detachments secondary to dialysis, three patients had such signs of chronicity and were therefore followed-up without incident.26
Treatment
Laser demarcation
Limited detachments secondary to dialysis respond well to laser demarcation. This is particularly true for the majority of detachments from dialyses which are in the inferotemporal quadrant. Walling off of the affected area here results in a permanent field defect superonasally, which is likely to be less important to the patient, than inferotemporal field loss. In Kennedy’s series of 71 patients, five were successfully treated with retinopexy in order to demarcate a local detachment.26
Scleral buckling
Dialyses respond well to segmental scleral buckling procedures. In a series of traumatic retinal detachments including 49 cases of dialysis, the primary success rate was 96%.30 In another series from France of 48 cases of retinal detachment secondary to dialysis, the primary success rate was 100%.27 Ross described a series of 50 eyes with a primary success rate of 94% and a final success rate of 98%.29 The primary success rate for surgery in Kennedy’s series was 97%.26
Retinal detachment secondary to “u” (“horseshoe”) tears
Introduction
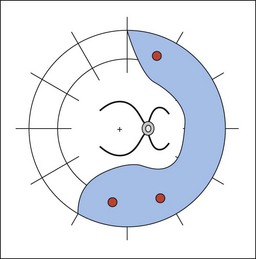
This category represents the most common group of rhegmatogenous retinal detachments. The detachment is secondary to one or more traction “U” tears, which in turn follow PVD (Fig. 105.4). A typical patient will present with visual loss, a symptomatic field defect, and a history of floaters and flashing lights some weeks previously.
Natural history
We know from studies prior to Gonin that the prognosis for vision in untreated cases is very poor. A relatively recent study of long-term findings in untreated retinal detachment showed severe loss of vision in all patients, with the best level of vision being hand movements. In addition there was a significant rate of discomfort and cosmetic problems.31 Following formation of tears, detachment tends to occur rapidly, due to a combination of recruitment of subretinal fluid through the break, and continuing vitreous traction on the flap. In the majority of cases, tears occur at the time of the PVD, or shortly afterwards. However, there is evidence that in pseudophakic eyes, chronic traction from a pre-existing PVD can lead to new, anterior breaks.32,33 Fluid currents within the eye also play a significant role in the development of the detachment, as described by Machemer in his Jackson Memorial Lecture in 1988.34 Subretinal fluid from superior tears spreads more rapidly than that from inferior ones, and this needs to be borne in mind when planning the timing of intervention in eyes with an attached macula. The rapid progression of most detachments in this category means that a majority of patients present with their macula already detached. In Burton’s series of 953 primary retinal detachments, 69.5% of cases had detached maculae preoperatively.35
Conservative management
Occasionally, a small, asymptomatic peripheral detachment from a “U” tear might appear stable, with subsequent development of a tide mark, in which case, careful observation might be appropriate (Fig. 105.5). Since these detachments tend to occur in an older age group, there are also cases in whom severe medical comorbidity precludes any form of treatment.
Treatment
Laser demarcation
Although laser photocoagulation creates an instant adhesion, this is not up to full strength for up to 14 days.15 Rapidly progressing fluid may extend through the area of demarcation before a strong enough adhesion develops. This form of treatment should therefore be used with caution in patients with RRD secondary to “U” tears.
Pneumatic retinopexy
The use of intraocular gas in the treatment of retinal detachment was first described by Ohm in 1911,36 and good results in a large series were reported by Rosengren.37 Modern pneumatic retinopexy was introduced by Hilton and Grizzard in 1986.38 Expanding gas is injected into the vitreous cavity, followed by application of cryotherapy or laser photocoagulation. The technique can be applied in an outpatient setting under local anesthesia. Postoperatively the patient positions their head so that the gas bubble is opposed to the break or breaks. This limits the flow of fluid into the subretinal space, and allows reabsorption of the existing fluid by the retinal pigment epithelium. The technique is most appropriate for detachments with breaks limited to one quadrant, usually superiorly. Complications of pneumatic retinopexy include raised intraocular pressure, and subretinal gas.39 The expanding gas may exert traction inferiorly leading to the creation of new, inferior breaks, particularly in the presence of inferior lattice degeneration.40 New or missed breaks are a common cause of failure following pneumatic retinopexy, accounting for half the failures in one series.41
Pneumatic retinopexy was found to have a comparable success rate to vitrectomy with cryotherapy and gas in a prospective randomized control trial in 120 cases.42 A large multicenter randomized trial compared pneumatic retinopexy with scleral buckling in 198 patients. There was a higher rate of primary reattachment in the scleral buckling group (82% versus 73%), but this difference did not achieve statistical significance (P>0.05). There was no difference in the final reattachment rate (98% versus 99%). However, the patients with pneumatic retinopexy had less morbidity and better final visual acuity.43
A recent meta-analysis comparing pneumatic retinopexy to primary scleral buckling, reported that scleral buckling had a higher primary success rate.44 However, most studies have indicated no difference in the final success rate between the two, and more importantly, no difference in the final visual acuity. A large retrospective series of 302 eyes treated with pneumatic retinopexy showed an average primary success rate of 68%, with a final reattachment rate of 95%.45 Given that pneumatic retinopexy is a relatively quick and simple procedure, with less morbidity than scleral buckling, it is worth considering as an initial procedure. This is particularly the case for patients who have “classic” indications, as the success rate appears higher in this group. In a subgroup of patients with phakic eyes, single breaks, and fluid confined to one superior quadrant, the primary success rate was 97%.45
There is evidence that pneumatic retinopexy is less effective in aphakic and pseudophakic eyes. In a series of 56 eyes, the primary success rate was 81% in a subgroup of phakic eyes but only 43% in eyes which were aphakic or pseudophakic.46 In summary, a high primary success rate with pneumatic retinopexy can be achieved in phakic eyes with “classic” indications. Even if treatment fails, a good final result can be expected following further surgery.
Most surgeons who use pneumatic retinopexy, apply it as a primary procedure, and then employ scleral buckling if it fails. However, pneumatic retinopexy can also be used as an effective method of treating detachments after failed scleral buckling. In most of these cases there is persistent elevation of the retinal break above the buckle, and retinopexy has already been applied. All that is necessary is temporary reduction in fluid flow through the break to allow the retina to settle. In a series of 36 eyes with failed scleral buckling surgery, injection of gas was successful in reattaching the retina in 25 (69.4%).47
Scleral buckling
The aim of buckling surgery is to create an indentation of the sclera beneath the retinal break. The possible mechanisms of action are well described elsewhere in this volume (see Chapter 100, Techniques of scleral buckling) but the effect is to reduce the rate of flow of fluid into the subretinal space, leading to resolution of the detachment. It is important to understand that buckling achieves only closure, and not sealing of the retinal break, the latter being the role of retinopexy. The implication of this is that buckling alone has the same initial success rate whether retinopexy is applied or not, but if the indentation fades, or the buckle is removed, the retinal redetachment will recur. This notion has been confirmed by Chignell who reported success in 26 of 29 cases of retinal detachment treated with scleral buckling and no retinopexy. Follow-up varied from 6 months to 2 years and no redetachments were reported,48 although no buckles needed to be removed during that period. When these cases were followed-up in the long term, late detachments were found in 4 of 46 patients. In all these cases, redetachment occurred because of reopening of the original retinal break, and was associated with progressive reduction of the height of the scleral buckle.49 In another, larger series of scleral buckling without retinopexy, initial success was achieved in 143 of 175 cases (82%), and final success in 158 cases (90%). Causes of initial failure were all related to malposition of the buckle or the development of new breaks, rather than anything to do with retinopexy. Follow-up was only 6 months, so the long-term effect of buckle fade in these patients is not known.50
There is a lack of consensus concerning the best type of buckle to use in any particular circumstance. Limited retinal detachments with single breaks can be treated with a radial element, or a small segmental buckle. Many surgeons supplement the segmental buckle with an encircling band. This has the advantage of helping to maintain the buckle height in the long term. However, if retinopexy has been applied to all the breaks, then this is theoretically unnecessary. Several non-randomized series have produced good results without encirclement and good long-term follow-up.51 By contrast, encirclement is associated with a higher risk of motility disturbance and refractive changes, and can also lead to long-term problems, such as erosion of the buckle through the sclera.52 Singh investigated the role of encirclement in aphakic patients in a prospective, randomized, controlled trial. A total of 84 patients with aphakic retinal detachments were randomized to either local scleral buckling or encirclement. The primary success rate was 90% and 91% in the two groups, respectively.53 Ho et al. reported no difference in success rates between three different buckling methods in a non-randomized study of 128 eyes. However, there were more complications in the group of eyes that were encircled.54
Vitrectomy
Conventional indications
As surgeons became comfortable using vitrectomy techniques to manage cases of vitreous pathology and complex retinal detachments, it became clear that the advantages of an internal approach could also be useful for simpler cases. Kloti was the first to report using vitrectomy for superior bullous detachments.55 A subsequent series reported on vitrectomy and fluid–gas exchange in 29 cases of RRD, in which scleral buckling would have been the usual approach. The reattachment rate following one operation was 79%, increasing to 93% after two operations.56 These results compared favorably with rates for conventional surgery.57 Vitrectomy offers a more successful approach for simple detachments with significant vitreous opacity, or for those with posterior breaks which would otherwise require a large scleral buckle. Other agreed indications include eyes with thin sclera which would make scleral buckling difficult or dangerous. However, as experience has been gained, the use of vitrectomy has increased, so that there is now considerable overlap with current indications for scleral buckling surgery.
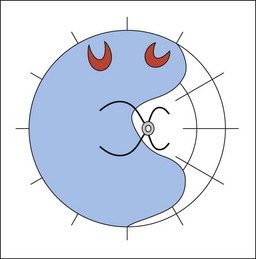
Currently, controversy surrounds the management of medium complexity, bullous, retinal detachments, which represent the majority of cases (Fig. 105.6). Some centers have moved away from scleral buckling towards vitrectomy for the primary management.3,58 Proponents of vitrectomy argue that it can directly eliminate vitreous traction, remove media opacities, and allow better detection and localization of retinal pathology, particularly when using wide-angle viewing systems. Vitrectomy eliminates the risks of buckle-related complications, such as drainage problems,59 choroidal effusions,60 diplopia,61 and extrusion of the explant.62 However, the use of vitrectomy introduces a new set of potential complications, including entry site breaks,63 postoperative nuclear sclerosis,64 and proliferative vitreoretinopathy.65
Many case series of primary vitrectomy for RRD have been reported. The primary reattachment rate varies between 64% and 100%.66 A large study from Japan compared 225 phakic eyes with superior retinal detachments associated with “U” tears. Scleral buckling was used in 138 eyes, and 87 eyes were treated with vitrectomy, according to surgeon preference. Primary and final anatomical success rate were identical between the two groups at 92% and 100%, respectively.67 It is relatively easy to compare reattachment rates between scleral buckling and vitrectomy, and when this is done, the results are similar. However, a valid comparison should also include assessment of the complications, and this is where difficulties occur. This is because the complications are qualitatively different, and there is no scientific method of comparing, e.g., diplopia from a scleral buckle with nuclear cataract from a vitrectomy.
The Scleral Buckling versus Primary Vitrectomy in Rhegmatogenous Retinal Detachment Study (SPR Study) was the first large prospective randomized clinical trial to compare outcomes of two different surgical methods in retinal detachment.68 A total of 45 surgeons in 25 centers recruited a total of 681 patients with “medium complexity” detachments. Medium complexity cases were primary RRDs with breaks of size from 1 to 2 clock hours, multiple breaks, superior bullous detachment, central extension of breaks, or marked vitreous traction. Cases were divided into phakic and aphakic/pseudophakic groups before being randomized into scleral buckling or PPV. The protocol allowed the use of a supplementary buckle in cases undergoing PPV at the discretion of the operating surgeon. Surgeons had carried out at least 100 cases using each method before participating in the study. The primary outcome measure was defined as the change in best corrected visual acuity (BCVA) between the initial examination and the final follow-up at 12 months. Secondary outcome measures were the rate of PVR, and primary anatomical success. The latter was defined as attachment of the retina central to the equator at the final follow-up visit without additional retinal procedures. With this definition, cases having supplemental laser or treatment of macular pucker would be classified as failures, so it is important to realize that the primary anatomical success rate is not equivalent to what many surgeons might understand as primary reattachment rate, which can be derived from the data for retinal redetachment provided in the study. The key results of the study are shown in Table 105.1 and in summary, there was a better improvement of BCVA with scleral buckling in phakic eyes, and a high primary success rate using vitrectomy in aphakic/pseudophakic eyes.
| Outcome | Scleral buckling | Vitrectomy |
|---|---|---|
| Phakic | ||
| Improvement in BCVA | −0.71* | −0.56 |
| Primary success | 63.6% | 63.8% |
| Primary reattachment | 73.7% | 74.9% |
| Aphakic/pseudophakic | ||
| Improvement in BCVA | −0.56 | −0.65 |
| Primary success | 53.4% | 72.0%* |
| Primary reattachment | 60.1% | 79.5%* |
* Difference statistically significant (P < 0.05). SPR, scleral buckling versus primary vitrectomy in the Rhegmatogenous Retinal Detachment Study; BCVA, best corrected visual acuity.
The SPR study is a very important contribution to the evidence base of retinal detachment surgery. Since the study was planned, attention has been focused on the “surgeon factor” in surgical trials, because most surgeons have a preferred technique with which they may get better outcomes. Traditional randomization results in only half the patients having a surgeon using their preferred operation, and a better study design for future trials might be expertise based.69 However, analysis of the results by surgeon in the SPR study has found that the majority of surgeons had similar success rates for both operations.70
Supplementary buckle
Some vitreous remains after vitrectomy, even when shaving of the vitreous base is performed, which may continue to exert traction on retinal breaks, and form a scaffold for later development of PVR. Inferior retinal breaks depend on patient positioning to maintain contact with the tamponade agent. For both these reasons, many surgeons have advocated supplementary scleral buckles. Gartry presented a series of 114 eyes treated with vitrectomy for retinal detachments uncomplicated by PVR. The indication for the majority was media opacity or large posterior breaks. Buckles were used for cases that had been operated on previously, and for those with breaks below one clock hour above the horizontal meridian.71
However, a large series of 275 pseudophakic eyes treated with vitrectomy and no buckling showed no evidence of failure resulting from factors associated with lack of a scleral buckle. The anatomical success rate after one operation was 241 (88%), and the final success rate was 265 (96%). No details are given about the distribution of fluid and the position of retinal breaks in this series. However, since the patients were consecutive, it can reasonably be assumed that many of them had inferior breaks. Of the 34 eyes that were not attached with one operation, 17 were associated with new breaks or opening of old ones. Sixteen had PVR and one had a suprachoroidal hemorrhage. Subsequent surgery included a scleral buckle in 12 eyes.72 A retrospective study of retinal detachments with breaks between 4 and 8 o’clock specifically looked for an advantage of supplementary buckles but failed to find an increased success rate.73 In the SPR study, the use of a buckle in cases randomized to the vitrectomy group was allowed at the discretion of the surgeon. Ancillary analysis found that the use of a supplementary buckle was associated with better success rates in the pseudophakic/aphakic group, but not in the phakic group.68 A supplementary scleral buckle has the disadvantage of introducing additional risks and complications. Although there may be theoretical advantages in selected cases, there is no evidence base to support its widespread use.
Laser versus cryotherapy
All techniques for retinal reattachment require some form of retinopexy to create a chorioretinal adhesion to seal retinal breaks, or wall off areas of detachment. Gonin used thermocautery to achieve this,2 but today only laser photocoagulation and cryotherapy are widely used. Debate continues about the relative merits of each technique.
Cryotherapy has been shown to promote dispersion of viable retinal pigment epithelial cells and to cause breakdown of the blood–retinal barrier. Ryan reported two cases of cystoid macula edema, which occurred following uncomplicated scleral buckling procedures for macular-on retinal detachment.74 Cystoid macular edema, and wrinkling of the inner limiting membrane has also been reported following cryotherapy alone.75 It must be remembered however, that macula pathology, particularly epiretinal membranes also occur following PVD without tears, and the association with cryotherapy is not necessarily causative.
Cryotherapy has been shown to cause breakdown of the blood–retinal barrier. In rabbit eyes treated with confluent laser in one eye and equivalent cryotherapy in the other, there was a significantly greater increase in vitreous fluorophotometry readings in the cryotherapy-treated eyes. However, both eyes returned to normal readings after 14 days.76 Similar findings in man were demonstrated in a randomized trial of cryotherapy and laser photocoagulation in conventional retinal detachment surgery. Patients were treated either with cryotherapy at the time of surgery, or with laser photocoagulation 4 weeks postoperatively. Postoperative flare was measured using laser flare photometry, and was significantly higher in the cryotherapy group than the laser group. In addition visual recovery was slower in the cryotherapy group. However, at 10 weeks postoperatively, there was no difference in visual acuity between the two groups.77 Cryotherapy produces more extensive retinal edema and necrosis in treated areas than laser. Lesions are similar at 14 days with atrophy of the retina and choroid, and a pigmented chorioretinal scar.78
Many studies have examined risk factors for the development of PVR, but results are contradictory. In a large retrospective study of 65 eyes with PVR and 325 controls, Cowley et al. found that the amount of cryotherapy applied, and the use of vitrectomy were independent risk factors for PVR.79 In another retrospective study comparing laser and cryotherapy, no difference in the rate of postoperative PVR was found in those eyes with round hole detachments or traction tears with no preoperative PVR. However, in eyes with traction tears and some preoperative PVR (“curled posterior edges”), cryotherapy was found to be associated with a higher risk of PVR (13/88 14.7%) compared with 1/56 (1.7%). Unfortunately, the size and number of the retinal breaks was not included in the multivariate analysis.80 The importance of including confounding factors was illustrated by the results of another multivariate analysis, which was a prospective study with good data collection, looking at factors associated with success of scleral buckling in a large number of eyes with rhegmatogenous retinal detachment. The vast majority of failures were due to PVR. While the number of applications of cryotherapy was found to be associated with failure after univariate analysis, it was not found to be a significant factor when the other variables such as the size and number of breaks was included.81 A prospective study looking at PVR in a subgroup of 140 patients undergoing vitrectomy for retinal detachment found that cryotherapy was not an independent risk factor for PVR formation.82
Sutureless vitrectomy
The use of sutureless vitrectomy using smaller gauge instruments, 25- and 23-gauge (25G, 23G), has become increasingly popular, but there has been some controversy about the use of sutureless systems in the management of RRD.83 Most surgeons consider that removal of peripheral vitreous is important, and that indentation of the periphery is helpful in locating retinal breaks. Both these steps are more difficult in 25G surgery, and there were early reports of high redetachment rates. In a series of 53 eyes managed by 25G vitrectomy, the primary success rate was only 74%, the reasons for failure being either new retinal breaks or PVR. In addition, three eyes (6%) in this series developed postoperative choroidal hemorrhage.84 The authors speculated that the lower flow rate associated with 25G might leave higher concentrations of cytokines in the eye. Other studies have reported higher success rates. A small study of 25G vitrectomy in the management of non-complex, pseudophakic retinal detachments reported primary success in all but one case.85 More recent studies have reported reasonable success rates (primary success 92.9%) for 25G vitrectomy and gas, without the use of a supplementary buckle.86
Variations
The national audit of primary surgery for RRD gave useful information on the situation in the UK. Of the surgeons who responded, 38% performed retinal detachment surgery. Of these, 105 (41%) declared a special interest in retinal surgery, and were therefore defined as “specialists” for the purposes of the audit.87 Detachments were graded for severity so that, e.g., grade 2 detachments were defined as those with breaks within the same quadrant, and/or less than two quadrants of retinal detachment. In this group, the success rate of specialists was 87% compared with only 70% for non-specialists. The overall proportion of patients who had scleral buckling was 83% of the sample, the remaining 17% had vitrectomy. Interestingly, no patients in this survey had pneumatic retinopexy, reflecting a significant difference in practice between the UK and the USA. The primary success rate overall (specialists and nonspecialists) was 77%.88 Since this report, the use of vitrectomy in the UK for retinal detachments has been increasing. Another report from a single center in the UK reported three cycles of audit over a 10-year period. They reported a significant increase in primary reattachment rates which rose from 67% in Audit 1 to 87% in Audit 3 (P = 0.0004). In the same period, the proportion of primary vitrectomy increased from 1.5% to 48%.89
It is not just changes in preferred technique which are occurring, but the range of pathology is also shifting, mostly because of the aging population, and the increasing number of patients undergoing cataract surgery. The proportion of aphakic/pseudophakic patients with RRD has increased to 30% over the last 10 years.90 These findings were confirmed in a similar study from London. More cases were pseudophakic and fewer aphakic in 1999 than in 1979–1980. Vitrectomy was a primary procedure in 63% of cases in 1999 but in only 1% in 1979–1980. Anatomical success rates were statistically similar: 79.8% primary and 88.8% final success in 1979–1980, compared with 84% primary and 93.6% final success in 1999.58
Variations between surgeons are also extensive. One survey of the American Society of Retinal Specialists (ASRS) members found that surgeons who had been in practice for 10 years or less were significantly more likely to select a pneumatic retinopexy for certain forms of retinal detachment.91 The increase in popularity of pneumatic retinopexy over scleral buckling was confirmed in another survey of retina and ASRS members living in North America. The number of respondents choosing it rather than scleral buckling for a particular case had doubled since a similar survey 7 years earlier. Another showed that the presence of factors that were additional to the “classic” indications for pneumatic retinopexy were more likely to make the respondents choose scleral buckling.92 Interestingly, this survey also found that pneumatic retinopexy was more likely to be applied to uninsured patients with similar indications.
Conclusion
The treatment of rhegmatogenous retinal detachment has advanced considerably since the pioneering work of Gonin. Both primary and final success rates are now high, and it is only a small minority of cases whose retinas remain detached after one or more operations. There is broad agreement about the best method for some categories of detachment, but for the majority of cases, there is both lack of agreement, and lack of an evidence base to make rational choices of technique. Despite the contribution of the SPR study, there remains a need for further evidence from well-conducted trials, and when setting up such trials, it is important to consider factors other than success rate. The goal of treatment should be to choose a method for any particular case that has the best chance of anatomical success, but with the lowest risk of introducing further ocular morbidity. As Wilkinson put it: “The best method of repairing a particular detachment will remain a matter of speculation and bias until more appropriate data are acquired.”93
1 Vail DT. An inquiry into results of the established treatment of detachment of the retina and a new theory. Trans Am Acad Ophthalmol Otolaryngol. 1912;17:29.
2 Gonin J. Le traitment de décollement retinien. Ann Oculist. 1921;158:175.
3 Ramulu PY, Do DV, Corcoran KJ, et al. Use of Retinal Procedures in Medicare Beneficiaries From 1997 to 2007. Arch Ophthalmol. 2010;128:1335–1340.
4 Tillery WV, Lucier AC. Round atrophic holes in lattice degeneration – an important cause of phakic retinal detachment. Trans Am Acad Ophthalmol Otolaryngol. 1976;81:509–518.
5 Morse PH, Scheie HG. Prophylactic cryoretinopexy of retinal breaks. Arch Ophthalmol. 1974;92:204–207.
6 Murakami-Nagasako F, Ohba N. Phakic retinal detachment associated with atrophic hole of lattice degeneration of the retina. Graefe’s Arch Clin Exp Ophthalmol. 1983;220:175–178.
7 Ung T, Comer MB, Ang AJ, et al. Clinical features and surgical management of retinal detachment secondary to round retinal holes. Eye. 2005;19:665–669.
8 Byer NE. The natural history of asymptomatic retinal breaks. Ophthalmology. 1982;89:1033–1039.
9 Byer NE. What happens to untreated asymptomatic retinal breaks, and are they affected by posterior vitreous detachment. Ophthalmology. 1998;105:1045–1050.
10 Benson WE, Nantawan P, Morse PH. Characteristics and prognosis of retinal detachments and demarcation lines. Am J Ophthalmol. 1977;84:641–644.
11 Brod RD, Flynn HW, Lightman DA. Asymptomatic rhegmatogenous retinal detachments. Arch Ophthalmol. 1995;113:1030–1032.
12 Jarret WH. Retinal detachment: is reparative surgery always necessary? Trans Am Ophthalmol Soc. 1988;86:307–320.
13 Greenberg PB, Baumal CR. Laser therapy for rhegmatogenous retinal detachment. Curr Opinion Ophthalmol. 2001;12:171–174.
14 Folk JC, Sneed SR, Folberg R, et al. Early retinal adhesion from laser photocoagulation. Ophthalmology. 1989;96:1523–1525.
15 Yoon YH, Marmor MF. Rapid enhancement of retinal adhesion by laser photocoagulation. Ophthalmology. 1988;95:1385–1388.
16 Okun E, Cibis PA. Photocoagulation in “limited” retinal detachment and breaks without detachment. In: McPherson A, ed. New and controversial aspects of retinal detachment. New York: Harper and Row; 1968:164–172.
17 Treplin MCW. Treatment of retinal detachments by laser photocoagulation. Trans Ophthalmol Soc UK. 1982;102:182–183.
18 Gratton I, Gazocchi M, Simonini F, et al. Argon laser photocoagulation in the management of retinal detachment and predisposing lesions. Lasers Surg Med. 1984;4:337–344.
19 Vrabec TR, Baumal CR. Demarcation laser photocoagulation of selected macular-sparring rhegmatogenous retinal detachments. Ophthalmology. 2000;107:1063–1067.
20 Tillery WV, Lucier AC. Round atrophic holes in lattice degeneration. Trans Am Acad Ophthalmol Otolaryngol. 1976;81:509–518.
21 Greven CM, Wall AB, Slusher MM. Anatomical and visual results in asymptomatic clinical rhegmatogenous retinal detachment repaired by scleral buckling. Am J Ophthalmol. 1999;128:618–620.
22 Smiddy WE, Green WR. Retinal dialysis: pathology and pathogenesis. Retina. 1982;2:94–116.
23 Dumas JJ. Retinal detachment following contusion of the eye. Int Ophthalmol Clin. 1967;7:19–38.
24 Zion VM, Burton TC. Retinal dialysis. Arch Ophthalmol. 1980;98:1971–1974.
25 Brown GC, Tasman WS. Familial retinal dialysis. Can J Ophthalmol. 1980;5:193–195.
26 Kennedy CJ, Parker CE, McAllister IL. Retinal detachment caused by retinal dialysis. Aust NZ J Ophthalmol. 1997;25:25–30.
27 Bonnet M, Moyenin P, Pecoldowa C, et al. Retinal detachment caused by a tear at the ora serrata. J Francais d’Ophthalmol. 1986;9:231–242.
28 Cox MS, Schepens CL, Freeman HM. Retinal detachment due to ocular contusion. Arch Ophthalmol. 1966;76:678–685.
29 Ross WH. Traumatic retinal dialyses. Arch Ophthalmol. 1981;99:1371–1374.
30 Johnston PB. Traumatic retinal detachment. Br J Ophthalmol. 1991;75:18–21.
31 Ivanisevic M. The natural history of untreated rhegmatogenous retinal detachment. Ophthalmologica. 1997;211:90–92.
32 Bradford JD, Wilkinson CP, Fransen SR. Pseudophakic retinal detachments. The relationships between retinal tears and the time following cataract surgery at which they occur. Retina. 1989;9:181–186.
33 Wilkinson CP. Phakic retinal detachments in the elderly. Retina. 1995;15:220–223.
34 Machemer R. The importance of fluid absorption, traction, intraocular currents and chorioretinal scars in the therapy of rhegmatogenous retinal detachments. Am J Ophthalmol. 1984;98:681–693.
35 Burton TC. Recovery of visual acuity after retinal detachment involving the macula. Trans Am Ophthalmol Soc. 1982;80:475–497.
36 Ohm J. Uber die behandlung der Netzhaulablosung durch operative Enlleerung der subretinalen Flussigheit und Einspiritzung von Luft in den Glaskorper. Graefes Arch Ophthalmol. 1911;79:442–450.
37 Rosengren B. Results of treatment of detachment of the retina with diathermy and injection of air into the vitreous. Acta Ophthalmol. 1938;16:573–579.
38 Hilton GF, Grizzard WS. Pneumatic retinopexy. A two-step outpatient operation without conjunctival incision. Ophthalmology. 1986;93:626–641.
39 Wirostko WJ, Han DP, Perkins SL. Complications of pneumatic retinopexy. Curr Opinion Ophthalmol. 2000;11:195–200.
40 Poliner LS, Grand MG, Schoch LH, et al. New retinal detachment after pneumatic retinopexy. Ophthalmology. 1987;94:315–318.
41 Grizzard WS, Hilton GF, Hammer ME, et al. Pneumatic retinopexy failures. Cause, prevention, timing, and management. Ophthalmology. 1995;102:929–936.
42 Van Effenterre G, Haut J, Larricart P, et al. Gas tamponade as a single technique in the treatment of retinal detachment: is vitrectomy needed? Graefe’s Arch Clinic Exp Ophthalmol. 1987;225:254–258.
43 Tornambe PE, Hilton GF. Pneumatic retinopexy. A multicenter randomized controlled clinical trial comparing pneumatic retinopexy with scleral buckling. The Retinal Detachment Study Group. Ophthalmology. 1989;96:772–783.
44 Sharma S. Meta-analysis of clinical trials comparing scleral buckling surgery to pneumatic retinopexy. Evid Base Eye Care. 2002;3:125–128.
45 Tornambe PE. Pneumatic retinopexy: the evolution of case selection and surgical technique. A twelve-year study of 302 eyes. Trans Am Ophthalmol Soc. 1997;95:551–578.
46 McAllister IL, Meyers SM, Zegarra H, et al. Comparison of pneumatic retinopexy with alternative surgical techniques. Ophthalmology. 1988;95:877–883.
47 Sharma T, Badrinath SS, Mukesh BN, et al. A multivariate analysis of anatomic success of recurrent retinal detachment treated with pneumatic retinopexy. Ophthalmology. 1997;04:2014–2017.
48 Chignell AH. Retinal detachment surgery without cryotherapy. Trans Ophthalmol Soc UK. 1977;97:30–32.
49 Chignell AH, Wong D. The role of induced choroidal retinal adhesions in retinal detachment surgery. Trans Ophthalmol Soc UK. 1986;105:580–582.
50 Fetkenhour CL, Hauch TL. Scleral buckling without thermal adhesion. Am J Ophthalmol. 1980;89:662–666.
51 Kreissig I, Simader E, Fahle M, et al. Visual acuity after segmental buckling and non-drainage: a 15-year follow-up. Eur J Ophthalmol. 1995;5:240–246.
52 Deramo VA, Haupert CL, Fekrat S, et al. Hypotony caused by scleral buckle erosion in Marfan syndrome. Am J Ophthalmol. 2001;132:429–431.
53 Singh M. Surgery of aphakic retinal detachment. Br J Ophthalmol. 1988;72:820–822.
54 Ho CL, Chen KJ, See LC. Selection of scleral buckling for primary retinal detachment. Ophthalmologica. 2002;216:33–39.
55 Kloti R. Amotio-chirurgie ohne sklraeindellung. Primäre vitrektomie. Klin Mbl Augenheilk. 1983;182:474–478.
56 Escoffery RE, Olk RJ, Grand MG, et al. Vitrectomy without scleral buckling for primary rhegmatogenous retinal detachment. Am J Ophthalmol. 1985;99:275–281.
57 Rachel WF, Burton TC. Changing concepts of failure after retinal detachment surgery. Arch Ophthalmol. 1979;97:480–483.
58 Minihan M, Tanner V, Williamson TH. Primary rhegmatogenous retinal detachment: 20 years of change. Br J Ophthalmol. 2001;85:546–548.
59 Wilkinson CP, Bradford RH. Complications of draining subretinal fluid. Retina. 1984;1:1–4.
60 Packer AJ, Maggiano JM, Aaberg TM, et al. Serous choroidal detachment after retinal detachment surgery. Arch Ophthalmol. 1983;101:1221–1224.
61 Smiddy WE, Loupe D, Michels RG, et al. Extraocular muscle imbalance after scleral buckling surgery. Ophthalmology. 1989;96:1485–1490.
62 Hilton GF, Wallyn RH. The removal of scleral buckles. Arch Ophthalmol. 1978;96:2061–2063.
63 Carter JB, Michels RG, Glaser BM, et al. Iatrogenic breaks complicating pars plana vitrectomy. Ophthalmology. 1990;97:848–854.
64 de Bustros S, Thompson JT, Michels RG, et al. Nuclear sclerosis after vitrectomy for idiopathic epiretinal membranes. Am J Ophthalmol. 1988;105:160–164.
65 Cowley M, Conway BP, Campochiaro PA, et al. Clinical risk factors for proliferative vitreoretinopathy. Arch Ophthalmol. 1989;107:1147–1157.
66 Brazitikos PD, D’Amico DJ, Tsinopoulos IT, et al. Primary vitrectomy with perfluoro-n-octane use in the treatment of pseudophakic retinal detachments with undetected retinal breaks. Retina. 1999;19:103–109.
67 Miki D, Hida T, Hotta K, et al. Comparison of scleral buckling and vitrectomy for retinal detachment resulting from flap tears in superior quadrants. Japn J Ophthalmol. 2001;45:187–191.
68 Heimann H, Bartz-Schmidt KU, Bornfeld N, et al. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment. A Prospective Randomized Multicenter Clinical Study. Ophthalmology. 2007;114:2142–2154.
69 Devereaux PJ, Bhandari M, Clarke M, et al. Need for expertise based randomised controlled trials. BMJ. 2005;330:88–91.
70 Heimann H, Bornfeld N, Bartz-Schmidt KU, et al. Analysis of the Surgeon Factor in the Treatment Results of Rhegmatogenous Retinal Detachment in the “Scleral Buckling versus Primary Vitrectomy in Rhegmatogenous Retinal Detachment Study. Klin Monatsbl Augenheilkd. 2009;226:991–998.
71 Gartry DS, Chignell AH, Franks WA, et al. Pars plana vitrectomy for the treatment of rhegmatogenous retinal detachment uncomplicated by advanced proliferative vitreoretinopathy. Br J Ophthalmol. 1993;77:199–203.
72 Campo RV, Sipperley JO, Sneed SR, et al. Pars plana vitrectomy without scleral buckle for pseudophakic retinal detachments. Ophthalmology. 1999;106:1811–1815.
73 Wickham LJ, Connor M, Aylward GW. Vitrectomy and gas for inferior break retinal detachments. Br J Ophthalmol. 2004;88:1376–1379.
74 Ryan SJ. Cystoid maculopathy in phakic retinal detachment procedures. Am J Ophthalmol. 1973;76:519.
75 Kimball RW, Morse PH, Benson WE. Cystoid macular edema after cryotherapy. Am J Ophthalmol. 1978;86:572–573.
76 Jaccoma EH, Conway BP, Campochiaro PA. Cryotherapy causes extensive breakdown of the blood-retinal barrier. Arch Ophthalmol. 1985;103:1728–1730.
77 Veckeneer M, Van Overdam K, Bouwens D, et al. Randomized clinical trial of cryotherapy versus laser photocoagulation for retinopexy in conventional retinal detachment surgery. Am J Ophthalmol. 2001;132:343–347.
78 Curtin VT, Fujino T, Norton EWD. Comparative histopathology of cryosurgery and photocoagulation. Arch Ophthalmol. 1966;75:674–682.
79 Cowley M, Conway BP, Campochiaro PA, et al. Clinical risk factors for proliferative vitreoretinopathy. Arch Ophthalmol. 1989;107:1147–1151.
80 Bonnet M, Fleury J, Guenoun S, et al. Cryopexy in primary rhegmatogenous retinal detachment: a risk factor for post-operative proliferative vitreoretinopathy. Graefe’s Arch Exp Ophthalmol. 1996;234:739–743.
81 Grizzard WS, Hilton GF, Hammer ME, Taren D. A multivariate analysis of anatomic success of retinal detachments treated with scleral buckling. Graefes Arch Exp Ophthalmol. 1994;232:1–7.
82 Kon CH, Asaria RHY, Occleston NL, et al. Risk factors for proliferative vitreoretinopathy after primary vitrectomy: a prospective study. Br J Ophthalmol. 2000;84:506–511.
83 Heimann H. Primary 25- and 23-gauge vitrectomy in the treatment of rhegmatogenous retinal detachment – advancement of surgical technique or erroneous trend? Klin Monats Augen. 2008;225:947–956.
84 Lai MM, Runby AJ, Sarrafizadeh R, et al. Repair of primary rhegmatogenous retinal detachment using 25-gauge transconjunctival sutureless vitrectomy. Retina. 2008;28:729–734.
85 Acar N, Kapran Z, Altan T, et al. Primary 25-gauge sutureless vitrectomy with oblique sclerotomies in pseudophakic retinal detachment. Retina. 2008;28:1068–1074.
86 Miller DM, Riemann CD, Foster RE, et al. Primary repair of retinal detachment with 25-gauge pars plana vitrectomy. Retina. 2008;28:931–936.
87 Thompson JA, Snead MP, Billington BM, et al. National audit of the outcome of primary surgery for rhegmatogenous retinal detachment. I. Sample and methods. Eye. 2002;16:766–770.
88 Thompson JA, Snead MP, Billington BM, et al. National audit of the outcome of primary surgery for rhegmatogenous retinal detachment. II. Clinical outcomes. Eye. 2002;16:771–777.
89 Johnson Z, Ramsay A, Cottrell D, et al. Triple cycle audit of primary retinal detachment surgery. Eye. 2002;16:513–518.
90 Ah-Fat FG, Sharma MC, Majid MA, et al. Trends in vitreoretinal surgery at a tertiary referral centre: 1987–1996. Br J Ophthalmol. 1999;83:396–398.
91 Snyder WB, Bloome MA, Birch DG. Pneumatic retinopexy versus scleral buckle: preferences of Vitreous Society members. Retina. 1992;12:43–45.
92 Wild MR, Ruby AJ, Rosenshein J. Pneumatic retinopexy: a survey of current practice patterns among the vitreous society members. Ophthalmic Surg Lasers. 2000;31:76–81.
93 Wilkinson CP. Wanted. Optimal data regarding surgery for retinal detachment. Retina. 1998;18:199–201.