Ophthalmic Anaesthesia
Ophthalmic surgery can be classified into subspecialties and intraocular or extraocular procedures may be performed (Table 30.1); each has different anaesthetic requirements.
TABLE 30.1
Categorization of Ophthalmic Surgery
Ophthalmology Subspecialities
Paediatric
Oculoplastic
Vitreoretinal
Anterior segment
Glaucoma
Neuro-ophthalmology
Extraocular Operations
Globe and orbit
Eyebrow and eyelid
Lacrimal system
Muscles
Conjunctiva
Cornea, surface
Intraocular Operations
Iris and anterior chamber
Lens and cataract
Vitreous
Retina
Cornea, full thickness
PHYSIOLOGY OF THE EYE
Control of Intraocular Pressure
Intraocular pressure depends on the rigidity of the sclera as well as any external pressure. Functionally, it is a balance between the production and removal of aqueous humour (approximately 2.5 μL min− 1). Factors which affect IOP are shown in Table 30.2. Chronic changes in IOP (normally 10–25 mmHg (mean 15)), either upwards or downwards cause structural effects and loss of function. There is a relationship between increasing axial length and increasing IOP. Low pressure results in blood–aqueous barrier breakdown, cataract, macular oedema and papilloedema. High pressure causes iris sphincter paralysis, iris atrophy, lens opacities and optic nerve atrophy.
TABLE 30.2
Factors Which Affect Intraocular Pressure (IOP)
| IOP | Increase IOP | Decrease IOP |
| Systemic | Age Large increase in blood pressure Increased carotid blood flow Increased central venous pressure Valsalva manoeuvre Carotid-cavernous fistula Plasma hypo-osmolality Hypercapnia Sympathetic stimulation |
Exercise Large decrease in blood pressure Decreased carotid blood flow Decreased central venous pressure Parasympathetic stimulation Pregnancy Hypothermia Acidosis Plasma hyperosmolality Adrenalectomy General anaesthesia |
| Local | Increased episcleral venous pressure Blockage of ophthalmic vein Blockage of trabecular meshwork Contraction of extraocular muscles Restricted extraocular muscle Acute external pressure Forced blinking Relaxation of accommodation Prostaglandin release (biphasic) Hypersecretion of aqueous |
Decreased episcleral venous pressure Decreased ophthalmic artery blood flow Prolonged external pressure Retrobulbar anaesthesia Ocular trauma Intraocular surgery Retinal detachment Choroidal detachment Inflammation Prostaglandins (biphasic) Accommodation Increased aqueous outflow |
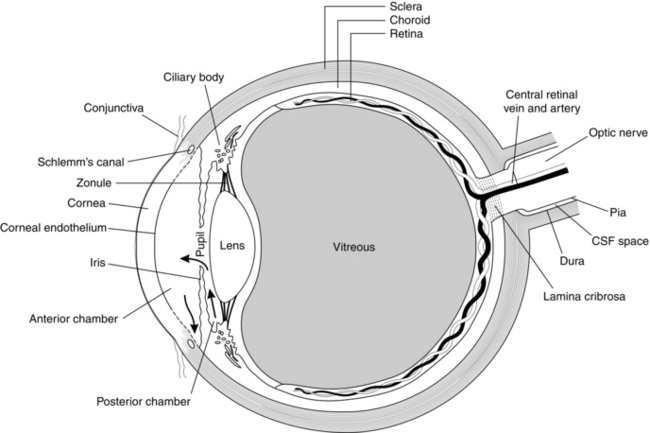
The aqueous flows from the ciliary body through the trabecular meshwork into the anterior chamber before exiting through the angle of Schlemm (Fig. 30.1). The sum of the hydrostatic inflow and the active aqueous production minus the active resorption and passive filtration must equal zero to achieve balance. Alteration of any individual feature can lead to changes in IOP.
CONDITIONS FOR INTRAOCULAR SURGERY
Effect of Anaesthetic Drugs on Intraocular Pressure
Muscle Relaxants
Succinylcholine increases intraocular pressure, with a maximal effect 2 min after i.v. administration, but the pressure returns to baseline values after 5 min. This effect is thought to be caused by the increase in tone of the extraocular muscles and intraocular vasodilatation. Pretreatment with a small dose of a non-depolarizing muscle relaxant does not obtund this response reliably. The problems involved with the use of succinylcholine in the patient with penetrating eye injury are discussed on page 616.
Non-depolarizing muscle relaxants have no significant direct effects on IOP.
CHOICE OF ANAESTHESIA
Ophthalmic surgery can be carried out under either local or general anaesthesia provided that there is both consent and compliance. The type of surgery, its urgency and the age and fitness of the patient influence the choice (Table 30.3). Local anaesthesia is preferred for older and sicker patients, because the stress response to surgery is diminished and complications such as postoperative confusion, nausea, vomiting and urinary retention are mostly eliminated. Younger patients may sometimes be too anxious for local anaesthesia and are usually managed with general anaesthesia.
TABLE 30.3
Preferred Anaesthetic Technique for Common Surgical Procedures in Ophthalmology
Local Anaesthesia
Cataract
Glaucoma techniques
Minor extraocular plastic surgery
Laser dacrocystorhinostomy
Minor anterior segment procedures
Simple vitrectomies
General Anaesthesia
Paediatric surgery
Squint surgery
Major oculoplastic surgery
Dacrocystorhinostomy
Penetrating keratoplasty
Orbital trauma repair
Penetrating eye injuries
Complex vitreoretinal surgery
General Anaesthesia
NOMENCLATURE OF BLOCKS
Relevant Anatomy
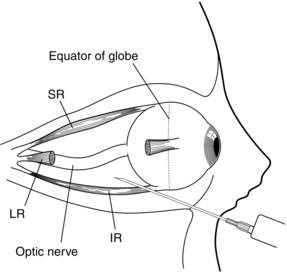
The orbit is a four-sided irregular pyramid with its apex pointing posteromedially and its base anteriorly. The annulus of Zinn is a fibrous ring which arises from the superior orbital fissure. Eye movements are controlled by four rectus muscles (inferior, lateral, medial and superior), and the superior oblique and inferior oblique muscles (Fig. 30.3). These muscles arise from the annulus of Zinn and insert on the globe anterior to the equator to form an incomplete cone. The distance from annulus to inferior temporal orbital rim ranges from 42 to 54 mm. It is very important that the needle should not be inserted too far, close to the annulus, where the vital nerves and vessels are tightly packed.
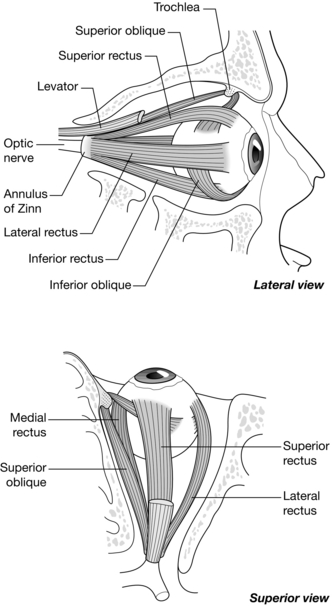
FIGURE 30.3 Extraocular muscles of the eye. See text for details. (Adapted from Gray, Henry. Anatomy of the human body. Lea & Febiger, Philadelphia 1918; Bartleby.com, 2000.)
The optic nerve (II), oculomotor nerve (III, containing superior and inferior branches), abducent nerve (VI), nasociliary nerve (a branch of nerve V), ciliary ganglion and vessels lie in the cone (Fig. 30.4). The ophthalmic division of the oculomotor nerve divides into superior and inferior branches before emerging from the superior orbital fissure. The superior branch supplies superior rectus and levator palpebrae superioris muscles. The inferior branch divides into three to supply the medial rectus, the inferior rectus and the inferior oblique muscles. The abducent nerve emerges from the superior orbital fissure beneath the inferior branch of the oculomotor nerve to supply the lateral rectus muscle. The trochlear nerve (IV) courses outside the cone but then branches and enters the cone to supply the superior oblique muscle. An incomplete block of this nerve leads to retained activity of the superior oblique muscle and this occurs frequently. Squeezing and closing of the eyelids are controlled by the zygomatic branch of the facial nerve (VII), which supplies the motor innervation to the orbicularis oculi muscle. This nerve emerges from the foramen spinosum at the base of the skull, anterior to the mastoid and behind the earlobe. It passes through the parotid gland before crossing the condyle of the mandible, and then passes superficial to the zygoma and malar bone before its terminal fibres ramify to supply the deep surface of the orbicularis oculi. The facial nerve also supplies secreto-motor parasympathetic fibres to the lacrimal glands, and glands of the nasal and palatine mucosa.
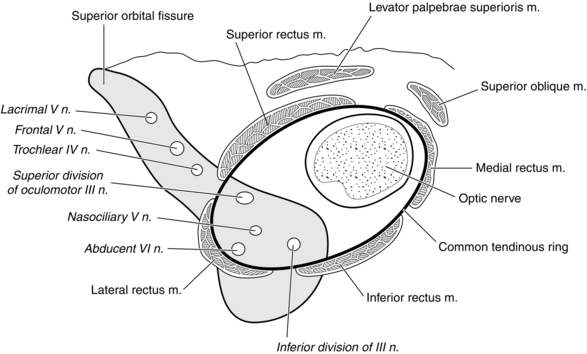
FIGURE 30.4 Anatomy of the right orbit: relationship of the four rectus muscles and the apex of the cone to the orbital nerve supply.
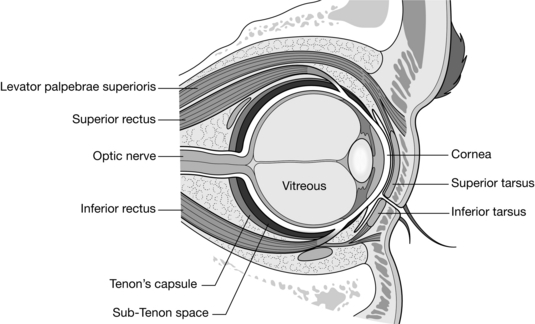
Tenon’s capsule or bulbar fascia is a membrane which envelops the eyeball from the optic nerve to the sclerocorneal junction, separating it from the orbital fat and forming a socket in which it moves (Fig. 30.5). The capsule originates at the limbus and extends posteriorly to the optic nerve and as sleeves along the extraocular muscles. Tenon’s capsule is divided arbitrarily by the equator of the globe into anterior and posterior portions. Anterior Tenon’s capsule is adherent to episcleral tissue from the limbus posteriorly for about 5–10 mm and is fused with the intermuscular septum of the extraocular muscles and overlying bulbar conjunctiva. The conjunctiva fuses with Tenon’s capsule in this area and the sub-Tenon space can be accessed easily through an incision 5–10 mm behind the limbus. The posterior sub-Tenon’s capsule is thinner and passes round to the optic nerve, separating the globe from the contents of the retrobulbar space. Posteriorly, the sheath fuses with the openings around the optic nerve.
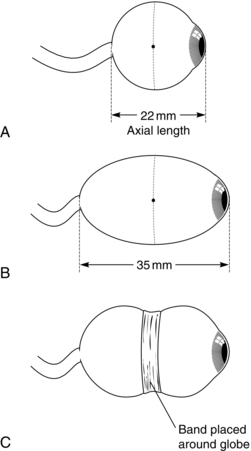
Selection of Patients and Blocks
Preoperative assessment is generally limited to medical history, drug history and physical examination. According to the UK Joint Colleges Guidelines 2012, routine investigations are unnecessary if local anaesthesia is to be employed and these are performed only if it is thought that the results may lead to improved general health of the patient. Patients are not fasted and this is particularly helpful in managing patients with diabetes mellitus who can receive all their normal medications and achieve better glycaemic control in the perioperative period. The blood sugar concentration should still be checked. Patients receiving anticoagulants and antiplatelet agents are advised to continue their usual medications unless told otherwise. Warfarin therapy is not considered an absolute contraindication to local anaesthesia provided that the preoperative INR value is in the therapeutic target range; a sub-Tenon’s block or topical anaesthesia is preferred. The axial length of the eye is usually measured before cataract surgery and serious caution in the use of needle blocks is required if the axial length exceeds 26 mm (Fig. 30.6) or if the axial length is unknown, e.g. in surgery for glaucoma. Antibiotics are not necessary in patients with valvular heart disease. Premedication is not usually necessary but, if needed, may be given intravenously just before the local anaesthetic block is inserted.
OPHTHALMIC REGIONAL BLOCKS
Needle-Based Blocks
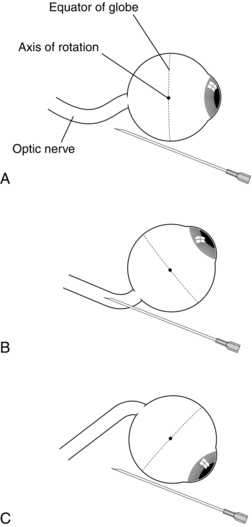
Modern Retrobulbar Block: Surface anaesthesia is obtained with local anaesthetic drops (oxybuprocaine 0.4% or similar). The conjunctiva is cleaned with aqueous 5% povidone iodine. Evidence-based literature suggests that the eye should be kept in the neutral (primary) gaze position at all times and a needle length shorter than 31 mm is inserted through the skin or conjunctiva in the inferotemporal quadrant as far lateral as possible below the lateral rectus. The needle is directed upwards and inwards, with the needle always tangential to the globe. A volume of 4–5 mL of local anaesthetic agent of choice such as 2% lidocaine is injected. A separate facial nerve block is not required.
Inferotemporal Peribulbar Block: Surface anaesthesia and asepsis are obtained as above. The globe is kept in a neutral gaze position and a needle of less than 31 mm in length is inserted as far as possible in the extreme inferonasal quadrant through the conjunctiva or lower lid. A peribulbar block is essentially similar to a modern retrobulbar block but the needle is not directed upwards and inwards and the needle always remains tangential to the globe along the inferior orbital floor (Fig. 30.7). A volume of 5–6 mL of local anaesthetic agent is injected. However, more than 60% of patients require a supplementary injection in the form of a medial peribulbar block.
Medial Peribulbar Block: A supplementary injection is often required either in the same quadrant or through an injection in the medial compartment and is called a medial peribulbar block. A needle is inserted between the caruncle and the medial canthus to a depth of 1–1.5 cm and 3–5 mL of local anaesthetic is injected. A single medial peribulbar block with 6–8 mL of local anaesthetic has been advocated if akinesia is essential in patients with myopic eyes.
Complications of Ophthalmic Regional Blocks
Orbital Haemorrhage
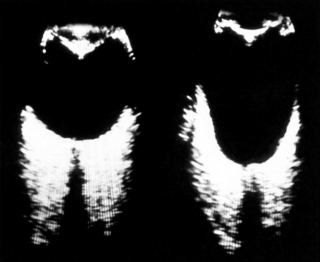
Orbital haemorrhage is a sight-threatening complication of intraconal and extraconal anaesthesia as well as, rarely, sub-Tenon’s block (Fig. 30.8). It occurs with a frequency of between 0.1 and 3% following needle-based blocks. The haemorrhage may be venous or arterial in origin and may be concealed or revealed. Venous bleeding is slow and usually stops. Venous haemorrhage usually presents as markedly bloodstained chemosis and raised IOP. It may be possible to reduce the IOP by digital massage and cautious application of an IOP-reducing device to such an extent that surgery can proceed safely. Before the decision is made to proceed with surgery or postpone it for a few days, it is advisable to measure and record IOP. Arterial bleeding is rapid, with blood filling the periorbital tissues, increasing tissue volume and pressure. This is transmitted to the globe, raising the IOP. Urgent measures must be taken to stop the haemorrhage and reduce IOP. Firm digital pressure usually stops the bleeding and, when it has been arrested, consideration must be given to reducing the IOP so that the blood supply to the retina is not compromised. Lateral canthotomy, acetazolamide or mannitol, or even paracentesis, may need to be considered in consultation with the ophthalmologist.
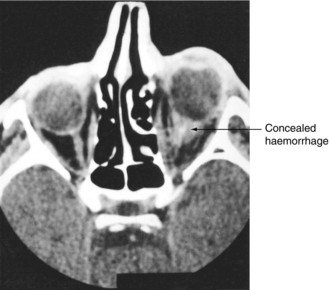
FIGURE 30.8 CT scan taken in coronal section of a patient following an intraconal haemorrhage. Note the marked proptosis of the right eye and the confined space occupied by the haemorrhage. This was a concealed haemorrhage because, despite elevated intraocular pressure and proptosis, no signs of bleeding or bruising were evident until the next day.
Prevention of Haemorrhage: Straining due to anxiety during the block leads to engorgement and potential puncture of vessels around the eye. Sedation may help and the patient should be encouraged to breathe quietly through an open mouth and so prevent a Valsalva manoeuvre. The fewer injections that are made into the orbit, the less are the chances of damaging a blood vessel. Cutting and slicing movements at the needle tip should be avoided. Fine needles are less traumatic than thicker ones. Deep intraorbital injections must be avoided. The inferotemporal quadrant has fewer blood vessels and is less hazardous. It is advisable to apply firm digital pressure to the orbit as soon as the needle is withdrawn after any intraorbital injection, as this reduces any tendency to ooze.
Central Spread of Local Anaesthetic Agent
Mechanism: The cerebral dura mater provides a tubular sheath for the optic nerve as it passes through the optic foramen. This sheath fuses to the epineurium of the optic nerve, providing a potential conduit for local anaesthetic to pass subdurally to the brain. Central spread can occur on injection if the needle tip has entered the optic nerve sheath. Central spread following sub-Tenon’s block has also been reported. Even an injection of a small volume of local anaesthetic may enter the central nervous system and/or cross the optic chiasma to the opposite eye and may cause life-threatening sequelae, e.g. catastrophic cardiorespiratory collapse. The time of onset of symptoms is variable but usually appears in the first 15 min after injection. Central spread may occur on rare occasions if an orbital artery is cannulated by the needle tip, resulting in retrograde spread up the artery until it meets a branch, where it can then flow in a cephalad direction; in addition to orbital haemorrhage, systemic collapse is almost instantaneous.
Signs and Symptoms of Central Spread: The symptomatology of central spread is varied and depends upon which part of the central nervous system is affected by the local anaesthetic. Because of the anatomical proximity of the optic nerve to the midbrain, it is usual for this area to be involved. Signs and symptoms involving the cardiovascular and respiratory systems, temperature regulation, vomiting, temporary hemiplegia, aphasia and generalized convulsions have been described. Palsy of the contralateral oculomotor and trochlear nerves with amaurosis (loss of vision) is pathognomonic of central nervous system spread and should be sought in any patient whose response to questions following block are not as crisp as they were beforehand.
Treatment of Central Spread: Cardiorespiratory arrest may occur and should be treated as at any other arrest. Bradycardia requires treatment with an anticholinergic drug. Asystole has been reported rarely, but if it occurs, intravenous vasoactive drugs are required. Respiratory depression or apnoea necessitates ventilatory support, intravenous fluid therapy and administration of supplemental oxygen. Convulsions are treated with an intravenous induction agent such as propofol, or a benzodiazepine.
Prevention of Central Spread: Intraconal or extraconal injections should always be undertaken with the patient looking in the neutral or the primary gaze position. The optic nerve is a C-shaped structure and there is slackness in the primary gaze position so that it lies out of the way of the advancing needle (Fig. 30.9). If the needle encounters the optic nerve in this position, it is unlikely to damage or perforate its sheath because slackness in the structure allows the nerve to be pushed aside. The most dangerous position is when the patient looks upwards and inwards, as this presents the stretched nerve to a needle directed from the inferotemporal quadrant. The injection should not be made deep into the orbit, where the optic nerve is likely to be tethered.
Damage to the Globe
Global puncture is a serious complication of ophthalmic blocks. It has been reported following both intraconal and extraconal blocks and even following sub-Tenon’s and subconjunctival injection. Perforation of the globe has entry and exit wounds whereas penetration of the globe has only the wound of entry. With appropriate care, it should be a very rare complication because the sclera is a tough structure and, in most patients, is not perforated easily. Puncture of the eyeball is most likely to occur in patients with high myopia, previous retinal banding, posterior staphyloma or a deeply sunken eye in a narrow orbit. Not all globes are the same length and not all orbits are the same shape. In most patients who present for cataract surgery, axial length of the eyeball is measured with ultrasound (Fig. 30.10) to calculate the power of the intraocular lens. Normal globes have an axial length of 20–24 mm. Patients with high myopia have much longer axial lengths and extreme caution with needle blocks should be exercised in these patients.
ANAESTHESIA FOR SPECIFIC OPHTHALMIC PROCEDURES REQUIRING GENERAL ANAESTHESIA
Kumar, C.M., Dodds, C. Sub-Tenon’s anesthesia. Ophthalmol. Clin. North Am. 2006;19:209–219.
Kumar, C.M., Dowd, T.C. Complications of ophthalmic regional blocks: their treatment and prevention. Ophthalmologica. 2006;220:73–82.
Kumar C.M., Dodds C., Fanning G.L., eds. Ophthalmic anaesthesia. Netherlands: Swets and Zeitlinger, 2002.
Joint guidelines from the the Royal College of Anaesthetists and the Royal College of Ophthalmologists: 2012. http://www.rcoa.ac.uk/system/files/LA-Ophthalmic-surgery-2012.pdf. Accessed 24.06.13