CHAPTER 68 Open-globe injuries
Introduction
In 1996, Kuhn and associates developed a classification system intended to standardize and simplify the assessment and reporting of ocular trauma and they defined commonly used eye trauma terms1. They defined ‘rupture’ as a full-thickness wound of the eyewall (sclera and/or cornea) caused by a blunt object that results in a momentary increase in the intraocular pressure and an inside-out injury mechanism. They also clarified ‘laceration’ as a full-thickness wound of the eyewall caused by a sharp object with an outside-in mechanism. Penetrating injuries are those which are caused by a single laceration, and a perforating injury involves two full-thickness lacerations (entrance and exit) of the eyewall1.
In 1997, the Ocular Trauma Classification Group further refined this classification system for ocular trauma by providing a method of categorization during the initial examination or at the time of the primary surgical intervention (Table 68.1)2. The system classifies open-globe injuries according to the type of injury (based upon the mechanism), the grade of injury (defined by visual acuity in the injured eye at initial examination), the status of the pupil (defined as the presence or absence of a relative afferent pupillary defect in the injured eye), and the zone of the injury (based upon the anteroposterior extent of the injury). This chapter will address open-globe injuries in general, which are defined as any full-thickness wound in the cornea and/or sclera.
| Type |
From Pieramici DJ, Sternberg P Jr., Aaberg TM Sr., et al. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group. American Journal of Ophthalmology 1997;123(6):820–31.
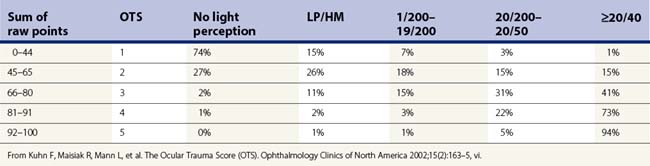
In 2002, Kuhn and associates established the ocular trauma score (OTS) in order to more accurately predict the functional outcome 6 months after a serious eye injury3. After analysis of over 2500 eye injuries, they established six variables with assigned raw points that can be summed and subsequently categorized into one of five groups (Tables 68.2 and 68.3).
Table 68.2 Calculation of the raw points for the Ocular Trauma Score
| Variable | Raw points |
|---|---|
| Initial vision | |
| NLP | 60 |
| LP/HM | 70 |
| 1/200–19/200 | 80 |
| 20/200–20/50 | 90 |
| ≥20/40 | 100 |
| Rupture | –23 |
| Endophthalmitis | –17 |
| Perforating injury | –14 |
| Retinal detachment | –11 |
| Afferent pupillary defect | –10 |
From Kuhn F, Maisiak R, Mann L, et al. The Ocular Trauma Score (OTS). Ophthalmology Clinics of North America 2002;15(2):163–5, vi.
Preoperative evaluation
Initial diagnosis
The diagnosis of open-globe injury should be considered in every patient who has sustained trauma to the eye or orbit. A complete history regarding the details leading up to and following the injury is crucial in the initial assessment. Injuries sustained while hammering metal on metal should be suspected to involve an intraocular foreign body until proven otherwise. Similarly, 6% of ocular paintball injuries were found to have a ruptured globe in a study that pooled the data from multiple case series4. Systemic, life-threatening conditions may occur in conjunction with an open-globe injury and should be addressed prior to any further evaluation.
Initial diagnostic examination
Signs that suggest open-globe injury
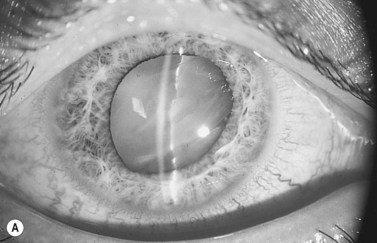
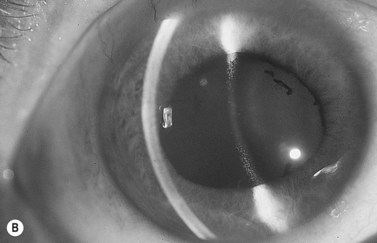
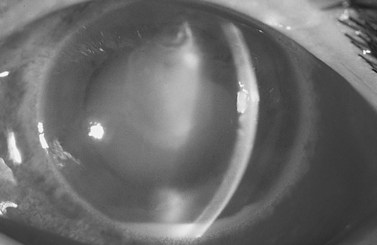
A complete ocular examination, including dilated fundus examination, should be performed when possible. Findings which suggest scleral rupture include a visual acuity of 20/400 or worse, marked chemosis, hyphema, an abnormally deep or shallow anterior chamber (Fig. 68.1), low intraocular pressure (IOP) or an IOP less than the non-traumatized eye, and a relative afferent pupillary defect5–7. The Seidel test may reveal an occult penetrating ocular injury. Finally, vitreous hemorrhage may obscure a retained intraocular foreign body.
Most frequent sites of rupture
In eyes which have not undergone prior surgery, the most frequent sites of rupture are at the limbus and parallel to the equator, and between the rectus muscle insertions and the equator8. Radially oriented ruptures under the rectus muscles are less common6. Eyes which have undergone previous surgery tend to rupture at the site of the prior surgical incision. A recent retrospective study of post-penetrating keratoplasty ruptured globes revealed that the average extent of wound dehiscence at the graft–host junction was 2.1 quadrants and involved the inferior quadrant more commonly than elsewhere9. Less frequent sites are in the cornea and at the posterior pole. Posterior ruptures, lying parallel to the equator, are usually found superiorly, in either the nasal or the temporal quadrant6.
Imaging studies
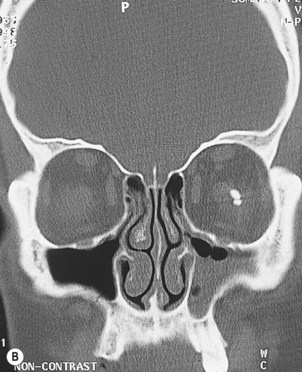
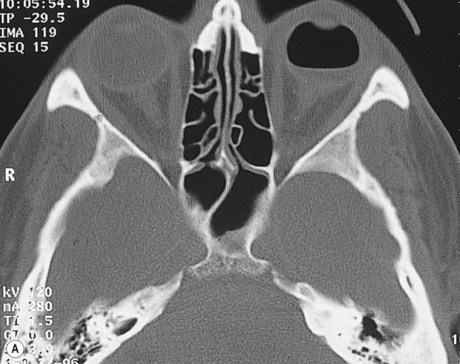
Computed tomography (CT) is the imaging technique of choice for initial assessment after ocular trauma, especially if a retained intraocular foreign body (IOFB) is suspected10,11. CT scan should be performed even if an IOFB can be visualized, since CT imaging may reveal additional IOFBs12. Thin-section axial and coronal CT images at 1.5 mm intervals are recommended for detecting IOFBs, fractures, and other soft-tissue injuries11 (Fig. 68.2). The disadvantage of CT is that non-metallic foreign bodies made of wood or plastic may be missed because they appear hypodense and may be confused with air13. Joseph et al. evaluated the use of CT scan alone for the diagnosis of open-globe injuries and found it had a sensitivity of 75% and specificity of 93%. They concluded that CT scan is not sensitive enough to be solely relied upon for diagnosis of open-globe injuries14.
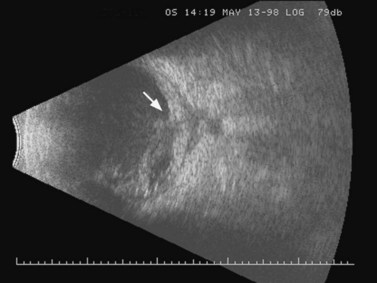
Contact B-scan ultrasonography (US) is also a useful test after ocular trauma because it can diagnose vitreous hemorrhage, retinal detachment, choroidal detachment, IOFB, and ruptured globe when clinical examination is inconclusive or the ocular media are opaque15–17 (Fig. 68.3). However, in one study, US detected less than 25% of open-globe injuries confirmed by exploration6. While CT is superior for detecting most foreign bodies, US can detect intraocular and intraorbital wooden foreign bodies13,18, is more useful for localizing foreign bodies relative to the ocular coats19, and is superior to CT in demonstrating ocular damage associated with an IOFB16.
Ultrasound biomicroscopy is a useful adjunct in evaluating eyes after trauma, especially in patients with media opacities, multiple traumatic injuries, or abnormal anatomy20. This high frequency ultrasound (50 MHz) reveals the appearance of a foreign body and surrounding tissues better than conventional low frequency ultrasound (10 Mhz)21. Like US, localization of foreign bodies near, or in, the eyewall is possible with ultrasound biomicroscopy.
Non-metallic objects that are difficult to visualize on CT or US can be visualized with magnetic resonance imaging (MRI)22. However, among the drawbacks of MRI is the potential for movement of ferromagnetic foreign bodies with deleterious effects23. Therefore, an initial CT is necessary to exclude the presence of an ocular metallic foreign body before performing an MRI24. Additionally, MRI is more expensive, not always readily available, and more sensitive to motion artifact than other forms of imaging. MRI is usually recommended if CT and US are negative, but suspicion of a retained foreign body remains high22.
Preoperative management
The patient is instructed to take nothing by mouth, in order to minimize the delay until general anesthesia can be safely initiated. A rigid shield (not a patch) should immediately be placed over the eye to minimize the possibility of extruding intraocular contents. Once the diagnosis of open-globe injury is made, further examination may be postponed until the time of surgical repair, unless management decisions hinge on the results of further examination. Topical medications are used only to facilitate the preoperative assessment, minimizing the risk of toxicity to intraocular contents. Anti-emetics are prescribed as needed to control vomiting and reduce the risk of expulsion of the intraocular contents. Tetanus immunity status should be updated. Broad-spectrum systemic antibiotic therapy should be instituted as soon as possible and continued for a total of 7–10 days to reduce the risk of post-traumatic endophthalmitis25. Because cultures from open-globe injuries reveal a high prevalence of Gram-positive bacillus species and polymicrobial infections containing Gram-negative species, antibiotic coverage must be broad26. A commonly used regimen includes vancomycin for Gram-positive coverage, including Bacillus species, and gentamicin or ceftazidime for Gram-negative coverage27. Colyer et al. recommend use of systemic 3rd or 4th generation fluoroquinolones, such as moxifloxacin or levofloxacin25. Orally administered moxifloxacin has been shown to achieve therapeutic levels within the aqueous and vitreous against the most common causative organisms in endophthalmitis in the non-inflamed eye28. If the suspicion of an open-globe injury proves to be incorrect after exploration, then the antibiotics may be discontinued.
Operative technique
Anesthesia considerations
All patients with a suspected or known open-globe injury are managed with general anesthesia, because local anesthesia, and its associated risks of retrobulbar hemorrhage and increased intraocular pressure, may cause further damage to the globe. However, some authors advocate the use of local anesthesia with sedation in the repair of an open-globe injury29. The goal of general anesthesia management involves intubation with full airway protection, while carefully avoiding further damage to the globe. An increase in intraocular pressure is still a concern with the use of general anesthesia because endotracheal intubation raises IOP, and succinylcholine, the muscle relaxant of choice in patients with a full stomach, also raises IOP30. There are several techniques described which minimize the effects of general anesthesia on intraocular pressure, and are discussed in further detail in Chapter 10. Children with open-globe injuries pose an additional risk, because struggling and crying associated with induction of general anesthesia may increase the intraocular pressure and the subsequent risk of extrusion of intraocular contents. In summary, the life of the patient is the primary concern, but every precaution should be undertaken to avoid further damage to the injured eye.
Exploration
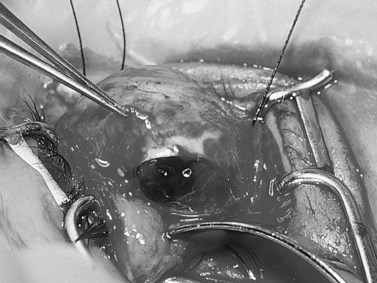
Scleral exploration is indicated if there is any doubt as to the structural integrity of the globe. The risks of this procedure are small and the benefits include producing a primary repair, minimizing extrusion of intraocular contents, and preventing secondary endophthalmitis. Scleral exploration is performed by making a 360° conjunctival peritomy, carefully hooking all four rectus muscles, and examining the sclera in all four quadrants and under the muscles (Fig. 68.4). Lid sutures, instead of a speculum, may be used to increase exposure without applying pressure to the globe. The finding of one rupture site should not preclude the search for others, because multiple scleral ruptures occasionally occur31.
Repair of open-globe injury
Primary closure of an open-globe injury is the focus of this chapter. For discussion of secondary repair, including anterior segment reconstruction and pars plana vitrectomy, the reader is referred to Chapter 67. Restoration of the structural integrity of the globe is the primary goal, regardless of the extent or type of wound. Visualization of anterior injuries is aided with the use of the operating microscope, while repair of posterior injuries may be enhanced with the use of surgical loupes.
Corneal wounds
Fine suture material, such as 10-0 nylon, should be used to suture corneal wounds and the knots should be buried, if possible. Deep, partial-thickness, interrupted corneal sutures should be placed with careful attention to proper tissue alignment. Suture bites of equal depth on opposing edges of the wound will prevent overriding of tissue. To ensure proper alignment, the first suture is placed to bisect the wound lengthwise and subsequent sutures are placed halfway between the suture and the end of the wound. Viscoelastic is extremely useful for reforming a flat anterior chamber or repositing prolapsed iris and is preferentially injected via a paracentesis tract, rather than through the corneal wound32. Uveal tissue which remains incarcerated in the wound can be freed by sweeping a cyclodialysis spatula parallel with the iris via a paracentesis port.
Corneoscleral and scleral wounds
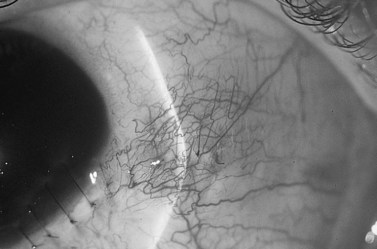
When repairing corneoscleral wounds, the initial suture should be an interrupted 9-0 nylon suture placed at the anatomic limbus to properly align the tissues and restore the normal anatomy. Following realignment of the limbus, the corneal wound should be repaired next (see above). Finally, the extent of the scleral wound should be visualized and then sutured (Fig. 68.5). Posterior scleral wounds may be under tension and may require 8-0 nylon or heavier suture. If the edges of the wound cannot be approximated to allow passage of the suture in one bite, then two separate passes can be made, with tension applied only after the suture is tied. Any prolapsed vitreous is excised using scissors held flush with the sclera or a vitrectomy cutter held at the external aspect of the wound. Traction on the vitreous, or blind insertion of the vitrectomy cutter into the wound, should be avoided. Prolapsed uvea is reposited if it does not appear necrotic or infected. If an extraocular muscle obscures the underlying scleral wound, it may be disinserted from its insertion site after it is secured with a double-armed locking suture. The muscle is sutured back to the original insertion site following closure of the scleral defect.
In some cases, prophylactic cryotherapy around the site of rupture and/or scleral buckling is considered in an attempt to prevent subsequent retinal detachment. The indications and technique for primary vitrectomy in the setting of open-globe injury are discussed in Chapter 67. In general, primary vitrectomy is reserved for situations where a non-magnetic foreign body, or magnetic foreign body not amenable to removal with a magnet, is encountered.
Lens management
Controversy exists regarding the proper management of concomitant open-globe injury and traumatic cataract33. The crystaline lens has been reported damaged in 9.7% and 32% of open-globe injuries occurring in assault-related and workplace-related injuries, respectively34,35. There are essentially three different management options, which include primary repair of the open-globe injury without primary removal of the lens, combined primary repair of the globe with primary lensectomy, and combined primary repair of the globe with primary lensectomy and intraocular lens implantation. Factors which must be considered in this decision include the size and location of the open-globe injury and the presence of lens-induced glaucoma and inflammation33. Because an exuberant fibrinous reaction can occur on the anterior lens capsule and masquerade as a cataract, conservative management is usually indicated. Even if the lens capsule has been violated, several cases have been described in which lens capsular disruption from an intraocular foreign body resulted in a visually insignificant lens opacity36. However, if the lens capsule is significantly disrupted and lens material is present in the anterior chamber in large quantities, then it is reasonable to perform a lensectomy at the time of primary repair.
Implantation of an intraocular lens is not recommended in the setting of an extensive perforating or contaminated injury, because the risk of endophthalmitis is increased37. However, in selected cases, intraocular lens implantation at the time of lensectomy and primary repair of a corneal laceration may result in an excellent anatomic and visual outcome38–41.
IOFB management
Intraocular foreign bodies are not only potentially damaging to intraocular structures, but they may also increase the risk of secondary endophthalmitis42,43. Although several studies have reported that the incidence of endophthalmitis is higher in eyes with IOFBs than in open-globe injuries without IOFBs, only two studies have been able to demonstrate this association by multivariate analysis44,45. Zhang et al., in the largest retrospective analysis of open-globe injuries to date, which included 4795 eyes, found that the presence of an IOFB was not an independent risk factor for endophthalmitis46. They did find that a laceration injury (defined by the Ocular Trauma Classification Group as a penetrating injury, perforating injury, or as an IOFB)2 was an independent risk factor for infection, and thus, these authors proposed that the nature of the injury itself, the intraocular intrusion of a foreign object, rather than the retained IOFB, may be the underlying risk factor for post-traumatic endophthalmitis46. Siderosis is also a possible complication of iron-containing foreign bodies.
Although the traditional recommendation has been that IOFB removal be prompt44,47, there have been two studies that have suggested that immediate IOFB removal may not be as important as previously thought in the prevention of endophthalmitis. Colyer and associates reported no cases of endophthalmitis in 79 eyes that had prompt primary open-globe wound closure, but had delayed IOFB removal of 2–661 days (mean 37 days) after injuries sustained in Operations Iraqi and Enduring Freedom25. Greven et al. reported no cases of endophthalmitis in 59 consecutive eyes that underwent IOFB removal, 20 of which were delayed over 24 hours48.
A delay in IOFB removal allows a capsule to surround the foreign body, which was a major concern in the previtrectomy era, when the capsule could render the magnet powerless to remove the IOFB12. The magnetic removal of the foreign body is a technique that has been used for more than a century49 and may be possible with ferromagnetic IOFBs. Currently, pars plana vitrectomy with forceps removal of the IOFB in the posterior segment is most common approach employed by retinal surgeons48, and it is indicated for non-magnetic IOFBs or those not amenable to magnetic removal (Fig. 68.6).
Postoperative management
Broad-spectrum intravenous antibiotic therapy is continued to complete a 72-hour course of treatment and some advocate for systemic coverage for 10 days or longer25. Treatment with topical antibiotic, cycloplegic, and corticosteroid drops is initiated following the primary repair. Oral or intramuscular analgesic medications are prescribed as needed. The patient is discharged on the third postoperative day.
In general, vitrectomy after open-globe repair is indicated in the setting of traumatic endophthalmitis, tractional retinal detachment, IOFBs, and possibly vitreous hemorrhage50. The timing of vitrectomy following primary repair of open-globe injuries is controversial50,51. There are data to suggest that eyes undergoing early pars plana vitrectomy (within 14 days) have a better visual outcome than those that undergo later vitrectomy6,47,52,53. Some authors have ceased using temporary keratoprostheses for vitrectomy, given the high rate of corneal graft failure; instead vitrectomy is performed using wide-angle viewing systems after 10–14 days, once the cornea has cleared sufficiently54.
Complications
Endophthalmitis
Endophthalmitis occurring as a complication of an open-globe injury can cause further devastation to an already traumatized eye (Fig. 68.7). Bacillus species, seen more commonly in post-traumatic endophthalmitis, can be particularly destructive42,55. Estimates of the rate of post-traumatic endophthalmitis range from 0 to 17% of open-globe injuries42,56–58. Factors which appear to increase the risk of endophthalmitis in open-globe injuries include the presence of an IOFB42, delay in removal of the IOFB beyond 24 hours44, disruption of the crystaline lens57, age 50 years or older44, and sustaining ocular trauma in a rural setting56. In the largest study of open-globe injuries to date, the following were found to be independent risk factors for post-traumatic endophthalmitis: laceration (including penetration, IOFB, and perforation and excluding rupture) and primary repair greater than 24 hours after injury; tissue prolapse and self-sealing of wounds were found to be protective.
Prevention of post-traumatic endophthalmitis involves early closure of the globe and removal of any IOFB, if applicable. Intravenous antibiotic therapy is instituted as soon as possible. Subconjunctival antibiotics are injected following primary repair and topical antibiotics are used in the postoperative period. Mieler and associates found positive cultures in seven of 27 (26%) eyes with retained IOFBs, but none of the eyes developed endophthalmitis; however, three of the seven eyes did receive prophylactic intravitreal antibiotics at the time of surgery47. In another study which examined culture results in open-globe injuries, routine intraoperative cultures were positive in almost 30% of patients; however, they did not help to identify eyes at increased risk for developing endophthalmitis or affect management decisions in eyes without clinical signs of endophthalmitis59. Controversy exists regarding the use of intravitreal antibiotics as prophylaxis; however, they may be considered in high risk cases, such as those with retinal periphlebitis, purulence around a foreign body, delayed primary closure, or soil-contaminated injury51,56,60. In those cases, the most recent antibiotic recommendations include vancomycin and ceftazidime60. Soheilian and associates found a significant benefit from intravitreal antibiotic injection (vs. placebo) in open-globe injuries with an IOFB in their prospective, randomized study45.
Successful treatment of post-traumatic endophthalmitis hinges on early diagnosis and aggressive treatment. Once the diagnosis is suspected, pars plana vitrectomy and injection of intravitreal broad-spectrum antibiotics, with coverage against Bacillus species and Gram-negative organisms, should be performed as soon as possible. Although the prognosis is better when the offending organism is less virulent42,57, this aggressive treatment regimen has resulted in preservation of useful visual acuity in several eyes infected with Bacillus species61. Coverage against fungal organisms should also be considered in the appropriate clinical setting26,55.
Prognosis
Although the prognosis for full recovery of vision is poor with major ocular injuries, the potential for preservation of useful vision justifies primary repair in most situations. Despite significant advances in vitreoretinal surgical techniques and a slight improvement in visual outcomes of eyes with open-globe injuries over the past 30 years, the percentage of eyes that achieve a visual acuity of 5/200 or better is still only hovering around 56–60%62–64.
Predictors of good visual outcome following primary repair of an open-globe injury include visual acuity of 20/800 or better on initial examination (some authors have found 20/200 to be more predictive), a laceration limited to the cornea, absence of an expelled or subluxed lens, lacerations located anterior to the rectus muscle insertions, and a rupture length of less than 11 millimeters6,65,66.
Enucleation
Primary enucleation (performed at the time of the initial surgical procedure) should be reserved for those cases in which the globe is considered irreparable, or an expulsive choroidal hemorrhage with loss of the intraocular contents has occurred. Savar and associates reported that primary enucleation after open-globe injury was performed on 11 of 660 patients (1.7%) in an urban setting67. Weichel and associates reported 31 primary enucleations performed out of 198 open-globe injuries (15.7%) in a combat setting58. Primary repair allows further evaluation and assessment of visual potential and preserves the possibility for secondary enucleation in the postoperative period. Secondary enucleation is considered if the eye no longer has light perception and the visual prognosis is hopeless. It is most commonly performed within a 2-week period following the open-globe injury in order to avoid the potential complication of sympathetic ophthalmia, which has been reported to occur after trauma at a rate of 0.28–3.1% during the 20th century, but the rate has been closer to 0–0.9% more recently67.
Approximately 70% of eyes that sustain open-globe injuries resulting in poor visual potential and are not treated with enucleation can be expected to become phthisical over a 5-year period. Enucleation will be required in about 34% of these eyes, most commonly to ameliorate pain68.
1 Kuhn F, Morris R, Witherspoon CD, et al. A standardized classification of ocular trauma. Ophthalmology. 1996;103(2):240-243.
2 Pieramici DJ, Sternberg PJr, Aaberg TMSr, et al. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group [see comments]. Am J Ophthalmol. 1997;123(6):820-831.
3 Kuhn F, Maisiak R, Mann L, et al. The Ocular Trauma Score (OTS). Ophthalmol Clin North Am. 2002;15(2):163-165. vi
4 Pahk PJ, Adelman RA. Ocular trauma resulting from paintball injury. Graefe’s Arch Clin Exp Ophthalmo. 2009;247(4):469-475.
5 Kylstra JA, Lamkin JC, Runyan DK. Clinical predictors of scleral rupture after blunt ocular trauma. Am J Ophthalmol. 1993;115(4):530-535.
6 Russell SR, Olsen KR, Folk JC. Predictors of scleral rupture and the role of vitrectomy in severe blunt ocular trauma [published erratum appears in Am J Ophthalmol 1988;106(5):640]. Am J Ophthalmol. 1988;105(3):253-257.
7 Werner MS, Dana MR, Viana MA, et al. Predictors of occult scleral rupture. Ophthalmology. 1994;101(12):1941-1944.
8 Benson WE, Jeffers JB. Blunt trauma. In: Tasman W, Jaeger EA, editors. Duane’s Clinical Ophthalmology. Philadelphia: Lippincott-Raven, 1997. v. 3
9 Kawashima M, Kawakita T, Shimmura S, et al. Characteristics of traumatic globe rupture after keratoplasty. Ophthalmology. 2009;116(11):2072-2076.
10 Lindahl S. Computed tomography of intraorbital foreign bodies. Acta Radiol. 1987;28(3):235-240.
11 Lustrin ES, Brown JH, Novelline R, et al. Radiologic assessment of trauma and foreign bodies of the eye and orbit. Neuroimaging Clin North Am. 1996;6(1):219-237.
12 Woodcock MGL, Scott RAH, Huntbach J, et al. Mass and shape as factors in intraocular foreign body injuries. Ophthalmology. 2006;113(12):2262-2269.
13 Topilow HW, Ackerman AL, Zimmerman RD. Limitations of computerized tomography in the localization of intraocular foreign bodies. Ophthalmology. 1984;91(9):1086-1091.
14 Joseph DP, Pieramici DJ, Beauchamp NJ. Computed tomography in the diagnosis and prognosis of open-globe injuries. Ophthalmology. 2000;107(10):1899-1906.
15 Das T, Namperumalsamy P. Ultrasonography in ocular trauma. Indian J Ophthalmol. 1987;35(3):121-125.
16 McNicholas MM, Brophy DP, Power WJ, et al. Ocular trauma: evaluation with US. Radiology. 1995;195(2):423-427.
17 Rubsamen PE, Cousins SW, Winward KE, et al. Diagnostic ultrasound and pars plana vitrectomy in penetrating ocular trauma. Ophthalmology. 1994;101(5):809-814.
18 Coleman DJ. Reliability of ocular and orbital diagnosis with B-scan ultrasound. 2. Orbital diagnosis. Am J Ophthalmol. 1972;74(4):704-718.
19 Coleman D, Rondeau M. Diagnostic imaging of ocular and orbital trauma. In: Shingleton B, Hersh P, Kenyon K, editors. Eye Trauma. St. Louis: Mosby-Year Book, 1991.
20 Deramo VA, Shah GK, Baumal CR, et al. Ultrasound biomicroscopy as a tool for detecting and localizing occult foreign bodies after ocular trauma. Ophthalmology. 1999;106(2):301-305.
21 Nouby-Mahmoud G, Silverman RH, Coleman DJ. Using high-frequency ultrasound to characterize intraocular foreign bodies. Ophthal Surg. 1993;24(2):94-99.
22 Green BF, Kraft SP, Carter KD, et al. Intraorbital wood. Detection by magnetic resonance imaging [see comments]. Ophthalmology. 1990;97(5):608-611.
23 Kelly WM, Paglen PG, Pearson JA, et al. Ferromagnetism of intraocular foreign body causes unilateral blindness after MR study. AJNR: Am J Neuroradiol. 1986;7(2):243-245.
24 Otto PM, Otto RA, Virapongse C, et al. Screening test for detection of metallic foreign objects in the orbit before magnetic resonance imaging. Invest Radiol. 1992;27(4):308-311.
25 Colyer M, Weber E, Weichel E, et al. Delayed intraocular foreign body removal without endophthalmitis during Operations Iraqi Freedom and Enduring Freedom. Ophthalmology. 2007;114(8):1439-1447.
26 Kunimoto DY, Das T, Sharma S, et al. Microbiologic spectrum and susceptibility of isolates: part II. Posttraumatic endophthalmitis. Endophthalmitis Research Group. Am J Ophthalmol. 1999;128(2):242-244.
27 Navon SE. Management of the ruptured globe. Internat Ophthalmol Clin. 1995;35(1):71-91.
28 Hariprasad SM, Shah GK, Mieler WF, et al. Vitreous and aqueous penetration of orally administered moxifloxacin in humans. Arch Ophthalmol. 2006;124(2):178-182.
29 Scott IU, Mccabe CM, Flynn HW, et al. Local anesthesia with intravenous sedation for surgical repair of selected open globe injuries. Am J Ophthalmol. 2002;134(5):707-711.
30 Libonati MM, Leahy JJ, Ellison N. The use of succinylcholine in open eye surgery. Anesthesiology. 1985;62(5):637-640.
31 Joondeph BC, Young TL, Saran BR. Multiple scleral ruptures after blunt ocular trauma. Am J Ophthalmol. 1989;108(6):744.
32 Colby K. Management of open globe injuries. Internat Ophthalmol Clin. 1999;39(1):59-69.
33 Pieramici DJ. Primary intraocular lens implantation for lens trauma. Ophthalmology. 1999;106(4):643-644.
34 Dannenberg AL, Parver LM, Brechner RJ, et al. Penetration eye injuries in the workplace. The National Eye Trauma System Registry. Arch Ophthalmol. 1992;110(6):843-848.
35 Dannenberg AL, Parver LM, Fowler CJ. Penetrating eye injuries related to assault. The National Eye Trauma System Registry. Arch Ophthalmol. 1992;110(6):849-852.
36 Pieramici DJ, Capone AJr, Rubsamen PE, et al. Lens preservation after intraocular foreign body injuries. Ophthalmology. 1996;103(10):1563-1567.
37 Koster HR, Kenyon KR. Complications of surgery associated with ocular trauma. Internat Ophthalmol Clin. 1992;32(4):157-178.
38 Rubsamen PE, Irvin WD, McCuen BWn, et al. Primary intraocular lens implantation in the setting of penetrating ocular trauma. Ophthalmology. 1995;102(1):101-107.
39 Muga R, Maul E. The management of lens damage in perforating corneal lacerations. Br J Ophthalmol. 1978;62(11):784-787.
40 Moisseiev J, Segev F, Harizman N, et al. Primary cataract extraction and intraocular lens implantation in penetrating ocular trauma. Ophthalmology. 2001;108(6):1099-1103.
41 Blum M, Tetz MR, Greiner C, et al. Treatment of traumatic cataracts. J Cataract Refract Surg. 1996;22(3):342-346.
42 Brinton GS, Topping TM, Hyndiuk RA, et al. Posttraumatic endophthalmitis. Arch Ophthalmol. 1984;102(4):547-550.
43 Coleman DJ, Lucas BC, Rondeau MJ, et al. Management of intraocular foreign bodies. Ophthalmology. 1987;94(12):1647-1653.
44 Thompson JT, Parver LM, Enger CL, et al. Infectious endophthalmitis after penetrating injuries with retained intraocular foreign bodies. National Eye Trauma System. Ophthalmology. 1993;100(10):1468-1474.
45 Soheilian M, Rafati N, Mohebbi M-R, et al. Prophylaxis of acute posttraumatic bacterial endophthalmitis: a multicenter, randomized clinical trial of intraocular antibiotic injection, report 2. Arch Ophthalmol. 2007;125(4):460-465.
46 Zhang Y, Zhang M, Jiang C, et al. Endophthalmitis following open globe injury. Br J Ophthalmol. 2010 Jan;94(1):111-114.
47 Mieler WF, Ellis MK, Williams DF, et al. Retained intraocular foreign bodies and endophthalmitis. Ophthalmology. 1990;97(11):1532-1538.
48 Greven CM, Engelbrecht NE, Slusher MM, et al. Intraocular foreign bodies: management, prognostic factors, and visual outcomes. Ophthalmology. 2000;107(3):608-612.
49 Hildebrand H. Sixty-six magnet operations with successful extraction of particles of iron from the inferior of the eye in fifty-three cases. Arch Ophthalmol. 1996;114(6):762-763.
50 Mieler WF, Mittra RA. The role and timing of pars plana vitrectomy in penetrating ocular trauma. Arch Ophthalmol. 1997;115(9):1191-1192.
51 Cebulla CM, Flynn HW. Endophthalmitis after open globe injuries. Am J Ophthalmol. 2009;147(4):567-568.
52 Brinton GS, Aaberg TM, Reeser FH, et al. Surgical results in ocular trauma involving the posterior segment. Am J Ophthalmol. 1982;93(3):271-278.
53 Coleman DJ. Early vitrectomy in the management of the severely traumatized eye. Am J Ophthalmol. 1982;93(5):543-551.
54 Colyer MH, Chun DW, Bower KS, et al. Perforating globe injuries during operation Iraqi Freedom. Ophthalmology. 2008;115(11):2087-2093.
55 Affeldt JC, Flynn HWJr, Forster RK, et al. Microbial endophthalmitis resulting from ocular trauma. Ophthalmology. 1987;94(4):407-413.
56 Boldt HC, Pulido JS, Blodi CF, et al. Rural endophthalmitis. Ophthalmology. 1989;96(12):1722-1726.
57 Thompson WS, Rubsamen PE, Flynn HWJr, et al. Endophthalmitis after penetrating trauma. Risk factors and visual acuity outcomes. Ophthalmology. 1995;102(11):1696-1701.
58 Weichel ED, Colyer MH, Ludlow SE, et al. Combat ocular trauma visual outcomes during operations iraqi and enduring freedom. Ophthalmology. 2008;115(12):2235-2245.
59 Rubsamen PE, Cousins SW, Martinez JA. Impact of cultures on management decisions following surgical repair of penetrating ocular trauma. Ophthal Surg Lasers. 1997;28(1):43-49.
60 Lieb DF, Scott IU, Flynn HW, et al. Open globe injuries with positive intraocular cultures: factors influencing final visual acuity outcomes. Ophthalmology. 2003;110(8):1560-1566.
61 Foster RE, Martinez JA, Murray TG, et al. Useful visual outcomes after treatment of Bacillus cereus endophthalmitis. Ophthalmology. 1996;103(3):390-397.
62 Pieramici DJ, MacCumber MW, Humayun MU, et al. Open-globe injury. Update on types of injuries and visual results. Ophthalmology. 1996;103(11):1798-1803.
63 Ramsay RC, Cantrill HL, Knobloch WH. Vitrectomy for double penetrating ocular injuries. Am J Ophthalmol. 1985;100(4):586-589.
64 Man C, Steel D. Visual outcome after open globe injury: a comparison of two prognostic models – the Ocular Trauma Score and the Classification and Regression Tree. Eye (Lond) 2009.
65 Sternberg PJr, de Juan EJr, Michels RG, et al. Multivariate analysis of prognostic factors in penetrating ocular injuries. Am J Ophthalmol. 1984;98(4):467-472.
66 Ehlers JP, Kunimoto DY, Ittoop S, et al. Metallic intraocular foreign bodies: characteristics, interventions, and prognostic factors for visual outcome and globe survival. Am J Ophthalmol. 2008;146(3):427-433.
67 Savar A, Andreoli MT, Kloek CE, et al. Enucleation for open globe injury. Am J Ophthalmol. 2009;147(4):595-600.e1.
68 Brackup AB, Carter KD, Nerad JA, et al. Long-term follow-up of severely injured eyes following globe rupture. Ophthalm Plastic Reconstruct Surg. 1991;7(3):194-197.