Disorders of the inert structures
Ligamentous instability
Ligamentous instability
If the history indicates that there is possibly instability, an examination to detect the exact location and degree of this is performed. It is important to make this supplementary examination only when symptoms and signs found in the routine clinical assessment indicate ligamentous instability to be the cause of disability. Indeed, it is important to realize that not every lengthened ligament leads to problems.1 If the athlete’s muscles are strong enough to provide dynamic stability, a slightly unstable knee will not cause trouble. Conversely, it is quite possible that an athlete with slight laxity of one or more ligaments has a chronic painful lesion as well. If the diagnosis of the latter is missed because the routine functional examination is not performed, it may well be that the patient is sent for surgery, which will solve the slight instability but does not cure the main problem.
Types of instability
Knee instability is the result of loss of static and dynamic function. Stability depends on the tautness of the ligaments, congruency of joint surfaces, effectiveness of the menisci and the well-balanced action of all musculotendinous units acting across the knee joint. Of these structures, muscles and tendons play a central role in joint stabilization. They are said to be the ‘first defenders’ in distortion and loading situations.2
Degree of instability
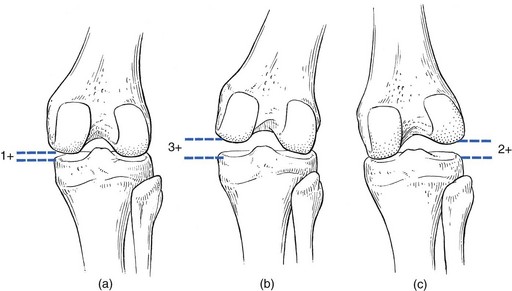
The degree of instability is demonstrated during stress tests and can be graded on the following scale (Fig. 1):
Classification of instability
Instability may be classified as straight or rotatory.
Straight instability
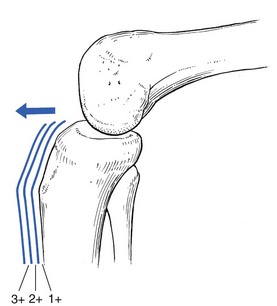
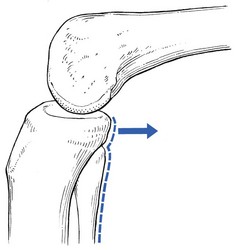
This is defined as an increased range of angular movement in the frontal plane, i.e. valgus/abduction or varus/adduction movement (Fig. 2), or an increased range of gliding movement in the sagittal plane, i.e. the simultaneous forward or backward gliding movement of the tibial condyles in relation to the femoral condyles (Fig. 3).
Rotatory instability
This implies increased rotation movement of the tibia on the femur. The posterior cruciate ligament, located in the centre of the joint, is the fundamental stabilizer and is the axis of the joint, both in flexion–extension and in rotation. Consequently, this ligament is always intact in rotatory instabilities; from the moment the ligament is completely torn, there is no longer a centre of rotation and any kind of straight instability can result.3,4
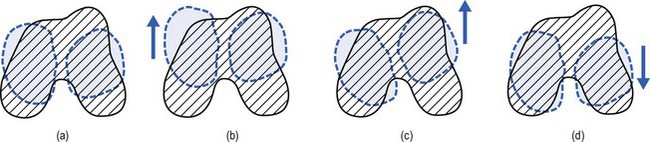
There are three types of rotatory instability:
• Anteromedial rotatory instability: there is an abnormal forward gliding movement of the medial tibial plateau with respect to the medial femoral condyle, while the lateral tibial plateau retains a relatively normal relationship with the lateral femoral condyle (Fig. 4b).
• Anterolateral rotatory instability: there is an abnormal forward gliding movement of the lateral tibial plateau with respect to the lateral femoral condyle, while the medial tibial plateau retains a relatively normal relationship with the medial femoral condyle (Fig. 4c).
• Posterolateral rotatory instability: there is an abnormal backward gliding movement of the lateral tibial plateau with respect to the lateral femoral condyle. Again, as in anterolateral rotatory instability, the medial tibial plateau remains in normal contact with the corresponding femoral condyle (Fig. 4d).
Functional examination
Tests
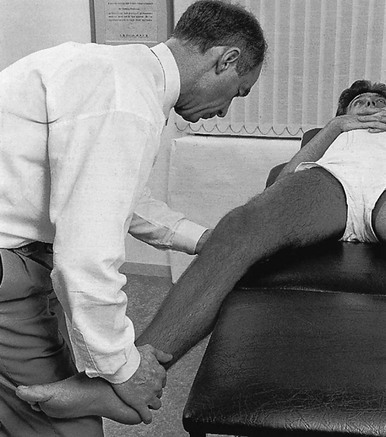
Passive abduction or valgus stress test in 30° of flexion
The patient is placed supine on the couch, the head resting on a pillow to enable observation of the examiner without active raising of the head (which often causes tightening of the hamstrings). The thigh rests on the couch and the lower leg hangs over the side, with the knee in 30° of flexion. One hand is placed about the lateral aspect of the knee, the other grasps the lower leg at the ankle (Fig. 5). Then abduction stress is applied gently and repeatedly, gradually increasing up to the point of pain. The degree of movement and the end-feel are estimated.
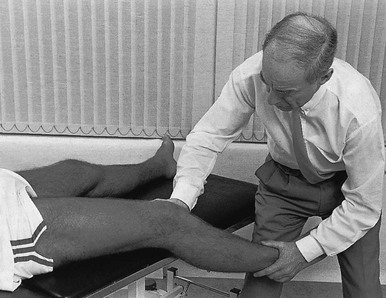
Passive adduction or varus stress test in 30° of flexion
This test is performed in the same position as the previous one, but the hands are changed; so one hand is placed about the medial aspect of the knee while the other grasps the lower leg at the outer side of the ankle (Fig. 6). The degree of movement and end-feel are estimated.
Lachman test
The test is performed with the patient supine and the knee in 20–30° of flexion. The distal femur is grasped from the lateral side to obtain control just above the lateral femoral condyle. The examiner uses the opposite hand to displace the proximal tibia directly anteriorly (Fig. 7).
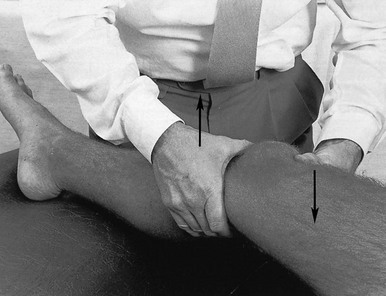
Fig 7 Lachman test.
In acute rupture of the anterior cruciate ligament this test is preferred to the anterior drawer test in the 90° flexed position because muscle defence by the hamstrings may prevent the forward movement of the tibia and give rise to a false-negative result.5 Liljedahl et al6 found only 3 of 35 patients to have a positive anterior drawer test in 90° of flexion, whereas with anaesthesia 31 and on arthrography 29 were positive.
Anterior drawer test in external and internal rotation
The test is first performed with the lower leg and foot externally rotated beyond the neutral position and as far as is comfortably possible, then internally rotated (Fig. 8).
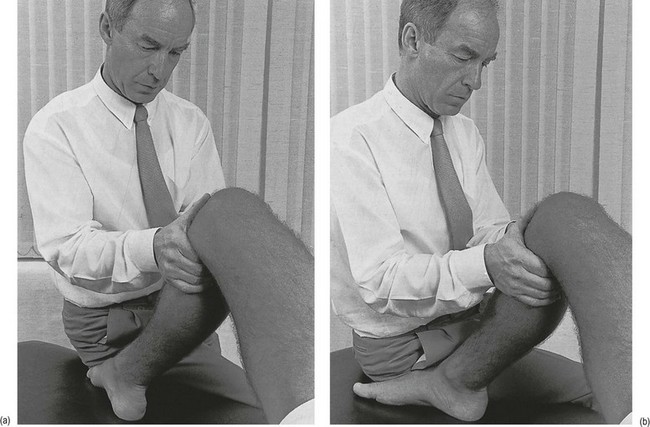
Prone rotation test7
Sometimes doubt remains as to whether the range of rotation has been increased. A decisive assessment can be made with the patient prone and the knees flexed to a right angle (Fig. 9). The movement of external or internal rotation is performed bilaterally and the range of movement is assessed by the twisted position of the feet.
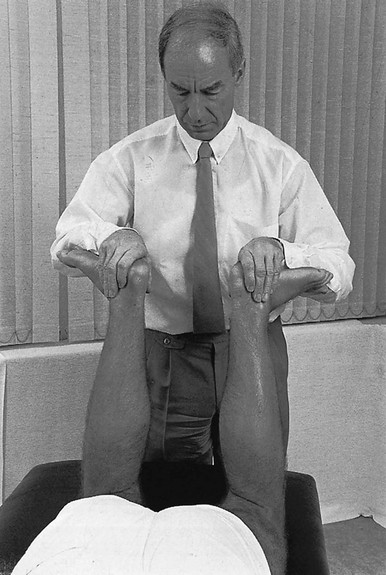
Fig 9 Prone rotation test.
Posterior drawer test
The patient is in supine position with the hip flexed to 45° and the knee to 90°. The foot is flat on the couch, in neutral position. The heels of both hands are placed anteriorly against the proximal part of the tibia (Fig. 10). Both thumbs at the anterior border of the joint can estimate the range of movement. The proximal part of the tibia is then pushed backwards repeatedly, first gently then with a strong jerk.
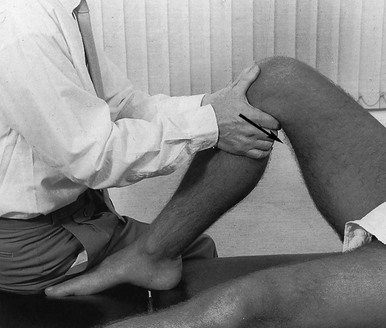
Fig 10 Posterior drawer test.
The posterior drawer test, which includes palpation of the tibia–femur step-off, was recently demonstrated to be the most sensitive and specific clinical test for posterior cruciate ligament deficiency (accuracy 96% with a 90% sensitivity and a 99% specificity).8
‘Jerk’ test and pivot-shift test
The patient lies supine, the hip flexed to about 45°, the knee to 90°. The examiner supports the patient’s leg, with one hand at the foot, the other at the proximal end of tibia and fibula. The hand at the foot rotates the tibia slightly internally while the other hand exerts a mild valgus stress at the knee (Fig. 11). Extreme internal rotation may dampen a shift significantly. Maintaining slight internal rotation and mild valgus stress, the examiner gradually extends the knee.
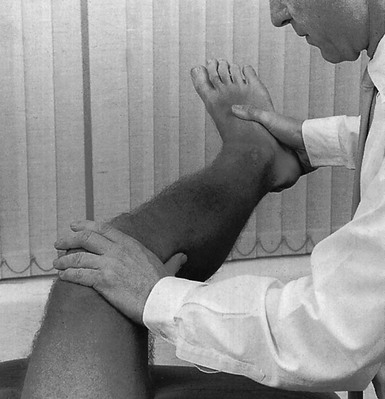
Fig 11 The ‘jerk’ test.
The test demonstrates an anterolateral rotatory instability because of a tear in the middle third of the lateral capsular ligaments. Frequently, the anterior cruciate ligament and/or menisci are also ruptured and increase the instability.9
Bach et al10 found that the degree of pivot shift, probably because of the role of the iliotibial band, strongly correlates with the position of the hip and knee joint. They advised 30° of hip abduction and 20° of tibial external rotation as the position in which instability is most clearly demonstrated.
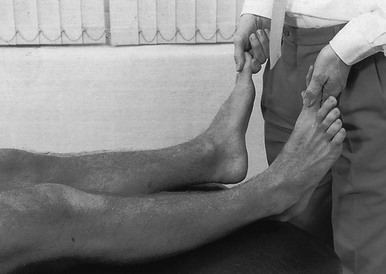
External rotation–recurvatum test
The patient lies supine on the couch. Both legs are lifted simultaneously by grasping the big toes (Fig. 12). The amount of external rotation of the proximal end of the tibia and the degree of recurvatum are observed. In a positive test, unilateral excess of external rotation and recurvatum is obvious, which is seen as increased tibia vara.
Clinical tests for knee instability are summarized in Table 1.
Table 1
Summary of clinical tests for instability
| Type of instability | Structures probably ruptured | Diagnostic test |
| Straight valgus | Capsuloligamentous structures of medial and posteromedial compartment, and posterior cruciate ligament | Abduction stress test in full extension |
| Straight varus | Lateral compartment ligaments and posterior cruciate ligament | Adduction stress test in full extension |
| Straight anterior | Middle third of medial and lateral compartment ligaments, and anterior cruciate ligament | Anterior drawer test Lachman test |
| Straight posterior | Posterior cruciate ligament and arcuate complex | Posterior drawer test |
| Rotatory anteromedial | Medial and posteromedial compartment ligaments, and anterior cruciate ligament | Anterior drawer test from mid-position and in internal rotation Abduction in 30° flexion Lachman test |
| Rotatory anterolateral | Middle third of lateral compartment ligaments, and anterior cruciate ligament | Anterior drawer test from mid-position Adduction in 30° flexion ‘Jerk’ test Pivot-shift test |
| Rotatory posterolateral | Arcuate complex | External rotation–recurvatum test Posterior drawer test from mid-position and in external rotation Adduction in 30° flexion |
Treatment
The best chance of success in treating a knee affected by ligamentous instability is within days of the original injury.11 Management can be non-surgical or by surgical repair. Which is chosen depends on the structure(s) at fault, the degree of rupture and the extent of the lesion.
Conservative treatment
In general, conservative treatment is indicated in all grade I and II sprains and in isolated grade III sprains of the medial collateral ligament. Acute complete tears of the anterior cruciate ligament, with an absent (0) or mild graded (1+) pivot-shift test, show excellent or good results in half of the cases.12
The results of conservative treatment of isolated grade III sprains of the lateral ligament compartment are generally poor and not acceptable.13
Surgery
Surgical treatment of knee ligament injuries, particularly of the anterior cruciate ligament, is still controversial because the complex functional role of these ligaments makes them difficult to reconstruct effectively.14 Given that reconstruction is performed using high-strength bone–ligament–bone autogenous graft, placed isometrically and securely fixed internally, failure rates after 2 years’ follow-up have decreased to about 30%.15
Conservative treatment in acute instability
Medial collateral ligament
Isolated acute grade III lesions of the medial collateral ligament seldom result in lasting instability. Successful conservative treatment of these lesions has been reported, with only a very small number of patients requiring subsequent reconstruction.16–20 However, this applies only to isolated injuries in which, for example, valgus stability in full extension is normal. The key to success in non-surgical management of complete tears of the medial collateral ligament is to exclude those with concurrent damage to the anterior cruciate ligament or menisci.18,20,21,22
Therapy must also include a structural rehabilitation programme with early protected motion, followed by progressive strengthening. A small residual amount of medial laxity does not appear to have any influence on the ability to return to competitive athletics.22
When surgical and non-surgical treatment is compared in isolated acute grade III lesions of the medial collateral ligament, similar results are obtained. However, non-surgically treated patients are rehabilitated in significantly less time.18 In combined injuries, it has been shown that the non-surgical management is successful only in 15%.
Rehabilitation in non-operated, acute complete tears22
In the first 2 weeks the knee is partially immobilized in a rehabilitative brace that prevents the joint from moving beyond the painful range and protects against hyperextension, excessive lateral rotation and valgus strain. In order to maintain mobility while healing, Cyriax advocates moving the ligament by deep transverse friction to and fro over the adjacent bone in imitation of its normal behaviour.23 The first day, 1 minute’s friction thus suffices, in that no unwanted adhesions have yet formed. Friction is followed by passive flexion and extension movements, within the limits of pain. This treatment is repeated daily. Within a week, tenderness is declining and friction is performed for an increasing time, for up to 15 minutes, on alternate days during the second week (see p. 701).
The average time from injury to return to full activity and competitive sports is about 9 weeks.
Anterior cruciate ligament
In acute complete rupture of the anterior cruciate ligament, surgical repair is the treatment of choice,24–26 although secondary repair operations can still be undertaken.
Buckley et al,27 in their study of conservatively treated partial anterior cruciate ligament tears, found that most patients developed a symptomatic knee but the majority did not have a sufficiently significant functional disability to warrant reconstructive surgery. Furthermore, they found that knee function following a partial tear did not appear to deteriorate with time (49 months after injury).
Posterior cruciate ligament
Recent studies have shown that conservative management is also acceptable in isolated complete ruptures of the posterior cruciate ligament. Good results are obtainable even in athletes who wish to return to competitive sport.28–32
In contrast, as found by Fowler and Messieh,31 surgical techniques of posterior cruciate ligament repair and reconstructions are generally difficult and the long-term results are unpredictable.
Lateral ligament compartment
The long-term results of non-surgically treated grade II sprains of the lateral ligament compartment of the knee are reported as good and acceptable; however, in grade III sprains the results are mostly poor and unacceptable, resulting in an unstable knee with severe symptoms and post-traumatic osteoarthritis.13 On examination in 30° of flexion, these grade III sprains showed a severe (3+) adduction instability. In full extension there is still some adduction instability, graded as mild (1+) or moderate (2+). Kannus13 emphasizes that in grade III sprains the anterior cruciate ligament is often injured as well, and the damage to it may be missed by clinical methods at the initial examination. Such ligamentous laxity seems too severe to be fully compensated for by muscle strength, i.e. dynamic stability.
Conservative treatment in chronic instability
In chronic grade III instability it is impossible to improve upon the loss of proprioception within the joint without surgical repair. Such repair is thereby limited to young and well-motivated patients with no radiological evidence of degenerative disease.33
Late examples of posterior cruciate and isolated lateral ligament instability cannot be repaired with confidence.11 Thus early detection and repair are most important.
Rehabilitation management after surgical repair
Rehabilitation takes at least 6 months. It should be instituted carefully, because revascularization and structural conversion of any transplanted tissue is a very slow process. The final result is obtained about 1 year after the operation.34–36
The rehabilitation programme can be divided into four phases:37
Assisted ambulatory phase
During the last decade a trend has developed to replace the period of immobilization after surgical repair by early mobilization in order to decrease the risk of contracture building up and to prevent detrimental effects on cartilage. For example, after complete rupture of the anterior cruciate ligament, the use of a high-strength bone–ligament–bone autogenous graft, placed isometrically and securely internally fixed, made it possible to commence joint motion, muscle re-education and, with the protection of a knee orthosis, even weight bearing up to 50% from the first week.38–42
A study of the results of accelerated programmes of rehabilitation after anterior cruciate ligament reconstruction indicated not only the need for individualized, evaluation-based rehabilitation, but also that caution should be used when introducing high loads or repetitive exercises within the first few months after surgery.43
For this reason postoperative clinical evaluation of graft failure, excessive pain and effusion must be strictly and regularly performed until termination of the rehabilitation. This includes joint arthrometer tests and stress diagnosis after the first week of rehabilitation and at every second week during the first 6 weeks, so as to have an accurate and objective evaluation of anterior displacement before progression to a more strenuous phase of rehabilitation.37
Excessive synovial fluid may be another sign that therapy has been too aggressive. It inhibits not only quadriceps contraction44–46 but also may degrade cartilage matrix.47
Programmes that are performed too aggressively, with running and agility drills 5 to 6 weeks after surgery and return to full activity and competition 16 weeks’ postoperatively, show 11–52% abnormal displacements at follow-up.48–50 In a less aggressive rehabilitation programme, with delay of high loads and strenuous activities for at least 4 months after surgery, abnormal displacements decreased to 15%, from which only 5% showed failure (6 mm or more of increase).43
Early strength training phase
Several studies recommend continuous passive motion via an externally applied force, especially if postoperative joint motion causes difficulties.39,51,52 It has been shown not to increase effusion or haemarthrosis.42 However, if pain and muscle spasm cause patients to resist these passive motions, strong forces could damage the healing graft and contraindicate the measure.
Isometric contractions and electrical stimulation of the quadriceps also start from the second day and are performed daily. Electrical stimulation not only stimulates quadriceps contraction, but also increases pain threshold. From the moment contraction of the quadriceps muscle is normal again, isotonic contractions, which cause higher muscular forces, are necessary to maintain strength. Because the effects on the maturing graft are unknown, and a direct relationship exists between the inert and contractile structures, it is advisable to start with a low load, which is applied close to the knee joint. Movements should also not pass 30° of extension because studies on strain in the normal and reconstructed anterior cruciate ligament during isotonic contraction have shown the final 30° of extension to be seven times that of full flexion to 30°.53
Attention should be paid to a normal, symmetrical gait, which maintains normal articular cartilage and muscle re-education.54,55 Any abnormalities during gait must therefore be identified and treated before weight bearing is increased.
Intensive strength training phase
In a study on this matter during standing, knee flexion of 30° or more, together with trunk flexion of 30° or more, increased the protective posterior drawer force of the hamstrings.56
Isokinetic contractions have their own value. Because muscular defects have been shown to be more likely diagnosed at special velocities, it is of great advantage to investigate that aspect of muscular deficiency. With the use of a device, resistance can be adjusted accurately at the indicated velocity.57 It is advisable to perform three sets of 10 repetitions twice a day on every other day and the load should not exceed 70% of maximum effort. However, because of the process of incorporation of the graft, it seems better not to start such exercises before the sixth postoperative week and also in the absence of pain and swelling. The effect of isokinetic exercises on force and endurance has been shown to be greater than that of isotonic exercises. The high loading contraindicates these exercises when there is patellofemoral crepitus, unless this is limited to the range of motion outside the crepitus.
Return to sports
To be successful in rehabilitation, exercises must also be similar to the specific demands of the individual sport or activity.58 Strenuous and difficult aspects are trained in isolation until proficiency has again been obtained. From that moment, and on condition that pain, effusion and patellofemoral crepitus are absent and forward translation of the tibia stays normal, training in the group can restart.
Tables 2 and 3 give a survey of the whole rehabilitation programme after anterior cruciate ligament (ACL) reconstruction.37
Table 2
Evaluation-based rehabilitation advanced weight bearing and minimal protection programme: range of motion after ACL reconstruction. Weeks 1–5a
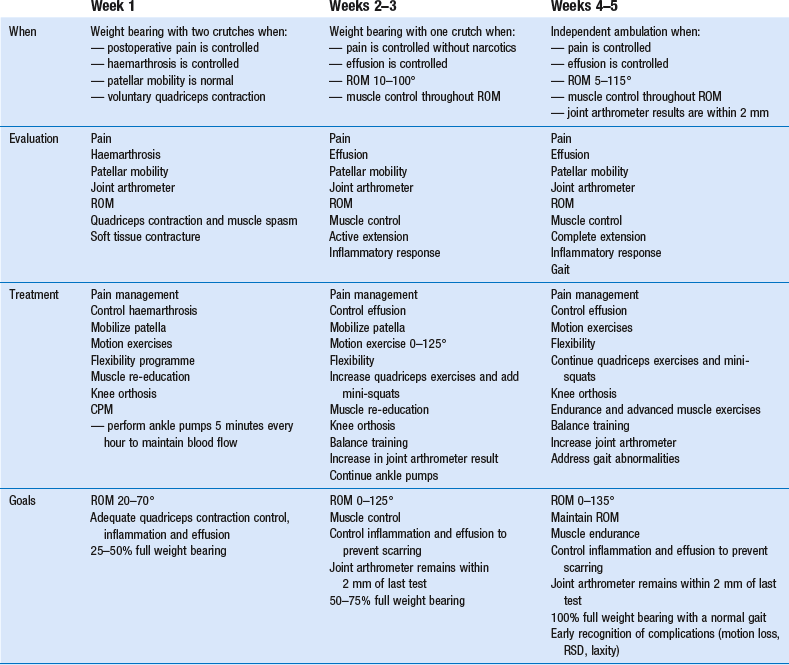
CPM, continuous passive motion; ROM, range of motion; RSD, reflex sympathetic dystrophy.
aRationale: Achieve full weight bearing and full range of motion without compromising graft fixation or graft maturation.
Table 3
Evaluation-based rehabilitation advanced muscle training after ACL reconstruction. Weeks 6–52a
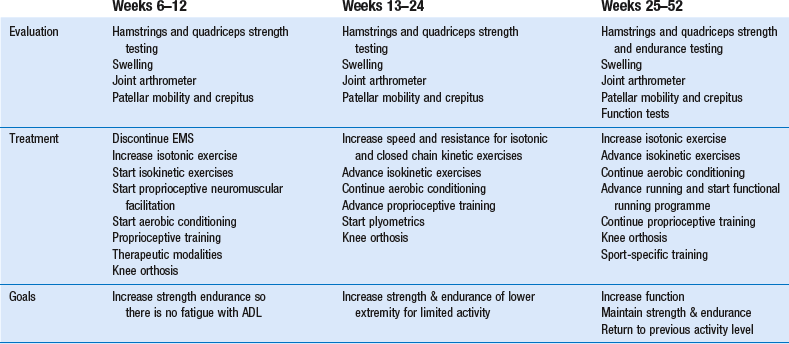
ADL, activities of daily living; EMS, electrical muscle stimulation.
aGeneral criteria: No effusion, painless range of motion, joint stability; performs activities of daily living without pain; range of knee motion 0–125°; full weight bearing.
References
1. McDaniel, WJ, Jr., Isolated partial tear of the anterior cruciate ligament. Clin Orthop 1976; 115:209. ![]()
2. Järvinen, M, Kannus, P, Quadriceps muscle atrophy and long-term recovery after knee ligament injury. Ann Chirurg Gynaecol 1987; 76:108–113. ![]()
3. Hughston, JC, Andrews, JR, Cross, MJ, Moschi, AM, Classification of knee ligament instabilities. J Bone Joint Surg. 1976;58A(2):159–179. ![]()
4. Muhr, G, Wagner, M. Kapselbandverletzungen des Kniegelenks. Diagnostikfibel. Berlin: Springer; 1981.
5. Claes, T, Martens, M. De voorste kruisband: Anatomie, Funktie en Pathologie. Spectrum Int. 1987; 30(4):1.
6. Liljedahl, SO, Lindvall, N, Wetterfors, J, Early diagnosis and treatment of acute ruptures of the anterior cruciate ligament. J Bone Joint Surg. 1965;47A(8):1503–1513. ![]()
7. Cyriax, JH. Textbook of Orthopaedic Medicine, vol 1, Diagnosis of Soft Tissue Lesions, 8th ed. London: Baillière Tindall; 1982.
8. Rubinstein, RA, Jr., Shelbourne, KD, McCarroll, JR, VanMeter, CD, Rettig, AC, The accuracy of the clinical examination in the setting of posterior cruciate ligament injuries. Am J Sports Med. 1994;22(4):550–557. ![]()
9. Anderson, AF, Rennirt, GW, Standeffer, WC, Jr., Clinical analysis of the pivot shift tests: description of the pivot drawer test. Am J Knee Surg. 2000;13(1):19–23. ![]()
10. Bach, BR, Warren, RF, Wickiewicz, TL, The pivot shift phenomenon: results and description of a modified clinical test for anterior cruciate ligament insufficiency. Am J Sports Med. 1988;16(6):571. ![]()
11. Trickey, EL, Ligamentous injuries around the knee. BMJ 1976; 2:1492. ![]()
12. Clancy, WG, Ray, JM, Zoltan, DJ, Acute tears of the anterior cruciate ligament. J Bone Joint Surg 1988; 60A:1483. ![]()
13. Kannus, P. Non-operative treatment of grade II and grade III sprains of the lateral ligament compartment of the knee. Am J Sports Med. 1989; 17(1):83.
14. Kannus, P, Jarvinen, M. Non-operative treatment of acute knee ligament injuries. Sports Med. 1990; 9(4):244.
15. Shelbourne, KD, Nitz, P, Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med 1990; 80:292–299. ![]()
16. Ellsasser, JC, Reynolds, FC, Omohundro, JR, The non-operative treatment of collateral ligament injuries of the knee in professional football players. J Bone Joint Surg 1974; 56A:1185. ![]()
17. Fetto, JF, Marshall, JL, Medial collateral ligament injuries to the knee: a rationale for treatment. Clin Orthop 1978; 132:206. ![]()
18. Jones, RE, Bradford Henley, M, Francis, P, Non-operative management of isolated grade III collateral ligament injury in high school football players. Clin Orthop Rel Res 1986; 213:137–140. ![]()
19. Hughston, JC, Eilers, AF, The role of the posterior oblique ligament in repairs of acute medial collateral ligament tears of the knee. J Bone Joint Surg 1973; 55A:923. ![]()
20. Sandberg, R, Balkfors, B, Nilsson, B, Westin, N, Operative versus non-operative treatment of recent injuries to the ligaments of the knee. A prospective randomized study. J Bone Joint Surg 1987; 69A:1120. ![]()
21. Hastings, DE, The non-operative management of collateral ligament injuries of the knee joint. Clin Orthop 1980; 147:22. ![]()
22. Indelicato, P, Hermansdorfer, J, Huegel, M, Nonoperative management of complete tears of the medial collateral ligament of the knee in intercollegiate football players. Clin Orthop 1990; 256:174–177. ![]()
23. Cyriax, J. Textbook of Orthopaedic Medicine, Vol II, Treatment by Manipulation, Massage and Injection, 11th ed. London: Baillière Tindall; 1984.
24. O’Donoghue, DH, Treatment of acute ligamentous injuries of the knee. Orthop Clin North Am 1973; 4:617. ![]()
25. Mathieu, P, Wybier, M, Busson, J, Morvan, G, The medial collateral ligament of the knee. Ann Radiol (Paris). 1997;40(3):176–181. ![]()
26. Hughston, JC, Complications of anterior cruciate ligament surgery. Orthop Clin North Am 1985; 16:237. ![]()
27. Buckley, SL, Barrack, RL, Alexander, AH, The natural history of conservatively treated partial anterior cruciate ligament tears. Am J Sports Med. 1989;17(2):221. ![]()
28. Barton, T, Posterior cruciate ligament insufficiency. Sports Med 1984; 1:419–430. ![]()
29. Barton, T, Torg, J, Natural history of the posterior cruciate ligament deficient knee. Am J Sports Med 1985; 13:439. ![]()
30. Longenecker, S, Hughston, J. Long-term follow-up of isolated posterior cruciate injuries. Am J Sports Med. 1987; 15:628.
31. Fowler, P, Messieh, S, Isolated posterior cruciate ligament injuries in athletes. Am J Sports Med 1987; 15:553. ![]()
32. Dejour, H, The natural history of rupture of the posterior cruciate ligament. Rev Chirurg Orthop 1988; 74:35. ![]()
33. MacNicol, MF. The Problem Knee. Diagnosis and Management in the Younger Patient. London: Heinemann Medical; 1986.
34. Gerber, CH, Funktionelle Rehabilitation nach komplexen Knieverletzungen. Wissenschaftliche Grundlagen u Praxis. Schweiz Zeitschr Sportmed 1980; 28:37–56. ![]()
35. Hermans, GPH, Rondhuis, G. Kniebandreconstructies bij ‘late’ instabiliteit. Ned Tijdschr Fysioth. 1981; 2:34.
36. Ahrendt, E, Frenzel, G. Erfahrungen in der Diagnostik, Therapie u Rehabilitation bei Kreuzbandverletzungen. Med Sport. 1982; 5:145–149.
37. Managine, RE, Noyes, FR, DeMaio, M, Sports Medicine Rehabilitation Series. Minimal protection programme: advanced weight bearing and range of motion after ACL reconstruction. Weeks 1–5. Orthopedics. 1992;15(4):504–515. ![]()
38. DeMaio, M, Noyes, FR, Managine, RE, Advanced muscle training after ACL reconstruction: weeks 6 to 52. Orthopedics. 1992;15(6):757–767. ![]()
39. Salter, RB, The biologic concept of continuous passive motion of synovial joints. The first 18 years of basic research and its clinical application. Clin Orthop 1989; 242:12–25. ![]()
40. Noyes, FR, Barber, D, DeMaio, M, Managine, RE, Early knee motion after open and arthroscopic anterior cruciate ligament reconstruction. Am J Sports Med 1987; 15:149–160. ![]()
41. Sachs, RA, Daniel, DM, Stone, ML, et al, Complications of knee ligament surgeryDaniel DM, Akeson WH, O’Connor JJ, eds. Knee Ligaments: Structure, Function, Injury and Repair. Raven Press: New York, 1990:505–520. ![]()
42. DeMaio, M, Noyes, FR, Managine, RE, Principles for aggressive rehabilitation after reconstruction of the anterior cruciate ligament. Orthopedics. 1992;15(3):385–392. ![]()
43. Barber-Westin, SD, Noyes, FR, Heckmann, TP, et al, The effect of exercise and rehabilitation on anterior–posterior knee displacements after anterior cruciate ligament autograft reconstruction. Am J Sports Med. 1999;27(1):84–93. ![]()
44. Spencer, J, Hayes, KC, Alexander, IJ, et al, Knee joint effusion and quadriceps inhibition in man. Arch Phys Med 1984; 65:171–177. ![]()
45. Stokes, M, Young, A. Investigations of quadriceps inhibition. Implications for clinical practice. Physiotherapy. 1984; 70(11):425–428.
46. Kennedy, JC, Alexander, IJ, Hayes, KC, et al, Nerve supply of the human knee and its functional importance. Am J Sports Med 1982; 10:329–335. ![]()
47. Fulkerson, JP, Schutzer, SF, Winters, TF, Jr., et al. Articular cartilage. In: Albright JA, Brand RA, eds. The Scientific Base of Orthopaedics. 2nd ed. Norwalk, CT: Appleton & Lange; 1987:347–371.
48. Glasgow, SG, Gabriel, JP, Sapega, AA, et al, The effect of early versus late return to vigorous activities on the outcome of anterior cruciate ligament reconstruction. Am J Sports Med 1993; 21:243–248. ![]()
49. Shelbourne, KD, Nitz, P, Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med 1990; 18:292–299. ![]()
50. Shelbourne, KD, Klootwyk, TE, Wilckens, JH, et al, Ligament stability 2 to 6 years after anterior cruciate ligament reconstruction with autogenous patellar tendon graft and participation in accelerated rehabilitation program. Am J Sports Med 1995; 23:575–579. ![]()
51. Dodds, JA, Keene, JS, Graf, BK, et al, Results of knee manipulations after anterior cruciate ligament reconstruction. Am J Sports Med 1991; 19:283–287. ![]()
52. Behrens, F, Kraft, EL, Oegema, TR, Jr., et al, Biochemical changes in articular cartilage after joint immobilization by casting or external fixation. J Orthop Res 1989; 7:335–343. ![]()
53. Arms, SW, The biomechanics of the anterior cruciate ligament rehabilitation and reconstruction. Am J Sports Med 1984; 412:8–18. ![]()
54. Palmoski, MJ, Colyer, RA, Brandt, KD, et al, Joint motion in the absence of normal loading does not maintain normal articular cartilage. Arthritis Rheum 1980; 23:325–334. ![]()
55. Ghosh, P, Sutherland, J, Bellenger, C, et al, The influence of weight bearing exercise on articular cartilage of meniscectomy joints. An experiment study in sheep. Clin Orthop 1990; 252:101–113. ![]()
56. Ohkoshi, Y, Yasuda, K, Kaneda, K, et al, Biomechanical analysis of rehabilitation in the standing position. Am J Sports Med 1991; 19:605–611. ![]()
57. Sapega, AA, Muscle performance evaluation in orthopedic practice. J Bone Joint Surg 1990; 72A:1562–1574. ![]()
58. American Academy of Orthopedic Surgeons. Athletic Training and Sports Medicine, 2nd ed. Parkridge IL: AAOS; 1991.