Chapter 141 Ocular Allergies
Clinical Manifestations
Allergic Conjunctivitis
Allergic conjunctivitis is the most common hypersensitivity response of the eye, affecting approximately 25% of the general population and 30% of children with atopy. It is caused by direct exposure of the mucosal surfaces of the eye to environmental allergens. Patients complain of variable ocular itching, rather than pain, with increased tearing. Clinical signs include bilateral injected conjunctivae with vascular congestion that may progress to chemosis, or conjunctival swelling, and a watery discharge (Fig. 141-1). Allergic conjunctivitis occurs in a seasonal or, less commonly, perennial form. Seasonal allergic conjunctivitis is typically associated with allergic rhinitis (Chapter 137) and is most commonly triggered by pollens. Major pollen groups in the temperate zones include trees (late winter to early spring), grasses (late spring to early summer), and weeds (late summer to early fall), but seasons can vary significantly in different parts of the country. Mold spores can also cause seasonal allergy symptoms, principally in the summer and fall. Seasonal allergy symptoms may be aggravated by coincident exposure to perennial allergens. Perennial allergic conjunctivitis is triggered by allergens such as animal danders or dust mites that are present throughout the year. Symptoms are usually less severe than with seasonal allergic conjunctivitis. Since pollens and soil molds may be present year round while exposure to perennial allergens such as furred animals may be intermittent, classification as intermittent (i.e., symptoms present <4 days a week or for <4 weeks) and persistent (symptoms present >4 days a week and for >4 weeks) has been proposed.
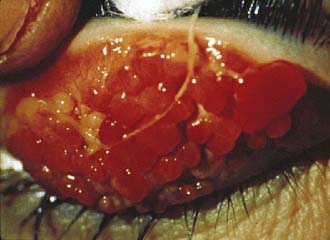
Vernal Keratoconjunctivitis
Vernal keratoconjunctivitis is a severe bilateral chronic inflammatory process of the upper tarsal conjunctival surface that occurs in a limbal or palpebral form. It may threaten eyesight if there is corneal involvement. Although vernal keratoconjunctivitis is not IgE mediated, it occurs most frequently in children with seasonal allergies, asthma, or atopic dermatitis. Vernal keratoconjunctivitis affects boys twice as often as girls and is more common in persons of Asian and African origin. It affects primarily children in temperate areas, with exacerbations in the spring and summer. Symptoms include severe ocular itching exacerbated by exposure to irritants, light, or perspiration. In addition, patients may complain of severe photophobia, foreign-body sensation, and lacrimation. Giant papillae occur predominantly on the upper tarsal plate and are typically described as cobblestoning (Fig. 141-2). Other signs include a stringy or thick, ropey discharge, cobblestone papillae, transient yellow-white points in the limbus (Trantas dots) and conjunctiva (Horner points), corneal “shield” ulcers, and Dennie lines (Dennie-Morgan folds), which are prominent symmetric skinfolds that extend in an arc from the inner canthus beneath and parallel to the lower lid margin. Children with vernal keratoconjunctivitis have measurably longer eyelashes, which may represent a reaction to ocular inflammation.
Diagnosis
Non-allergic conjunctivitis can be viral, bacterial, or chlamydial in origin. It is typically unilateral but can be bilateral with symptoms initially developing in one eye (Chapter 618). Symptoms include stinging or burning rather than itching and often a foreign body sensation. Ocular discharge can be watery, mucoid, or purulent. Masqueraders of ocular allergy also include nasolacrimal duct obstruction, foreign body, blepharoconjunctivitis, dry eye, uveitis, and trauma.
Treatment
Primary treatment of ocular allergies includes avoidance of allergens, cold compresses, and lubrication. Secondary treatment regimens include the use of oral or topical antihistamines (see Table 142-1) and, if necessary, topical decongestants, mast cell stabilizers, and anti-inflammatory agents (Table 141-1). Drugs with dual antihistamine and mast cell blocking activities provide the most advantageous approach in treating allergic conjunctivitis, with both fast-acting symptomatic relief and disease-modifying action. Children often complain of stinging or burning with use of topical ophthalmic preparations and usually prefer oral antihistamines for allergic conjunctivitis. It is important not to contaminate topical ocular medications by allowing the applicator tip to contact the eye or eyelid. Using refrigerated medications may decrease some of the discomfort associated with their use. Topical decongestants act as vasoconstrictors, reducing erythema, vascular congestion, and eyelid edema, but do not diminish the allergic response. Adverse effects of topical vasoconstrictors include burning or stinging and rebound hyperemia or conjunctivitis medicamentosa with chronic use. Combined use of an antihistamine and a vasoconstrictive agent is more effective than use of either agent alone. Use of topical nasal corticosteroids for allergic rhinoconjunctivitis decreases ocular symptoms, presumably through a naso-ocular reflex.
Table 141-1 TOPICAL OPHTHALMIC MEDICATIONS FOR ALLERGIC CONJUNCTIVITIS
| DRUG AND TRADE NAMES | MECHANISM OF ACTION AND DOSING | CAUTIONS AND ADVERSE EVENTS |
|---|---|---|
NSAID, nonsteroidal anti-inflammatory drug.
Baroody FM, Foster KA, Markaryan A, et al. Nasal ocular reflexes and eye symptoms in patients with allergic rhinitis. Ann Allergy Asthma Immunol. 2008;100:194-199.
Bielory L. Allergic and immunologic disorders of the eye: II. Ocular allergy. J Allergy Clin Immunol. 2000;106:1019-1032.
Bielory L. Intranasal corticosteroids reduce ocular symptoms of allergic rhinitis as a class effect. J Allergy Clin Immunol. 2008;121:538-539.
Bielory L. Ocular allergy treatment. Immunol Allergy Clin North Am. 2008;28:189-224.
Bielory L, Friedlaender MH. Allergic conjunctivitis. Immunol Allergy Clin North Am. 2008;28:43-58.
Bousquet J, Khaltaev N, Cruz AA, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy. 2008;63(Suppl 86):8-160.
Donshik PC, Ehlers WH, Ballow M. Giant papillary conjunctivitis. Immunol Allergy Clin North Am. 2008;28:83-103.
Jun J, Bielory L, Raizman MB. Vernal conjunctivitis. Immunol Allergy Clin North Am. 2008;28:59-82.