Chapter 33 Occipitocervical Region
Surgical Anatomy
Dorsal Surgical Anatomy of the Occipitocervical Region
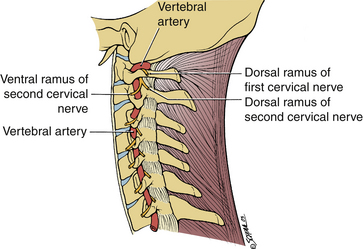
Dorsal approaches to the OC area are most commonly used for OC fusions. During the approach, dissection through several muscular layers is required. The trapezius muscle constitutes the first superficial layer. The trapezius arises from the external occipital protuberans, the ligamentum nuchae, and the spines of the seventh cervical and all thoracic vertebrae.1 The upper fibers insert into the lateral third of the clavicle and form the curve of the shoulder. The middle fibers insert into the medial edge of the acromion and the superior margin of the spine of the scapula, and the lower fibers ascend also onto the scapular spine (Fig. 33-1). The nerve supply of the trapezius muscle is the accessory nerve.
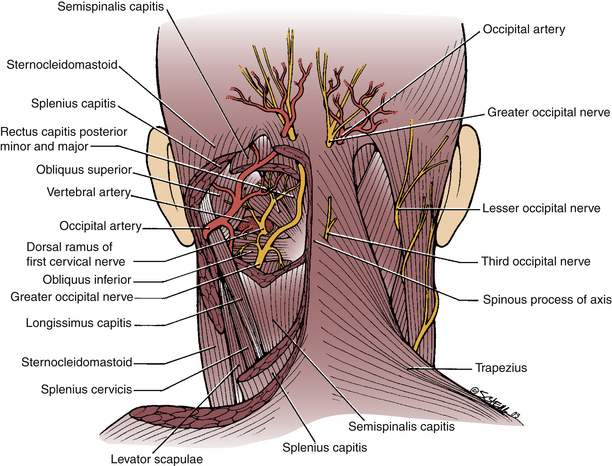
FIGURE 33-1 Dorsal surgical anatomy of the occipitocervical region. Superficial (right) and deep (left).
The main vessels in the dorsal OC area are the occipital artery and the vertebral artery. The occipital artery arises from the external carotid artery in the front of the neck and runs dorsally and rostrally deep to the mastoid process and then courses dorsally immediately deep to the muscles attached to the superior nuchal line. It then pierces the trapezius muscle 2.5 cm from the midline to ramify on the back of the head (see Fig. 33-1). As for the vertebral artery, only the third part of this artery is significant during the approach. It emerges from the foramen and the transverse process of the atlas and hooks dorsomedially around the dorsal surface of the lateral mass of the atlas (see Fig. 33-1). It is partly separated from the arch of the atlas by the first cervical nerve (Fig. 33-2; see also Fig. 33-1). It then passes ventromedially in front of the thickened lateral edge of the dorsal atlanto-occipital membrane, which forms an arch over the artery. Occasionally, this arch may be ossified and is referred to as the ponticulus posticus.2 This condition must be recognized preoperatively because failure to do so can lead to catastrophic results if the lateral mass C1 screws are placed through the vertebral arteries. The artery then pierces the dura mater and enters the vertebral canal. The suboccipital plexus of veins is a network of veins that drains into the deep cervical vein and into the vertebral venous plexus around the vertebral artery. The greater occipital nerve is the medial branch of the dorsal ramus of the second cervical nerve, which is the thickest cutaneous nerve in the body. It appears at the middle of the lower border of the inferior oblique muscle and curves superior medially across the suboccipital triangle. It runs rostrally on that muscle and then pierces the trapezius muscle about 2 cm lateral to the occipital protuberans (see Fig. 33-1).
Ventral Anatomy of the Occipitocervical Junction
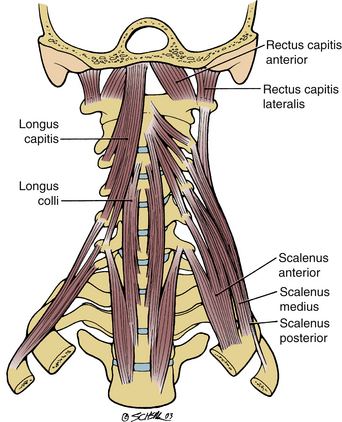
Three muscles originate from the ventral aspect of the atlas: longus colli, rectus capitis anterior, and rectus capitis lateralis (Fig. 33-3).
1. The longus colli muscle is the longest and most medial of the muscles. It extends from the anterior tubercle of the atlas to the lower part of the body of the upper thoracic vertebrae. Between these points it is attached to all the vertebral bodies and into the third to sixth cervical transverse processes.
2. The rectus capitis anterior is a short, wide muscle that originates from the ventral surface of the lateral mass of the atlas and is inserted into the base of the skull ventral to the occipital condyle.
3. The rectus capitis lateralis is a short muscle that runs vertically between the rostral surface of the transverse process of the atlas and jugular process of the occipital bone. It lies dorsal to the jugular foramen and is separated from the rectus capitis anterior by the ventral ramus of the first cervical nerve, which supplies both muscles. The function of these muscles is to stabilize the skull on the vertebral column (see Fig. 33-3).
Vertebral Artery
The anatomy of the vertebral artery must be understood because injury to this artery may have dire consequences. The artery starts as a branch of the subclavian artery and passes to the transverse process of the sixth cervical vertebra.1 The artery then ascends vertically through the foramina transversaria accompanied by the vertebral veins and plexus of sympathetic nerve fibers derived from the cervicothoracic ganglion of the sympathetic trunk. Between the transverse processes, it lies medial to the intertransverse muscles and ventral to the ventral rami of the cervical nerves. Upon entering the axis it turns laterally under the superior articular facet in the foramen transversarium and enters the foramen transversarium of the atlas, which is placed farther laterally than the others. Therefore at this level, the artery takes a lateral course (see Fig. 33-2). The artery then emerges on the rostral surface of the atlas between the rectus capitis lateralis muscle and the superior articular process of the atlas. Here it lies with the ventral ramus of the first cervical nerve and curves with it horizontally around the lateral and dorsal aspect of the superior articularis process. It then traverses the articular process and the dorsal arch of the atlas, where it lies rostrally to the dorsal ramus of the first cervical nerve. The artery then turns rostrally and pierces the dura and arachnoid mater. It enters the cranial cavity through the foramen magnum. It then runs ventrally and rostrally over the ventral surface of the medulla oblongata to meet and join the opposite vertebral artery at the inferior border of the pons to form the basilar artery. Through the branches of these vessels, blood is supplied to the hindbrain, midbrain, and dorsal aspect of the cerebrum and the rostral aspect of the spinal medulla. The vertebral vein originates from a plexus of veins that is formed by the union of veins from the internal venous plexus and suboccipital triangle. It accompanies the vertebral artery through the foramina transversaria and exits the sixth cervical transverse process. It passes ventral to the subclavian artery and ends by entering the dorsal surface of the brachiocephalic vein near its origin.
Atlanto-Occipital Joint
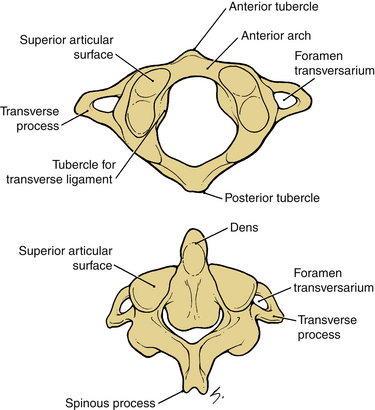
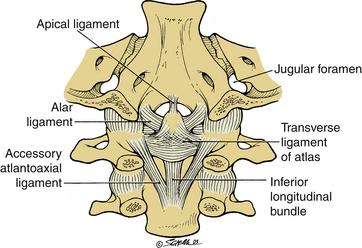
The atlas is a ring of bone with a lateral mass on each side (Fig. 33-4, top).1 The lateral masses are articulated rostrally with the occipital condyles and caudally with the superior articular facets of the axis. Each has a transverse process projecting laterally from it. The atlas is attached to the occiput by strong ligaments, which hold these bones together. However, the articular surfaces, which the atlas has with the skull and axis, are of two different configurations. The kidney-shaped occipital condyles lie on the ventrolateral aspect of the foramen. They fit into the superior articular facets of the atlas, which are also kidney shaped (see Fig. 33-4). The joint allows flexion and extension and slight side-to-side rocking of head motion, but no rotation. The stability of these joints depends on the aid of ligaments, the tectorial membrane, and the longitudinal bands of the cruciate ligament, which all bind the skull to the axis. The ligaments of the joints of the atlas include the anterior longitudinal ligament, which tapers rostrally to be attached to the tubercle of the axis and continues as a narrow band to the base of the skull. The dorsal atlanto-occipital membrane is a rostral continuation of the ligamentum flavum. This membrane passes from the dorsal arch of the atlas to the margin of the foramen magnum dorsal to the atlanto-occipital joint. The lateral margins of the membrane arch over the corresponding vertebral artery and the first cervical nerve. In some cases, these margins may be ossified. The tectorial membrane is a broad ligamentous sheet, which is the rostral continuation of the posterior longitudinal ligament. It passes from the dorsal surface of the body of the axis to the cranial surface of the occipital bone, and it holds the axis to the skull and covers the dorsal surfaces of the dens with its ligaments and the ventral margin of the foramen magnum. The cruciate ligament is formed by rostral and ventral longitudinal bands, which pass from the transverse ligament to the cranial surface of the occipital bone and the body of the axis, respectively. The apical ligament of the dens is a cordlike ligament, which stretches from the apex of the dens to the cranial surface of the occipital bone, immediately above the foramen magnum. The alar ligaments are strong ligaments that arise from the sloping sides of the dens (Fig. 33-5). They pass laterally and upward to the medial sides of the occipital condyle and tighten when the atlas, carrying the skull, rotates around the dens. They are the main factor in limiting rotation of the atlantoaxial joint. The first and second cervical spinal nerves pass dorsally to the OC and C1-2 joint capsules, respectively, and not ventral to the articular facets, as is the case with the remaining subaxial cervical vertebrae.
Approaches to the Occipitocervical Region
Dorsal Approach to the Occipitocervical Region
The dorsal approach is most commonly used when fusion of the OC region is indicated. This approach has been described by different authors, including Grantham et al.3 and Wertheim and Bohlman.4 Key in the approach is positioning of the patient to allow safe intubation and protect the neural elements. Longitudinal traction should be applied preoperatively to provide stability during the intubation process. The patient is then logrolled into the prone position. Support for the head may also be provided using a Mayfield three-point headrest. Radiography or intraoperative fluoroscopy is used to confirm the alignment of the occiput to the atlas and the remainder of the cervical spine. The skin is then prepared, and the subcutaneous tissues are injected with a solution of epinephrine 1:500,000. A midline incision is made, extending from the external occipital protuberance to the spinous process of the fourth or fifth cervical vertebra. The spinous process of the C2 is the most prominent of the spinous processes encountered during the approach. The spinous process of C2 is bifid, allowing the short external rotators of the head to be attached to the cervical spine. Once the skin is incised, the incision is extended into the deep fascia and then into the ligamentum nuchae. It is very important to remain in the midline to avoid excessive bleeding. This placement can be confirmed by palpating the alignment of the spinous processes and by visualizing the avascular midline plane of the ligamentum nuchae. By staying in the midline, the paramedian venous plexuses are avoided. The paravertebral muscles are stripped off the spinous processes and the lamina subperiosteally to avoid excessive bleeding.
Although some may believe that it is safe to use Cobb elevators in dissecting the muscles subperiosteally off the lamina, the authors do not recommend this technique. The fact that the laminae are weaker in this region than in the lumbar spine may lead to fracture of the lamina because of excessive force, as well as increased blood loss caused by uncontrolled stripping of the musculature. However, a Cobb elevator may be used to gently retract the muscles, placing them under tension, while the muscles are stripped off of the lamina using a freer elevator or cautery in a controlled manner. At the base of the skull, full-thickness scalp flaps are reflected along the occipital ridge about 2 to 3 cm laterally. The extensive lateral dissection along the lamina of the cervical spine should be to the groove, which indicates the junction of the lamina along with the articular facet. Once the occipital exposure is completed, special care must be taken during the dissection of the arches of C1. The vertebral artery runs on the rostral surface of the arch and the lateral third of the arch (see Figs. 34-1 and 34-2). To expose this area safely, only 1 cm on each side of the dorsal arch of C1 is dissected. In this area, it is important to elevate the muscles subperiosteally. Cauterizing in this area is not recommended because of the thin membrane that attaches the base of the skull to the arch of atlas. Once exposure of the bony occipital protuberance, the dorsal arch of the atlas, and the remainder of the laminae of the cervical spine is accomplished, arthrodesis may be completed. This may be performed using the technique described previously by Grantham or modifications that were introduced by other authors.3 With this technique, 24-gauge stainless-steel wires are used along with an iliac crest bone graft that is contoured to span the distance from the occiput and the upper cervical laminae after the laminae and occiput are decorticated with a burr. Occipital plates or rods that are inserted into the lateral mass of C1 and C2 using screws may also be used to provide more rigid fixation.
Ventral Approaches
Indications for ventral approaches include ventral bony tumors with neural compression, extradural tumors, intradural midline lesions, and irreducible subluxations.5–9 The ventral approach may also be used for repair of nonunion of C2 odontoid fractures and for odontoid resection.10 The ventral aspect of the OC junction may be approached via an extension of the ventral retropharyngeal/extrapharyngeal approach to the upper cervical spine or via a transoral approach.
Ventral Retropharyngeal Approach
The ventral retropharyngeal approach to the upper cervical spine has been described by Whitesides11 and McAfee et al.12 This approach allows exposure of the ventral aspect of the axis and atlas and also may allow exposure of the clivus and ventral aspect of the foramen magnum. Decompression and OC fusion may be performed through this approach.
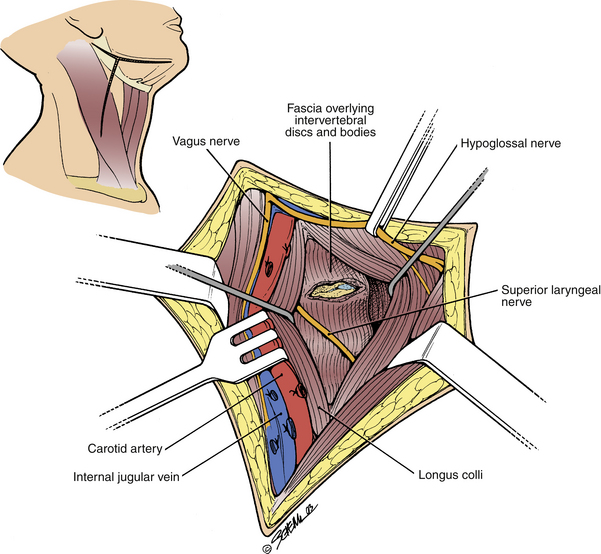
Cortical somatosensory-evoked potentials may be measured. The patient is positioned on the operative wedge frame, and the neck is extended as far as allowed while the patient is awake without signs of neurologic compromise. A modified transverse submandibular incision is used (Fig. 33-6). The incision is made on the patient’s right side, if the surgeon is right handed. This exposure is the rostral extension of the ventral lateral exposure to the midpart of the cervical spine. The fascial planes that are dissected through are the same as those described in the ventral approach to the cervical spine, consisting of the superficial fascia and the deep fascia layers. The submandibular incision is made through the platysmal muscle and the superficial fascia and skin are immobilized in the platysmal plane of the superficial fascia. The marginal mandibular branch of the facial nerve is found with the aid of the nerve stimulator by ligating and dissecting the retromandibular veins superiorly. The common facial vein is continuous with the retromandibular vein, and the branches of the mandibular nerve usually cross the latter vein superficially and superiorly. The superficial branches of the fascial nerve are protected. The ventral border of the sternocleidomastoid muscle is mobilized by longitudinally transecting the superficial layer of deep cervical fascia. The submandibular salivary gland is resected, and the duct is sutured adequately to prevent the formation of a salivary fistula. The jugular-digastric lymph node from the submandibular and carotid angles can be resected and sent for frozen section if a neoplasm is in question. The dorsal belly of the digastric muscle and the stylohyoid muscle are identified, and the digastric tendon is divided and tagged for later repair. As described by Whitesides,11 rostral traction at the base of the origin of the stylohyoid muscle can cause injury to the facial nerve as it exits from the skull. After the digastric and stylohyoid muscles are divided, the hyoid bone and the hypopharynx are mobilized medially. The hypoglossal nerve, which is identified with a nerve stimulator, is then completely mobilized from the base of the skull to the ventral border of the hypoglossal muscle (see Fig. 33-6). It is retracted rostrally through the remainder of the procedure. The dissection then proceeds to the retropharyngeal space between the carotid sheath laterally and the pharynx medially. Rostral exposure to the atlas and the base of the skull is facilitated by ligating the branches of the carotid artery and internal jugular vein (see Fig. 33-6). The vessels to be ligated (from caudally and progressing rostrally) include the superior thyroid artery and vein, lingual artery and vein, ascending pharyngeal artery and vein, and facial artery and vein. After ligation, the carotid sheath is easily mobilized laterally. The superior pharyngeal nerve, which is also identified with the help of the nerve stimulator, is mobilized from its origin near the nodose ganglion to the entrance into the larynx. The alar and prevertebral fasciae are transected longitudinally to expose the longus colli muscle, which runs longitudinally. It is important at this point to maintain the orientation of the anterior tubercle of the atlas because rotation and lateral dissection may endanger the vertebral artery. The dissection along the prevertebral fascia may be extended cranially to reach the base of the skull and the clivus through this approach. Once this exposure is achieved, ventral decompression and, if necessary, fusion of the OC junction may be initiated.
Transoral Approach
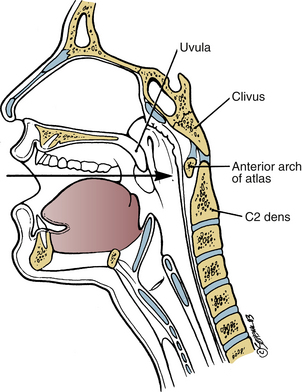
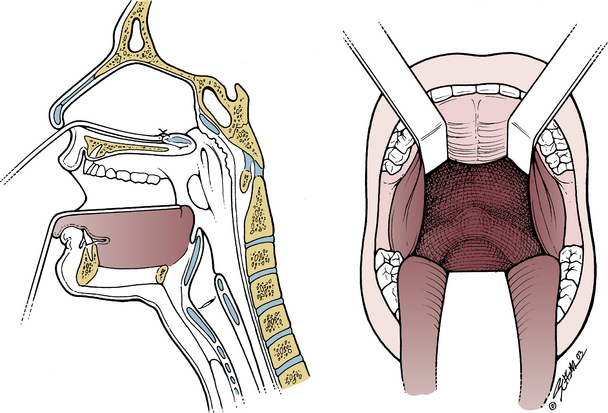
The transoral procedure allows exposure of the clivus, the arches of the atlas, and the ventral aspect of C2 (Fig. 33-7). Adequate interdental distance (at least 25 mm) is necessary for this exposure. If this is not achievable or there is a disease involving the temporomandibular joint, a transmandibular splitting approach or other more extensive approaches may be necessary.13
Preoperative management includes assessment of the interdental space. After this is found to be adequate, the dorsal pharynx should be cultured to allow adequate preoperative antibiotic coverage. Palpation of the dorsal pharynx is then performed to identify the landmarks. This is performed after the dorsal pharynx is anesthetized with topical anesthetic to prevent the gag reflex. The anterior tubercle of C1 and the ventral body of C2 are palpable because they are directly dorsal to the mucous membrane. A tracheotomy is performed, although some authors avoid tracheotomy by using a nasal tracheal fiberoptic intubation while the patient is awake. The nasal tracheal tube does not impinge on the surgical field for lesions below the foramen magnum. They reserve tracheotomy for patients for whom long-term ventilatory problems are expected.7,14 A nasogastric tube may be used to retract the uvula and soft palate to allow adequate exposure (Fig. 33-8). The nasogastric tube is passed through the nose and out of the mouth to elevate the soft palate. Intraoral retractors are used to depress the tongue to allow better exposure. The uvula of the palate may also be sutured to the roof of the mouth, and the tongue is retracted interiorly (see Fig. 33-8). Before the midline incision of the mucosa is made, the area is infiltrated with a 1:600,000 solution of epinephrine. The midline incision is then made, extending about 2 cm above the ventral arches of the atlas and 2 cm below the prominence of the arch. The desired structures can be accessed by retracting the mucosa laterally. This retraction assists exposure of the clivus of the occiput, C1, and C2. The rotation of the atlas may be deceiving, and the ventral aspect of the lateral mass may be mistakenly perceived as the anterior tubercle of C1.14 This wall places the vertebral artery at risk of being injured; it will also come closer to the midline because the atlas is rotated. If access to the clivus more superiorly is necessary, the hard palate may be split with a reciprocating saw to allow more access. When access to the retropharyngeal space using the transoral approach is limited either due to a transdental distance of less than 25 mm or to severe macroglossia, other approaches may be used. These include extended maxillotomy or mandibular osteotomy approaches.13,15,16
Extended Approaches to the Craniocervical Junction
Extended Maxillotomy
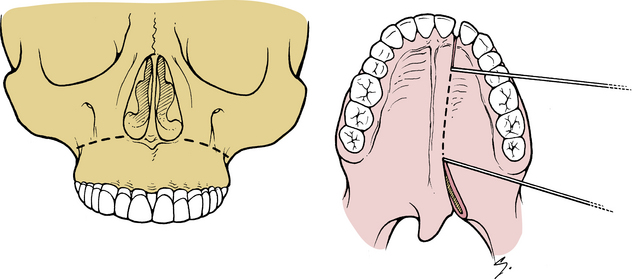
James and Crockard16 described surgical access to the base of the skull and upper cervical spine by extended maxillotomy, which provides a much wider surgical access to the base of the skull. With this technique, a tracheotomy and placement of the gastric tube are performed first. Next, the patient is positioned in the supine or three-quarter supine position with some degree of neck extension to assist access to the palate. Surgical exposure of the cranial base is performed through an incision made above the mucogingival reflection from the first molar tooth on either side, and the soft tissues are reflected subperiosteally to expose the ventral and lateral walls in the maxilla (Fig. 33-9). The osteotomy sites include (1) a transverse standard LeFort osteotomy cut that is made using an air-powered reciprocating saw, and (2) a sagittal cut that separates the two parts of the maxilla by sawing to the side of the midline suture (see Fig. 33-9). The bone between the central and incisor teeth is divided using a fine osteotome to avoid damage to the adjacent dental roots. This median section is completed with division of the soft palate in the midline. This exposure allows larger access to the clivus, through which a clivectomy can be performed. Excision of tumors and approaches to aneurysms can also be performed through this exposure. Complete details of the procedure may be found in the technique described by James and Crockard.16
Bilateral Sagittal Split Mandibular Osteotomy
Another approach that may be of use in gaining access to the retropharyngeal space when there is limited exposure is the bilateral sagittal split mandibular osteotomy (as described by Vishteh et al.13). In their technique, the sagittal split mandibular osteotomy is performed on both sides of the mandible, as an adjunct to the transoral approach to the ventral craniovertebral junction. They described the osteotomy as a stair-step split mandibulotomy (Fig. 33-10). Before the osteotomy is performed, a plate is placed in the appropriate position across the lateral osteotomy site on which the procedure is to be performed. A drill hole is made on each side, and screws are placed. The remaining drill holes are drilled, and the plate is removed and set aside. The osteotomy site courses through the lateral cortex medially above the lingula along the ventral border of the ramus lateral to the second and third molars and through the lateral cortex.
Transcondylar Approach to Craniovertebral Junction (Extreme Radial Craniocervical Approach)
Access to the craniovertebral junction through a ventral approach sometimes has it limitations, including inadequate exposure or inability to perform craniocervical fusion; difficulty in reaching lateral located lesions; narrowing of the interdental distance less than 25 mm, and thereby limiting the exposure; and the risk of infection from a contaminated field. The extreme lateral/transcondylar approach has been described by al-Mefty et al.17 and Bejjani et al.18 to access extradural non-neoplastic lesions of the ventral craniovertebral junction, where decompression and stabilization are necessary. The advantages of this approach include a more direct access to the lesion and direct visualization of the dural sac, eliminating manipulation of the brainstem or upper spinal cord. Identification and control of the ipsilateral vertebral artery are also assisted, along with direct visualization and protection of the lower cranial nerves. This approach also provides a more sterile field than the transoral approach. OC fusion and instrumentation can be performed during the same procedure, as opposed to the transcondylar approach.
The patient is placed in a halo brace with the neck and head in the neutral position. The positioning of the patient is in the supine position with the entire body being rotated 45 degrees to the opposite side. Intubation is performed while the patient is awake. Intraoperative monitoring is also recommended, including bilateral somatosensory-evoked potentials, bilateral brainstem auditory-evoked response, and the cranial nerves 10, 11, and 12.17 The skin incision begins behind the ear at the level of external auditory canal and extends medially to the midline and inferiorly to level of C4, where it curves ventrally to reach the ventral border of the sternomastoid muscle. The skin flap is elevated ventrally. This elevation exposes the greater auricular nerve and the sternomastoid muscle. Blunt dissection is performed along the ventral border of the sternomastoid muscle and falls superiorly to the mastoid process, where it is attached. The sternomastoid, splenius capitis, longissimus, and semispinalis muscles are detached from the mastoid in one layer and retracted. The eleventh cranial nerve must be identified and preserved where it enters the middle third of sternomastoid muscle. The dorsal belly of the digastric muscle is kept in place to protect the facial nerve as it exits the stylomastoid foramen. The deep muscular layer forms the suboccipital triangle, which is delineated by the major and minor rectus capitis muscles medially, the superior oblique muscle superiorly, and the inferior oblique muscle inferiorly. The apex of the triangle is the transverse process of C1. The horizontal segment of the vertebral artery and C1 root can be seen in this triangle. The C2 nerve root can be followed laterally where it crosses over the vertebral artery and its vertical segment between C1 and C2. The nerve root is protected. The vertebral artery is then identified from the transverse foramen of C2 to its entry to the dura mater. The vertebral artery is moved out of the foramen of C1 after this foramen is opened with a diamond drill, and the artery is then held inferomedially. The C1 nerve root may be sacrificed. After exposure is complete, the mastoid tip is drilled to expose the occipital condyle and the jugular bulb. The occipital condyle and the condylar surface of C1 are exposed widely and drilled out. The hypoglossal canal is then identified and the 12th nerve is preserved. After the lateral bone structures are resected, the odontoid process and the surrounding ligaments are clearly seen. The odontoid process is drilled until the contralateral condyle is identified. In patients with severe odontoid invagination, the jugular bulb must be skeletonized to permit a more superior extension. Complete details of the procedure may be found in the technique described by al-Mefty et al.17
Salas et al.19 described variations of the extreme lateral cranial cervical approach in an anatomic study and clinical analysis of 69 patients. The variations include the transfacet oral approach, the retrocondylar approach, the partial transcondylar approach, the complete transcondylar approach, the extreme lateral transjugular approach, and the transtubercular approach.19,20 These are all variations to allow improved access and exposure to the pathology, depending on the location of the pathology.
Al-Mefty O., Borba L.A., Aoki N., et al. The transcondylar approach to extradural nonneoplastic lesions of the craniovertebral junction. J Neurosurg. 1996;84(1):1-6.
Crockard H.A. Anterior approaches to lesion of the upper cervical spine. Clin Neurosurg. 1988;34:389-416.
Grantham S.A., Dick H.M., Thompson R.C.Jr., Stinchfield F.E. Occipitocervical arthrodesis. Indications, technic and results. Clin Orthop. 1969;65:118-129.
McAfee P.C., Bohlman H.H., Riley L.H.Jr., et al. The anterior retropharyngeal approach to the upper part of the cervical spine. J Bone Joint Surg [Am]. 1987;69:1371-1383.
1. Romanes G.J. Cunningham’s manual of practical anatomy. Head and neck and brain. London: Oxford University Press; 1967.
2. Young J.P., Young P.H., Ackermann M.J., et al. The ponticulus posticus: implications for screw insertion into the first cervical lateral mass. J Bone Joint Surg [Am]. 2005;87(11):2495-2498.
3. Grantham S.A., Dick H.M., Thompson R.C.Jr., Stinchfield F.E. Occipitocervical arthrodesis. Indications, technique, and results. Clin Orthop. 1969;65:118-129.
4. Wertheim S.B., Bohlman H.H. Occipitocervical fusion. Indications, technique, and long-term results in thirteen patients. J Bone Joint Surg [Am]. 1987;69(6):833-836.
5. Clark C.R. Occipitocervical fusion for the unstable rheumatoid neck. Orthopedics. 1989;12:469-473.
6. Crockard H.A. Midline ventral approaches to the craniocervical junction and upper cervical spine. In: Sherk H.H., editor. The cervical spine: an atlas of surgical procedures. Philadelphia: Lippincott; 1994:93-112.
7. Crockard H.A., Calder I., Ransford A. One-stage transoral decompression and posterior fixation in rheumatoid atlantoaxial subluxation. J Bone Joint Surg. 1990;[Br] 72:682-685.
8. Crockard H.A., Pozo J.L., Ransford A.P., et al. Transoral decompression and posterior fusion for rheumatoid atlantoaxial subluxation. J Bone Joint Surg [Br]. 1986;68(3):350-356.
9. Menezes A.H., Traynelis V.C., Gantz B.J. Surgical approaches to the craniovertebral junction. Clin Neurosurg. 1994;41:187-203.
10. Vender J.R., Harrison S.J., McDonnell D.E. Fusion and instrumentation at C1-3 via the high anterior cervical approach. J Neurosurg. 2000;92(Suppl 1):24-29.
11. Whitesides T.E.Jr. Lateral retropharyngeal approach to the upper cervical spine. In TCSR Socitety, editor: The cervical spine. Philadelphia: Lippincott; 1983. 517–527
12. McAfee P.C., Bohlman H.H., Riley L.H.Jr., et al. The anterior retropharyngeal approach to the upper part of the cervical spine. J Bone Joint Surg [Am]. 1987;69:1371-1383.
13. Vishteh A.G., Beals S.P., Joganic E.F., et al. Bilateral sagittal split mandibular osteotomies as an adjunct to the transoral approach to the anterior craniovertebral junction. Technical note. J Neurosurg. 1999;90(Suppl 4):267-270.
14. Crockard H.A. Anterior approaches to lesion of the upper cervical spine. Clin Neurosurg. 1988;34:389-416.
15. Hall J.E., Denis F., Murray J. Exposure of the upper cervical spine for spinal decompression by a mandible and tongue-splitting approach. J Bone Joint Surg [Am]. 1977;59:121-123.
16. James D., Crockard A. Surgical access to the base of skull and upper cervical spine by extended maxillotomy. Neurosurgery. 1991;29:411-416.
17. Al-Mefty O., Borba L.A., Aoki N., et al. The transcondylar approach to extradural nonneoplastic lesions of the craniovertebral junction. J Neurosurg. 1996;84(1):1-6.
18. Bejjani G.K., Sekhar L.N., Riedel C.J. Occipitocervical fusion following the extreme lateral transcondylar approach. Surg Neurol. 2000;54(2):109-115.
19. Salas E., Sekhar L.N., Ziyal I.M., et al. Variations of the extreme-lateral craniocervical approach: anatomical study and clinical analysis of 69 patients. J Neurosurg. 1999;90(Suppl 4):206-219.
20. Ture U., Pami M.N. Extreme lateral-transatlas approach for resection of dens of the axis. J Neurosurg. 2002;96(Suppl 1):73-82.