Chapter 75 Numbness/Saphenous Nerve
Introduction
Leg numbness due to nerve damage is one of the considerable complications after anterior cruciate ligament (ACL) reconstruction using both bone–patellar tendon–bone (BPTB) and medial hamstring tendons. Such patients especially complain of uncomfortable feelings when falling on their knees. Harvesting a BPTB graft includes risks of damaging nerves and causes sensory disturbance.1,2 Pagnani et al3 pointed out the risk of saphenous nerve damage by harvesting medial hamstring tendons in the region of the pes anserinus.
Many authors have reported the nerve distribution patterns of the infrapatellar regions.2,4–12 It is well known that both the medial cutaneous nerve of the femoral nerve and the infrapatellar branch of the saphenous nerve are distributed throughout the infrapatellar region and the anterior lower leg region.9,10,12 The saphenous nerve descends laterally along the femoral artery and enters the adductor canal. It then leaves the artery at the distal end of the canal to proceed vertically along the medial side of the knee and runs between the sartorius and gracilis tendons. In contrast, the medial femoral cutaneous nerve originates from the anterior cutaneous branches of the femoral nerve. The medial femoral cutaneous nerve runs laterally to the femoral artery, and then it crosses anteriorly to the artery at the apex of the femoral triangle to be distributed to the anteromedial thigh and the infrapatellar region. Branches of the medial femoral cutaneous nerve and the infrapatellar branch of the saphenous nerve connect to each other9,10,12 and form the subsartorial plexus in the infrapatellar region.13
Bone–Tendon–Bone Autograft
Anterior knee pain including leg numbness has been reported as a main complication of ACL reconstruction using BPTB grafts. In previous reports, the rate of postoperative anterior knee pain ranged from 4% to more than 40%.8,14,15 Mishra et al at first described a technique using two horizontal incisions for patellar tendon harvest for the purpose of more cosmetic scarring and reducing pain and flexion limitation.16 Kartus et al17 changed to two vertical incisions and reported of an insensitive area compared with the insensitive area that resulted from a traditional vertical incision, which averaged 24 cm. Tsuda et al18 changed the method of approaching the retinaculum layer, opening it horizontally rather than splitting it to protect nerves using two horizontal incisions, and they reported a 17% rate of postoperative leg numbness. Portland et al19 compared a horizontal incision and a vertical incision and reported a infrapatellar numbness of 43% resulting from a horizontal incision and 59% resulting from a horizontal incision.
Hamstring Autograft
The donor site morbidity associated with harvesting a hamstring tendon graft is well recognized to be less common than that associated with harvesting a BPTB autograft.20 However, sensory disturbance is frequently observed in regions on the anterior lower leg after ACL reconstruction using medial hamstring tendons.21,22
Clinical Examination
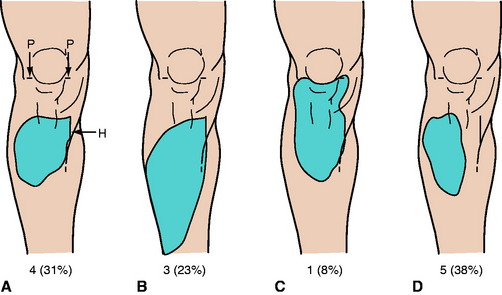
We clinically examined 103 patients who had arthroscopically assisted ACL reconstructions using medial hamstring tendons to investigate the frequencies and areas of sensory disturbance.23 As an operative procedure, we made two horizontal incisions for the arthroscopy portal and one longitudinal incision (2.5–3 cm) at the pes anserinus for the tendon harvest and the tibial drill holes. We performed an inside-out technique and used Endobutton (Smith & Nephew Endoscopy, Andover, MA) for femoral fixation. The clinical examination was performed for an average of 13 months (range 6–18 months) after the operation. We detected sensory disturbance on the anterior surface of the lower leg in 60 of 103 (58%) patients. We randomly selected 13 patients with sensory disturbance and neurologically examined in detail the regions of sensory disturbance. The regions of sensory disturbance were of various sizes and shapes (Fig. 75-1). These regions were generally quadrilateral and located lateral to the longitudinal incision for tendon harvest and distal to the horizontal incisions for the arthroscopy portal. In the detailed neurological examination, in 8 of 13 legs (62%) the region was very close to the longitudinal incision (see Fig. 75-1, A to C), and in the other 5 legs (38%) it was relatively far away from the longitudinal incision (see Fig. 75-1, D). The region was lower than the superior end of the longitudinal incisions in 12 of 13 legs (92%); however, in one leg (8%), the region was close to the horizontal incisions (see Fig. 75-1, C). The region was located in the upper half of the lower leg in 10 legs (77%); however, in three legs (23%), the region was wider than others (see Fig. 75-1, B).
Anatomical Investigations
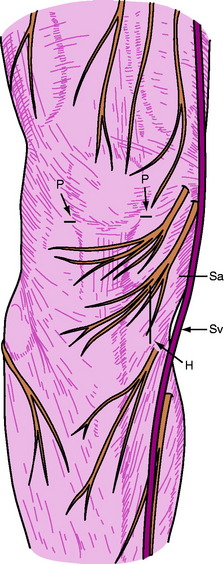
In our anatomical study, 51 lower limbs of 26 adult cadavers were used.24 In the mediodistal region of the patella, the nerve branches pierced the fascia cruris in various patterns and ran on the outer surface of the fascia to supply the skin (Fig. 75-2). On the outer surface of the fascia, the nerve branches often were connected to each other. In the regions near the horizontal and longitudinal skin incision lines, the nerve branches ran on the outer surface of the fascia cruris in all legs.
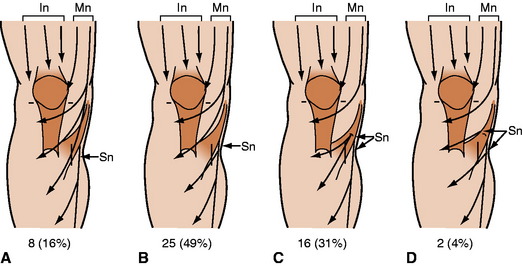
In 33 of 51 legs (65%; Fig. 75-3, A, B), the infrapatellar branch of the saphenous nerve ran along the inferoposterior border of the sartorius muscle. The infrapatellar branch of the saphenous nerve pierced the distal part of the sartorius muscle in 16 of 51 legs (31%; see Fig. 75-3, C). In two legs (4%; see Fig. 75-3, D), the branch of the saphenous nerve emerged from the anterosuperior border of the sartorius muscle and ran lateralward horizontally. The infrapatellar region and the anterior region of the lower leg were generally supplied by branches of both the medial femoral cutaneous nerve and the saphenous nerve in various patterns. Branches of the medial femoral cutaneous nerve were also distributed to the anterior surface of the leg in eight legs (16%; see Fig. 75-3, A), and branches of the saphenous nerve were also observed to supply the infrapatellar region in two legs (4%; see Fig. 75-3, D). Branches of these nerves and their connections were distributed to the region around the insertion of the sartorius muscle. At least, therefore, the branches of these two nerves showed a complementary distribution and a broad transitional zone. One or more branches of the nerve ran across the line of the longitudinal incision in 88% of the cases.
Discussion
In numerous clinical anatomical studies, nerve distribution patterns of the infrapatellar region have been discussed.2,4–8,10,25 The nerve branches supplying the skin of the medioinferior region of the patella are recognized as the infrapatellar branch of the saphenous nerve in most studies. However, according to our study and standard anatomy textbooks,13,16 branches of the saphenous nerve and the medial femoral cutaneous nerve, which originate from the anterior cutaneous branches of the femoral nerve, are distributed to this region. In addition, the branches of the medial femoral cutaneous nerve sometimes extend to the anterior lower leg region. Interestingly, although both nerves are clearly distinguishable in origin, it is very difficult to identify the border between their distribution territories due to their numerous connections because of their complementary distribution.
On the basis of the detailed clinical and anatomical investigations, the sensory disturbance is considered to be closely related to the skin incisions. Nerve injury due to the incisions used for the arthroscopy portal as well as the related anatomical findings have been reported.2,11 In the present clinical findings, the sensory disturbance region was located in close proximity to the arthroscopy portals in only one case (see Fig. 75-1, C). The branch of the medial femoral cutaneous nerve might have been injured by the incisions for the arthroscopy portal. There have been few reports on nerve injuries related to the skin incision for tendon harvest.13 The line of skin incision for tendon harvest at the pes anserinus runs across the nerve branches originating from the medial femoral cutaneous nerve and the saphenous nerve. In some patients, the region of the sensory disturbance is not adjacent to the longitudinal skin incision (see Fig. 75-1, D). These cases might be explained by the various patterns of the connections and the overlapping distribution territories of the saphenous nerve and the medial femoral cutaneous nerve.
The possibility of nerve injury during harvesting of the semitendinosus tendon with a tendon stripper cannot be overlooked. The main trunk of the saphenous nerve runs distally on the medial (outer) surfaces of the tendons of the gracilis and semitendinosus muscles along the medial collateral ligament. Because the sensory disturbance region was located lateral to the longitudinal incision line in all patients, the tendon harvest using a tendon stripper cannot be the main reason for the sensory disturbance. Injury or entrapment of the main trunk of the saphenous nerve has been reported,26,27 but the sensory disturbance region due to such injury is much wider than that found in our study. If the tendon stripper caused the nerve injury, the main trunk of the saphenous nerve could be damaged as well as the branches of the nerve, as previously pointed out by Pagnani.3 Therefore it is very important to be careful of the main trunk of the saphenous nerve due to its close positional relationship to the tendons to avoid sensory disturbance after ACL reconstruction.
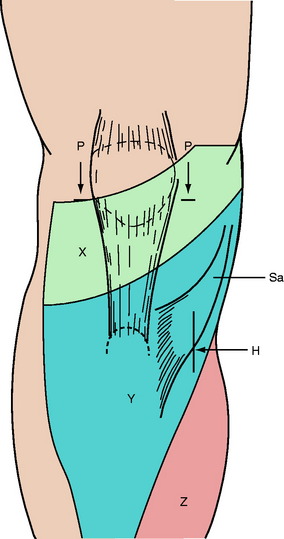
The complicated anatomical variations of the nerve branches in the infrapatellar region and the anterior lower leg region preclude absolute avoidance in any surgical knee incision (Fig. 75-4). Ebrahein and Mekhail6 described a safety zone to avoid injury of the infrapatellar branch of the saphenous nerve. However, their zone must be supplied by the branches of the medial femoral cutaneous nerve. Therefore it might be very difficult to find a completely safe zone based on the findings of the present anatomical study.24 Nevertheless, an oblique incision for the tendon harvest would be a good candidate to minimize the area of the sensory disturbance to avoid cutting the courses of the various branches of the nerves, based on our findings of the nerve courses and distribution.
1 Graf B, Uhr F. Complications of intra-articular anterior cruciate reconstruction. Clin Sports Med. 1988;7:835-848.
2 Mochida H, Kikuchi S. Injury to infrapatellar branch of saphenous nerve in arthroscopic knee surgery. Clin Orthop Relat Res. 1995;320:88-94.
3 Pagnani MJ, Warner JJP, O’Brien SJ, et al. Anatomic considerations in harvesting the semitendinosus and gracilis tendons and a technique of harvest. Am J Sports Med. 1993;21:565-571.
4 Arthornthurasook A, Gaew-Im K. Study of the infrapatellar nerve. Am J Sports Med. 1988;16:57-59.
5 Arthornthurasook A, Gaew-Im K. The sartorial nerve: its relationship to the medial aspect of the knee. Am J Sports Med. 1990;18:41-42.
6 Ebrahein NA, Mekhail AO. The infrapatellar branch of the saphenous nerve: an anatomic study. J Orthop Trauma. 1997;11:195-199.
7 Ganzoni N, Wieland K. The ramus infrapatellaris of the saphenous nerve and its importance for medial parapatellar arthrotomies of the knee. Reconstr Surg Traumat. 1978;16:95-100.
8 Kartus J, Ejerhed L, Eriksson BI, et al. The localization of the infrapatellar nerves in the anterior knee region with special emphasis on central third patellar tendon harvest: a dissection study on cadaver and amputated specimens. Arthroscopy. 1999;15:577-586.
9 Pürner J. [Peripheral course of saphenous nerve.]. Anat Anz. 1971;129:114-132.
10 Sirang H. [Saphenous nerve: origin, course, and branches.]. Anat Anz. 1972;130:158-169.
11 Tifford CD, Spero L, Luke T, et al. The relationship of the infrapatellar branches of the saphenous nerve to arthroscopy portals and incisions for ACL surgery: an anatomic study. Am J Sports Med. 2000;28:562-567.
12 Von Lanz T, Wachsmuth W. Praktische Anatomie. Band I, Teil 4. Bein und Statik. Berlin: Springer-Verlag, 1972;73-89. 292–300
13 Berry MM, Starding SM, Bannister LH. Nervous system. In: Williams PL, Bannister LH, Berry MM, et al, editors. Gray’s anatomy. The anatomical basis of medicine and surgery. ed 38 (Brit). New York: Churchill Livingstone; 1995:1280-1282.
14 Bach BRJr, Jones GT, Sweet FA, et al. Arthroscopy-assisted anterior cruciate ligament reconstruction using patellar tendon substitution: two to four-year follow-up results. Am J Sports Med. 1994;22:758-767.
15 Shelboune KD, Trumper RV. Preventing anterior knee pain after anterior cruciate ligament reconstruction. Am J Sports Med. 1997;25:41-47.
16 Mishra AK, Fanton GS, Dillingham MF, et al. Patellar tendon graft harvesting using horizontal incisions for anterior cruciate ligament reconstruction. Arthroscopy. 1995;11:749-752.
17 Kartus J, Ejerhed L, Sernert N, et al. Comparison of traditional and subcutaneous patellar tendon harvest: a prospective study of donor site-related problems after ACL reconstruction using different graft harvesting techniques. Am J Sports Med. 2000;28:328-335.
18 Tsuda E, Okamura Y, Ishibashi Y, et al. Techniques for reducing anterior knee symptoms after ACL reconstruction using a bone-patellar tendon-bone autograft. Am J Sports Med. 2001;29:450-456.
19 Portland GH, Martin D, Keene G, et al. Injury to the infrapatellar branch of the saphenous nerve in anterior cruciate ligament reconstruction: comparison of horizontal versus vertical harvest site incisions. Arthroscopy. 2005;3:281-285.
20 Corry IS, Webb JM, Clingeleffer AJ, et al. Arthroscopic reconstruction of the anterior cruciate ligament: a comparison of patellar tendon autograft and four-strand hamstring tendon autograft. Am J Sports Med. 1999;27:444-454.
21 Bertnam C, Porsche M, Hackenbroch MH, et al. Saphenous neuralgia after arthroscopically assisted ACL reconstruction with a semitendinosus and gracilis tendon graft. Arthroscopy. 2000;16:763-766.
22 Mochizuki T, Muneta T, Yagishita K, et al. Skin sensory change after arthroscopically-assisted anterior cruciate ligament reconstruction using medial hamstring tendons with a vertical incision. Knee Surg Sports Traumatol Arthrosc. 2004;12:198-202.
23 Mochizuki T, Akita K, Muneta T, et al. Anatomical bases for minimizing sensory disturbance after arthroscopically-assisted anterior cruciate ligament reconstruction using medial hamstring tendons. Surg Radiol Anat. 2003;25:192-199.
24 Clemente CD, editor. Anatomy of the human body. ed 30 (Am). Philadelphia: Lea & Febiger; 1985:1231-1234.
25 Leonhardt H, Tillmann B. Untere Extremität. In: Leonhardt H, Tillmann B, Töndury G, et al, editors. Anatomie des Menschen. Band IV. Topographie der Organsysteme, Systematik der peripheren Leitungsbahnen. Stuttgart: Georg Thieme Verlag; 1988:448-449.
26 Abram LJ, Froimson AI. Saphenous nerve injury. An unusual arthroscopic complication. Am J Sports Med. 1991;19:668-669.
27 Kopell HP, Thompson WAL. Knee pain due to saphenous-nerve entrapment. N Engl J Med. 1960;263:351-353.