Numbness and sensory disturbance
Sensory symptoms are very common, occurring in about 8% of the general population. Sensory symptoms and signs alone may lead to a diagnosis. They can also be very helpful in clarifying the diagnosis in patients with other symptoms and signs. However, sensory symptoms and signs are ‘softer’ than many other neurological symptoms and can occur without an established underlying cause.
Clinical features
What is it?
Sensory symptoms can be broadly divided into:
 positive symptoms: an intrusive feeling of altered sensation, often referred to as numbness, tingling, pins and needles, though sensations may include pain
positive symptoms: an intrusive feeling of altered sensation, often referred to as numbness, tingling, pins and needles, though sensations may include pain negative symptoms: the realization that sensation is lost, usually noticed when the patient inadvertently touches the affected part.
negative symptoms: the realization that sensation is lost, usually noticed when the patient inadvertently touches the affected part.A limb may be described as numb when it is in fact weak, or vice versa.
Where is it?
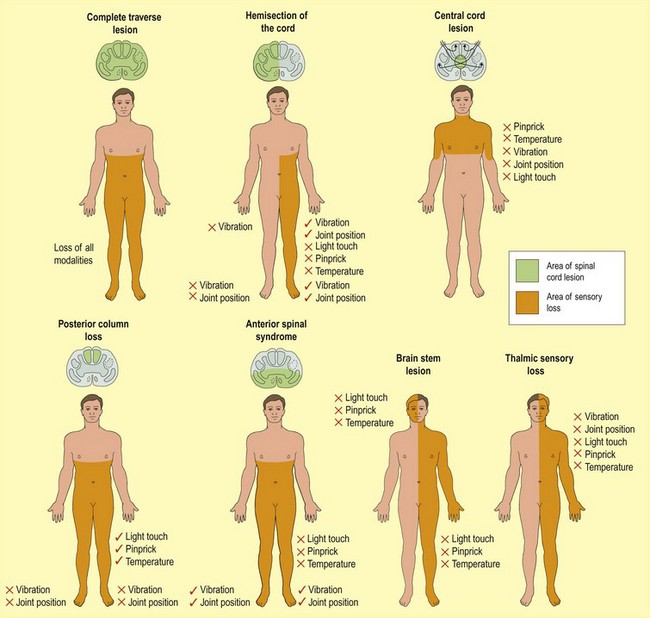
The distribution of the sensory symptoms and signs is important in determining the cause of the symptoms (Fig. 1). The common patterns of sensory symptoms follow the patterns of sensory loss illustrated. However this can be imprecise. For example, patients with carpal tunnel syndrome commonly feel their whole hand is numb, sometimes even the arm. Their feelings of tingling are usually more clearly localized to the hand, though they may be uncertain which fingers are affected. Patients with cervical root compression often describe numbness affecting the whole arm; their tingling however normally is more clearly related to a single root dermatome. In other circumstances, even relatively minor symptoms can be very helpful. For example, a patient with numbness and weakness in both legs with upper motor neurone signs could have a problem at any level of the spinal cord, or possibly brain stem. If they have sensory symptoms or signs in the arms, this indicates the level to be in the cervical cord or above.
How did it come on?
Important clinical features are the timing of the onset and pattern of sensory disturbance.
Transient sensory disturbance
Transient disturbances of sensation can arise from any level in the nervous system:
 Cerebral hemisphere and brain: include migraine, epilepsy, transient ischaemic attacks, and CNS demyelination.
Cerebral hemisphere and brain: include migraine, epilepsy, transient ischaemic attacks, and CNS demyelination.These types of symptoms are also often unexplained or may be psychogenic.
The timing of the onset and its duration, as well as the distribution, helps clarify this (Table 1).
| Condition | Quality and distribution of numbness |
|---|---|
| Focal epileptic seizure | Tingling, spreads down one side of the body in seconds as with the motor ‘Jacksonian march’. There may be other epilepsy symptoms, such as altered awareness and limb jerking |
| Migraine aura | Tingling, builds up over minutes and is unilateral. The area of sensory loss reflects the cortical representation, spreading from one area of cortex to an adjacent area (e.g. lip to arm, to thigh, to foot). There are often other migraine symptoms: visual, headache/nausea |
| Transient ischaemic attack (TIA) | Sudden-onset loss of sensation may be focal or unilateral. It may be associated with other deficits: visual, motor or speech |
| Stroke | Onset as TIA but slower recovery, may have residual signs |
| CNS demyelination | These usually come on over 2–3 days and last 4–5 weeks. In established multiple sclerosis, symptoms may last days, or be brought on by exercise or heat. Commonly in feet or hands but may have any distribution, and may have other symptoms: weakness, sphincter disturbance, with CNS signs |
| Peripheral nerve or root entrapment | A common problem. Symptoms within distribution of nerve or root may fluctuate; may be brought on by specific actions or in particular situations |
| Psychogenic | Fluctuating with variable quality. Other symptoms of anxiety, depression and hyperventilation |