Chapter 26 Notchplasty
Anatomy
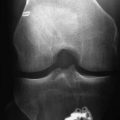
The subtle anatomy of the intercondylar notch in three dimensions plays an important role in the incidence of ACL injuries as well as in optimizing surgical techniques of notchplasty and the ultimate outcome of reconstructions. Several investigators1–5 have shown that a small notch width or a small notch width index (notch width divided by condylar width) is directly correlated to increased risk of ACL injuries, especially in women (Fig. 26-1). A debate has surfaced that it is not a small notch width alone that leads to an increased risk of injury but rather a smaller ligament within the notch that may play a role. Shelbourne et al6 showed when reconstruction is performed with the same size of graft, regardless of notch width or gender, the success rates were similar. Anderson et al7 compared magnetic resonance imaging (MRI) of groups of male and female basketball players and found smaller ligaments in the female athletes as well as differences in notch width. Charlton et al8 found gender variations in both notch width and ACL volume in the groups they compared. Regardless of the debate, it is clear that radiographic findings of a small notch is predictive of ACL injury. In addition, the shape of the notch on an anteroposterior (AP) notch view may also play a role regarding ACL injury risk, with an A-framed notch being relatively more stenotic and leading to increased risk of injury compared with a wider and forgiving inverted U-shaped notch. It should be emphasized that no one is currently promoting prophylactic notchplasty in athletes with an intact ACL who incidentally have been found to have a small notch.
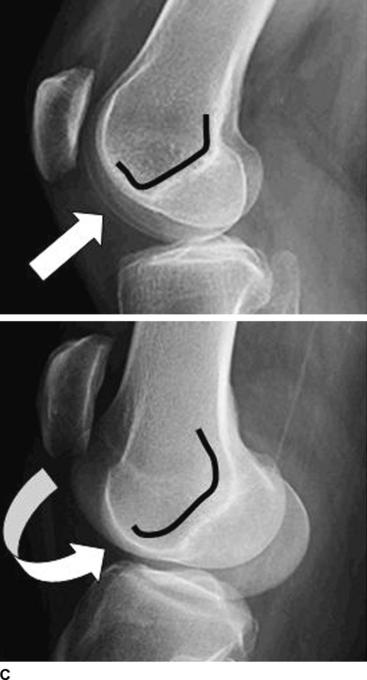
While the AP perspective is clearly important when evaluating the intercondylar notch, the lateral perspective may be as or more important for preoperative planning. On a lateral radiograph, Blumensaat’s line represents the roof of the intercondylar notch. The slope (angular orientation relative to the femur), position (anterior/posterior translational position relative to the central axis of the femur), and trueness (absolutely straight or curved at the ends) are highly variable among patients (Fig. 26-2). Numerous authors have demonstrated an increased risk of ACL reconstruction failure or postoperative extension loss if graft roof impingement is apparent on the lateral perspective.9,10 Howell et al10–13 have been instrumental in increasing the surgical community’s awareness of the importance of identifying potential graft roof impingement preoperatively to guide either tunnel placement or the extent of notchplasty intraoperatively. A preoperative lateral radiograph should be routinely obtained in full extension. If the slope of the roof of the notch is acute or its relative position is too posterior, either the tibial tunnel should be placed more posteriorly to avoid impingement14–16 or an aggressive roofplasty needs to be performed.16,17 Failure to recognize this impingement will lead to an increased risk of graft failure.
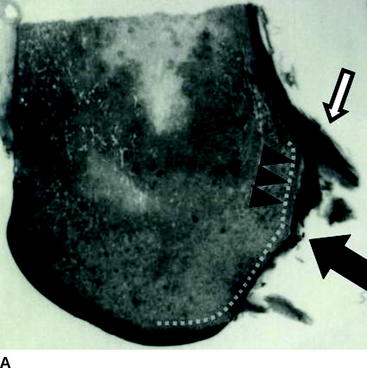
Review of the preoperative lateral radiograph should also assess the trueness of Blumensaat’s line. Is it a straight line from front to back with sharp corners or edges at the inlet and outlet of the notch, or is it rounded at the ends with bumps or curves in the middle that may affect femoral tunnel selection? The roof of the notch is rarely perfectly flat; it usually has a slight curve at the inlet (anterior aspect of the notch) and the outlet (the over-the-back) position. Anteriorly, the gentle transitioning curve or blending of the femoral groove and femoral condyles into the articular surface prevents a sharp edge or corner cutting into the anterior aspect of the ACL in full extension. Posteriorly within the notch, a change in slope occurs approximately 1 cm anterior to the true over-the-back position. This change of slope is usually located at the anterior edge of the leading aspect of the ACL insertion onto the lateral femoral condyle and has been termed the “resident’s ridge” by Clancy18 (Fig. 26-3). Preoperative or intraoperative awareness of the resident’s ridge is essential for optimal placement of the femoral tunnel and successful outcome of the reconstruction. If the change of slope is acute and mistaken for the true over-the-back position, the femoral tunnel will be placed too far anteriorly and lead to one of the most common causes of failure for ACL reconstructions. At the time of notchplasty, a prominent resident’s ridge should be taken down with a bur or osteotome to confirm optimal placement of the femoral tunnel guide and ensure proper positioning of the femoral tunnel. Finally, the true outlet of the notch or over-the-back position on the femur is frequently gently curved, making it difficult to lock in the extended tongues of the femoral guides designed to offset the tunnel position relative to the posterior cortex. This edge may need to be flattened or a preliminary concavity created at the site of the femoral tunnel to allow the guide to be properly seated.
Indications and Potential Risks
Historically, more aggressive notchplasties were necessary to avoid roof impingement due to the relatively anteriorly placed tibial tunnels based on the original description of reconstruction by Clancy.19 Over time, aggressive notchplasties for routine ACL reconstructions have become less commonplace in favor of tibial tunnels placed onto the posterior edge of the tibial ACL footprint, which allows for less risk of impingement and minimal notchplasty. In these cases notchplasty is performed primarily to optimize visualization of the femoral tunnel placement. Devices have been developed to base the tibial tunnel off the notch roof, virtually guaranteeing the absence of impingement in full extension and potentially obviating the need for any notchplasty at all.20
In addition to primary or revision ACL reconstruction in which notchplasty is performed as an adjunct to the procedure, notchplasty may be indicated as the primary procedure itself. As noted previously, no one is currently recommending prophylactic notchplasties to reduce the risk of ACL injuries; however, in patients who have postoperative extension loss or arthrofibrosis, notchplasty may be the procedure of choice. Shelbourne and Johnson21 performed arthroscopic débridement of scar tissue and manipulation under anesthesia with notchplasty in this population with good success in regaining motion in selected patients. Clearly, prevention is the best treatment, and initial adequate notchplasty may help prevent future extension loss. Tonino et al and Millet et al in separate papers22,23 agree that inadequate notchplasty or space available for the ACL graft at the time of initial surgery was a common cause of arthrofibrosis, and adequate notchplasty might have prevented the complication.
One might argue that notchplasty is a benign procedure and therefore an aggressive notchplasty is indicated in everyone. This may not be true. LaPrade et al24 found that aggressive notchplasty, in a canine model, led to early degenerative changes in the patellofemoral joint. Jarvela et al25 correlated their clinical findings of postoperative patellofemoral arthritis 7 years after ACL reconstruction with a large notchplasty. In contrast, Morgan et al26 failed to show abnormal pressure changes (in vitro using pressure-sensitive film) on the patellofemoral joint after notchplasty. Another potential risk of aggressive notchplasty is alteration of the biomechanical effects of the ACL reconstruction itself. Markolf et al27 showed increased graft forces, particularly with the knee flexed at 90 degrees after notchplasty, and surmised that this could lead to an increased risk of graft failure. Anatomically, the ACL is meant to fill the notch and lie gently on the roof of the notch in full extension. This serves as an added buttress versus anterior displacement in addition to the tension along the fibers of the ligament itself. With aggressive notchplasty, this normal relationship may not occur.
Techniques and Avoiding Complications
Preoperative planning continues to play an important role when considering the necessity and extent of notchplasty. Preoperative notch and lateral radiographs may reveal relative notch stenosis, spurs, or osteophytic overgrowth.28 These can be related to gender, genetics, degeneration, or the chronicity of the ACL injury. Nonetheless, when recognized preoperatively, it allows the surgeon to be more aggressive at the time of surgery to ensure the postoperative notch will be adequate to house the new ligament without impingement. When preoperatively evaluating the lateral view, it is very important to obtain the image with the knee in full extension, which allows careful interpretation of the slope and relative anterior/posterior position of the roof of the notch. This interpretation may indicate either a more aggressive notchplasty or the need to move the tibial tunnel more posteriorly to avoid notch roof impingement.
The notchplasty itself can be performed either arthroscopically or via a mini-open incision. The two primary goals are (1) to avoid impingement and graft irritation and (2) to optimize visualization for femoral tunnel placement. With the advent of central tibial tunnel placement 7 to 10 mm anterior to the PCL, it is rarely necessary to perform an aggressive notchplasty to avoid graft impingement. Proper tibial tunnel placement obviates impingement unless secondary osteophytic overgrowth has occurred due to chronicity of injury. For nonchronic reconstructions, the most important goal is adequate visualization for placement of the femoral tunnel, avoiding mistaking the resident’s ridge for the real over-the-back position, and careful visualization of the posterior cortex of the femoral condyle. Currently, we use only a minimal notchplasty in virtually all of our primary reconstructions.
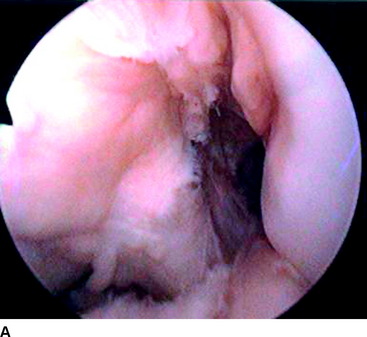
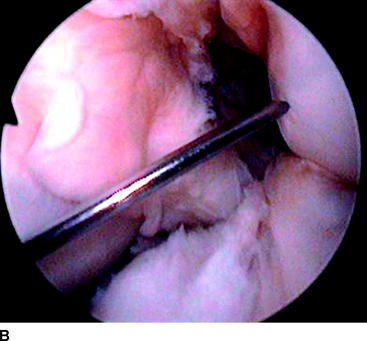
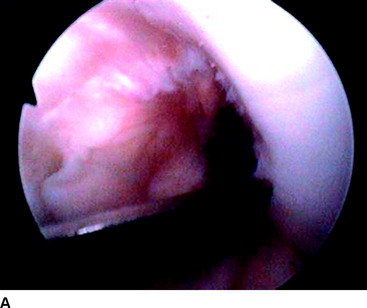
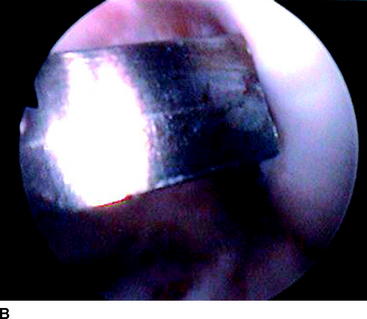
Bony notchplasty usually begins anteriorly and progresses posteriorly. Arthroscopically, a subtle pink color change can be visualized at the entrance of the femoral notch where the articular surface of the lateral femoral condyle thins and curves acutely into the surface of the wall of the notch (Fig. 26-4). This subtle change is usually about 1 to 2 mm onto the articular surface and marks our initial site of anterior notchplasty. This edge can be taken down with a small osteotome or a high-speed bur/shaver (Fig. 26-5). Once the leading edge is removed, the high-speed bur/shaver is used to flatten the remaining wall to the same depth in a front-to-back direction. The goal is to create a smooth flat surface that does not irritate the graft and allows direct visualization to the posterior outlet (over-the-back position) of the notch. In general, the extent of this minimal notchplasty is effective for visualization of the over-the-back position in most patients.
Approximately, two-thirds to three-quarters of the way back, the bur frequently becomes more erratic and is difficult to maintain on the surface of the wall of the notch. This is due to a change in slope that occurs within the notch and a change in density of the bone itself. This is the resident’s ridge.18 The change in slope occurs immediately anterior to the ACL insertion onto the femur. The erratic nature of the bur is secondary to the increased cortical thickness of the ACL insertion itself. The resident’s ridge should be carefully flattened with the bur to match the entire flat surface of the wall of the notch. This will allow excellent visualization of the true over-the-back position on the femur and allow optimal placement of the femoral over-the-back guide. Indeed, at the time of notchplasty, we will usually make a small “prehole” or concavity where we expect the tunnel placement to be. This allows the over-the-back guide to slide more securely in place over the back of the lateral femoral condyle. It should be noted that leaving the cortical edge on the most posterior aspect of the notch is important during notchplasty and guide placement. Notchplasty that is too aggressive on the posterior wall of the notch can make proper positioning of the over-the-back guide difficult.
Technically, the surgeon must work stepwise from known to unknown and from front to back in the notch. Débridement of soft tissue is usually straightforward; however, care must be taken to avoid viable anatomical structures including previous reconstructed ligaments. If a Cyclops lesion is present (scar tissue anteriorly in the notch, frequently with an adherent fat pad), flexing and extending the knee under arthroscopic visualization may help to identify the ACL so that the surgeon can target the scar tissue itself. In some cases it may be necessary to remove even the reconstructed ligament to regain full extension. Fortunately, débridement and notchplasty in post-ACL patients with arthrofibrosis are usually successful in regaining motion and normal gait as well as returning to athletic activities.29,30 In patients with significant bony overgrowth, the surgeon should begin by carefully taking down obvious osteophytes under direct visualization and then working posteriorly. Osteophytes are usually softer than the native bone and are removed easier by the bur/shaver. In revision cases in which osteophytes may be present posteriorly, we recommend obtaining intraoperative radiographs to confirm femoral tunnel placement prior to drilling to ensure optimal position.
1 Souryal TO, Moore HA, Evans JP. Bilaterality in anterior cruciate ligament injuries in athletes: associated with intercondylar notch stenosis. Am J Sports Med. 1988;16:449-454.
2 Souryal TO, Freeman TR. Intercondylar notch size and anterior cruciate ligament injuries in athletes: a prospective study. Am J Sports Med. 1993;21:535-539.
3 Schickendantz MS, Weiker GG. The predictive value of radiographs in the evaluation of unilateral and bilateral anterior cruciate ligament injuries. Am J Sports Med. 1993;21:110-113.
4 LaPrade RF, Burnett QM. Femoral intercondylar notch stenosis and correlation to anterior cruciate ligament injuries: a prospective study. Am J Sports Med. 1994;22:198-203.
5 Houseworth SW, Mauro VJ, Mellon BA, et al. The intercondylar notch in acute tears of the anterior cruciate ligament: a computer graphics study. Am J Sports Med. 1987;15:221-224.
6 Shelbourne KD, Davis TT, Klootwyck TE. The relationship between intercondylar notch width of the femur and the incidence of anterior cruciate ligament tears: a prospective study. Am J Sports Med. 1998;26:402-408.
7 Anderson AF, Dome DC, Gautam S, et al. Correlation of anthropometric measurements, strength, anterior cruciate ligament size, and intercondylar notch characteristics to sex differences in ACL tear rates. Am J Sports Med. 2001;29:58-66.
8 Charlton WPH, St John TA, Ciccotti MG, et al. Differences in femoral notch anatomy between men and women: a magnetic resonance imaging study. Am J Sports Med. 2002;30:329-333.
9 Feagin JA, Cabaud HD, Curl WW. The anterior cruciate ligament: radiographic and clinical signs of successful and unsuccessful repairs. Clin Orthop. 1982;164:54-58.
10 Howell SM, Taylor MA. Failure of reconstruction of the anterior cruciate ligament due to impingement by the intercondylar roof. J Bone Joint Surg. 1993;75A:1044-1055.
11 Howell SM. Arthroscopic roofplasty: a method for correcting extension deficit caused by roof impingement of an anterior cruciate ligament graft. Arthroscopy. 1992;8:375-379.
12 Howell SM, Barad SJ. Knee extension and its relationship to the slope of the intercondylar notch. Implications for positioning the tibial tunnel in anterior cruciate ligament reconstructions. Am J Sports Med. 1995;23:288-294.
13 Howell SM, Gittins ME, Gottlieb JE, et al. The relationship between the angle of the tibial tunnel in the coronal plane and loss of flexion and anterior laxity after ACL reconstruction. Am J Sports Med. 2001;29:567-574.
14 Miller MD, Olszewski AD. Posterior tibial tunnel placement to avoid anterior cruciate ligament graft impingement: an in-vitro and in-vivo study. Am J Sports Med. 1997;25:818-822.
15 Morgan CD, Kalman VR, Grawl DM. Definitive landmarks for reproducible tibial tunnel placement in anterior cruciate ligament reconstruction. Arthroscopy. 1995;11:275-288.
16 Berns GS, Howell SM. Roofplasty requirements in vitro for different tibial hole placements in anterior cruciate ligament reconstruction. Am J Sports Med. 1993;21:292-298.
17 Tanzere M, Lenczner E. The relationship of intercondylar notch size and content to notchplasty requirement in anterior cruciate ligament surgery. Arthroscopy. 1990;6:89-93.
18 Hutchinson MR, Ash SA. Resident’s ridge: assessing the cortical thickness of the lateral wall and roof of the intercondylar notch. Arthroscopy. 2003;19:931-935.
19 Clancy WG, Nelson DA, Reider B, et al. Anterior cruciate ligament reconstruction using one-third of the patellar ligament, augmented by extra-articular tendon transfers. J Bone Joint Surg. 1982;64A:352-359.
20 Howell SM, Lawhorn KW. Gravity reduces the tibia when using a tibial guide that targets the intercondylar roof. Am J Sports Med. 2004;32:1702-1710.
21 Shelbourne KD, Johnson GE. Outpatient surgical management of arthrofibrosis after ACL surgery. Am J Sports Med. 1994;22:192-197.
22 Tonino P, Risinger RJ, Garcia M, et al. Arthrofibrosis following ACL reconstruction. In: Freedman KM, editor. Complications in orthopaedics: ACL surgery. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2005:35-40.
23 Millet PJ, Wickiewicz TL, Warren RF. Motion loss after ligament injuries to the knee. Part 1: causes. Am J Sports Med. 2001;29:664-675.
24 LaPrade RF, Terry GC, Montgomery RD, et al. The effects of aggressive notchplasty on the normal knee in dogs. Am J Sports Med. 1998;26:193-200.
25 Jarvela T, Paakkala T, Kannus P, et al. The incidence of patellofemoral osteoarthritis and associated findings 7 years after ACL reconstruction using bone-patellar tendon-bone autograft. Am J Sports Med. 2001;29:18-24.
26 Morgan EA, McElroy JJ, DesJardins JD, et al. The effect of intercondylar notchplasty on the patellofemoral articulation. Am J Sports Med. 1996;24:843-846.
27 Markolf KL, Hame SL, Hunter M, et al. Biomechanical effects of femoral notchplasty in anterior cruciate reconstruction. Am J Sports Med. 2002;30:83-89.
28 Miller MD, Olszewski AD. The appearance of roofplasties on lateral hyperextension radiographs. Am J Sports Med. 1999;27:513-516.
29 Shelbourne KD, Johnson GE. Outpatient surgical management of arthrofibrosis after ACL surgery. Am J Sports Med. 2006;22:192-197.
30 Watanabe BM, Howell SM. Arthroscopic findings associated with roof impingement of an anterior cruciate ligament graft. Am J Sports Med. 1995;23:616-625.