CHAPTER 26 Nonunion of the Olecranon and Proximal Ulna
GENERAL CONSIDERATIONS
Nonunion of olecranon and proximal ulna fractures is a relatively uncommon complication with the use of current techniques of osteosynthesis.9,35,59 Although this problem is perhaps less common today than in the past, it continues to challenge the orthopedic surgeon. Olecranon and proximal ulna fracture nonunion can result in profound functional disability. Patients consistently report pain.55 Other features typically include some degree of instability or limitation of elbow joint motion.
The main predisposing factors for a nonunion of the proximal ulna are inadequate fixation, premature motion, smoking,7 or a combination of all of these.3,4,20,31,32,37,45,63,73,75
INCIDENCE
Nonunion of fractures of the proximal ulna and olecranon has been reported to occur in 5% of all olecranon fractures44 and about 5% of all nonunions.10,11,22 Within a 10-year period (1980 to 1990), 196 olecranon fractures were treated at the Mayo Clinic, and there were only two instances of olecranon nonunion (1%).55
Nonunion is also a recognized complication of the proximal osteotomy of the olecranon to expose a fracture of the distal humerus.70 From 1980 to 1990 at the Mayo Clinic, this complication occurred in only one such patient.55 Other authors have reported a high rate of olecranon nonunion in these patients. Gainor and coworkers30 studied 10 patients who had a transverse osteotomy of the olecranon for surgical exposure of a complex distal humerus fracture. Nine of the osteotomies were reconstructed with a large lag screw and tension band wire, and one with smooth pins and a tension band wire. Within an average follow-up period of 24 months, nonunion of the olecranon osteotomy occurred in three of the patients.30
DIAGNOSIS
A definitive clinical diagnosis of nonunion cannot be determined until a pseudoarthrosis is evident radiographically. Six months is usually the minimum accepted time before a definite diagnosis of nonunion may be considered. A slow union is an indolent union that maintains the radiographic appearance of the early stages of a healing fracture; the fracture line is visible, and no decalcification or sclerosis is present at the bone ends.44 Delayed union is described as fracture healing in which evidence of attempted union is present radiographically. Reactive hyperemia, early resorption of bone ends, and some widening of the fracture site are usually associated with delayed union.
Nonunion is assumed when all evidence of bone healing has ceased. The bone ends and medullary canals are capped, the endosteal blood supply does not extend across the fracture site, and sclerosis of the bone ends is present in at least 25% of patients.32,34 False motion and a varying radiographic defect between the bone ends also are usually present. If a visible fracture line is not present on the plain radiographs, a tomogram is helpful.
CLINICAL PRESENTATION
The term “nonunion,” although describing the pathologic condition, misrepresents the clinical problem. The integrity of the ulna plays an important role not only in the function of the joint but also in the articular surfaces and elbow stability. Clinically, tenderness is consistently reported. Some degree of instability and limitation of motion are the other clinical features of the olecranon nonunion.55 Yet it is important to note that a small percentage of patients may function well with the nonunited fracture.38
CAUSES
Ossification in the olecranon begins at two or more centers, and the growing epiphysis may be misinterpreted or confused radiographically with a fracture line or nonunion.62,66 Olecranon nonunion rarely occurs in children, but it may result when displaced fractures are unrecognized or when inadequate internal fixation results in loss of reduction.43,53
Bilateral congenital pseudoarthrosis of the olecranon has been reported with radiographic features distinct from the kind of congenital pseudoarthrosis of the forearm previously reported.16 A vascularized fibular graft has been reported as successful in this circumstance.2 Nonunion of the olecranon has been reported in an infant following a birth injury and in adolescent stress fractures.39,40,67,75,76 Fracture separation of a nonunited ossification center in three adults has been reported.38 Primary bone grafting is recommended in these cases because of the high incidence of fibrous nonunion following simple open reduction and internal fixation.38
Walker71 reported a case of painful unilateral physeal nonunion in an adult weight lifter. After failure of conservative treatment, surgical union was achieved, using tension band wiring augmented with autologous iliac crest bone graft. Unilateral olecranon physeal nonunion may have a mechanical etiology as opposed to a genetic etiology in individuals with bilateral physeal persistence.54 These types of fractures heal reliably with fixation.52
Generally children have a higher rate of periosteal response and union. Fracture healing in the older age group of patients is good despite the fact that their fractures tend to heal at a slower rate than those in the younger patient.11 Fracture healing may be slowed in the diabetic patient, in the patient undergoing irradiation treatment,21,33,60 in the adult with a stress fracture,51,52,54 or as a result of smoking.17
There are several predisposing factors to nonunion of olecranon fractures: (1) inadequate fixation or immobilization,23,74 (2) distraction, (3) compounding of fracture, (4) infection, (5) comminution,64,69 (6) loss of blood supply,14 (7) defects between the fragments or interposition of soft tissue, (8) abnormalities of the electro-chemical or cellular physiologic mechanisms involved in fracture healing resulting from smoking (Box 26-1),1,3,8,14,17,44,66 and (9) adverse events associated with total elbow replacement.42
BOX 26-1 Causes or Predisposing Factors Contributing to Nonunion of the Olecranon
Inadequate, nonrigid internal fixation
Defects between bone fragments
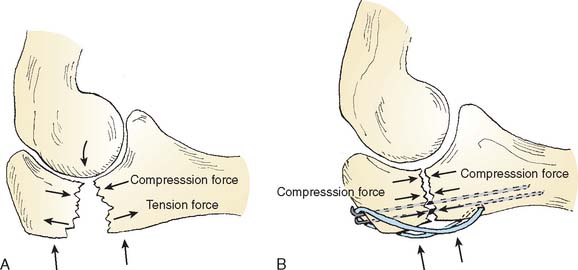
Technically, the most important factor in the treatment of either fresh fractures or nonunion of the olecranon is the need to convert the tensile forces arising from the forearm flexors and the triceps acting across the fracture or the nonunion site to a compressive force (Fig. 26-1).18,64 In tissue culture experiments, Bassett5,6 has shown that tension forces may prevent osseous precursors from forming cartilage or bone to promote the growth of fibrous tissue. Tension forces tend to produce an osteoclast-induced positive electrical potential that may interfere with bone healing. Compression forces, on the other hand, tend to effect an osteoblast-induced negative electrical potential that produces an enhancing effect on fracture healing.7,8,44
CLASSIFICATION
Generally, nonunions have been pathologically classified into two types, according to the biologic activity at the ends of the fracture fragments.36,50 The hypervascular type of nonunion has rich blood supply at the ends of the fragments and may be confirmed by increased technetium Tc-99m uptake. The avascular type has nonviable ends of the fracture fragments and also may be confirmed by a decreased technetium Tc-99m uptake.36,49,72
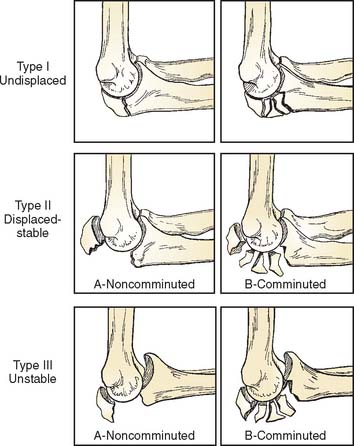
Nonunion of the proximal ulna distal to the insertion of the medial collateral ligament carries a better prognosis for reconstruction because the articular surface of the trochlear notch is intact.4,47,60 Any reconstruction for nonunion in an unstable injury at this level (Fig. 26-2) may need medial collateral ligament repair or reconstitution in addition to rigid internal fixation.47
TREATMENT OPTIONS FOR OLECRANON NONUNION
INDICATIONS
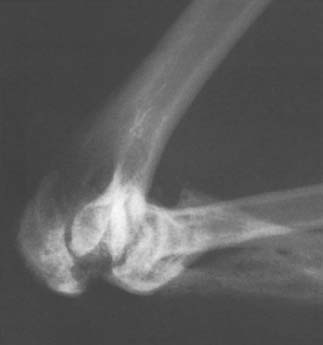
Asymptomatic nonunion with adequate elbow joint function requires no active treatment (Fig. 26-3). For symptomatic olecranon nonunion, the goals of treatment are the same as those of primary treatment for any displaced fracture: (1) to restore congruity of the sigmoid notch, (2) to restore or retain ligamentous stability, (3) to restore triceps extensor function, and (4) to restore mobility of the joint.
Nonunion of Monteggia fracture-dislocations requires special considerations.
Treatment of Infected Nonunion of the Olecranon
Muscle, myocutaneous, and vascularized fibular bone grafts have been used successfully in the treatment of nonunions.25 Successful use of a flexor carpi ulnaris local muscle flap has been reported by Meals46 and avoids the complications associated with microvascular repairs. The use of an external fixator or distraction arthroplasty is usually the most effective means of immobilization until soft tissue coverage and control of the infection can be achieved.
Treatment of Nonunion in Which Articular Cartilage Has Not Been Severely Damaged
Electrical Stimulation
If there is minimal displacement and if the overall alignment is acceptable, consideration might be given to electrical stimulation.7,8,13,56,61 A healing effect of electrical stimulation has been noted with coexisting low-grade infections. This noninvasive method can be used on an outpatient basis. However, the expense and the need to immobilize the joint have caused electrical stimulation to lose favor in recent years. The authors believe electrical stimulation is not a viable treatment option for olecranon or proximal ulna nonunions because of prolonged immobilization of the elbow joint, which is often already compromised by injury and which can lead to elbow stiffness.
Biologic Enhancement
The introduction of bone morphogenic protein (BMP-7) has been demonstrated to facilitate healing at several anatomic sites, including the olecranon region.26 Most heal within 4 to 5 months. This basic strategy is effective because the technology is becoming more refined, resulting in efficient delivery systems of effective product.
Excision
Encouraging early descriptions of the results of proximal fragment excision are available.22,27,29 In 1947, McKeever and Buck reported that 80% of the sigmoid notch could be excised without producing instability of the elbow joint (Fig. 26-4).45 Gartsman and colleagues31 found that restoration of elbow extensor function was equal after excision or fixation, as measured by static and dynamic strength testing. Excision of the proximal fragment with meticulous reattachment of the triceps tendon is an excellent option for treatment of an older patient with nonunion of a small avulsion fragment or a fragment involving less than 50% of the olecranon surface.31,37,45,47,73 Excision of nonunited fracture fragments is, of course, contraindicated in the growing child with an open proximal epiphysis.
TECHNICAL OPTIONS AND CONSIDERATIONS
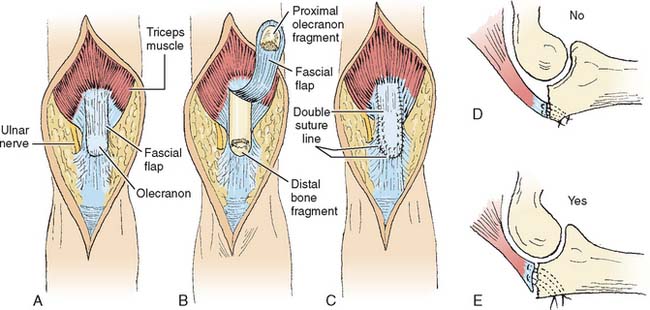
Excision
Small avulsion fragments are uncommon. Best results are obtained by simple excision and meticulous repair or advancement of the triceps tendon to the olecranon. Care must be taken to repair the medial and lateral retinacular portions of the triceps tendon using nonabsorbable suture material. Stay sutures should be placed directly through drill holes extending through the posterior cortex of the distal olecranon fragment (Fig. 26-5). The tendon margin is placed adjacent to the articular surface rather than to the posterior cortex. This improves the stability at the expense of a slightly decreased lever arm. Early active motion is permitted and encouraged 5 days after surgery through a range of 0 to 90 degrees, but flexion beyond 90 degrees should not be permitted for 4 to 6 weeks, depending on the extent of tendon advancement.
Osteosynthesis
Clearly, in a younger patient or in the older individual with a nonunion involving more than 50% of the sigmoid notch, osteosynthesis is the preferred treatment.64 There are three requirements for a successful outcome: ulnohumeral reduction, rigid fixation, and augmentation of healing, that is, bone graft and possibly BMP-7. Rigid fixation can be provided by different techniques, depending on the fracture type. Intramedullary screws, low-profile dynamic compression plates (DCP), or locking olecranon plates each have their place. We have relied on a corticocancellous bone plate fixed with cortical screws to augment the healing response.55 Other than this, the technique for osteosynthesis depends on the characteristics of the fracture. The more frequently used techniques are discussed in the following sections.
Tension Band Wiring
Fixation by a tension band wiring technique coupled with bone grafting is an effective technique for treating undisplaced nonunions (Fig. 26-6).55,74 If tension band wiring is to be used for nonunion in which central portions of the sigmoid notch are missing, pin fixation should be avoided, but if it is used, it should always be placed toward the posterior rather than the articular side of the proximal ulna. This will allow more compression toward the posterior surface, and it tends to prevent narrowing of the notch. When compression is placed close to the articular surface, narrowing of the sigmoid notch may result in subsequent arthritic changes. Comminuted or unstable fragments with anterior subluxation or instability warrant consideration of other treatment options discussed below.
Plating
Plating with a six-hole plate is useful in instances of oblique or transverse olecranon fracture nonunions. Rigid fixation can be achieved by the use of a tubular DCP or a 3.5-mm AO plate. The recent anatomic plates specifically designed and contoured to fit the olecranon repair are particularly useful. These in-clude the LCP AO plate and the Mayo clinic congruent olecranon plate (Acumed, Hillsboro, OR). In any instance, motion should be started immediately. For nonunion of the Monteggia fracture, the ulna should be rigidly fixed with plating and bone grafting. In chronic states, no attempt is made to reduce the dislocation and the radial head is resected (Fig. 26-7).
Plating may be the only available method of salvaging nonunion of comminuted fractures and achieving rigid stability in unstable fractures that involve the coronoid process with rupture of the medial collateral ligament.69 Anatomic visualization and reconstitution of the joint surface is mandatory. Sufficient bone must be removed to regain not only normal alignment of the olecranon itself but also an adequate contour of the joint surface of the ulna articulating with the trochlea. Repair or reconstruction of the lateral collateral ligament should always be carried out and the medial collateral liga-ment should be addressed if instability persists at the operating table.68 A curve at the end of a tubular plate by design or introduced at the time of surgery can enhance fixation of a proximal fragment.24,58
Lag Screw Fixation
Lag screw fixation with a longitudinal intramedullary screw (AO cancellous lag screw) may be used, but bicortical screw fixation provides better fixation if the nonunion is amenable to this.70 Biomechanical studies by Murphy and associates51 have demonstrated that a lag screw combined with tension band wiring has the greater strength of fixation when compared with tension band wiring with Kirschner wires, lag screws alone, or figure-of-eight wiring alone. In the recent Mayo Clinic series, eight patients had a successful intramedullary screw fixation for olecranon nonunion.55 This type of fixation is viable only for single fragment transverse or oblique nonunions of the olecranon or proximal ulna in which axial compression will effectively stabilize the fracture and not narrow the olecranon-to-coronoid distance. Sufficient length to engage the metaphysis of the ulna adequately and overdrilling of the proximal fragment to achieve compression are required (Fig. 26-8).
Nonunion of an oblique or transverse fracture is well suited to bicortical screw fixation, which was described first in 1969 by Taylor and Scham and later reported by Wadsworth in 1976; this is still a reasonable strategy and involves the use of a washer beneath the screw head.65,70
Bone Grafting
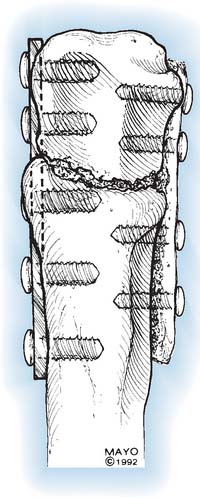
A corticocancellous bone graft fixed with screws is a particularly useful technique.55 Supplementary intramedullary screw fixation is also particularly useful (Figs. 26-9 and 26-10). We and others58 have used this bone grafting in combination with screw-and-plate rigid fixation (Fig. 26-11).
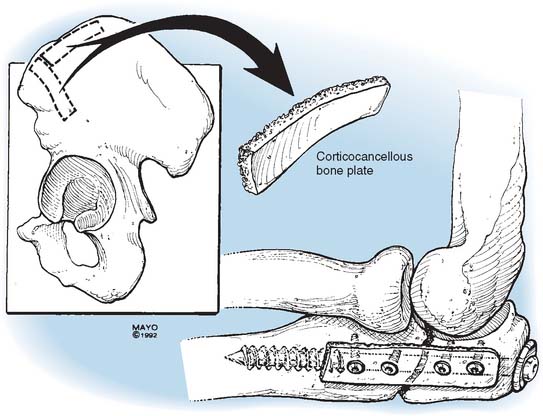
Technical Considerations: Corticocancellous Bone Plate.
A midline incision over the posterior aspect of the elbow is used or the prior incision is re-entered if possible.55 Dissection exposes the proximal ulna. The medial and lateral aspects of the olecranon are identified, and the nonunion site is exposed. The ulnar nerve is identified, dissected, and protected as needed. The surfaces of the proximal ulna both medially and laterally are flattened by removing prominent callus, and the nonunion is entered. The pseudoarthrosis is removed to allow adequate bone grafting. A corticocancellous bone plate, measuring about 60 by 10 mm, is then harvested from the anterior iliac crest (Fig. 26-12). This is carefully placed over the radial aspect of the olecranon and ulna, and is secured with one or two 2.7-mm mini cortical screws on either side of the nonunion.
If a large proximal fragment is present, either a spongiosa (cancellous) intramedullary screw (see Fig. 26-12) or a contoured DCP plate placed over the medial ulna cortex is used (Fig. 26-13). Great care is taken to avoid narrowing the coronoid and olecranon distance. Cancellous bone graft is packed around the nonunion site.
Treatment of Nonunions of the Olecranon when Articular Cartilage Has Been Severely Damaged
This problem calls for an entirely different approach from any described previously. If the olecranon nonunion is an isolated problem and if the humeroulnar articular surface is destroyed beyond restoration from recent or old trauma, the factors of pain, malalignment, infection, age, and instability become important.57 A salvage situation often precludes lesser procedures and arthrodesis, total joint replacement, and allograft replacement may be considered.
Distraction Arthroplasty
In cases of nonunion of the olecranon with severe articular destruction, union must be initially achieved before the question of mobilization can be addressed. If imaging shows evidence of articular incongruity and if attempts at mobilization with dynamic splinting and active exercise are unsuccessful, distraction arthroplasty may be a reasonable and possibly the final treatment option (Fig. 26-14).
The concept of distraction arthroplasty has been used since the mid-1980s for treating the stiff elbow and has been adapted for the treatment of the olecranon nonunion. Thus, in those patients in whom there is contracture of soft tissue around the olecranon nonunion, the distraction device is an ideal adjunct because this may be combined with soft tissue release.48
The specific technique is well described in Chapter 33. In the initial Mayo series,55 four patients were managed by distraction arthroplasty combined with internal fixation and bone grafting of the olecranon nonunion. In all four patients, union was achieved and the arc of motion improved from a mean of 48 degrees to a mean of 95 degrees.
Arthrodesis
When stressful use of the elbow mandates a stable joint, such as in a manual laborer, arthrodesis is rarely a consideration for proximal ulna nonunions associated with significant articular distortion (see Chapter 70).
Joint Replacement
In a salvage situation, when pain and instability are paramount and only sedentary activity is acceptable, total joint replacement has been successful, using a linked prosthetic replacement. Joint replacement is effective in elderly patients with severe arthrosis, ankylosis, or osteoporosis (Fig. 26-15). In our experience, these patients are treated successfully with joint replacement and the postoperative rehabilitation period averaged 3 months. But this is considered the ultimate salvage procedure. When total replacement is performed in the face or because of the olecranon nonunion, Marra et al42 have shown osteosynthesis occurs only in about 50% of patients. However, of importance, the function of a stable, undisplaced fibrous nonunion is comparable to a solidly united fracture.
Treatment of Nonunion with Monteggia Fracture-Dislocation
Nonunion with anterior fracture dislocation is the most severe and most difficult injury of the proximal ulna because the coronoid is involved.10,19,57 Cases are divided into two treatment groups: injuries with a restorable articular surface, and those in which articular surface damage precludes restoration.
In the first group, accurate realignment and restoration of the articular surface is mandatory. After taking down and repositioning or shortening the fragments, rigid internal fixation must be achieved. The subluxed distal ulnar segment is reduced, and the anterior capsule is dissected from the coronoid process and tubercle to protect the vital anterior neurovascular structures. Exposure is generally achieved by the posterior approach described by Bryan and Morrey.15 The medial collateral ligament is identified and repaired or reconstructed. Shortening of the ulna distal to the coronoid may be necessary to prevent pressure of the ulnar articular surface against the trochlea of the humerus. Internal fixation is best achieved with either a long lag screw or a six- to eight-hole tubular AO plate and screws. Early motion is initiated at 3 weeks.
COMPLICATIONS OF TREATMENT OF NONUNIONS
The complications of treatment for nonunion of olecranon fractures include recurrent nonunion, heterotopic ossification, neurapraxia, diminished range of motion, traumatic arthritic changes, pain, reflex sympathetic dystrophy, and infection.41,55 When rigid internal fixation is achieved and early motion can be initiated at 5 to 7 days in the functional range of 30 to 130 degrees, less permanent contracture may be anticipated. Unless ossification occurs in the brachialis muscle or the anterior capsule, ectopic calcification is usually of little consequence.
In the Mayo series, there was only one patient with postoperative ulnar nerve paresthesias after operative treatment of olecranon nonunion.55 Eriksson and associates28 reported a higher rate of nerve complications (10%) with fresh olecranon fractures. Isolation and protection of the nerve are warranted for virtually all reconstructive surgeries for nonunion at the elbow. The use of a nerve stimulator and high-power loops is helpful for dissection of scar tissue about the ulnar nerve.
RESULTS
Papagelopoulos and Morrey55 reported the Mayo Clinic experience in 24 consecutive patients treated from 1976 to 1991 for nonunion of olecranon fractures. The mean age of these patients was 42 years, and the mean interval from fracture to treatment for nonunion was 19 months. Management was through rehabilitation and activity as tolerated for three patients, continued immobilization for one, and operative treatment for 20. Operations included excision of the olecranon fragment (1), osteosynthesis (16), and joint replacement (3). Four patients also had distraction arthroplasty. At a mean follow-up time of 18 months, no patient had severe residual elbow pain but three had moderate and six had mild symptoms. The mean arc of motion was 98 degrees, representing an average improvement of 11 degrees. Twelve patients had an excellent result, four good, six fair, and two poor. Union had been achieved in 15 of the 16 patients treated through osteosynthesis. Ring et al58 also noted that not all of those that attain union are considered satisfactory due to associated injuries.
Danziger and Healy23 reviewed five patients treated surgically for nonunion of the olecranon. Four of the five fractures leading to nonunion were comminuted or oblique. Three nonunions occurred after tension band wiring, one nonunion occurred after open reduction internal fixation with a semitubular plate, and one nonunion occurred after treatment with a cast. The median interval from fracture to treatment of nonunion was 8 months. All nonunions were treated surgically. Four patients were treated with a tension band plate technique. All nonunions united at a median of 3 months. The median follow-up period was 36 months (range, 12 to 48 months).
1 Adler S., Fay G.F., McAusland W.R.Jr. Treatment of olecranon fractures. J. Trauma. 1962;2:597.
2 Bae D.S., Waters P.M., Sampson C.E. Use of free vascularized fibular graft for congenital ulnar pseudarthrosis: surgical decision making in the growing child. J. Pediatr. Orthop. 2005;25:755.
3 Bakalim G., Wilppula E. Fractures of the olecranon I, II, III. Ann. Chir. Gynaecol. Fenn. 1971;60:95.
4 Barford B. Quoted in personal communication with drawing by Colton, C. L.: Fracture of the olecranon in adults: classification and management. Injury. 1973;5:121.
5 Bassett C.A. Contributions of endosteum, cortex and soft tissue to osteogenesis. Surg. Gynecol. Obstet. 1961;112:145.
6 Bassett C. Pulsing electromagnetic fields: a new method to modify cell behavior in calcified and noncalcified tissues. Calcif. Tissue Int. 1982;34:1.
7 Bassett C., Andrew L., Valdes M.G., Hernandez E. Modification of fracture repair with selected pulsing electromagnetic fields. J. Bone Joint Surg. 1982;64A:888.
8 Becker R. Bioelectric factors controlling bone structure. In: Frost H.M., editor. Bone Biodynamics. Boston: Little, Brown & Co., 1964.
9 Berger P. Le Traitement des Fractures de et Particulièrement la Suture de par un Procédé (Cedarg de). Ga. 2 Hebd. de Med. 1902:193.
10 Boyd H.B., Boles J.C. The Monteggia lesion. A review of 159 cases. Clin. Orthop. Relat. Res. 1969;66:94.
11 Boyd H.B., Lipinski S.W., Wiley J.H. Observations on nonunions of the shafts of the long bones, with a statistical analysis of. 842 patients. J. Bone Joint Surg.. 1961;43A:159.
12 Breen T., Gelberman R.H., Leffert R., Botte M. Massive allograft replacement of hemiarticular traumatic defects of the elbow. J. Hand Surg. 1988;13A:6.
13 Brighton C.T., Black J., Friedenberg Z.B., Esterhai J.L., Day L.J., Connolly J.F. A multicenter study of the treatment of nonunion with constant direct current. J. Bone Joint Surg. 1981;63:1.
14 Brooks M. The Blood Supply of Bone. New York: AppletonCentury-Crofts, 1971.
15 Bryan R.S., Morrey B.F. Extensive posterior exposure of the elbow. Clin. Orthop. 1982;166:188.
16 Burge P., Benson M. Bilateral congenital pseudar-throsis of the olecranon. J. Bone Joint Surg. 1987;69:460.
17 Chen F., Osterman A.L., Mahony K. Smoking and bony union after ulna-shortening osteotomy. Am. J. Orthop. 2001;30:486.
18 Colton C.L. Fractures of the olecranon in adults: classification and management. Injury. 1973;5:121.
19 Conn J., Wade P.A. Injuries of the elbow (a ten-year review). J. Trauma. 1961;1:248.
20 Coughlin M.J., Slabaugh P.B., Smith T.K. Experience with the McAtee olecranon device in olecranon fractures. J. Bone Joint Surg. 1979;61A:385.
21 Cozen L. Does diabetes delay fracture healing? Clin. Orthop. Relat. Res. 1972;82:134.
22 Crenshaw A.H., Perez E.A. Fractures of the shoulder, arm and forearm. In: Canale S.T., Beaty J.H., editors. Campbell’s Operative Orthopedics. 11th ed. Philadelphia: Mosby Elsevier; 2008:3371-3459.
23 Danziger M.B., Healy W.L. Operative treatment of olecranon nonunion. J. Orthop. Trauma. 1992;6:290-293.
24 Davila S., Mikuli D., Haiman M., Zagar Z., Popovi L., Antabak A. Treatment of pseudarthroses of the olecranon with the anatomical hook plate. Lijecn. Vjesn. 2000;122:226.
25 Dell P.C., Sheppard J.E. Vascularized bone grafts in the treatment of infected forearm nonunions. J. Hand Surg. 1984;9:653.
26 Dimitriou R., Dahabreh Z., Katsoulis E., Matthews S.J., Branfoot T., Giannoudis P.V. Application of recombinant BMP-7 on persistent upper and lower limb nonunions. Injury. 2005;36(suppl 4):S51.
27 Dunn N. Operation for fracture of the olecranon. Br. Med. J. 1939;1:214.
28 Eriksson E., Sahlen O., Sandohl U. Late results of conservative and surgical treatment of fracture of the olecranon. Acta Chir. Scand. 1957;113:153.
29 Foille D.J. Note sur les Fractures de l’Olecrane Par Projectiles de Guerre. Marseille Med. 1918;55:241.
30 Gainor B.J., Moussa F., Schott T. Healing rate of transverse osteotomies of the olecranon used in reconstruction of distal humerus fractures. J. South. Orthop. Assoc. 1995;4:263.
31 Gartsman G.M., Sculco T.P., Otis J.C. Operative treatment of olecranon fractures. J. Bone Joint Surg. 1981;63A:718.
32 Green D.P., Rockwood C.A. Fractures. Philadelphia: J. B. Lippincott Co., 1975.
33 Green N. Radiation induced delayed union of fractures. Radiology. 1969;93:635.
34 Heppenstall R.B. Fracture Treatment and Healing. Philadelphia: W. B. Saunders Co., 1980;83.
35 Howard J.L., Urist M.R. Fracture dislocation of radius and ulna at the elbow joint. Clin. Orthop. 1958;12:276.
36 Judet, J., and Jude, R.: L’Ostéogenèse et les Retards de Consolidation et les Pseudarthroses des Os Longs. Huitième Congres SICOT 1966, p. 315.
37 Kiviluoto O., Santauirta S. Fractures of the olecranon. Analysis of 37 consecutive cases. Acta Orthop. Scand.. 1978;49:28.
38 Kovach J., Baker B.E., Mosher J.F. Fracture separation of the olecranon ossification center in adults. Am. J. Sports Med.. 1985;13:2.
39 Lee K.S., Lee S.H., Ha K.H., Lee S.J. Congenital pseudarthrosis of the ulna treated by free vascularized fibular graft—a case report. Hand Surg.. 2000;5:61.
40 Lehman M.A. Nonunion of an olecranon fracture following birth injury. Bull. Hosp. Joint Dis.. 1965;26:187.
41 Levy R.N., Sherry H.S. Complications of treatment of fractures and dislocations of the elbow. In: Epps C.H., editor. Complications in Orthopedic Surgery. Philadelphia: J. B. Lippincott Co.; 1975:237.
42 Marra G., Morrey B.F., Gallay S.H., McKee M.D., O’Driscoll S.W. Fracture and nonunion of the olecranon in total elbow arthroplasty. J. Shoulder Elbow Surg.. 2006;15:486.
43 Mathews J.G. Fractures of the olecranon in children. Injury. 1980;12:207.
44 Mayer P.J., Evarts C.M. Nonunion, delayed union, malunion, and avascular necrosis. In: Epps C.H., editor. Complications in Orthopedic Surgery. Philadelphia: J. B. Lippincott; 1975:159.
45 McKeever F.M., Buck R.M. Fracture of olecranon process of the ulna. J. A. M. A.. 1947;135:1.
46 Meals R.A. The use of a flexor carpi ulnaris muscle flap in the treatment of an infected nonunion of the proximal ulna. Clin. Orthop. Relat. Res.. 1989;240:168.
47 Morrey B.F., An K.N. Functional anatomy of the ligaments of the elbow. Clin. Orthop. Relat. Res.. 1985;201:84.
48 Morrey B.F. Distraction arthroplasty. Clinical applications. Clin. Orthop. Relat. Res.. 1993;293:46.
49 Muller M.E., Allgower M., Willenegger H. Manual of Internal Fixation. Berlin: Springer-Verlag, 1970.
50 Muller M.E. Treatment of nonunion by compression. Clin. Orthop. Relat. Res. 1965;43:83.
51 Murphy D.F., Greene W.B., Gilbert J.A., Dameron T.B. Displaced olecranon fracture in adults. Clin. Orthop. Relat. Res. 1987;2:224.
52 Nakaji N., Fujioka H., Tanaka J., Sugimoto K., Yoshiya S., Fujita K., Kurosaka M. Stress fracture of the olecranon in an adult baseball player. Knee Surg. Sports Traumatol Arthrosc. 2006;14:390.
53 Newell R.L.M. Olecranon fractures in children. Injury. 1975;37:33.
54 Orava S., Hulkko A. Delayed unions and nonunions of stress fractures in athletes. Am. J. Sports Med. 1988;16:517.
55 Papagelopoulos P.J., Morrey B.F. Treatment of nonunion of olecranon fractures. J. Bone Joint Surg. Br. 1994;76:627.
56 Paterson D.C., Lewis G.N., Cass C.A. Treatment of delayed union and nonunion with an implanted direct current stimulator. Clin. Orthop. 1980;148:117.
57 Regan W., Morrey B.F. Fractures of the coronoid process of the ulna. J. Bone Joint Surg. 1989;71A:1348.
58 Ring D., Jupiter J.B., Gulotta L. Atrophic nonunions of the proximal ulna. Clin. Orthop. Relat. Res. 2003;409:268.
59 Rommens P.M., Kuchle R., Schneider R.U., Reuter M. Olecranon fractures in adults: Factors influencing outcome. Injury. 2004;35:1149.
60 Rothman R. The effect of iron deficiency anemia on fracture healing. Clin. Orthop. Relat. Res. 1971;77:276.
61 Sharrard W.J.W., Sutcliffe M.S., Robson M.J., Maceachern A.G. The treatment of fibrous nonunion of fractures by pulsing electromagnetic stimulation. J. Bone Joint Surg. 1982;64B:189.
62 Silberstein M.J., Bradeur A.E., Graviss E.R., Luisiri A. Some vagaries of the olecranon. J. Bone Joint Surg. 1981;63A:722.
63 Smith F.M. Surgery of the Elbow. Philadelphia: W. B. Saunders Co., 1972;260.
64 Srivastava K.P., Vyas O.N., Varshney A.K., Singh C.P. Compression osteosynthesis in fractures of the olecranon. Int. Surg. 1978;63:20.
65 Taylor T.K.F., Scham S.M. A posteromedial approach to the proximal end of the ulna for the internal fixation of olecranon fractures. J. Trauma. 1969;9:594.
66 Tonna E.A. The cellular complement on the skeletal system studied autoradiographically with tritiated thymidine (H3 DTR) during growth and aging. J. Biophys. Biochem. Cytol.. 1961;9:813.
67 Torg J.S., Moyer R.A. Nonunion of a stress fracture through the olecranon epiphyseal plate observed in an adolescent baseball pitcher. J. Bone Joint Surg. 1977;59A:264.
68 Tullos H.S., Schwab G., Bennett J.B., Woods W.G. Factors influencing elbow instability. Instruc. Course Lect. 1981;30:193.
69 Waddell G., Howat T.W. A technique of plating severe olecranon fractures. Injury. 1973;5:135.
70 Wadsworth T.G. Screw fixation of the olecranon after fracture of osteotomy. Clin. Orthop. Relat. Res. 1976;119:197.
71 Walker L.G. Painful olecranon physeal nonunion in an adult weight lifter. A case report. Clin. Orthop. 1995;311:125.
72 Weber B.G., Cech O. Pseudarthrosis: Pathology, Biomechanics, Therapy, Results. Berne: Hans Huber Medical Pub., 1976.
73 Weber B., Vasey H. Osteosynthese bei Olecranon Fraktur. Z. Unfallmed. Berufskr. 1963;2:90.
74 Weisband I.D. Tension band wiring technique for treatment of olecranon fractures. J. Am. Osteopath. Assoc. 1978;77:390.
75 Weseley M.S., Barnfield P.A., Einstein A.I. The use of the Zuelzer hook plate in fixation of olecranon fractures. J. Bone Joint Surg. 1976;58A:859.
76 Wilkerson R.D., Johns J.C. Nonunion of an olecranon stress fracture in an adolescent gymnast. Am. J. Sports Med. 1990;18:4.