Chapter 7 Nonoperative Management of Anterior Cruciate Ligament Deficient Patients
Anterior Cruciate Ligament Deficiency: The Need for Muscle Strengthening
The knee joint’s location in the middle of the lower limb kinetic chain is imposed to high loads, which reach multiple the body mass, particularly in the single stance phase of sport activities.1,2 Rupture of the anterior cruciate ligament (ACL) destabilizes the knee joint,3–5 thus making ACL deficient knees prone to repeated subluxations, which form a potential cause for secondary damage to the joint.6–8 Subsequently, dynamic stabilization through the quadriceps and hamstrings becomes very crucial for the protection of the injured knee.9,10 Apart from its mechanical role, the ACL functions as a sensory organ due to the mechanoreceptors within its substance.11 After its rupture, this function is lost, and therefore optimization of the lower limb muscle properties becomes increasingly important in order to compensate for the resulting anterior and rotational knee instability.
Exercise in ACL deficient patients aims at the improvement of various aspects of muscle properties including reflexes, strength, endurance, and coordination with other muscles. Functional exercise that reeducates the neuromuscular coordination holds the central role in rehabilitation programs, as growing evidence supports the development of preprogrammed compensatory muscle activation strategies for efficient shear force dissipation during injured knee loading.12–16 However, the fundamental issue of the need for strength testing and the value of strengthening exercises still leaves room for investigation.
Among the criteria for progression of ACL rehabilitation is the level of quadriceps and hamstring weakness.17,18 Strength testing and exercise have been traditionally incorporated into musculoskeletal rehabilitation regimens. Although the connection between the level of quadriceps strength and functional status has been disputed,19–22 some studies support the interrelation between functional performance of the knee and thigh muscle strength. It is of clinical importance for ACL rehabilitation that patients with greater than normal strength in the injured limb seem to reduce abnormalities during low- and high-stress activities.23 Quadriceps strength appears to determine the functional ability of the ACL deficient or operated limb to a great degree.24,25 Its weakness coincides with low functional performance26 and pathological gait pattern.27 In addition, functional improvement in ACL deficient athletes after training followed the same pattern as the strength of both the quadriceps and hamstrings.23,28
Likewise, increase in hamstring strength after functional exercise incorporating strengthening, stretching, and plyometric drills paralleled a decrease in peak landing forces, and hence safer landing.29 Hamstring strength has also been associated with the level of knee function10,30 and performance,31 and increasing the hamstring–quadriceps (H:Q) strength ratio has be come a rule in order to promote dynamic control of the ACL deficient knee.32,33 Even more, this improvement has been connected with the return to physical activity after ACL injury,34 and the strength of both thigh muscle groups reflects the functional improvement23,28 and the ability to return to physical activity.34
It appears that changes in muscle strength might be a global reflection of muscle properties, including neural changes.35 It seems that adequate strength ensures that a solid basis is built for other refined neuromuscular properties. In other words, adequate strength secures the proper background for the development of global muscle properties. Therefore, it appears that objective evaluation of strength has a valuable position in the functional assessment after ACL injury, and in combination with our findings, it could be suggested that therapeutic intervention should minimize strength weakness, which persists over time when not addressed.
Importance of the Hamstrings, Especially in Soccer Players: Our Research
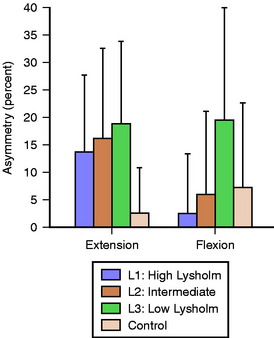
The first study focused on revealing a possible connection of quadriceps and hamstring strength deficits with the level of knee function determined by Lysholm score.30 Three groups of ACL deficient amateur soccer players were examined at different levels of knee function and were compared with a group of controls matched for the preinjury level of activity. The median Lysholm scores of the low, intermediate, and high knee functioning groups were 64.5, 76, and 86 points, respectively. Weakness depicted by the contrast to the healthy condition was significant in all cases and ranged from 19% to 35% according to the muscle or the patient group. Regarding the side-to-side deficit, these major muscle groups did not follow the same pattern. The strength asymmetry of the quadriceps was consistently significant even in the high functioning knees, being greater than 14%, in contrast to the hamstrings, which revealed acceptable symmetry within the normal levels (about 2% to less than 6%) at the high and intermediate knee function groups. Only the poorly functioning athletes had a significant 19% deficit (Fig. 7-1), which places hamstring strength asymmetry (H asymmetry) as a discriminating factor for knee functionality.
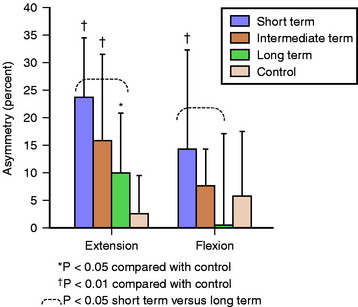
The importance of assessing H asymmetry is highlighted in our recent study that examined different groups of amateur athletes involved in cutting and twisting sports such as soccer, basketball, and handball at different times since ACL rupture.36 We tested the quadriceps and hamstring strength of 36 patients with unilateral ACL deficiency who were divided into three equal groups with mean times for chronicity of about 4, 11, and 57 months for short term, intermediate term, and long term, respectively. We investigated how the strength weakness evolved with time, using the strength of matched healthy controls as a baseline score. Additionally, we questioned whether the quadriceps’ and hamstrings’ side-to-side asymmetry in strength would be consistently significant in all stages of chronicity.
As in the previous study, significant weakness was evident in both muscles in all patient groups, ranging from 21% to 32%. Considering the side-to-side asymmetry of ACL deficient knees, the quadriceps deficit persisted through time, whereas the hamstrings regained symmetry even after 1 year without organized rehabilitation. Regarding the side-to-side strength differences, they tended to lower with time, but in the case of quadriceps, they varied from 10% to 23%, whereas the hamstrings were significantly asymmetric only in the short-term group (14%) and acquired acceptable symmetry within 1 year postinjury (Fig. 7-2).
The quadriceps muscle is affected to a greater degree after ACL injury possibly because of (1) postinjury neural inhibition due to the loss of afferent feedback from ACL to gamma motor neurons37,38 and (2) the adaptation toward a “quadriceps avoidance gait” pattern39,40 to prevent anterior subluxation,41,42 which unloads the limb, promoting quadriceps weakness in ACL deficient patients.12 The greater atrophy of the quadriceps (10% versus 4%) reported even 1 year postinjury7 may also add to the explanation of their higher deficit compared with the hamstrings. In contrast, evidence exists that the hamstrings are recruited in weight-bearing activities in a subconscious attempt to counteract anterior shear forces.5,43 This stimulus might have assisted with the improvements in our patients. Evidence in the literature also supports the development of subtle electrophysiological modifications in ACL deficient patients that retune the hamstrings and preprogram their muscle activation strategies to optimize shear force dissipation during injured knee loading.14–16
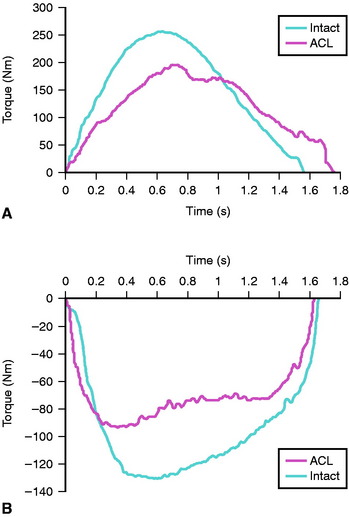
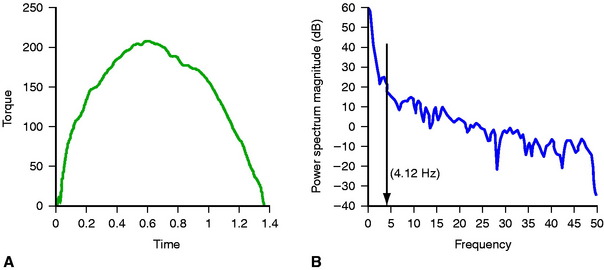
In another study, we investigated the quality of muscle contraction when ACL deficient patients performed maximal exercise via the smoothness of the torque curve throughout knee extension and flexion.44 Our methodology comprised transformation of each torque-time curve pattern into the frequency domain (power spectrum) via fast Fourier transform in order to quantify the smoothness of the isokinetic curve (Fig. 7-3). Each curve of biological signal that is not a perfect sine is actually the sum of other curves, and therefore it can be analyzed into its fundamental components. Our biological interpretation of this method is based on the notion that disturbed motion is generally connected to poor level of joint functionality. Irregular torque output has been connected to other pathologies such as anterior knee pain.45,46 In contrast, smoothness of torque generation is indicative of enhanced force control.47 The frequency contained at three levels of the total power of the signal (90%, 95%, and 99%) was calculated in order to exclude noise from the 100% power level but still include enough harmonics. Both extension and flexion isokinetic curves demonstrated increased irregularities as expressed by the higher-frequency contents by 18.8%, 10.6%, and 40.0% for knee extension and 49.5%, 24.5%, and 16.3% for knee flexion, according to the power level of assessment (Fig. 7-4). Although the results regarding quadriceps were expected on the basis of previous reports using different methodologies, the hamstrings’ increased irregularity had not been reported elsewhere. This finding might be of functional importance and open a future area of investigation.
The higher oscillations characterizing the isokinetic curve of the ACL deficient knee, which is expressed in increased frequency contents, may be attributed to mechanical and/or neuromuscular factors. Increased anterior gliding of the tibia during knee extension might account for the mechanical part. Quadriceps inhibition37,38 and poorly coordinated activation within the hamstrings43,48 must explain the neural aspects of abnormalities of mechanical output. This loss of smoothness in extension-flexion might be clinically important and should be investigated further. Quantification of irregularity of the extension-flexion curve is an innovative approach and could be a valuable tool in the assessment of ACL deficient knees.
Review of the Literature on the Role of the Quadriceps and Hamstrings in Anterior cruciate ligament Deficient Knees
The quadriceps is the muscle group suffering the most dramatic effects after ACL tear.19,30,36,49 For this reason, in addition to its functional importance for normal gait, it attracts most of the attention from clinicians and researchers. Quadriceps torque deficit is more than double hamstring deficit, which is attributed to its susceptibility for quick atrophy due to disuse10,18 and neural inhibition.37,38 Marked weakness of the quadriceps prevents the knee from functioning normally, and given that this weakness is exaggerated in many cases,30 it should be managed adequately. If the voluntary deficit measured via superimposed electrical burst to the maximal voluntary contraction exceeds 5%, treatment with electrical stimulation effectively ameliorates loss of the quadriceps strength and should be implemented from the early stages.50 Although in ACL deficient knees there is no graft to be stressed due to the anterior instability of the tibia caused by quadriceps contraction particularly near extension,9,42,51 this might be harmful for other capsuloligamentous structures.
In contrast, the hamstrings are properly located to counteract anterior tibial instability at flexion angles exceeding 30 degrees.52–54 However, doubts exist regarding the efficacy of the hamstrings to counterbalance shear loading of the knee,53,55 based on two concerns: first, whether the magnitude of the posteriorly directed muscle force is enough to counteract shear forces in the functionally more important knee angles near extension,41,54,56 and second, whether reflex activation of the hamstrings during abrupt perturbations of the knee is fast enough to develop tension in time with the peak external destabilizing moment.57,58
Considering the development of the properly directed stabilizing force, studies on cadavers,55,59 animals,54,60 and mathematical models53,61,62 support that beyond 30 degrees of knee flexion, the posteriorly directed vector of hamstring force becomes adequate in stabilizing the ACL deficient knee (Fig. 7-5). In addition, it should not be underestimated that even when the line of pool of the hamstrings is inefficient, co-contraction could increase joint stability due to joint compression63 and widening of the pressure distribution along the articular surfaces of the knee.64 Additionally, it has been reported that the hamstrings cause greater stiffness to the ACL deficient knee than they do to the intact knee.65
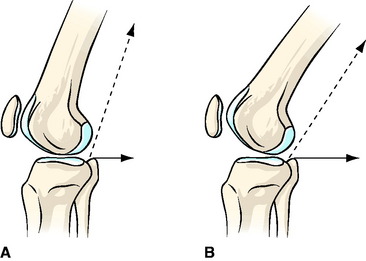
Fig. 7-5 As the knee flexes from A to B, the anti-shear vector of the hamstring force (solid line) increases.
Regarding the question of the timely activation of the hamstrings, an overfocus on their reflex latency of 40 to 50 ms, which is a medium latency response,66–68 may be misleading in regard to their efficacy to prevent instability. Growing evidence in the literature supports the development of preprogrammed compensatory muscle activation strategies.12–16 These strategies suggest that subtle electrophysiological modifications of the subjects are implemented by deficient patients after ACL injury to optimize shear force dissipation during injured knee loading. Hence, feed-forward mechanisms can be adopted that initiate hamstring co-contraction during the expectation of knee loading, not only as a reflex response.13,16,69,70 Therefore the hamstrings should be well conditioned in order to have a greater potential to enhance knee stability.
Bracing in anterior cruciate ligament Deficient Patients: Is It Effective?
The use of functional knee braces is a common practice for enhancing knee stability after rupture of the ACL or reconstruction, with contradictory opinions about their importance in knee unloading.71–73 A favorable change of firing pattern for the hamstrings was observed more often when ACL deficient patients performed single-leg landings wearing a brace69 and in skiers during periods of increased knee flexion.74 The greater biceps femoris activity was exhibited by the more unstable knees. Lam et al75 found that wearing a functional brace improved hamstring reflex responses in ACL deficient knees after fatigue induced by repeated extension and flexion against spring resistance. Although their protocol did not replicate a functional weight-bearing condition, it gives a potentially useful message that bracing in ACL deficient knees may enhance protection. Wojtys et al76 showed that braces can decrease anterior tibial translation by a large margin.
In contrast, other findings have shown a slowing of hamstring muscle reaction times with bracing76 or decreased activation.71,77
However, patients with torn ACLs who do not cope well with their injury and do not choose surgery might benefit from bracing.78
Rehabilitation
Rehabilitation after ACL rupture is a multifactorial issue. However, the general goals consist of gaining good functional stability, optimizing the functional level, and minimizing the risk for reinjury.79 Interventions follow a general scheme depending on chronicity and are generally grouped into the acute phase focusing on range of motion, pain management, regaining ambulation, and retarding atrophy; the advanced phase, which aims to increase strength and endurance; and the return-to-play phase, with the final neuromuscular optimization of knee function.80 Progression from one stage to the other follows certain criteria, one being the achievement of adequate strength for the demands of each stage.
Rehabilitation should aim at limiting thigh muscle weakness after ACL rupture, reducing the quadriceps side-to-side deficit to clinically acceptable levels, and assisting the hamstrings to regain strength faster. These benefits could enhance the natural reaction of the body against anterior knee instability. The effect of organized rehabilitation protocols on the time course of strength adaptations after ACL injury has yet to be examined. A promising research area is the investigation of whether early and intensive postinjury strengthening of the hamstrings will allow more ACL deficient patients to cope with their injury. Nevertheless, only a small fraction of ACL deficient athletes who choose not to have a reconstruction return to their previous level of exercise, and those who do so progress through rehabilitation through specific training and by achieving certain criteria.81 The majority follow a more conservative lifestyle attributed either to knee problems79 or to social reasons and fear of reinjury.82
Excessive atrophy and weakness of the quadriceps are evident in ACL deficient patients and, in cases of quadriceps inhibition, might not be reversible without electrical stimulation, which should commence from the early stages.38 Quadriceps activity potentially leads to knee instability, but it can be exercised safely either through a closed kinetic chain or in angles flexed more than 45 degrees. This deficit should not be neglected because it persists through time.36
Hamstring strength has been connected with the functional outcome of the ACL deficient30 and ACL reconstructed knee10 or the possibility of engaging in higher levels of sports participation.32 Strengthening of the hamstrings holds a key position in the conservative treatment of the ACL deficient knee,32,83 and it appears that strength training of a specific muscle also increases its coactivation level.84 A 3-month, high-resistance training program with four sets of 8 RM (repetitions maximum: load that permits the completion of only eight repetitions) performed 3 times per week may increase the capacity of the hamstrings to provide stability to the knee joint during fast extension.85 This improvement was expressed through a significantly elevated H eccentric:Q concentric ratio.
As a rule, ACL rupture leads to a decrease in the level of physical activity, especially in those who were involved in cutting and twisting sports.86,87 ACL deficient athletes appear to reduce physical activity to 4 degrees Tegner from an initial 9 and 10 degrees.88 Characteristically, Lysholm et al3 reported that although the activity of 62% of their sample was higher than 7 degrees Tegner prior to ACL rupture, after the injury only 10% remained above this limit. Reduction of physical activity markedly affects the healthy side as well,30,36 complicating the return to high-demand activities. To counteract that, closed kinetic chain exercises with great hip flexion angles are an evidence-based method to re-educate coordination and physiological properties with safety, along with open chain single-joint exercise for more specific effects.
Hip control is crucial for the control of knee rotation and proper lower limb alignment, but it is important to remember that the knee is not only directly interrelated with the hip joint but is also connected with the ankle joint. Rudolph et al89 found that coping patients partly relieved the ACL deficient knee by demonstrating a higher contribution of the ankle extensors to the total moment production of the lower limb. Likewise, hamstring tasks to control knee instability can be reinforced by synergists including the anterior tibialis, soleus,90,91 and muscles of the deep posterior compartment muscle group.90 Those synergists have the potential to control the anterior translation and internal rotation of the tibia. This occurs via their reverse action on the ankle and the subtalar joints during closed kinetic chain activities, when the foot is planted on the ground and subsequently the peripheral movement is restricted. Concerning the gastrocnemius, its origin above the knee joint complicates the effect of its action. Fleming et al 92 implanted the more precise and accurate differential variable reluctance transducer (DVRT)93,94 on the anteromedial bundle of the ACL and showed that isometric gastrocnemius muscle contraction strained the ACL within the last 15 degrees of knee extension. Additionally, gastrocnemius muscle contraction combined with quadriceps or hamstring muscle contraction increased the strain up to the last 30 degrees of flexion in comparison with isolated contractions of these muscles. This study ensured muscle specificity in contraction by applying transcutaneous electrical muscle stimulation in subjects under spinal anesthesia. However, there are studies indirectly showing that gastrocnemius contraction could stabilize the tibia under certain circumstances. O’Connor,95 using a two-dimensional mathematical model, found that simultaneous contraction of the quadriceps, hamstrings, and gastrocnemius totally unloaded the ACL at 22 degrees of flexion. Kvist and Gullquist96 showed that when the gastrocnemius is coactivated with the quadriceps in a closed chain exercise (squatting) with the center of gravity over or posterior to the foot, joint compression is increased but anterior tibial translation is not. They also suggest that ACL deficient patients should enhance the spontaneous coactivation of quadriceps with certain neuromuscular training. However, Fleming et al97 questioned the safety of closed kinetic exercises, leaving the area still open for investigation.
1 Besier TF, Lloyd DG, Cochrane JL, et al. External loading of the knee joint during running and cutting maneuvers. Med Sci Sports Exerc. 2001;33:1168-1175.
2 Scott SH, Winter DA. Internal forces of chronic running injury sites. Med Sci Sports Exerc. 1990;22:357-369.
3 Lysholm M, Messner K. Sagittal plane translation of the tibia in anterior cruciate ligament-deficient knees during commonly used rehabilitation exercises. Scand J Med Sci Sports. 1995;5:49-56.
4 Noyes FR, Matthews DS, Mooar PA, et al. The symptomatic anterior cruciate-deficient knee. J Bone Joint Surg Am. 1983;65:163-174.
5 Solomonow M, Baratta R, Zhou BH, et al. The synergistic action of the anterior cruciate ligament and thigh muscles in maintaining joint stability. Am J Sports Med. 1987;15:207-213.
6 Finsterbush A, Frankl U, Matan Y, et al. Secondary damage to the knee after isolated injury of the anterior cruciate ligament. Am J Sports Med. 1990;18:475-479.
7 Gerber C, Hoppeler H, Claassen H, et al. The lower extremity musculature in chronic symptomatic instability of the anterior cruciate ligament. J Bone Joint Surg Am. 1985;67:1034-1043.
8 Hogervorst T, Rijcken THP, Hart CPVD, et al. Abnormal bone scans in anterior cruciate ligament deficiency indicate structural and functional abnormalities. Knee Surg Sports Traumatol Arthrosc. 2000;8:137-142.
9 Beynnon BD, Braden CF, Johnson RJ, et al. Quadriceps muscle contraction protects the anterior cruciate ligament during anterior tibial translation. Am J Sports Med. 1995;23:187-190.
10 Wojtys EM, Huston LJ. Neuromuscular performance in normal and anterior cruciate ligament-deficient lower extremities. Am J Sports Med. 1994;22:89-104.
11 Georgoulis AD, Pappa L, Moebius U, et al. The presence of proprioceptive mechanoreceptors in the remnants of the ruptured ACL as a possible source of re-innervation of the ACL autograft. Knee Surg Sports Traumatol Arthrosc. 2001;9:364-368.
12 Kalund S, Sinkjaer T, Arendt-Nielsen L, et al. Altered timing of hamstring muscle action in anterior cruciate ligament deficient patients. Am J Sports Med. 1990;18:245-248.
13 Dyhre-Poulsen P, Simonsen EB, Voigt M. Dynamic control of muscle stiffness and H reflex modulation during hopping and jumping in man. J Physiol. 1991;437:287-304.
14 DeMont RG, Lephart SM. Effect of sex on preactivation of the gastrocnemius and hamstring muscles. Br J Sports Med. 2004;38:120-124.
15 Di Fabio RP, Graf B, Badke MB, et al. Effect of knee joint laxity on long-loop postural reflexes: evidence for a human capsular-hamstring reflex. Exp Brain Res. 1992;90:189-200.
16 McNair PJ, Marshall RN. Landing characteristics in subjects with normal and anterior cruciate ligament deficient knee joints. Arch Phys Med Rehab. 1994;75:584-589.
17 Shelbourne KD, Johnson BC. Effects of patellar tendon width and preoperative quadriceps strength on strength return after anterior cruciate ligament reconstruction with ipsilateral bone-patellar tendon-bone autograft. Am J Sports Med. 2004;32:1474-1478.
18 Wilk KE. Accelerated rehabilitation after anterior cruciate ligament reconstruction with central-third patellar tendon. In: Brotzman SB, Wilk KE, editors. Clinical orthopaedic rehabilitation. ed 2. Philadelphia: Mosby; 2003:288-289.
19 Keays SL, Bullock-Saxton J, Keays AC. Strength and function before and after anterior cruciate ligament reconstruction. Clin Orthop. 2000;373:174-183.
20 Tibone JE, Antich TJ, Fanton GS, et al. Functional analysis of anterior cruciate ligament instability. Am J Sports Med. 1986;14:276-284.
21 Rudolph KS, Axe MJ, Snyder-Mackler L. Dynamic stability after ACL injury: who can hop? Knee Surg Sports Traumatol Arthrosc. 2000;8:262-269.
22 Murray SM, Warren RF, Otis JC, et al. Torque-velocity relationships of the knee extensor and flexor muscles in individuals sustaining injuries of the anterior cruciate ligament. Am J Sports Med. 1984;12:436-440.
23 Patel RR, Hurwitz DE, Bush-Joseph CA, et al. Comparison of clinical and dynamic knee function in patients with anterior cruciate ligament deficiency. Am J Sports Med. 2003;31:68-74.
24 Lund-Hansen H, Gannon J, Engebretsen L, et al. Isokinetic muscle performance in healthy female handball players and players with a unilateral anterior cruciate ligament reconstruction. Scand J Med Sci Sports. 1996;6:172-175.
25 Lewek M, Rudolph K, Axe M, et al. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech. 2002;17:56-63.
26 Gauffin H, Tropp H. Altered movement and muscular activation patterns during the one legged jump in patients with an old anterior cruciate ligament rupture. Am J Sports Med. 1992;20:182-192.
27 Liu W, Maitland ME. The effect of hamstring muscle compensation for anterior laxity in the ACL-deficient knee during gait. J Biomech. 2000;33:871-879.
28 Zatterstrom R, Friden T, Lindstrand A, et al. Rehabilitation following acute anterior cruciate ligament injuries—a 12-month follow-up of a randomized clinical trial. Scand J Med Sci Sports. 2000;10:156-163.
29 Hole CD, Smith GH, Hammond J, et al. Dynamic control and conventional strength ratios of the quadriceps and hamstrings in subjects with anterior cruciate ligament deficiency. Ergonomics. 2000;43:1603-1609.
30 Tsepis E, Vagenas G, Giakas G, et al. Hamstring weakness as an indicator of poor knee function in ACL-deficient patients. Knee Surg Sports Traumatol Arthrosc. 2004;12:22-29.
31 Vergis A, Hindriks M, Gillquist J. Sagittal plane translations of the knee in anterior cruciate deficient subjects and controls. Med Sci Sports Exerc. 1997;29:1561-1566.
32 Giove TP, Sayers JMIII, Kent BE, et al. Non-operative treatment in the torn anterior cruciate ligament. J Bone Joint Surg. 1983;65A:184-192.
33 Walla DJ, Albright JP, McAuley E, et al. Hamstring control and the unstable anterior cruciate ligament-deficient knee. Am J Sports Med. 1985;13:34-39.
34 Pincivero DM, Lephart SM, Karunakara RA. Reliability and precision of isokinetic strength and muscular endurance for the quadriceps and hamstrings. Int J Sports Med. 1996;18:113-117.
35 Corcos DM, Slobodan J, Gottlieb GL. Electromyographic analysis of performance enhancement. In: Zelaznik HN, editor. Advances in motor learning and control. Chicago: Human Kinetics; 1996:137.
36 Tsepis E, Vagenas G, Ristanis S, et al. Thigh muscle weakness in ACL-deficient knees persists without structured rehabilitation. Clin Orthop Rel Res. 2006;450:211-218.
37 Konishi Y, Fukubayashi T, Takeshita D. Possible mechanism of quadriceps femoris weakness in patients with ruptured anterior cruciate ligament. Med Sci Sports Exerc. 2002;34:1414-1418.
38 Snyder-Mackler L, Luca PF, Williams PR, et al. Reflex inhibition of the quadriceps femoris muscle after injury or reconstruction of the anterior cruciate ligament. J Bone Joint Surg. 1994;76:555-560.
39 Andriacchi T. Dynamics of pathological motion: applied to the anterior cruciate deficient knee. J Biomech. 1990;23:99-105.
40 Wexler G, Hurwitz D, Bush-Joseph CA, et al. Functional gait adaptations in patients with anterior cruciate ligament deficiency over time. Clin Orthop Rel Res. 1998;348:166-175.
41 Beynnon BD, Fleming BC, Johnson RJ, et al. Anterior cruciate ligament strain behavior during rehabilitation exercises in vivo. Am J Sports Med. 1995;23:24-34.
42 Hirokawa S, Solomonow M, Lu Y, et al. Anterior-posterior and rotational displacement of the tibia elicited by quadriceps contraction. Am J Sports Med. 1992;20:299-306.
43 Tsuda E, Okamura Y, Otsuka H, et al. Direct evidence of the anterior cruciate ligament-hamstring reflex arc in humans. Am J Sports Med. 2001;29:83-87.
44 Tsepis E, Giakas G, Vagenas G, et al. Frequency content asymmetry of the isokinetic curve between ACL deficient and healthy knee. J Biomech. 2004;37:857-864.
45 Dvir Z. Isokinetics of the knee muscles. Dvir Z, editor. Isokinetics: muscle testing, interpretation, and clinical applications. New York: Churchill Livingstone; 1995:110.
46 Lysholm J. The relation between pain and torque in an isokinetic strength test of knee extension. Arthroscopy. 1987;3:182-184.
47 Tracy BL, Enoka RM. Older adults are less steady during submaximal isometric contractions with the knee extensor muscles. J Appl Physiol. 2002;92:1004-1012.
48 Boerboom AL, Hof AL, Halbertsma JPK, et al. A typical hamstrings electromyographic activity as a compensatory mechanism in anterior cruciate ligament deficiency. Knee Surg Sports Traumatol Arthrosc. 2001;9:211-216.
49 Wojtys EM, Huston LJ. Longitudinal effects of anterior cruciate ligament injury and patellar tendon autograft reconstruction on neuromuscular performance. Am J Sports Med. 2000;28:336-344.
50 Snyder-Mackler L, Delitto A, Bailey SL, et al. Strength of the quadriceps femoris muscle and functional recovery after reconstruction of the anterior cruciate ligament. A prospective, randomized clinical trial of electrical stimulation. J Bone Joint Surg Am. 1995;77:1166-1173.
51 Nisell R, Ericson MO, Nemeth G, et al. Tibiofemoral joint forces during isokinetic knee extension. Am J Sports Med. 1989;17:49-54.
52 More RC, Bryant TK, Neiman R, et al. Hamstrings—an anterior cruciate ligament protagonist. Am J Sports Med. 1993;21:231-237.
53 Pandy M, Shelbourne KB. Dependence of cruciate-ligament loading on muscle forces and external load. J Biomech. 1997;30:1015-1024.
54 Renstrom P, Arms SW, Stanwyck TS, et al. Strain within the anterior cruciate ligament during hamstring and quadriceps activity. Am J Sports Med. 1986;14:83-86.
55 Markolf KL, O’Neill G, Jackson SR, et al. Effects of applied quadriceps and hamstrings muscle loads on forces in the anterior and posterior cruciate ligaments. Am J Sports Med. 2004;32:1144-1149.
56 Kain CC, McCarthy JA, Arms S, et al. An in vivo analysis of the effect of transcutaneous electronical stimulation of the quadriceps and hamstrings in anterior cruciate ligament deformation. J Bone Joint Surg. 1988;16:147-152.
57 Krogsgaard MR, Dyhre-Poulsen P, Fischer-Rasmussen T. Cruciate ligament reflexes. J Electromyogr Kinesiol. 2002;12:177-182.
58 Shultz SJ, Perrin DH. Using surface electromyography to access sex differences in neuromuscular response characteristics. J Athletic Train. 1999;34:165-176.
59 Li G, Rudy TW, Sakane MA, et al. The importance of quadriceps and hamstring muscle loading on knee kinematics and in-situ forces in the ACL. J Biomech. 1999;32:395-400.
60 Aune AK, Nordsletten L, Skjeldal S, et al. Hamstrings and gastrocnemius co-contraction protects the anterior cruciate ligament against failure: an in vivo study in the rat. J Orthop Res. 1995;13:147-150.
61 Imran A, O’Connor JJ. Control of knee stability after ACL injury or repair: interaction between hamstrings contraction and tibial translation. Clin Biomech (Bristol, Avon). 1998;13:153-162.
62 Shelburne KB, Torry MR, Pandy MG. Effect of muscle compensation on knee instability during ACL-deficient gait. Med Sci Sports Exerc. 2005;37:642-648.
63 Steele JR, Brown JM. Effects of chronic anterior cruciate ligament deficiency on muscle activation patterns during an abrupt deceleration task. Clin Biomech. 1999;14:247-257.
64 Baratta R, Solomonow M, Zhou BH, et al. Muscular coactivation: the role of the antagonist musculature in maintaining knee stability. Am J Sports Med. 1988;16:113-122.
65 Jennings AG, Seedhom BB. The measurement of muscle stiffness in anterior cruciate injuries—an experiment revisited. Clin Biomech. 1998;13:138-140.
66 Jennings AG, Seedhom BB. Proprioception in the knee and reflex hamstring contraction latency. J Bone Joint Surg Br. 1994;76:491-494.
67 Beard DJ, Kyberd PJ, O’Connor JJ, et al. Reflex hamstring contraction latency in anterior cruciate ligament deficiency. J Orthop Res. 1994;12:219-228.
68 Friemert B, Bumann-Melnyk M, Faist M, et al. Differentiation of hamstring short latency versus medium latency responses after tibia translation. Exp Brain Res. 2005;160:1-9.
69 Smith J, Malanga GA, Yu B, et al. Effects of functional knee bracing on muscle-firing patterns about the chronic anterior cruciate ligament-deficient knee. Arch Phys Med Rehab. 2003;84:1680-1686.
70 Johansson H, Sjolander P, Sojka P. A sensory role for the cruciate ligaments. Clin Orthopaed. 1991;268:161-178.
71 Ramsey DK, Wretenberg PF, Lamontagne M, et al. Electromyographic and biomechanic analysis of anterior cruciate ligament deficiency and functional knee bracing. Clin Biomech (Bristol, Avon). 2003;18:28-34.
72 DeVita P, Lassiter TJr, Hortobagyi T, et al. Functional knee brace effects during walking in patients with anterior cruciate ligament reconstruction. Am J Sports Med. 1998;26:778-784.
73 Vailas JC, Pink M. Biomechanical effects of functional knee bracing. Practical implications. Sports Med. 1993;15:10-18.
74 Nemeth G, Lamontagne M, Tho K, et al. Electromyographic activity in expert downhill skiers using functional braces after anterior cruciate ligament injuries. Am J Sports Med. 1997;25:635-641.
75 Lam RY, Ng GY, Chien EP. Does wearing a functional knee brace affect hamstring reflex time in subjects with anterior cruciate ligament deficiency during muscle fatigue? Arch Phys Med Rehabil. 2002;83:1009-1012.
76 Wojtys EM, Kothari SU, Huston LJ. Anterior cruciate ligament functional brace use in sports. Am J Sports Med. 1996;24:539-546.
77 Acierno SP, D’Ambrosia C, Solomonow M, et al. Electromyography and biomechanics of a dynamic knee brace for anterior cruciate ligament deficiency. Orthopaedics. 1995;18:1101-1107.
78 Beynnon BD, Good L, Risberg MA. The effect of bracing on proprioception of knees with anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2002;32:11-15.
79 Kvist J. Rehabilitation following anterior cruciate ligament injury. Current recommendations for sports participation. Sports Med. 2004;34:269-280.
80 Chmielewski TL, Mizner LR, Padamonski W, et al. Knee. In: Kolt GS, Snyder-Mackler L, editors. Physical therapies in sport and exercise. St. Louis: Churchill Livingstone; 2003:386-389.
81 Chmielewski TL, Rudolph KS, Fitzgerald GK, et al. Biomechanical evidence supporting a differential response to acute ACL injury. Clin Biomech. 2001;16:686-691.
82 Mikkelsen C, Werner S, Eriksson E. Closed kinetic chain alone compared to combined open and closed kinetic chain exercises for quadriceps strengthening after anterior cruciate ligament reconstruction with respect to return to sports: a prospective matched follow-up study. Knee Surg Sports Traumatol Arthrosc. 2000;8:337-342.
83 Hagood S, Solomonow M, Baratta R, et al. The effect of joint velocity on the contribution of the antagonist musculature to knee stiffness and laxity. Am J Sports Med. 1990;18:182-187.
84 Solomonow M, Krogsgaard M. Sensorimotor control of knee stability. A review. Scand J Med Sci Sports. 2001;11:64-80.
85 Aagaard P, Simonsen EB, Trolle M, et al. Specificity of training velocity and training load on gains in isokinetic knee joint strength. Acta Physiol Scand. 1996;156:123-129.
86 St Clair Gibson A, Lambert MI, Durandt JJ, et al. Quadriceps and hamstrings peak torque ratio changes in persons with chronic anterior cruciate ligament deficiency. J Orthop Sports Phys Ther. 2000;7:418-427.
87 Bonamo JJ, Fay C, Firestone T. The conservative treatment of the anterior cruciate deficient knee. Am J Sports Med. 1990;18:618-623.
88 Jorgensen U, Bak K, Ekstrand J, Scavenius M. Reconstruction of the anterior cruciate ligament with the iliotibial band autograft in patients with chronic knee instability. 2001;9:137-145.
89 Rudolph KS, Eastlack ME, Axe MJ, et al. Movement patterns after anterior cruciate ligament injury: a comparison of patients who compensate well for the injury and those who require operative stabilization. J Electromyogr Kinesiol. 1998;8:349-362.
90 Nyland JA, Shapiro R, Caborn DN, et al. The effect of quadriceps femoris, hamstring, and placebo eccentric fatigue on knee and ankle dynamics during crossover cutting. J Orthop Sports Phys Ther. 1997;25:171-184.
91 Chmielewski TL, Rudolph KS, Snyder-Mackler L. Development of dynamic knee stability after acute ACL injury. J Electromyogr Kinesiol. 2002;12:267-274.
92 Fleming BC, Renström PA, Ohlen G, et al. The gastrocnemius muscle is an antagonist of the anterior cruciate ligament. J Orthop Res. 2001;19:1178-1184.
93 Fleming BC, Beynnon BD. In vivo measurement of ligament/tendon strains and forces: a review. Ann Biomed Eng. 2004;32:318-328.
94 Beynnon BD, Fleming BC. Anterior cruciate ligament strain in-vivo: a review of previous work. J Biomech. 1998;31:519-525.
95 O’Connor JJ. Can muscle co-contraction protect knee ligaments after injury or repair? J Bone Joint Surg Br. 1993;75B:41-48.
96 Kvist J, Gillquist J. Sagittal plane knee translation and electromyographic activity during closed and open kinetic chain exercises in anterior cruciate ligament-deficient patients and control subjects. Am J Sports Med. 2001;29:72-82.
97 Fleming BC, Renström PA, Beynnon BD, et al. The effect of weight-bearing and external loading on anterior cruciate ligament strain. J Biomech. 2001;34:163-170.