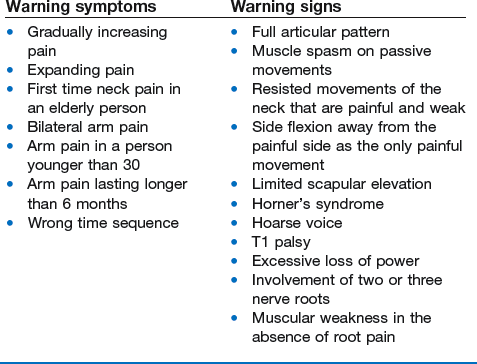
Non-mechanical disorders
Warning signs
Warning signs
Warning signs disclosed by the history
Arm pain lasting longer than 6 months
Most lateral disc protrusions tend to resolve spontaneously. For lumbar disc lesions this may take up to 12 months (see Ch. 33). For cervical disc protrusions causing discoradicular pain, the process is faster and most protrusions will have disappeared after 2–4 months, depending on the size of the protrusion (the larger the protrusion, the faster it fades).1 Therefore, if the pain lasts longer than 4 months, it is unlikely that an ordinary discoradicular lesion is responsible and another cause should be sought.
Warning signs disclosed by the functional examination
Side flexion away from the painful side as the only painful movement
As mentioned earlier, this partial articular pattern is always suspicious and suggests a costoscapuloclavicular lesion (see online section The shoulder girdle) or a visceral lesion in the upper part of the thorax: the apex of the lung or mediastinum.
Horner’s syndrome
This syndrome is caused by an interruption of the sympathetic nerve supply to the eye and is characterized by the classic triad of miosis (constricted pupil), partial ptosis, and loss of hemifacial sweating (anhidrosis). Horner’s syndrome may result from several nervous conditions: a lesion of the primary neurone, a brainstem stroke or trauma to the brachial plexus. When the syndrome is accompanied by cervicoscapular pain, the cause is involvement of the cervical sympathetic ganglia at the base of the neck that results from a tumour of the lung apex (e.g. Pancoast)2 or a dissecting carotid aneurysm.3
Involvement of two or three nerve roots
Unlike in the lumbar spine, root syndromes resulting from cervical discoradicular lesions are always monoradicular. It may be, however, that a radicular weakness does not precisely match the classic pattern. This is somewhat exceptional and is explained by intradural connections between the ventral rootlets of C5, C6 and C7 segments. So it is possible for an individual to have some overlap between myotomes, with one myotome encompassing one or two adjacent segments.4 It may also be possible to have two disc lesions at two (consecutive) levels at the same time. These situations are rare, however, and therefore, when there is involvement of two or more nerve roots, a more serious lesion should be assumed until there is proof to the contrary.
References
1. Rao, R, Neck pain, cervical radiculopathy, and cervical myelopathy: pathophysiology, natural history, and clinical evaluation. Instr Course Lect 2003; 52:479–488. ![]()
2. Owen, TD, Ameen, A, Cervical radiculopathy: Pancoast tumour? Br J Clin Pract 1993; 47:225–226. ![]()
3. Biousse, V, Touboul, PJ, D’Anglejan-Chatillon, J, et al, Ophthalmologic manifestations of internal carotid artery dissection. Am J Ophthalmol. 1998;126(4):565–577. ![]()
4. Tanaka, N, Fujimoto, Y, An, HS, et al, The anatomic relation among the nerve roots, intervertebral foramina, and intervertebral discs of the cervical spine. Spine (Phila Pa 1976). 2000;25(3):286–291. ![]()