Chapter 178 Non–Group A or B Streptococci
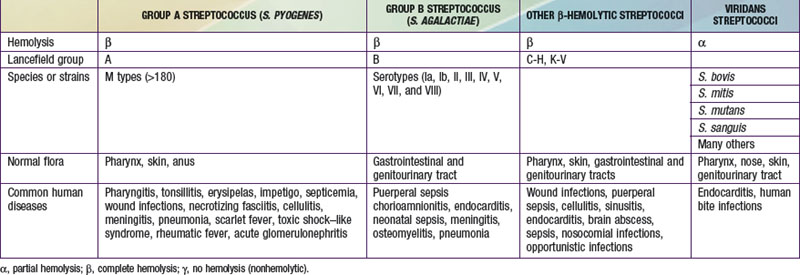
The genus Streptococcus comprises >30 species. Streptococcus pneumoniae (Chapter 175), group A streptococcus (Chapter 176), and group B streptococcus (Chapter 177) are the most common causes of human streptococcal infections. The β-hemolytic streptococci of Lancefield groups C to H and K to V and the α-hemolytic streptococci that cannot be classified within a Lancefield group (the viridans streptococci) commonly colonize intact body surfaces (the pharynx, skin, gastrointestinal tract, genitourinary tract) and also cause infections in humans (see Table 178-1 on the Nelson Textbook of Pediatrics website at www.expertconsult.com ![]() ). Of the non–group A β-hemolytic streptococci, groups C and G streptococcus are the most frequent cause of human disease. The enterococci were once classified among the group D streptococci but are now a separate genus, Enterococcus (Chapter 179).
). Of the non–group A β-hemolytic streptococci, groups C and G streptococcus are the most frequent cause of human disease. The enterococci were once classified among the group D streptococci but are now a separate genus, Enterococcus (Chapter 179).
Table 178-1 RELATIONSHIP OF STREPTOCOCCI IDENTIFIED BY HEMOLYSIS AND LANCEFIELD GROUPING TO SITES OF COLONIZATION AND DISEASE
Arditi M, Shulman ST, Davis AT, et al. Group C beta-hemolytic streptococcal infections in children: Nine pediatric cases and review. Rev Infect Dis. 1989;11:34-45.
Broyles LN, Van Beneden C, Beall B, et al. Population-based study of invasive disease due to β-hemolytic streptococci of groups other than A and B. Clin Infect Dis. 2009;48:706-712.
Faden H. Group C and group G streptococcal disease among children. Pediatr Infect Dis J. 2005;24:1014-1015.
Gerber MA, Randolph MF, Martin NJ, et al. Community-wide outbreak of group C streptococcal pharyngitis. Pediatrics. 1991;87:598-603.
Hashikawa S, Iinuma Y, Furushita M, et al. Characterization of group C and group G streptococcal strains that cause streptococcal toxic shock syndrome. J Clin Microbiol. 2004;42:186-192.
Liao CH, Liu LC, Huang YT, et al. Bacteremia caused by group G streptococci, Taiwan. Emerg Infect Dis. 2008;14:837-840.
Meier FA, Centor RM, Graham LJr, et al. Clinical and microbiological evidence for endemic pharyngitis among adults due to group C streptococci. Arch Intern Med. 1990;150:825-829.
Turner JC, Hayden FG, Lobo MC, et al. Epidemiologic evidence for Lancefield group C beta-hemolytic streptococci as a cause of exudative pharyngitis in college students. J Clin Microbiol. 1997;35:1-4.






