CHAPTER 61 New concepts in fat grafting
Technical steps
Method for obtaining fat
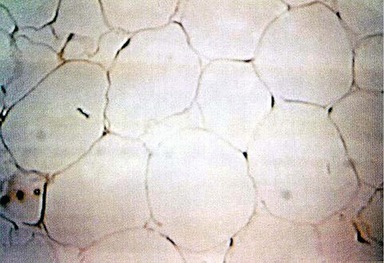
We then proceed with the liposuction, using cannulas of 3 to 6 mm caliber. The obtained fat is aspirated with a pressure around 370 mmHg, with the intention of protecting the fat cell. Studies have shown that higher pressures can damage the fat cell (Fig. 61.1).
Histological evaluation
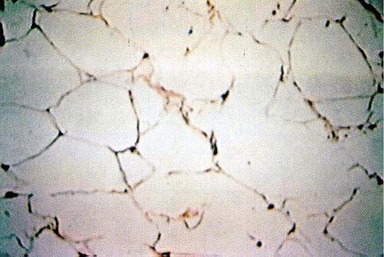
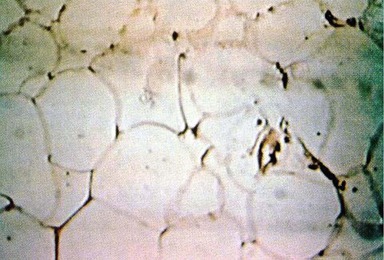
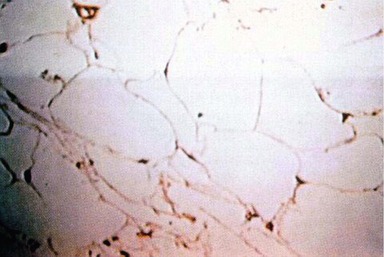
• From 0 to 60 min: fat cells were preserved with good shape and well-distinguished nucleus.
• After 60 min: fat cell destruction varied from 30% to 70%, with high tissue alteration.
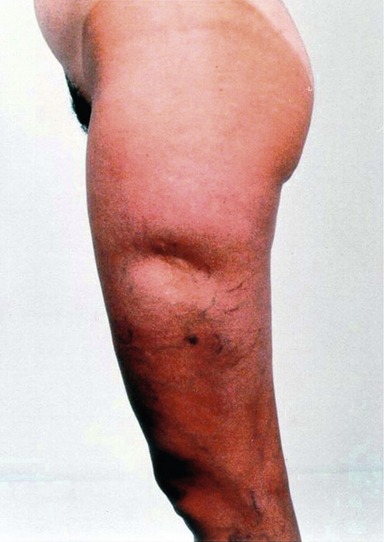
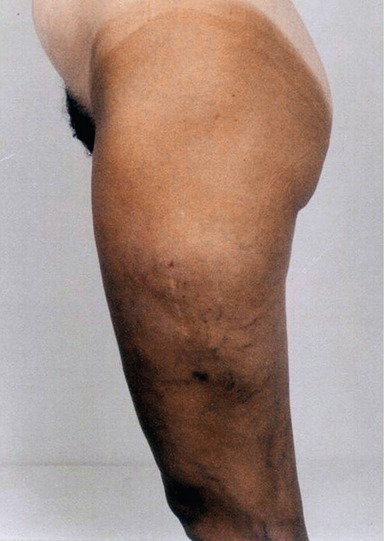
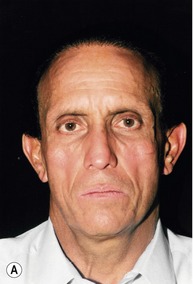
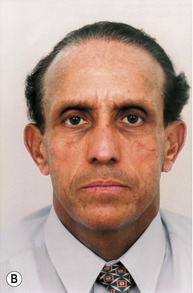
Here we show some cases to illustrate the results and to exemplify the procedure after grafting with a 40 × 12 mm needle and with an infiltration cannula (Fig. 61.8).
Conclusion
• We conducted microscopic experimental studies and established some concepts that can be applied to enhance clinical practice. These are: (1) a defined pressure of 370 mmHg and (2) a preparation time of 60 minutes.
• Regarding the cannula diameter, we have established that 3 to 6 mm allows us to collect a more even material and fat cells with greater vitality.
• We also established that the fat must be washed with saline solution, so that we can remove those cells with less viability, in other words, the fat cells that would be destroyed by the liposuction process. This fat, when prepared and filtered as described above, is presented in a more homogeneous form. Using this standard pattern, we achieve an average time of 60 minutes between the harvest and the injection of the fat.
• Through histological evaluation, we observed that the cells suffered damage over time, and after 120 minutes considerable morphological modifications occur which jeopardize the fat grafting procedure.
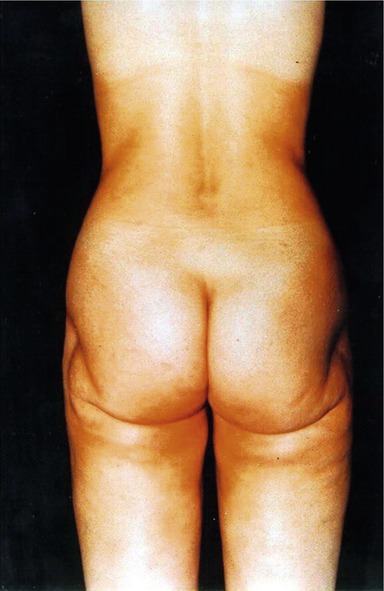
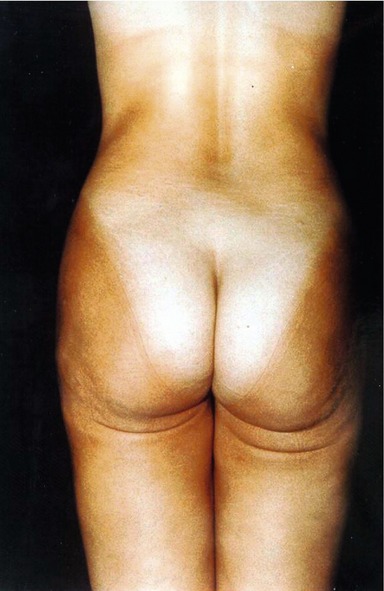
• The goal of fat grafting is the augmentation by fat tissue integration at the recipient site, and not via a fibrosis reaction as described in some papers. We prefer the technique described here to ensure the graft’s viability (Figs 61.9–61.15).
Aboudib Júnior JH, De Castro CC, Gradel J. Hand rejuvenescence by fat filling. Ann Plast Surg. 1992;28(6):559–564.
Carpaneda CA, Ribeiro MT. Study of the histologic alterations and viability of the adipose graft in humans. Aesthet Plast Surg. 1993;17(1):43–47.
Collins PC, Field LM, Narins RS. Liposuction surgery and fat transplantation. Clin Dermatol. 1992;10(3):365–372.
Curi M, Singer MJ, Iaconelli LM, et al. Transplante autógeno de gordura em ratos. Ver Paul Med. 1991;109(1):24–26.
Eppley BL, Sadove AM. A physicochemical to improving free fat graft survival: Preliminary observations. Aesthet Plast Surg. 1991;15(3):215–258.
Eppley BL, Synders RV, Jr., Winkelman T, Delfino JJ. Autologous facial fat transplantation: Improve graft maintenance by microbead bioactivation. J Oral Maxillofac Surg. 1992;50(5):477–482. discussion 482–483 –
Guerrerosantos J, Flores M, De-Leon O. Free fat autografting for cervico-facial augmentation: A 5-year study. Plastic Surgery Forum. 1988;11:216.
Ham AW, Cormack DH. Histologia, 8th edn. Amsterdam: G. Koogan; 1983. pp. 222–228
Illiouz YG. Present results of fat injection. Aesthet Plast Surg. 1988;12:175.
Lam A, Moy R. The potential for fat transplantation. J Dermatol Surg Oncol. 1992;18(5):432–434.
Lewis CM. The correction of deep gluteal depression by autologous fat grafting. Aesthet Plast Surg. 1992;16(3):247–250.
Loeb R. Nasolabial fold undermining and fat grafting based on histological study. Aesthet Plast Surg. 1991;15(1):61–66.
Neuber G. Asepsis und kunstiche Bluteere. Verhandl d Deutsch Gesellsch F Chir, Berlin. 1910;22:159.
Peer LA. The neglected “free fat graft,” its behavior and clinical use. Am J Surg. 1956;92:40.
Queiroz Filho W, De Souza Pinto EB. Estudo comparativo da lipoaspiração ultra-sônica e lipoaspiração superficial. Revista Catarinense. Jornada Sul Brasileira de Cirurgia Plástica, 1993.
Smahel J. Adipose tissue in plastic surgery. Ann Plast Surg. 1986;16:444.
Wertheimer E, Shapiro B. The physiology of adipose tissue. Physiol Rev. 1948;28:451.
Souza Pinto EBS. Superficial liposuction and fat graft. Cellulitis. RAPS International. The VI Annual Meeting; Beverly Hills, CA, July 20–21, 1991.
De Souza Pinto EB. Lipoaspiração dos membros inferiores. Anais do XII Congresso Brasileiro de Cirurgia Plástica; 10 a 14 de novembro de 1985; Gramado RS, pp. 640–641.