Neurologic Assessment
After reading this chapter, you will be able to:
1. Define key terms related to neurologic assessment.
2. Describe the functional anatomy of the nervous system.
3. Explain the cortical function of the different lobes of the brain.
4. Describe the functions of the brainstem, the cerebellum, and the12 pairs of cranial nerves.
5. Describe common techniques used to assess the mental status.
6. Obtain and interpret Glasgow Coma Scale assessment.
7. Describe the importance of assessing level and content of consciousness in intensive care unit patients.
8. Describe common techniques used to assess the cranial nerves, the sensory system, the motor system, coordination, and gait.
9. Describe common techniques used to assess deep, superficial, and brainstem reflexes.
10. Explain the control of the breathing and circulation by the central nervous system.
11. Briefly describe ancillary tests used in neurologic assessment.
12. Identify the importance of intracranial pressure monitoring and the value of assessing cerebral perfusion pressure.
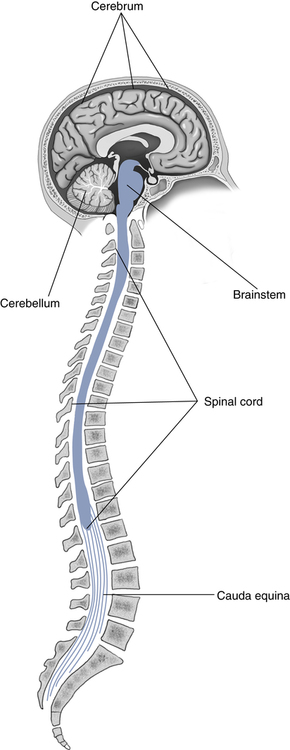
Functional Neuroanatomy
To perform or understand a neurologic assessment, the examiner needs a basic understanding of anatomy and function of the nervous system. The neurologic system is made up of two major parts: the central and peripheral nervous systems. The central nervous system (CNS) contains the brain and spinal cord (Fig. 6-1), whereas the peripheral nervous system is composed of the 12 cranial nerves and the 31 spinal nerves. The brain consists of three parts: the cerebrum, which contains two hemispheres; the brainstem (midbrain, pons, and medulla); and the cerebellum.
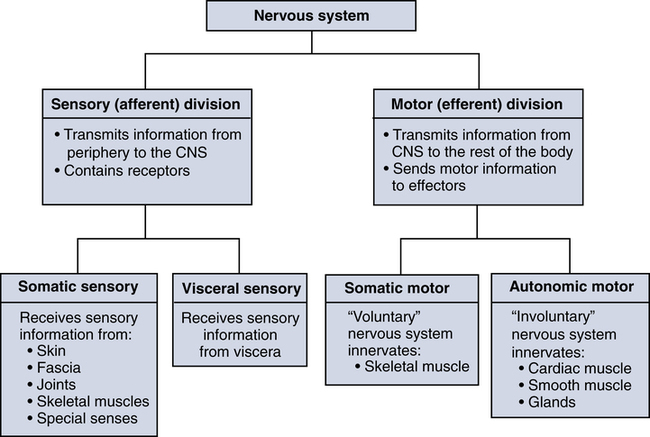
The peripheral nervous system is organized according to its function into sensory (afferent, from the Latin word afferens, to bring to) and motor (efferent, from Latinefferens, to bring out) divisions. This functional organization allows the clinician to understand how signals are transmitted to and from the CNS (Fig. 6-2).
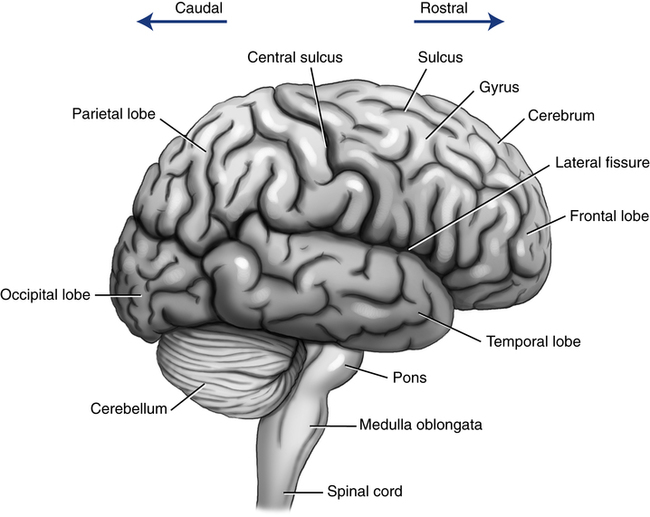
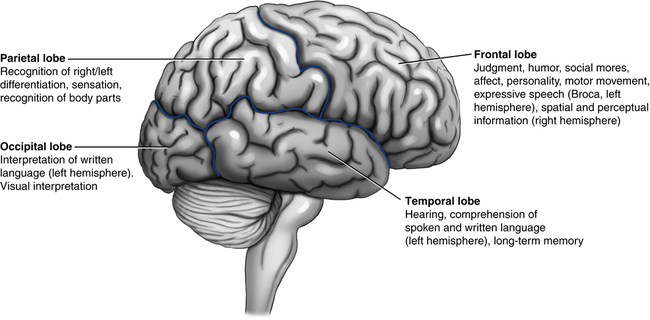
The cerebrum is the largest part of the brain and is made up of two hemispheres and areas that control specific intellectual or motor functions (Fig. 6-3). Lesions in the cerebrum can lead to abnormalities in functions such as movement, level of consciousness, ability to speak and write, emotions, and memory.
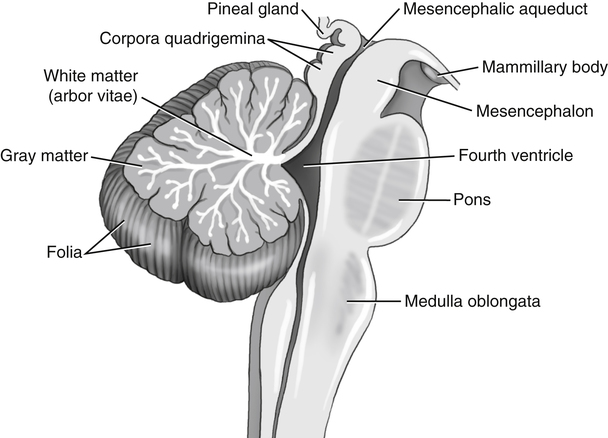
The brainstem is the lower part of the brain where it connects to the spinal cord. It consists of the midbrain, pons, and the medulla oblongata (Fig. 6-4). Most of the cranial nerves originate in the brainstem. Many neurologic functions of particular importance to the RT, such as regulation of heart rate, blood pressure, and breathing, are located in the brainstem. In addition, the brainstem contains reflex centers for certain cranial nerve functions such as the pupillary reflex, which is discussed later in this chapter. Lesions in the brainstem can cause a wide range of breathing problems from hyperventilation to apnea.
The spinal cord lies within the center of the vertebral bodies and extends from the base of the brain down to the level of the first lumbar (L1) vertebra (see Fig. 6-1). The rest of the space between the vertebral bodies is taken up by the loose collection of the nerve roots that originate in the lower portion of the spinal cord and the cerebrospinal fluid (see Lumbar Puncture). This collection of nerve roots is called the cauda equina (Latin for horse’s tail). The fact that the spinal cord does not extend below L1 will become important when we discuss the anatomy of lumbar puncture. The spinal cord spans a distance of approximately 45 cm in the average adult. It serves the purpose of connecting the brain to the various parts of the body for motor and sensory function. It is an oval cylinder that has two tapering bulges: one in the cervical region and one in the lumbar region. The bulges are formed by the accumulation of extra neurons for the innervations of the upper and lower extremities, respectively.
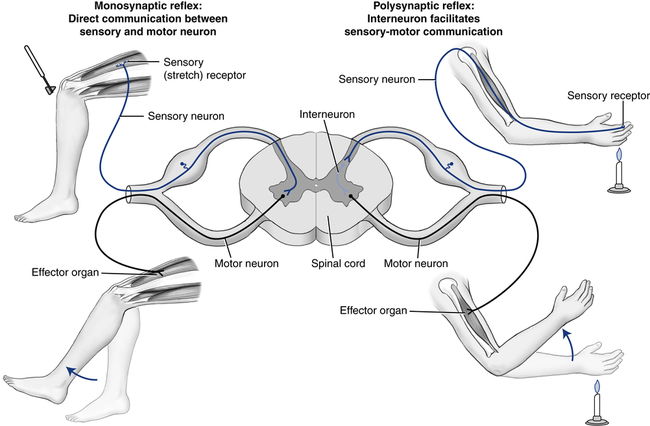
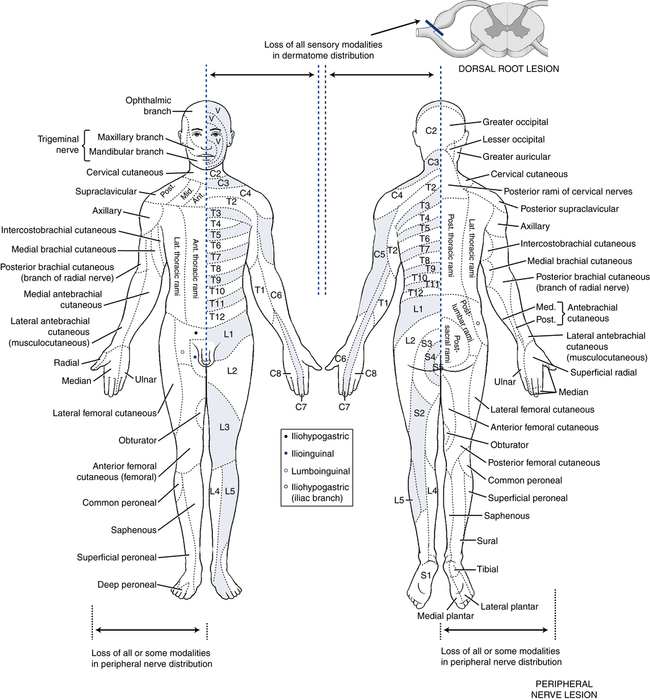
Two sets of nerve fibers called spinal nerves project from both sides of the spinal column at 31 locations along the spine. Sensory and motor nerve roots separate as they exit the spinal cord until their fibers combine at the level of the dorsal root ganglion. The dorsal nerve root consists of posterior nerve fibers that carry sensory information into the spinal cord. The ventral nerve root consists of anterior nerve fibers that conduct motor impulses out of the spinal cord. Because all spinal nerves contain both motor and sensory fibers, they are called mixed nerves. Each has the ability to provide sensory input to the brain (e.g., feel pain) and the ability to cause muscle movement (e.g., extend the arm on command) (Fig. 6-5).
A herniated vertebral disk is the most common nerve root pathology that results in compression on the nerve roots. This usually results in pain with radiation into the affected area of skin (dermatome) supplied with afferent nerve fibers by a single posterior spinal root (Fig. 6-6).
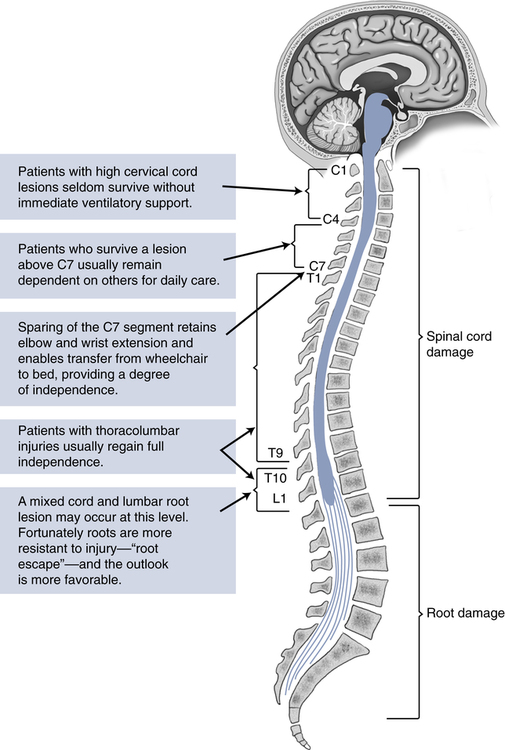
Two spinal nerves important for respiratory function are the right and left phrenic nerves that innervate the diaphragm to control breathing. The phrenic nerves arise from the cervical spine roots of C3 to C5. Damage to this portion of the spinal cord (or above) can result in complete paralysis of the diaphragm as well as the intercostal muscles and make the patient dependent on a ventilator for life. The additional muscles of respiration, such as intercostal muscles, are innervated by the spinal nerves that originate in the thoracic portion of the spinal cord. These nerves, although normal, will be cut off from the efferent impulses originating above the injury (C3 to C5 level, or above) and will be rendered ineffective. Figures 6-6 and 6-7 illustrate the typical outcome after spinal cord or root injury.
Assessment of Consciousness
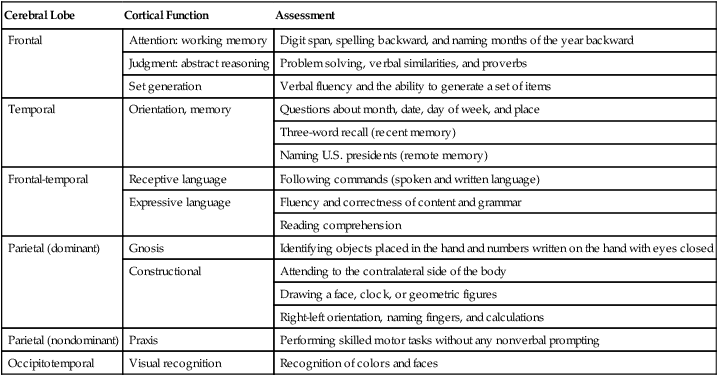
The cerebral hemispheres (or lobes) represent the highest and most complex level of neurologic function. Although a great deal of the mental status reflects integration of cortical function, it can still be divided into functional areas that correspond to anatomic regions of the cerebral hemispheres (Fig. 6-8). Table 6-1 gives a brief overview of areas of cortical function that can be assessed by components of the mental status examination.
TABLE 6-1
Assessment of Cerebral Cortical Function
| Cerebral Lobe | Cortical Function | Assessment |
| Frontal | Attention: working memory | Digit span, spelling backward, and naming months of the year backward |
| Judgment: abstract reasoning | Problem solving, verbal similarities, and proverbs | |
| Set generation | Verbal fluency and the ability to generate a set of items | |
| Temporal | Orientation, memory | Questions about month, date, day of week, and place |
| Three-word recall (recent memory) | ||
| Naming U.S. presidents (remote memory) | ||
| Frontal-temporal | Receptive language | Following commands (spoken and written language) |
| Expressive language | Fluency and correctness of content and grammar | |
| Reading comprehension | ||
| Parietal (dominant) | Gnosis | Identifying objects placed in the hand and numbers written on the hand with eyes closed |
| Constructional | Attending to the contralateral side of the body | |
| Drawing a face, clock, or geometric figures | ||
| Right-left orientation, naming fingers, and calculations | ||
| Parietal (nondominant) | Praxis | Performing skilled motor tasks without any nonverbal prompting |
| Occipitotemporal | Visual recognition | Recognition of colors and faces |
Assessing Consciousness
Assessment of consciousness begins when you first encounter the patient. A neurologically healthy patient will be awake and interacting with those around. If asleep, the patient can be easily aroused to an awake, alert state. Different levels of consciousness from full alertness to coma have been defined (Box 6-1). These and other terms used to categorize consciousness are frequently used imprecisely, so it is often recommended to avoid using them. Instead, a brief description of the applied stimulus and arousal pattern is preferred.
Glasgow Coma Scale
The Glasgow Coma Scale (GCS) was published in 1974 by Graham Teasdale and Bryan J. Jennett at the University of Glasgow as the neurologic assessment tool in patients with head injury. It has multiple limitations outside of its initial scope in acute traumatic brain injury patients, especially in ICU patients, but the simplicity of the scale makes it widely useful for nearly every member of the health care team from emergency medical services personnel for initial evaluation to ICU staff in daily neurologic assessment. The GCS is commonly incorporated in other, more complex and comprehensive acute illness scoring systems in the ICU. It is the most widely used instrument for quantifying neurologic impairment. The GCS is used to test best motor response, best verbal response, and eye opening. Although it is easy to perform and readily reproducible, it is poorly suited to patients who have impaired verbal responses caused by aphasia, hearing loss, or tracheal intubation or more subtle alterations of consciousness, such as delirium. A scale that goes from 3 (deep coma or death) to 15 (fully awake) is useful for rapid triage (Table 6-2). Endotracheal intubation makes it impossible to test the patient’s verbal response, so the letter “T” is often attached to the GCS score to indicate the presence of the tube (e.g., GCS 5T).
TABLE 6-2
| Action | Response | Score |
| Eyes open | Spontaneously | 4 |
| To speech | 3 | |
| To pain | 2 | |
| None | 1 | |
| Best verbal response | Oriented | 5 |
| Confused | 4 | |
| Inappropriate words | 3 | |
| Incomprehensive sounds | 2 | |
| Best motor response | Obeys commands | 6 |
| Localized pain | 5 | |
| Flexion withdrawal | 4 | |
| Abnormal flexion | 3 | |
| Abnormal extension | 2 | |
| Flaccid | 1 | |
| Total | 15 |