4 Neuro-ophthalmology
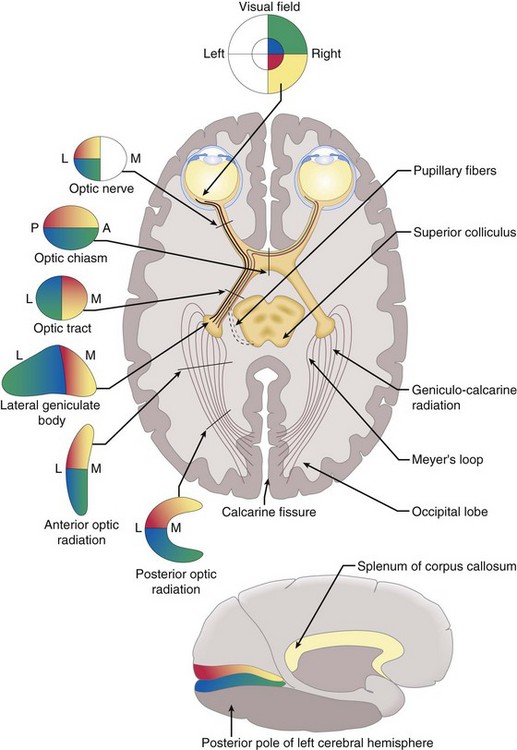
Anatomy of the Visual Pathway
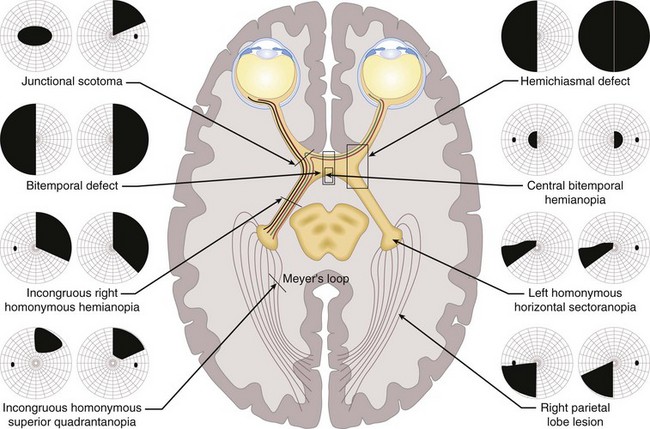
Optic nerve → chiasm → optic tract → lateral geniculate body → optic radiation → occipital lobe (Figure 4-1)
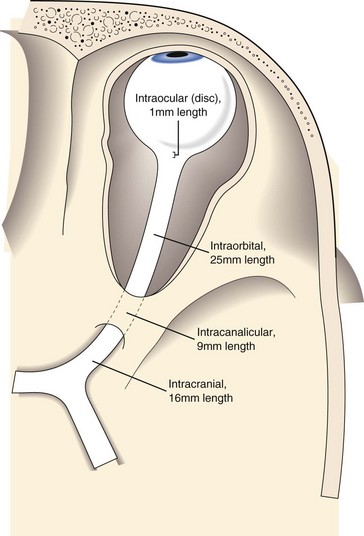
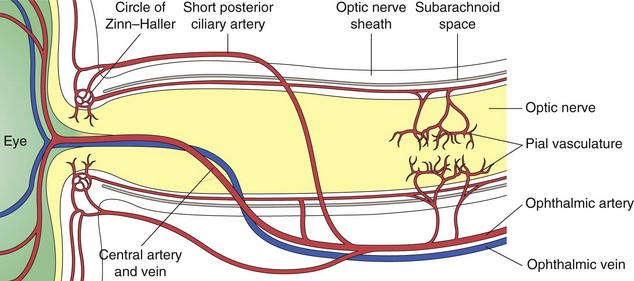
Optic nerve
composed of 1.2 million nerve fibers; approximately 1.5 mm in diameter, enlarges to 3.5 mm posterior to lamina cribrosa due to myelin sheath; located 3–4 mm from fovea; causes absolute scotoma (blind spot) 15° temporal to fixation and slightly below horizontal meridian; approximately 45-50 mm in length (1 mm intraocular, 25 mm intraorbital, 9 mm intracanalicular, 10–15 mm intracranial) (Figure 4-2); acquires myelin posterior to lamina cribosa
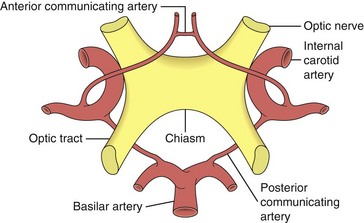
Chiasm
Optic tract
Lateral geniculate body
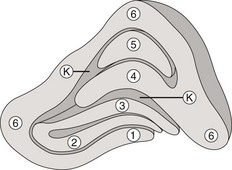
part of the thalamus (Figure 4-5)
Optic radiation
myelinated nerve fibers; connect LGB to occipital cortex
Primary visual cortex (striate cortex, V1, Brodmann’s area 17)
medial face of occipital lobe, divided horizontally by calcarine fissure
Other areas
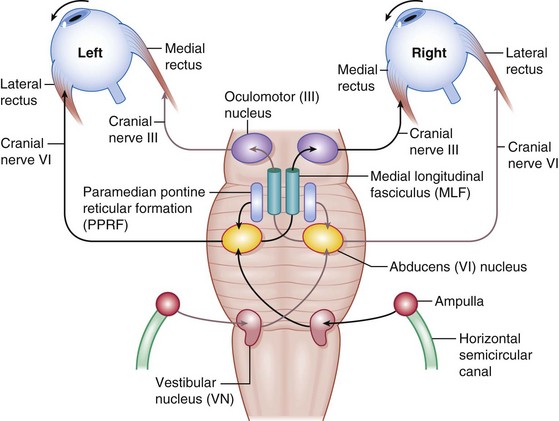
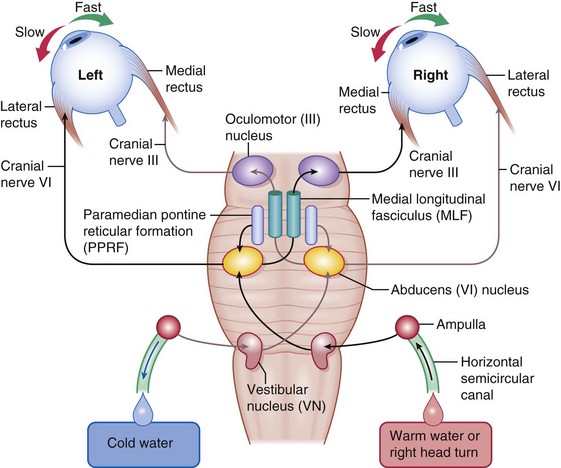
Figure 4-6 Horizontal eye movement pathways.
(From Bajandas FJ, Kline LB: Neuro-Ophthalmology Review Manual. Thorofare, NJ, Slack, 1988.)
Physiology
Testing
Color vision tests
Ishihara pseudoisochromatic or Hardy-Rand-Ritter plates; Farnsworth tests
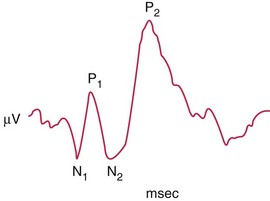
Visually evoked cortical potentials / responses (VEP, VER)
measure macular visual function, integrity of primary and secondary visual cortex, and continuity of optic nerve and tract radiations; fovea has large area in occipital cortex, close to recording electrodes; smaller area representing more peripheral retina lies deep within calcarine fissure (Figure 4-8)
Optokinetic nystagmus (OKN)
presence suggests visual input is present; slow phase is noted in direction of moving stimulus
Can use to diagnose functional visual loss
Visual Field (VF) Defects (Figure 4-9)
Types
Neurologic VF defects
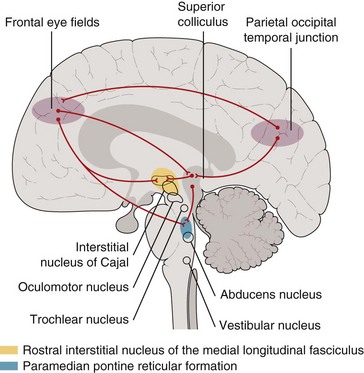
Eye Movements under Supranuclear Control
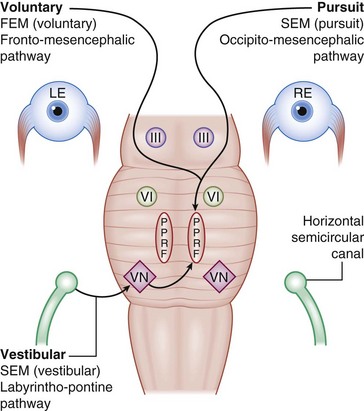
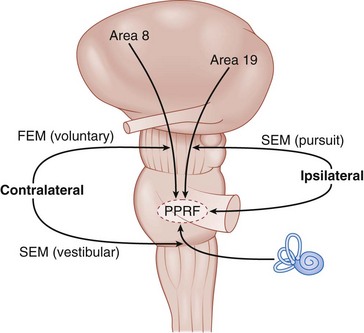
Horizontal gaze center (Figures 4-10,4-11)
Saccadic system
Nonoptic reflex systems
integrate eye movements with body movements
Diplopia
Etiology
Differential diagnosis (DDx)
Eye Movement Disorders
Central Disorders (Supranuclear) (Figure 4-13)
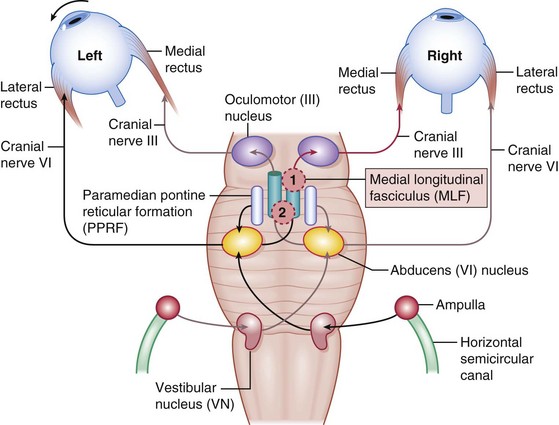
Horizontal Gaze Palsies
Möbius’ Syndrome
Horizontal gaze palsy with CN 6, 7, 8, and 9 palsies (facial diplegia, deafness, abnormal digits)
Ocular Motor Apraxia
Acquired
Pseudogaze palsies
myasthenia gravis, chronic progressive external ophthalmoplegia (CPEO), Duane’s syndrome
Internuclear ophthalmoplegia (INO) (Figure 4-14)
Vertical Gaze Abnormalities
Parinaud’s Syndrome (Dorsal Midbrain Syndrome)
Skew Deviation
Vertical misalignment of visual axes due to imbalance of prenuclear inputs; comitant or incomitant
Whipple’s Disease
Oculomasticatory myorhythmia (vertical eye movements and facial activity similar to myoclonus)
Nystagmus
Childhood Nystagmus
Most commonly, congenital, latent, sensory, and spasmus nutans (see Ch. 5, Pediatrics / Strabismus)
Physiologic Nystagmus
Several forms of nystagmus, including end-gaze, optokinetic, caloric, and rotational
Acquired Nystagmus
Pattern helps localize pathology, may have oscillopsia
Convergence-Retraction
Cocontraction of lateral recti produces convergence movement (abnormal saccades) on attempted upgaze
Dissociated
Asymmetric between the 2 eyes (different direction, amplitude, frequency, etc); always pathologic
Gaze-Evoked
Nystagmus in direction of gaze, absent in primary position, fast phase toward lesion (cerebellar)
Other Eye Movement Disorders
Ocular Bobbing
Intermittent conjugate rapid downward eye movements followed by slow return to primary position
Cranial Nerve Palsies (FIGURE 4-16)
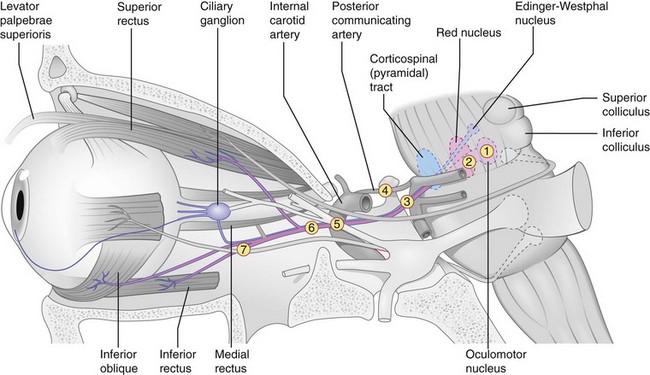
Oculomotor Nerve (CN 3) Palsy
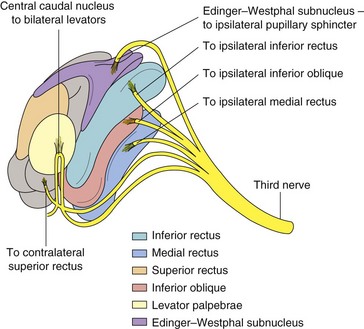
Anatomy
Only 1 subnucleus (midline location) supplies both levator palpebrae superioris; fibers from superior rectus (SR) subnucleus supply contralateral SR; Edinger-Westphal nucleus supplies both pupils (Figure 4-18)
7 syndromes (Figure 4-17)
 ): extremely rare; contralateral SR paresis and bilateral ptosis; pupil involvement is both or neither
): extremely rare; contralateral SR paresis and bilateral ptosis; pupil involvement is both or neither ): ischemic, infiltrative (tumor), or inflammatory (rare)
): ischemic, infiltrative (tumor), or inflammatory (rare)
 ): supratentorial mass may cause uncal herniation compressing CN 3
): supratentorial mass may cause uncal herniation compressing CN 3 ): most common nontraumatic, isolated, pupil involving CN 3 palsy; aneurysm at junction of PCom and carotid artery compresses nerve, particularly external parasympathetic pupillomotor fibers; usually painful
): most common nontraumatic, isolated, pupil involving CN 3 palsy; aneurysm at junction of PCom and carotid artery compresses nerve, particularly external parasympathetic pupillomotor fibers; usually painful ): associated with multiple CN palsies (3, 4, V1, 6) and Horner’s; CN 3 palsy often partial and pupil sparing; may lead to aberrant regeneration
): associated with multiple CN palsies (3, 4, V1, 6) and Horner’s; CN 3 palsy often partial and pupil sparing; may lead to aberrant regeneration ): tumor, trauma, pseudotumor, or cellulitis; associated with multiple CN palsies (3, 4, V1, 6), proptosis, chemosis, injection; ON can appear normal, swollen, or atrophic
): tumor, trauma, pseudotumor, or cellulitis; associated with multiple CN palsies (3, 4, V1, 6), proptosis, chemosis, injection; ON can appear normal, swollen, or atrophic ): small-caliber parasympathetic pupillomotor fibers travel in outer layers of nerve closer to blood supply (but more susceptible to damage by compression); fibers at core of nerve are compromised by ischemia; may explain pupil sparing in 80% of ischemic CN 3 palsies and pupil involved in 95% of compressive CN 3 palsies (trauma, tumor, aneurysm)
): small-caliber parasympathetic pupillomotor fibers travel in outer layers of nerve closer to blood supply (but more susceptible to damage by compression); fibers at core of nerve are compromised by ischemia; may explain pupil sparing in 80% of ischemic CN 3 palsies and pupil involved in 95% of compressive CN 3 palsies (trauma, tumor, aneurysm)
Aberrant regeneration
Other causes of CN 3 palsy
Workup
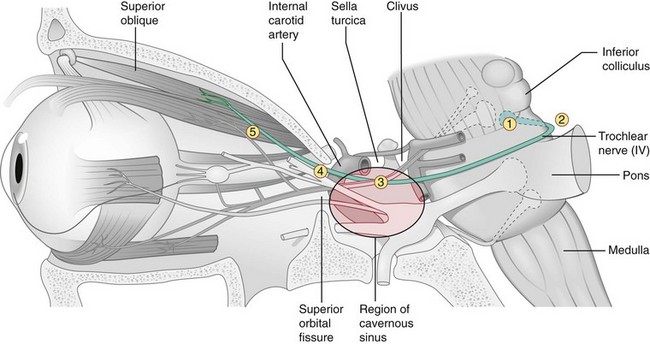
Trochlear Nerve (CN 4) Palsy
5 syndromes (Figure 4-19)
 ): hemorrhage, infarction, demyelination, trauma; may have contralateral Horner’s or INO
): hemorrhage, infarction, demyelination, trauma; may have contralateral Horner’s or INO ): injury as nerve emerges from dorsal surface of brain stem; trauma (contracoup forces transmitted to brain stem by free tentorial edge), tumor (pinealoma, tentorial meningioma), meningitis, neurosurgical trauma
): injury as nerve emerges from dorsal surface of brain stem; trauma (contracoup forces transmitted to brain stem by free tentorial edge), tumor (pinealoma, tentorial meningioma), meningitis, neurosurgical trauma ): multiple CN palsies (3, 4, V1, 6) and Horner’s; proptosis, chemosis, injection
): multiple CN palsies (3, 4, V1, 6) and Horner’s; proptosis, chemosis, injectionDiagnosis
Parks-Bielschowsky 3-step test (used for hypertropia due to weakness of a single muscle)
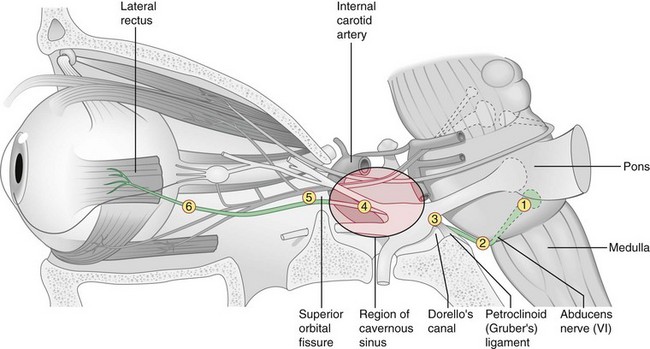
Abducens Nerve (CN 6) Palsy
6 syndromes (Figure 4-20)
 ):
):
 ): increased ICP can cause downward displacement of brain stem with stretching of CN 6 (tethered at exit from pons and Dorello’s canal); occurs in 30% of patients with pseudotumor cerebri; also hemorrhage, meningitis, inflammation (sarcoidosis), infiltration (lymphoma, leukemia, carcinoma)
): increased ICP can cause downward displacement of brain stem with stretching of CN 6 (tethered at exit from pons and Dorello’s canal); occurs in 30% of patients with pseudotumor cerebri; also hemorrhage, meningitis, inflammation (sarcoidosis), infiltration (lymphoma, leukemia, carcinoma) ): portion of CN 6 within Dorello’s canal is in contact with tip of petrous pyramid and is susceptible to processes affecting the petrous bone
): portion of CN 6 within Dorello’s canal is in contact with tip of petrous pyramid and is susceptible to processes affecting the petrous bone
 ):
):
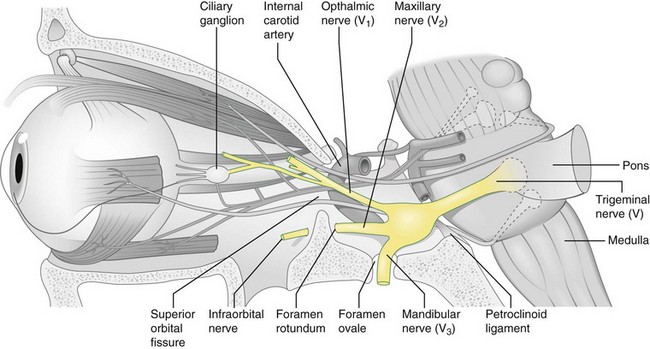
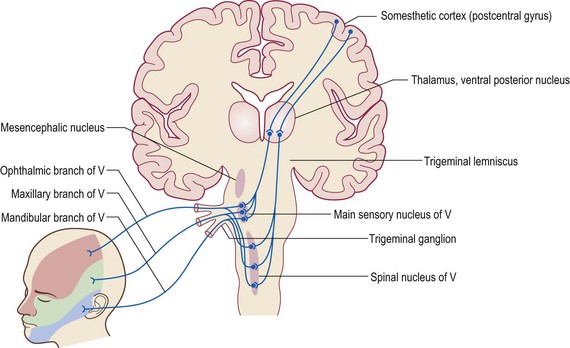
Trigeminal Nerve (CN 5) Palsy
Anatomy
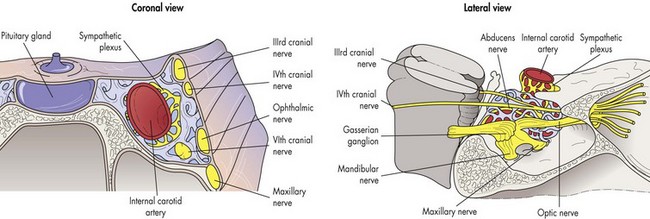
nerve emerges from ventral pons; passes below tentorium to ganglion; divides into 3 divisions (Figure 4-21)
Supplies sensory to face and eye, motor to muscles of mastication (Figure 4-22)
Facial Nerve (CN 7) Palsy
Anatomy
Supranuclear palsy
Emotional and reflex movements (smiling, spontaneous blinking) are preserved (extrapyramidal)
Brain stem lesion (pons)
ipsilateral facial weakness involving both upper and lower face; due to tumor, vascular causes
Peripheral CN 7 lesion
acute unilateral facial nerve palsy is most common cranial neuropathy
Disorders of CN 7 overactivity
Multiple CN Palsies
CN 3, 4, and 5
due to lesion of brain stem, cavernous sinus (Figure 4-24), and / or superior orbital fissure
Pupils
Innervation (Figure 4-25)
Iris Sphincter
Parasympathetic innervation from Edinger-Westphal nucleus
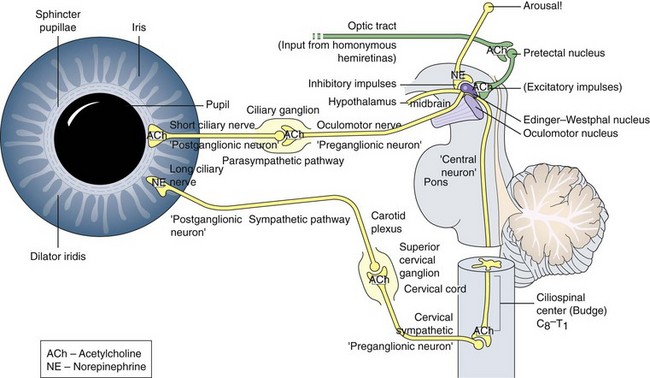
Figure 4-25 Parasympathetic and sympathetic innervation of the iris muscles.
(From Kardon RH: The pupils. In: Yanoff M, Duker JS (eds) Ophthalmology, 2nd edn. St Louis, Mosby, 2004.)
Disorders
Anisocoria
Horner’s Syndrome
Preganglionic
from hypothalamus to superior cervical ganglion
Postganglionic
superior cervical ganglion to iris dilator
Argyll-Robertson Pupil
Bilateral small, irregular pupils with light-near dissociation caused by tertiary syphilis
Ocular Muscle Disorders
Ophthalmoplegia
Progressive
Episodic
Myasthenia Gravis (MG)
Other findings
jaw weakness, dysphagia, dysarthria, dyspnea, muscle bulk usually preserved until late
DDx
Myotonic dystrophy, CPEO, involutional ptosis, toxins (snake, arthropod, bacteria [botulism])
Diagnosis
Eye Movements In Coma
Optic Nerve
Optic Disc Swelling
Orthograde transport (ganglion cells to LGB): slow component = 2 mm/day; fast component = 500 mm/day
Idiopathic Intracranial Hypertension (IIH; Pseudotumor Cerebri)
Papilledema with normal neuroimaging and CSF
90% female, mean age = 33 years old; associated with obesity
Optic Neuritis
Other findings
Treatment
Major Clinical Study
Optic Neuritis Treatment Trial (ONTT)
Optic Neuropathies
Anterior Ischemic Optic Neuropathy (AION)
Arteritic:
Traumatic Optic Neuropathy
ON Tumors
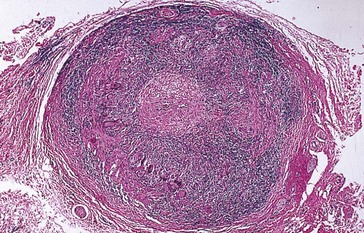
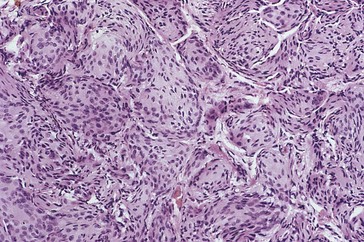
ON Glioma (Figure 4-27)
Low-grade astrocytoma
usually in children aged <10 years
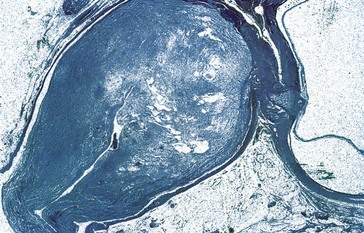
Figure 4-27 Glioma demonstrating central necrosis.
(From Yanoff M, Fine BS 2002 Ocular Pathology, 5th edn. Mosby, St Louis.)
‘Benign’ but 14% mortality rate (highest with hypothalamus involvement)
10–50% have neurofibromatosis (15% of patients with NF have ON gliomas)
Chiasm Compression
Meningioma
Pituitary Apoplexy
Acute hemorrhage and expansion of a pituitary tumor, usually secondary to ischemic necrosis
Craniopharyngioma
Usually causes compression of chiasm from above and behind; occurs in children and young adults
Retrochiasmal Disorders
Cause homonymous VF defects (see Figure 4-9)
Cortical Lesions
Disorders During Pregnancy
Brain Tumors
(Table 4-1)
| By origin: | |
| Glial (gliomas) | Astrocytoma |
| Neuronal | Neuroblastoma, medulloblastoma |
| Connective tissue | Sarcoma |
| Lymphoreticular | Primary (non-Hodgkin’s) CNS lymphoma |
| Blood vessels | Hemangioma, angioma |
| Bone | Osteoma |
| Neural crest Congenital rests: Notochord Adipose cells Ectodermal derivatives Glands: Pituitary gland Pineal gland |
Meningioma (arachnoid cells), primary CNS melanoma |
| Chordoma | |
| Lipoma | |
| Craniopharyngioma, teratoma, dermoid | |
| Adenoma | |
| Pineocytoma, pineoblastoma, germ cell tumors | |
| By age: | |
| <20 years old | CNS tumors are second most common type of malignancy (leukemia is first); approximately 66% located in posterior fossa; gliomas of cerebellum, brain stem, optic nerve; pinealomas; primitive neuroectodermal tumors; craniopharyngiomas |
| 20–60 years old | Meningiomas, gliomas of cerebral hemispheres, pituitary tumors |
| >60 years old | Malignant gliomas, metastases |
Headaches
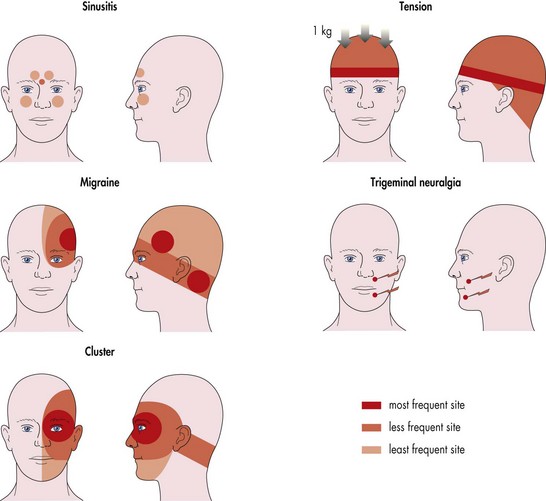
Figure 4-29 Location of pain for the common headache syndromes.
(From Weinstein JM: Headache and facial pain. In: Yanoff M, Duker JS (eds) Ophthalmology. London, Mosby, 1999.)
Migraines
Types
Precipitating factors
Treatment
Temporomandibular Joint (TMJ) Syndrome
Unilateral ear or preauricular pain, radiates to temple, jaw, or neck; worse with chewing
Visual Disturbances
Functional Visual Loss
Transient Visual Loss
Visual Obscurations
Last seconds; occur in papilledema (change in posture or eye movement) or optic disc drusen
Vascular Disorders
Cerebral Aneurysm
Occurs in 5% of population; rarely symptomatic before age 20; associated with hypertension
Location
Findings
Treatment
Carotid Artery Dissection
Etiology
Findings
Vertebrobasilar Dissection
40% of all dissecting aneurysms; basilar more common than vertebral
Cerebral blindness / cortical blindness
Bilateral occipital lobe lesions; pupils react normally; may deny blindness (Anton’s syndrome)
Cerebral Venous and Dural Sinus Thrombosis
Cavernous sinus thrombosis
aseptic or septic (infection of sinus or face; rarely otitis or orbital cellulitis)
Lateral sinus thrombosis
Superior sagittal sinus (SSS) thrombosis
Intracranial Arachnoid Cyst
Congenital malformation: CSF-filled cyst most commonly in middle cranial fossa (Sylvian fissure)
Neuro-Ophthalmic Manifestations of Aids
Review Questions (Answers start on page 359)
American Academy of Ophthalmology. Neuro-ophthalmology. vol 5. 2012. AAO. San Francisco.
Burde RM, Savino PJ, Trobe JD. Clinical Decisions in Neuro-ophthalmology, 3rd edn. Philadelphia: Mosby; 2002.
Kline LB, Bajandas F. Neuro-ophthalmology Review Manual, 6th edn. Thorofare, NJ: Slack; 2007.
Liu GT, Volpe NJ, Galetta S. Neuro-ophthalmology Diagnosis and Management. Philadelphia: WB Saunders; 2001.
Loewenfeld IE, Lowenstein O. The Pupil Anatomy: Physiology and Clinical Applications, 2nd edn. Philadelphia: Butterworth-Heineman; 1999.
Milder B, Rubin ML, Weinstein GW. The Fine Art of Prescribing Glasses Without Making a Spectacle of Yourself. Gainesville, FL: Triad Scientific Publications; 1991.
Miller NR, Newman NJ. Walsh & Hoyt’s Clinical Neuro-ophthalmology, 5th edn. Baltimore, MD: Lippincott Williams and Wilkins; 1999.
Walsh TJ. Neuro-ophthalmology: Clinical Signs and Symptoms, 4th edn. Baltimore, MD: Williams and Wilkins; 1997.

 of tongue
of tongue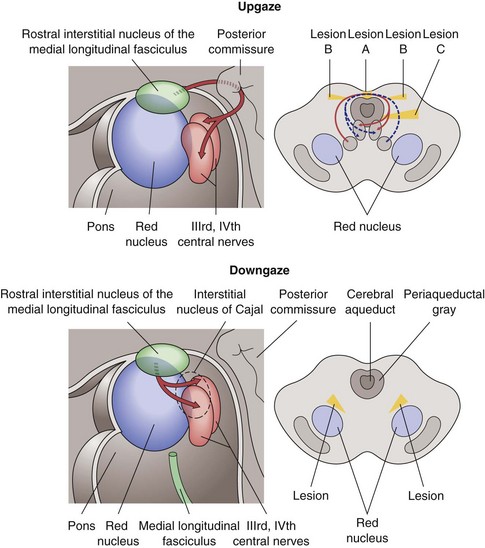
 syndrome may develop oculopalatal myoclonus
syndrome may develop oculopalatal myoclonus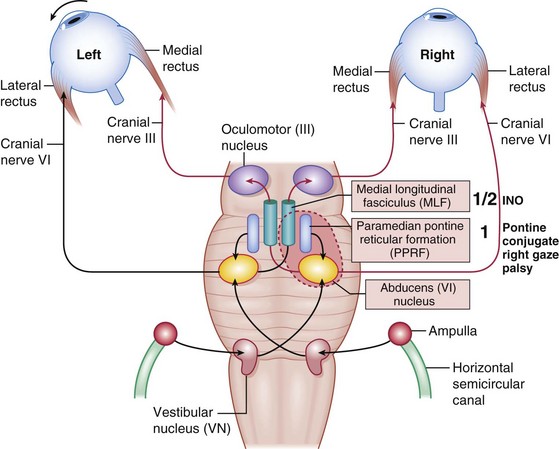
 syndrome (paralytic pontine exotropia).
syndrome (paralytic pontine exotropia).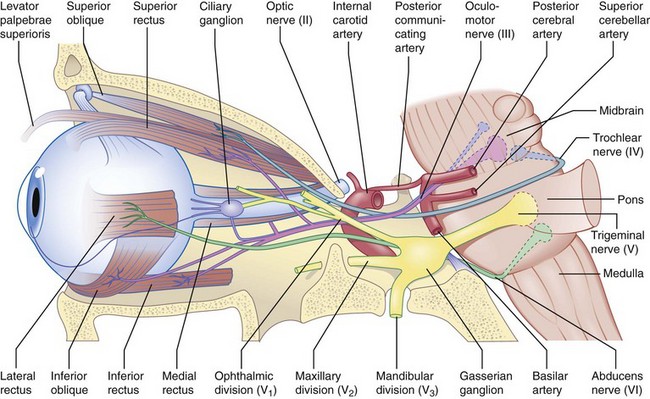
 ): multiple CN palsies (3, 4, V1, 6) and Horner’s
): multiple CN palsies (3, 4, V1, 6) and Horner’s ):
):
 ):
):
 ):
):
 of tongue; external ear sensation; dampens stapedius
of tongue; external ear sensation; dampens stapedius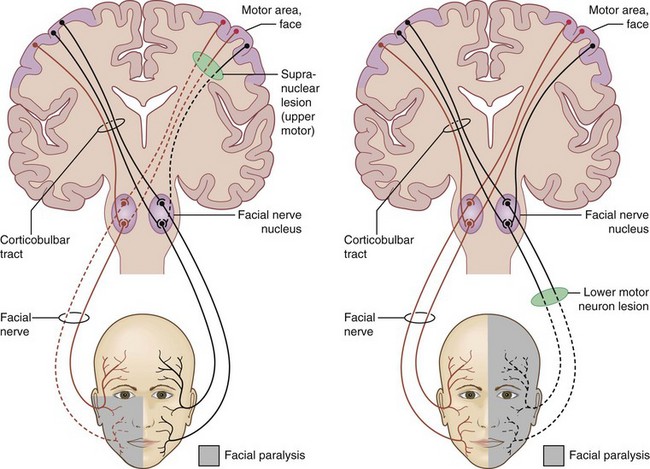
 syndrome is
syndrome is