CHAPTER 243 Nerve Injuries of the Lower Extremity
Epidemiology
It is commonly recognized that traumatic injury of the lower extremity nerves is less common than injury to the upper extremity nerves. In a recent review of lower extremity nerve injuries in Wroclaw, Poland,1 the incidence of lower extremity nerve injuries was 20% of upper extremity nerve injuries. Irrespective of series, the peroneal nerve was the single most common lower extremity nerve to be injured.
All the mechanisms of nerve damage, stretch, contusion, laceration, and compression may be in play in the lower extremity, together or in isolation. Throughout the leg, the relative mix of these mechanisms will vary. For those injuries in the pelvis, surgical options will be significantly limited; elsewhere, the decision making, management, and surgical treatment of lower extremity injuries will be similar to that in the upper extremity, whereas mechanisms and results will vary from location to location. Unfortunately, intraoperative iatrogenic injuries to all nerves of the lower extremity occur. They will be included as traumatic injuries to lower extremity nerves as well. For uniformity and consistency of reporting, all grades of motor recovery calculated originally by the Louisiana State University Health Sciences Center (LSUHSC) system will be transposed into the British Medical Research Grading (BMRC) system2 (Table 243-1) given its nearly universal acceptance. For descriptions of the standard anatomy of individual nerves, the reader is referred to Sunderland’s Nerve and Nerve Injuries.3
TABLE 243-1 British Medical Research Council Scale of Muscle Recovery for Entire Nerve2,85
| M0 | No contraction |
| M1 | Return of perceptible contraction in proximal muscles |
| M2 | Return of perceptible contraction in proximal and distal muscles |
| M3* | All important muscles contract against resistance |
| M4 | All synergistic and independent movements are possible |
| M5 | Full recovery of all muscles |
* A grade of 3 for an individual muscle is only contraction against gravity.
From Medical Research Council. Aids to the Examination of the Peripheral Nervous System [pamphlet]. Memorandum No. 45. London, Her Majesty’s Stationery Office; 1976; and Seddon H. Peripheral Nerve Injuries. Medical Research Council Special Report, Series No. 282. London: Her Majesty’s Stationery Office; 1954.
Lumbosacral Plexus Injuries
Traumatic nerve avulsion injuries of the lumbar and sacral roots are usually seen in severe fractures of the sacrum and pelvis. Only 61 cases of frank root avulsion are documented in the English-speaking literature,4 mostly associated with lumbar and pelvic fractures. The development of a pseudomeningocele (Fig. 243-1) gives evidence of such an avulsion. Furthermore, the nerves and plexus may be injured distal to the exiting nerve roots. Many posttraumatic cases remain undiagnosed because of the high mortality in this patient population. Huittinen5 performed autopsies on 42 fatalities with pelvic fractures and established that 20 patients (48%) had evidence of injury to the lumbosacral plexus.6
In the past, these injuries (Fig. 243-2) were considered inoperable, and no specific treatment directed at nerve repair was offered. More recently, this position has been challenged with the strategies of nerve transfer and nerve grafting.7 Although these approaches remain experimental, they represent an advance beyond the previous nihilist approach to high lumbosacral injuries.
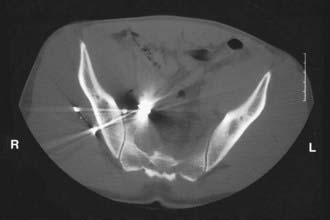
FIGURE 243-2 Gunshot injury to right lower extremity associated with a lumbosacral plexus injury. No operative repair was offered.
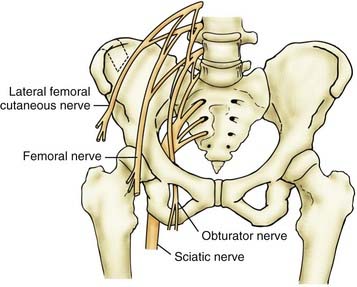
Obturator Nerve
The obturator nerve (Fig. 243-3) is the only nerve of the pelvis to pass through the pelvis without innervating any pelvic structures. This nerve is infrequently affected by external trauma, and the deficits, both sensory and motor, are usually mild. Injury to this nerve has been associated with total hip arthroplasties, acetabular fractures (Figs. 243-4 and 243-5),8 anterior extrusion of cement for total hip arthroplasty, and malpositioned acetabular screws. Loss of adductor function is usually well tolerated, and diminution of sensation in the medial thigh obturator distribution rarely causes significant deficit. Nevertheless, such a deficit has been reported in a few cases as causing significant disability.9
Femoral Nerve
The femoral nerve (see Fig. 243-3) is largely protected by its retroperitoneal position from most daily external trauma but is subject to a number of injuries (Table 243-2). Penetrating injuries to the groin can damage the nerve and may be associated with life-threatening injuries to both the femoral artery and vein.10 Pelvic fractures can sometimes be associated with femoral nerve injuries,11 including acetabular fractures.12 Similarly, missile injuries to the retroperitoneum and proximal thigh can result in injury to the femoral nerve.11,13,14–16 In a civilian practice, however, most injuries to the femoral nerve are iatrogenic16,17 and have been associated with abdominal hysterectomy for more than a century18–21 as well as with oophorectomy,22 renal transplantation,23 abdominal and pelvic laparoscopic procedures,24 laparoscopic hernia repair,25,26 and aortic surgery.27 Although sciatic injuries are more common with total hip arthroplasty (THA) and represent 80% of THA-associated nerve injuries, femoral nerve injury can also result from this procedure. The anterior extrusion of cement with exothermic femoral nerve coagulation has been shown to be a mechanism for injury.28,29 In addition, secondary iliacus hematomas have also been reported as causative factors in operative and postoperative femoral palsies associated with THA.30 The nerve may also be injured by nearby femoral artery31,32 or vein33,34 catheterization. Iliacus hematoma can occur in relationship to minor trauma (Fig. 243-6) and normal coagulation status35,36 as well as secondary to anticoagulation therapy37 or hemophilia.38 Although unusual, femoral injury has also been reported as a complication of injection injury or toxic reaction to local anesthetic.39
Surgery
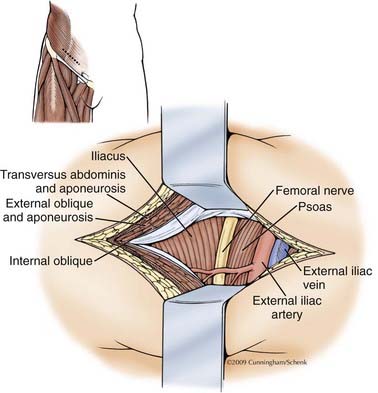
Surgery is divided into two approaches depending on level involved: thigh-level exposure and retroperitoneal exposure (Figs. 243-7 and 243-8). The inguinal ligament separates the exposable area. By a combination of approaches, the inguinal ligament is left intact, with dissection of the intervening segment achieved from both above and below. If necessary, the inguinal ligament can be divided and subsequently repaired.
Results
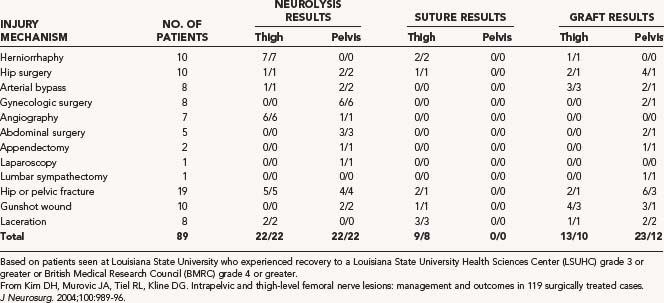
Kim and colleagues16 reported on the management of 89 traumatic injuries of the femoral nerve gathered over a 32-year period (see Table 243-2). Fifty-two patients, or 58.4% of injuries, were iatrogenic. All patients demonstrating an adequate nerve action potential (NAP) and treated by neurolysis had a successful recovery based on recovery to a LSUHSC grade 3 or better or a BMRC grade of about 4, as did those suffering injury from a lacerating mechanism. Of those injuries repaired with simple neurorrhaphy at the thigh level, 89% were judged to be successful. Of the femoral lesions that required grafting, 52% made a successful recovery. In the civilian missile category, 75% of patients had a successful recovery of thigh-level injuries, whereas only 33% of patients with pelvic-level injuries has a successful recovery. Secer,15 in his review of 40 years of treatment of missile injuries, collected 19 femoral nerve injuries separated into high, intermediate, and low categories, treated between 4 and 6 months postinjury. One patient was treated with intrafascicular nerve grafting, 9 with end-to-end suture, and 9 with neurolysis. BMRC M3 or greater motor function was reported in 78% of all femoral injuries collectively, whereas BMRC sensory recovery to S3 or greater occurred 89% of the time. Similarly, Roganovic and Pavlicevic13 reported on 15 patients suffering missile injury during the Bosnian conflict to the femoral nerve at an intermediate level, 14 of whom required graft repair and 12 of whom had grafts less than 4 cm in length. They demonstrated recovery to BMRC M3 or greater in 73% of patients.
Lateral Femoral Cutaneous Nerve
The union of the posterior branches of the L2 and L3 roots forms the lateral femoral cutaneous nerve (LFCN) (see Fig. 243-3). Tightening of the abdominal fascia and “scissoring” of the LFCN may be a mechanism responsible for compression after abdominal or gynecologic operations as well as direct injury from retractor blades on the lateral abdominal wall. Postpartum delivery injuries in the mother have also caused injury to the LFCN or exacerbated the symptoms of prior compression. LFCN injury was the most common nerve injury associated with parturition in nulliparous patients with prolonged second-stage labor.40
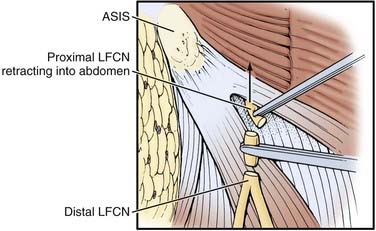
Harvesting of iliac crest in proximity to anterior superior iliac spine (ASIS) (Fig. 243-9) has been known to damage this nerve. Damage was more common with a bone graft depth of more than 30 mm. The incidence of nerve injury was 20% with graft length of more than 45 mm, 16% when graft length was between 30 and 45 mm, and 8% when graft length was less than 30 mm. It is recommended that the iliac crest graft should be no closer than 15 to 20 mm posterior from the ASIS.41 Direct external pressure on the LFCN medial to the ASIS is thought to be responsible in posterior spine operations, especially in the Relton-Hall frame.42 The symptoms after direct nerve injury may be quite persistent and unremitting in contradistinction to those complaints caused by simple compression. The natural history of meralgia paresthetica is usually one of resolution43 but rarely in large series. Postsurgical injury patients may, however, need operation. Symptomatic treatment with tricylic antidepressants or gabapentin may provide adequate relief for some. In addition, local administration of topical steroids with or without anesthetic may prove efficacious.43 After surgery has been selected, there are two operative strategies that may be offered.44 The operations for decompression are described elsewhere (see Chapter 241). For more proximal LFCN injuries, there are no simple surgical treatments to be recommended, and most education is focused on prevention. Occasionally, spinal cord stimulation has been offered45 in the absence of any direct definitive treatment. In some cases, section of the LFCN may be helpful (Fig. 243-10), but this remains a controversial treatment.
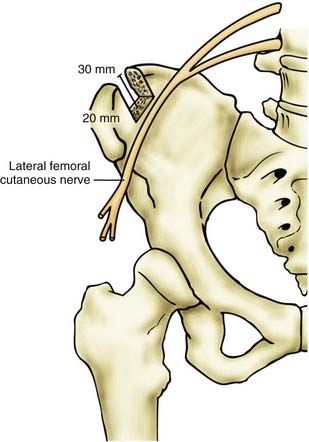
FIGURE 243-9 Diagram illustrating danger zones for lateral femoral cutaneous nerve injury with iliac crest harvesting. Damage was more common41 with a graft depth of greater than 30 mm and proximity to the anterior superior iliac spine of less than 1.5 to 2 cm.
(© M. Schenk and W. K. Cunningham, Biomedical Illustration Services, University of Mississippi Medical Center, Jackson, Mississippi.)
Sciatic Nerve
The sciatic nerve is the largest nerve of the body and arises from the L4-S3 nerve roots (Fig. 243-11). At the level of the buttock, iatrogenic injuries are more common than noniatrogenic injuries,46 with injection leading this list, followed by injuries sustained during THA.
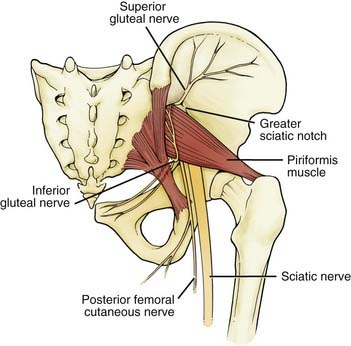
FIGURE 243-11 The emergence of the sciatic nerve under the piriformis and its descent inferiorly.
(© M. Schenk and W. K. Cunningham, Biomedical Illustration Services, University of Mississippi Medical Center, Jackson, Mississippi.)
Sciatic nerve injury has been reported in all categories of the Thompson and Epstein classification of hip fractures. The precise mechanisms of injury varies; direct femoral head compression, compression by acetabular fragments, laceration by acetabular fragments, and trapped acetabular fragments have all been described.47–49 Conversely, others have described grossly normal-appearing nerves with clinical paresis, suggesting a pure stretch mechanism.50
The surgical repair of the hip joint, THA, has also been associated with significant sciatic injury. The frequency varies among studies, ranging from 0.65% to 3.7%, but most large series average 1.7%. These rates are elevated in revision surgeries (3% to 8%) and in patients with developmental dysplasia of the hip to about 5%. With simple THA, the incidence is about 1%. Because only a severe injury presents as a clinical problem, injury may be more frequent than is generally appreciated.51 The specific etiologies are variable. Direct injury from scalpel, electrocautery, retractors, wires, reamers, Gigli saw, bone fragments, or cement protrusion; constriction by suture, wire, or cable; heat from polymerization of cement; compression from dislocation; excessive lengthening (>4 cm); and subfascial hematoma have all been reported as mechanisms of nerve injury. Still, in more than 50% of THA-associated palsies, the exact mechanism remains unknown.52
Injection injuries remain a significant source of traumatic injuries to the sciatic nerve at the buttock level.46 Most can be attributable to misplaced gluteal injections. The sciatic nerve is injured more than any other peripheral nerve in this manner. The principle cause for these injuries, as with all nerve injection injuries, is “carelessness combined with an appalling ignorance of elementary anatomy.”3 Most of these injuries result from needle insertion in the inferior medial section of the buttock instead of the superior lateral quadrant. Unfortunately, animal experiments suggest that there is little to gain by immediate surgical maneuvers such as washing the nerve or internal neurolysis.53
Surgery
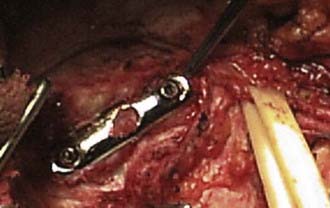
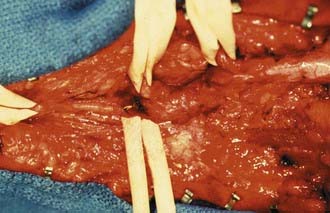
Exposure of the sciatic nerve is divided into two approaches: upper sciatic exposure for hip and buttock-level pathology (Fig. 243-12), and a lower exposure for thigh-level injuries (Fig. 243-12, inset, and Fig. 243-13). The sciatic nerve may be surgically separated both at the buttock level (Fig. 243-14) and at the thigh level, even in thick scar (Figs. 243-15 to 243-17). When even more exposure is required, the superior exposure may be connected to the inferior portion of the buttock exposure for a complete exposure of the sciatic nerve.
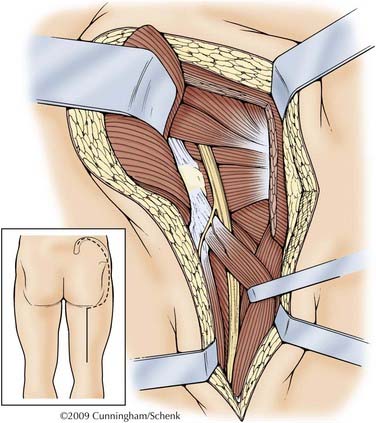
FIGURE 243-12 The proximal approach follows the general instruction of Henry.78 A “question mark” incision is used starting at the posterior superior iliac spine and running a handbreadth along the iliac spine and then turning toward the greater trochanter. This will expose the superior edge of the gluteus maximus. The lateral attachment of the gluteus maximus is then cut and elevated and further divided inferiorly. The inferior edge of the gluteus maximus is mobilized along the line of the gluteal cleft medially until the body of the gluteus maximus can be retracted medially. The sciatic nerve is then deep and medial to the gluteus maximus, often in fatty tissue coming out from under piriformis muscle.
(© M. Schenk and W. K. Cunningham, Biomedical Illustration Services, University of Mississippi Medical Center, Jackson, Mississippi.)

FIGURE 243-15 Plain radiograph of femur in missile wound showing retained bullet fragments. Patient had complete sciatic palsy.
Results
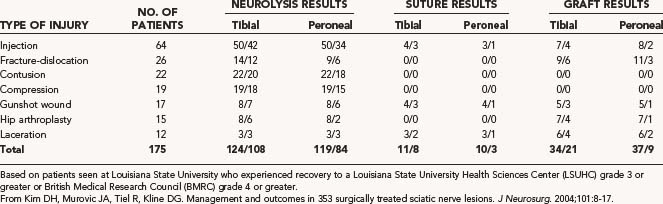
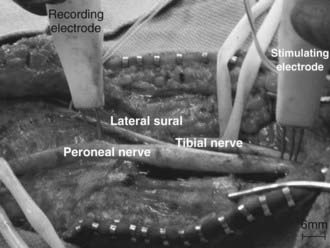
The largest reported series of sciatic injuries is the Louisiana State University (LSU) experience (Tables 243-3 and 243-4) covering more than 32 years.11 Reviewing their results, it becomes immediately apparent that recovery is more favored in the tibial distribution than the peroneal distribution and more favorable at the thigh level than at the buttock level, irrespective of mechanism of injury. This differential in recovery has also been shown by Roganovic and Pavlicevic13 in missile injuries to the sciatic nerve suffered in the Bosnian conflict.
Peroneal Nerve
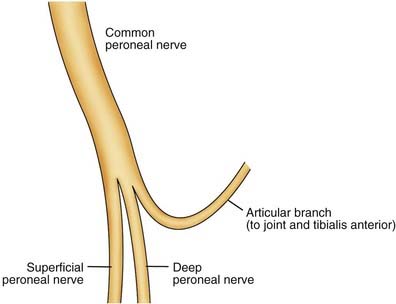
The common peroneal nerve is the most commonly injured nerve of the lower extremity. The nerve originates as the continuation of the lateral division of the sciatic nerve. This usually occurs at the junction of the upper two thirds and lower third of the thigh (Fig. 243-18).
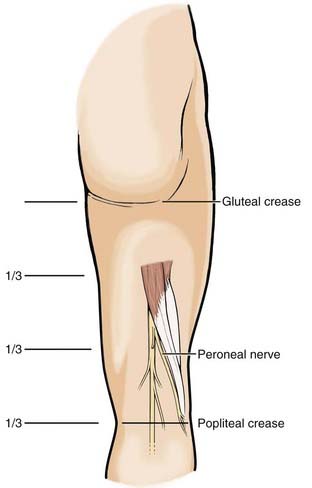
FIGURE 243-18 The peroneal nerve separates from the sciatic nerve two thirds of the way between the gluteal crease and the popliteal crease.
(© M. Schenk and W. K. Cunningham, Biomedical Illustration Services, University of Mississippi Medical Center, Jackson, Mississippi.)
Compression injury of the nerve is caused by a variety of external mechanisms. Iatrogenic injuries include tight-fitting casts,54 lithotomy position,55 and anesthetic positioning palsy.56 The bedridden state has also been associated with peroneal compression.57 Peroneal palsy is also associated with the prolonged squatting position when used during childbirth58 and when used while picking strawberries,59,60 grubbing for potatoes,61 and engaging in do-it-yourself roofing.62 Deliberate tibial bone lengthening has been associated with peroneal nerve injury.63 As long as the knee joint and its ligaments and menisci are intact, the peroneal nerve is relatively protected from excessive stretch. After the ligaments of the knee joint are disrupted, however, the nerve may be exposed to stretch greater than its intrinsic elasticity, and internal nerve injury or even nerve rupture may occur. The incidence of peroneal nerve injury in conjunction with knee dislocations has been reported to be between 14% and 40%, with most studies reporting an incidence of 25% to35%.64 Because knee dislocation may also allow popliteal artery or vein damage, it is of paramount importance to always evaluate the distal pulses.64 Nerve evaluation and repair remain secondary to viability of the affected limb.64
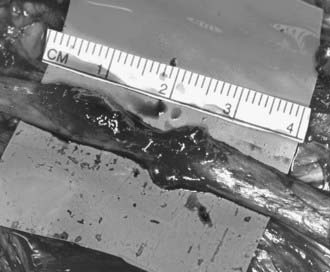
It is common for this stretch injury to result in a neuroma-in-continuity over a large distance (Fig. 243-19). With careful inspection, there is usually an associated but milder posterior tibial nerve injury. Although complete foot drop often is seen with peroneal stretch injuries, the posterior tibial examination often shows mild atrophy of the soleus and gastrocnemius, weakness of the posterior tibialis muscle, and mild weakness in toe flexion.
In cases of total knee arthroplasty, the incidence of peroneal palsy was found to be 0.87%, from a retrospective review of 2626 consecutive cases. The possible causes were thought to be direct traction on the nerve, traction on the surrounding tissue resulting in vascular compromise to the nerve, and direct pressure to the nerve from overtight bandages.65 The peroneal nerve has also been reported to be injured during knee arthroscopy.66–68 Delee in 1985 reported an overall incidence of 0.8%.69
Missile injuries also affect the peroneal nerve. Many missile wounds of the extremities can be managed nonoperatively, especially if they are caused by low-velocity missiles.70 Civilian missile wounds to the peroneal nerve are infrequent and usually of a lower velocity. In the LSU experience, missile injuries contributed to only 4% of 278 patients evaluated for peroneal-level injuries.70 Injuries caused by high-velocity missiles and closer proximity to the nerve may require surgical evaluation and treatment.
Surgery
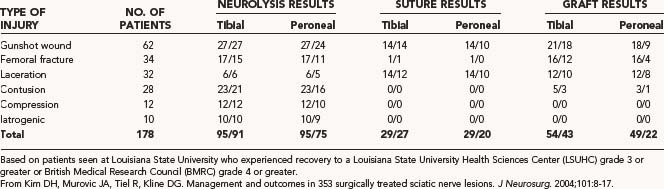
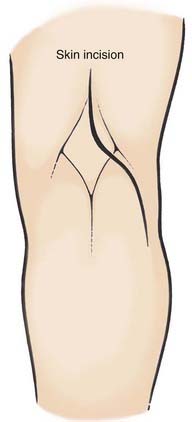
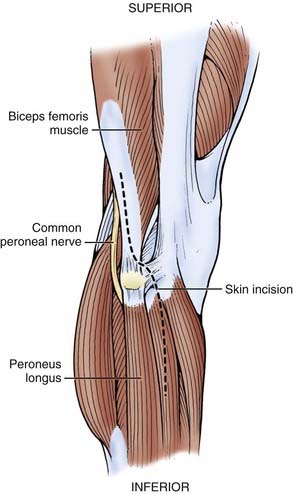
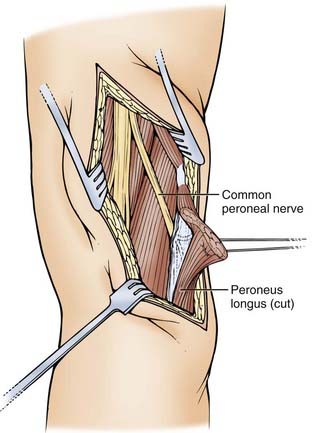
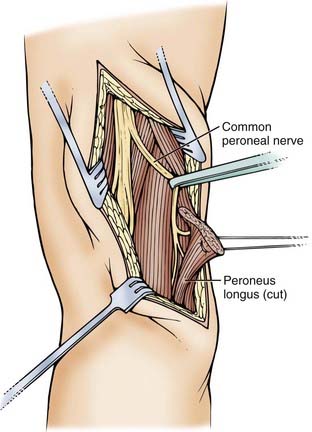
A skin incision is made starting parallel and medial to the biceps femoris tendon and extended inferiorly to the popliteal crease, where it is directed more laterally to overly the superior portion of the fibula (Figs. 243-20 to 243-24). If the nerve is lost in dense scar tissue, it may be advantageous to go distally to find the branches of the peroneal nerve under cover of the peroneus longus and dissect proximally. With the proximal and distal peroneal nerve neurolysed, dissection may proceed from either end for complete neurolysis of the damaged nerve.
The injury is evaluated (Figs. 243-25 to 243-27), NAP testing is done if indicated, and the nerve is repaired. The peroneal longus fascia is then trimmed, and the subcutaneous tissues are reapproximated. No attempt is made to close the previously divided fascial layers or reapproximate the superior edge of peroneus longus.71

FIGURE 243-25 A repaired laceration from a pet lemur bite just medial to short head of biceps above the popliteal crease. Note foot drop.
(Courtesy of Dr. Nicolas Theodore.)
Results
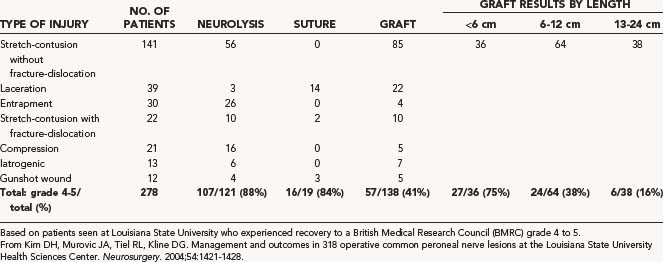
The popular image of results of treating peroneal injuries are usually described as poor, but review of the LSU data suggest that this is primarily true for the long stretch injuries requiring grafting such as knee dislocations (Table 243-5).70 The results for neurolysis70,72 and suture70 repair are generally quite acceptable, and short grafts (<6 cm) also do relatively well.70 In the series by Gousheh and colleagues73 from the Iraq-Iran war, peroneal injuries in the lower third of the thigh recovered to a BMRC grade 3 or higher more than 60% of the time irrespective of the type of surgical treatment. In Roganovic and Pavlicevic’s series, 17 of 30 patients with low peroneal injuries recovered to a BMRC grade 3 or better. Excellent recovery with long grafts has been reported by others,74 but long grafts often give discouraging results. Roganovic and Pavlicevic reported only 13.8% of patients with a high peroneal injury, making a useful recovery with graft repair of missile wounds.13
Posterior Tibial Nerve
Tibial nerve injuries are usually recognized by the inability to plantar-flex and the absence of sensation on the plantar aspect of the foot. They may also be recognized by atrophy of the foot intrinsic muscles and loss of muscle mass in the instep (Fig. 243-28) as well as by a decrease in the bulk of the posterior and fleshy gastrocnemius and soleus muscles (Fig. 243-29).

FIGURE 243-29 Marked atrophy of medial gastrocnemius and soleus muscles is seen in the same patient as in Figure 243-28.
As with other lower extremity nerves, the posterior tibial nerve is subject to all the same mechanisms of injury.75,76 Contusive compression injuries can occur (Figs. 243-30 and 243-31). Lacerations to the nerve are more common at the popliteal level, as are iatrogenic injuries associated with vascular and orthopedic operations.75 Hematoma in the popliteal fossa has been associated with posterior tibial injury.77 Lesser saphenous vein stripping has caused a complete tibial laceration.78 Both popliteus muscle rupture79,80 and strain81 have been associated with tibial nerve injury, probably from compression by a swollen popliteus muscle. Fractures of the tibia contribute significantly to injury at both the superior and inferior segments of the nerve by mechanisms of both stretch and contusion but rarely to a level requiring graft repair.75 High tibial osteotomy has also been associated with tibial nerve injury,82 probably related to intraoperative retraction. Ankle arthroscopy has also been associated with complete tibial laceration associated with overaggressive intra-articular manipulation.83
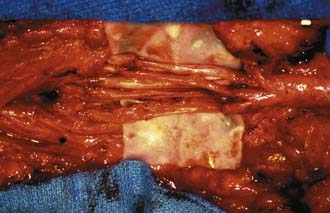
FIGURE 243-31 Same patient as in Figure 243-30 is shown after resection of neuroma and graft approximation.
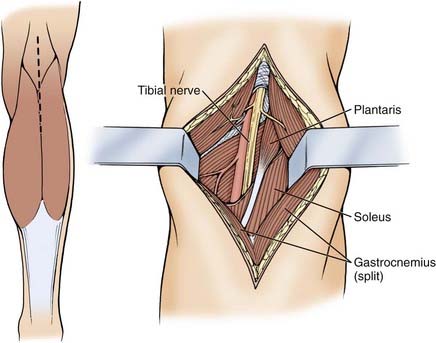
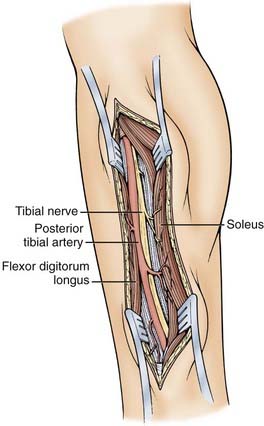
Surgery
The surgical approaches to the posterior tibial nerve can be separated into superior (Fig. 243-32) and inferior (Fig. 243-33) exposures. As with other nerves described, these exposures may be joined for a more complete exposure of the tibial nerve if indicated.
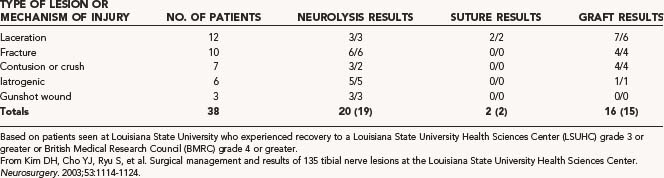
Results
The LSU experience (Table 243-6) indicates the utility of repairing these injuries.75 The reestablishment of plantar flexion and the recovery of plantar sensibility represent the primary goals of the operation. Laceration and fracture represent the most common reasons for injury to the nerve. As can be seen, good to excellent results may be expected for repair of this nerve. Roganovic and colleagues reported 85% recovery for lower-level tibial injuries associated with all surgical procedures, including neurolysis, end-to-end repair, and graft repair.84 This is a nerve where a reasonable attempt at repair should always be carried out given its favorable outcome.
Ducic I, Dellon L, Larson EE. Treatment concepts for idiopathic and iatrogenic femoral nerve mononeuropathy. Ann Plast Surg. 2005;55:397-401.
Fritzlen T, Kremer M, Biddle C. The AANA Foundation Closed Malpractice Claims Study on nerve injuries during anesthesia care. AANA J. 2003;71:347-352.
Gentili F, Hudson AR, Kline D, Hunter D. Early changes following injection injury of peripheral nerves. Can J Surg. 1980;23:177-182.
Gosk J, Rutowski R, Rabczynski J. The lower extremity nerve injuries—own experience in surgical treatment. Folia Neuropathol. 2005;43:148-152.
Henry AK. Exposures in the Lower Limb: Extensile Exposure, 2nd ed. New York: Churchill Livingstone; 1973. 180-197
Huittinen VM. Lumbosacral nerve injury in fracture of the pelvis. A postmortem radiographic and patho-anatomical study. Acta Chir Scand Suppl. 1972;429:3-43.
Kim DH, Midha R, Murovic JA, Spinner RJ. Kline & Hudson’s Nerve Injuries: Operative Results For Major Nerve Injuries, Entrapments, and Tumors, 2nd ed. Philadelphia: Saunders; 2008.
Krivickas LS, Wilbourn AJ. Peripheral nerve injuries in athletes: a case series of over 200 injuries. Semin Neurol. 2000;20:225-232.
Murata Y, Takahashi K, Yamagata M, et al. Injury to the lateral femoral cutaneous nerve during harvest of iliac bone graft, with reference to the size of the graft. J Bone Joint Surg Br. 2002;84:798-801.
Noble J, Munro CA, Prasad VSSV, Midha R. Analysis of upper and lower extremity peripheral nerve injuries in a population of patients with multiple injuries. J Trauma Injury Infect Crit Care. 1998;45:116-122.
Roganovic Z, Pavlicevic G. Difference in recovery potential of peripheral nerves after graft repairs. Neurosurgery. 2006;59:621-632.
Roganovic Z, Pavlicevic G, Petkovic S. Missile-induced complete lesions of the tibial nerve and tibial division of the sciatic nerve: results of 119 repairs. J Neurosurg. 2005;103:622-629.
Rolfe Birch G. Surgical Disorders of the Peripheral Nerves. Philadelphia: Saunders; 1998.
Rose HA, Hood RW, Otis JC, et al. Peroneal-nerve palsy following total knee arthroplasty: a review of the hospital for special surgery experience. J Bone Joint Surg Am. 1982;64:347-351.
Sunderland S. Nerve and Nerve Injuries, 2nd ed. New York: Churchill Livingstone; 1978.
Tiel RL, Happel LT, Kline DG. Nerve action potential recording method and equipment. Neurosurgery. 1996;39:103-108.
Vasilev SA. Obturator nerve injury: a review of management options. Gynecol Oncol. 1994;53:152-155.
Warner MA, Warner DO, Harper CM, et al. Lower extremity neuropathies associated with lithotomy positions. Anesthesiology. 2000;93:938-942.
1 Gosk J, Rutowski R, Rabczynski J. The lower extremity nerve injuries—own experience in surgical treatment. Folia Neuropathol. 2005;43:148-152.
2 Medical Research Council. Aids to the Examination of the Peripheral Nervous System [pamphlet]. Memorandum No. 45. London: Her Majesty’s Stationery Office; 1976.
3 Sunderland S. Nerve and Nerve Injuries, 2nd ed. New York: Churchill Livingstone; 1978.
4 Sasaka KK, Phisitkul P, Boyd JL, et al. Lumbosacral nerve root avulsions: MR imaging demonstration of acute abnormalities. Am J Neuroradiol. 2006;27:1944-1946.
5 Huittinen VM. Lumbosacral nerve injury in fracture of the pelvis. A postmortem radiographic and patho-anatomical study. Acta Chir Scand Suppl. 1972;429:3-43.
6 Huittinen VM, Slatis P. Fractures of pelvis: trauma mechanism, types of injury and principles of treatment. Acta Chir Scand. 1972;138:563.
7 Tung TH, Martin DZ, Novak CB, et al. Nerve reconstruction in lumbosacral plexopathy—case report and review of the literature. J Neurosurg. 2005;102:86-91.
8 Yang KH, Han DY, Park HW, Park SJ. Intraarticular entrapment of the obturator nerve in acetabular fracture. J Orthop Trauma. 2001;15:361-363.
9 Fricker RM, Troeger H, Pfeiffer KM. Obturator nerve palsy due to fixation of an acetabular reinforcement ring with transacetabular screws—a case report. J Bone Joint Surg Am. 1997;79:444-446.
10 Rakolta GG, Omer GE. Combat-sustained femoral nerve injuries. Surg Gynecol Obstet. 1969;128:813-817.
11 Kim DH, Murovic JA, Tiel R, Kline DG. Management and outcomes in 353 surgically treated sciatic nerve lesions. J Neurosurg. 2004;101:8-17.
12 Gruson KI, Moed BR. Injury of the femoral nerve associated with acetabular fracture. J Bone Joint Surg Am. 2003;85:428-431.
13 Roganovic Z, Pavlicevic G. Difference in recovery potential of peripheral nerves after graft repairs. Neurosurgery. 2006;59:621-632.
14 Gousheh J, Razian M. War injuries to the femoral nerve based on a series of 27 cases. Ann Chir Plast Esthet. 1991;36:527-531.
15 Secer HI, Daneyemez M, Tehli O, et al. The clinical, electrophysiologic, and surgical characteristics of peripheral nerve injuries caused by gunshot wounds in adults: a 40-year experience. Surg Neurol. 2008;69:143-152.
16 Kim DH, Murovic JA, Tiel RL, Kline DG. Intrapelvic and thigh-level femoral nerve lesions: management and outcomes in 119 surgically treated cases. J Neurosurg. 2004;100:989-996.
17 Ducic I, Dellon L, Larson EE. Treatment concepts for idiopathic and iatrogenic femoral nerve mononeuropathy. Ann Plast Surg. 2005;55:397-401.
18 Irvin W, Andersen W, Taylor P, Rice L. Minimizing the risk of neurologic injury in gynecologic surgery. Obstet Gynecol. 2004;103:374-382.
19 Morgan K, Thomas EJ. Nerve injury at abdominal hysterectomy. Br J Obstet Gynaecol. 1995;102:665-666.
20 Mcdaniel GC, Kirkley WH, Gilbert JC. Femoral nerve injury associated with Pfannenstiel incision and abdominal retractors. Am J Obstet Gynecol. 1963;87:381.
21 Gumpertz K. Narkoselahmung des nervos caurali. Dtsch Med Wochenschr. 1896;22:504-505.
22 Kumar B, Reddy KC, Kapoor T. Femoral nerve injury following oophorectomy. Br J Hosp Med. 2006;67:269.
23 Hall MC, Koch MO, Smith JA. Femoral neuropathy complicating urologic abdominopelvic procedures. Urology. 1995;45:146.
24 Barnett JC, Hurd WW, Rogers RM, et al. Laparoscopic positioning and nerve injuries. J Minim Invas Gynecol. 2007;14:664-672.
25 Keating JP, Morgan A. Femoral nerve palsy following laparoscopic inguinal herniorrhaphy. J Laparoendosc Surg. 1993;3:557.
26 Lange B, Langer C, Markus PM, Becker H. Paralysis of the femoral nerve following totally extraperitoneal laparoscopic inguinal hernia repair. Surg Endosc Other Intervent Tech. 2003;17:1157.
27 Boontje AH, Haaxma R. Femoral neuropathy as a complication of aortic surgery. J Cardiovasc Surg. 1987;28:286-289.
28 Jerosch J. Femoral nerve palsy in hip replacement due to pelvic cement extrusion. Arch Orthop Trauma Surg. 2000;120:499-501.
29 Tani Y, Miyawaki H. Femoral neuropathy caused by reinforcement ring malposition and extruded bone-cement after revision total hip arthroplasty. J Arthroplasty. 2002;17:516-518.
30 Gogus A, Ozturk C, Sirvanci M, et al. Femoral nerve palsy due to iliacus hematoma occurred after primary total hip arthroplasty. Arch Orthop Trauma Surg. 2008;128:657-660.
31 Hsin HT, Hwang JJ. Isolated femoral nerve neuropathy after intra-aortic balloon pump treatment. J Formosan Med Assoc. 2007;106:S29-S32.
32 Warfel BS, Marini SG, Lachmann EA, Nagler W. Delayed femoral nerve palsy following femoral vessel catheterization. Arch Phys Med Rehabil. 1993;74:1211-1215.
33 Kannan S. Femoral nerve palsy after femoral vein cannulation. Anesth Analg. 2000;90:1246-1247.
34 Kuruvilla A, Kuruttukulam G, Francis B. Femoral neuropathy following cardiac catheterization for balloon mitral valvotomy. Int J Cardiol. 1999;71:197-198.
35 Marquardt G, Angles SB, Leheta F, Seifert V. Spontaneous haematoma of the iliac psoas muscle: a case report and review of the literature. Arch Orthop Trauma Surg. 2002;122:109-111.
36 Pirouzmand F, Midha R. Subacute femoral compressive neuropathy from iliacus compartment hematoma 16. Can J Neurol Sci. 2001;28:155-158.
37 Baldini M, Princi L, Raimondi PL. Femoral nerve palsy secondary to anti-coagulant therapy. Neurochirurgia. 1981;24:109-110.
38 Ashrani AA, Osip J, Christie B, Key NS. Iliopsoas haemorrhage in patients with bleeding disorders—experience from one centre. Haemophilia. 2003;9:721-726.
39 Frerk CM. Palsy after femoral nerve block. Anaesthesia. 1988;43:167-168.
40 Wong CA, Scavone BM, Dugan S, et al. Incidence of postpartum lumbosacral spine and lower extremity nerve injuries. Obstet Gynecol. 2003;101:279-288.
41 Murata Y, Takahashi K, Yamagata M, et al. Injury to the lateral femoral cutaneous nerve during harvest of iliac bone graft, with reference to the size of the graft. J Bone Joint Surg Br. 2002;84:798-801.
42 Mirovsky Y, Neuwirth M. Injuries to the lateral femoral cutaneous nerve during spine surgery. Spine. 2000;25:1266-1269.
43 Khalil N, Nicotra A, Rakowicz W. Treatment for meralgia paraesthetica 1. Cochrane Database Syst Rev. 2008;3:CD004159.
44 Tiel RL. The surgical treatment of entrapment neuropathies of the lower extremity. Semin Neurosurg. 2001;12:109-123.
45 Barna SA, Cosgrove GR, Hu MM, et al. Spinal cord stimulation for treatment of meralgia paresthetica. Pain Phys. 2005;8:315-318.
46 Kline DG, Kim D, Midha R, et al. Management and results of sciatic nerve injuries: a 24-year experience. J Neurosurg. 1998;89:13-23.
47 Cornwall R, Radomisli TE. Nerve injury in traumatic dislocation of the hip. Clin Orthop Relat Res. 2000;377:84-91.
48 Armstrong J. Traumatic dislocation of the hip joint: review of one hundred and one dislocations. J Bone Joint Surg Br. 1948;30:430-435.
49 Epstein HC. Traumatic dislocations of hip. Clin Orthop Relat Res. 1973:116-142.
50 Epstein HC, Wiss DA, Cozen L. Posterior fracture dislocation of the hip with fractures of the femoral head. Clin Orthop Relat Res. 1985;201:9-17.
51 Weber E, Daube J, Coventry M. Peripheral neuropathies associated with total hip arthroplasty. J Bone Joint Surg Am. 1976;58:66-69.
52 DeHart M, Riley L. Nerve injuries in total hip arthroplasty. J Am Acad Orthop Surg. 1999;7:101-111.
53 Gentili F, Hudson AR, Kline D, Hunter D. Early changes following injection injury of peripheral nerves. Can J Surg. 1980;23:177-182.
54 Weiss APC, Schenck RC, Sponseller PD, Thompson JD. Peroneal nerve palsy after early cast application for femoral fractures in children. J Pediatr Orthop. 1992;12:25-28.
55 Warner MA, Warner DO, Harper CM, et al. Lower extremity neuropathies associated with lithotomy positions. Anesthesiology. 2000;93:938-942.
56 Fritzlen T, Kremer M, Biddle C. The AANA Foundation Closed Malpractice Claims Study on nerve injuries during anesthesia care. AANA J. 2003;71:347-352.
57 Aprile I, Caliandro P, La Torre G, et al. Multicenter study of peroneal mononeuropathy: clinical, neurophysiologic, and quality of life assessment. J Peripher Nerv Syst. 2005;10:259-268.
58 Babayev M, Bodak MP, Creatura C. Common peroneal neuropathy secondary to squatting during childbirth. Obstet Gynecol. 1998;91:830-832.
59 Seppalainen AM, Aho K, Uusitupa M. Strawberry pickers foot drop. BMJ. 1977;2:767.
60 Koller RL, Blank NK. Strawberry pickers palsy. Arch Neurol. 1980;37:320.
61 Koehler PJ. Hereditary neuropathy with liability to pressure palsies: the first publication (1947). Neurology. 2003;60:1211-1213.
62 Dawson DM, Hallett M, Wilbourn AJ, et al, 3rd ed. Philadelphia: Lippincott-Raven. 1999. 270-296
63 Nogueira MP, Paley D, Bhave A, et al. Nerve lesions associated with limb-lengthening. J Bone Joint Surg Am. 2003;85:1502-1510.
64 Johnson ME, Foster L, Delee JC. Neurologic and vascular injuries associated with knee ligament injuries. Am J Sports Med. 2008;36:2448-2462.
65 Rose HA, Hood RW, Otis JC, et al. Peroneal nerve palsy following total knee arthroplasty: a review of the hospital for special surgery experience. J Bone Joint Surg Am. 1982;64:347-351.
66 Krivic A, Stanec S, Zic R, et al. Lesion of the common peroneal nerve during arthroscopy. Arthroscopy. 2003;19:1015-1018.
67 Kim TK, Savino RM, McFarland EG, Cosgarea AJ. Neurovascular complications of knee arthroscopy. Am J Sports Med. 2002;30:619-629.
68 Johnson DS, Sharma DP, Bangash IH. Common peroneal nerve palsy following knee arthroscopy. Arthroscopy. 1999;15:773-774.
69 Delee JC. Complications of arthroscopy and arthroscopic surgery: results of a national survey. Arthroscopy. 1985;1:214-220.
70 Kim DH, Murovic JA, Tiel RL, Kline DG. Management and outcomes in 318 operative common peroneal nerve lesions at the Louisiana State University Health Sciences Center. Neurosurgery. 2004;54:1421-1428.
71 Tiel R. The surgical treatment of entrapment neuropathies of the lower extremity. Semin Neurosurg. 2001;12:109-123.
72 Mont MA, Dellon AL, Chen F, et al. The operative treatment of peroneal nerve palsy. J Bone Joint Surg Am. 1996;78:863-869.
73 Gousheh J, Arasteh E, Beikpour H. Therapeutic results of sciatic nerve repair in Iran-Iraq war casualties. Plast Reconstruct Surg. 2008;121:878-886.
74 McMahon MS, Craig SM. Interfascicular reconstruction of the peroneal nerve after knee ligament injury. Ann Plast Surg. 1994;32:642-644.
75 Kim DH, Cho YJ, Ryu S, et al. Surgical management and results of 135 tibial nerve lesions at the Louisiana State University Health Sciences Center. Neurosurgery. 2003;53:1114-1124.
76 Gosk J, Rutowski R. Traumatic injuries of the tibial nerve: etiopathogenesis and surgical outcome. Ortop Traumatol Rehabil. 2005;7:406-410.
77 Logigian EL, Berger AR, Shahani BT. Injury to the tibial and peroneal nerves due to hemorrhage in the popliteal fossa: case reports. J Bone Joint Surg Am. 1989;71:768-770.
78 Prandl EC, Schintler M, Scharnagl E, Haas F. Severing of the tibial nerve with stripping of the lesser saphenous vein: a rare complication of surgery for varicosity. Chirurg. 2006;77:856-857.
79 Geissler WB, Corso SR, Caspari RB. Isolated rupture of the popliteus with posterior tibial nerve palsy. J Bone Joint Surg Br. 1992;74:811-813.
80 de Ruiter GCW, Torchia ME, Amrami KK, Spinner RJ. Neurovascular compression following isolated popliteus muscle rupture: a case report. J Surg Orthop Adv. 2005;14:129-132.
81 Ortiguera CJ, Bremner BRB, Peterson JJ. Popliteus strain causing tibial nerve palsy with a permanent partial deficit: a case report. Am J Sports Med. 2006;34:1176-1180.
82 Georgoulis AD, Makris CA, Papageorgiou CD, et al. Nerve and vessel injuries during high tibial osteotomy combined with distal fibular osteotomy: a clinically relevant anatomic study. Knee Surg Sports Traumatol Arthrosc. 1999;7:15-19.
83 Freedman DM, Barron OA. Iatrogenic posterior tibial nerve division during ankle arthroscopy. Arthroscopy. 1998;14:769-772.
84 Roganovic Z, Pavlicevic G, Petkovic S. Missile-induced complete lesions of the tibial nerve and tibial division of the sciatic nerve: results of 119 repairs. J Neurosurg. 2005;103:622-629.
85 Seddon H. Peripheral Nerve Injuries. Medical Research Council Special Report, Series No. 282. London: Her Majestys Stationary Office; 1954.