49
Neonatal resuscitation
Physiology
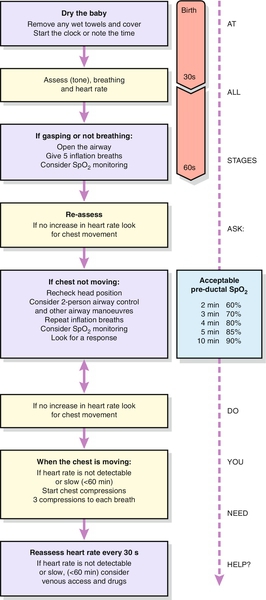
Clamping of the cord after delivery leads to acute hypoxia. This is thought to be the major stimulant for a baby to start breathing. Physical stimuli such as cold air, rubbing or physical discomfort may also provoke respiratory efforts. If the baby fails to start breathing, the baby’s oxygen concentration falls further, the baby loses consciousness and enters ‘primary apnoea’.
After 5–10 min of primary apnoea, spinal centres, which are normally suppressed by higher centres, begin to cause shuddering of the baby’s body at a rate of approximately 12/min (agonal gasps). Once this gasping stops, the baby enters ‘secondary’ (or ‘terminal’) apnoea and without intervention, the outcome is death.
The only way to tell whether a non-breathing newborn infant is in primary or secondary apnoea is by assessment of its response to resuscitation. If in primary apnoea, nearly all infants will start breathing within a few breaths; if secondary, the baby will usually gasp for some time before starting regular respiration. In reality, however, both are initially managed in the same way. Most babies born in primary apnoea will breathe spontaneously within 60–90 s given a clear airway. The basic approach to all resuscitation is therefore Airway, Breathing and Circulation (ABC).
Practical aspects of neonatal resuscitation
Dry, wrap and keep the baby warm
Dry the baby immediately and then wrap in a warm dry towel. A naked, wet baby can still become hypothermic despite a warm room, especially if there is a draught. Cold babies have an increased oxygen consumption and are more likely to become hypoglycaemic and acidotic. Babies also have a large surface area-to-weight ratio and heat can therefore be lost very quickly. Most of the heat loss is by evaporation and outcome is therefore improved by drying (Fig. 49.1).
Airway
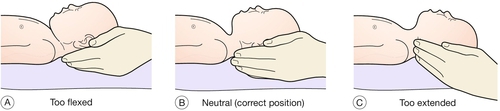
Position the baby with the head in the neutral position. Overextension may collapse the newborn baby’s pharyngeal airway, just as will flexion (Fig. 49.2).
A folded towel placed under the neck and shoulders may help to maintain the airway in a neutral position and a jaw thrust may be needed to bring the tongue forward and open the airway, especially if the baby is unresponsive.
Meconium-stained liquor is relatively common. Fortunately, meconium aspiration is a rare event and often occurs in utero before delivery. If the baby is active, no specific action (other than drying and wrapping the baby) is needed. If the baby is not active, inspect the oropharynx with a laryngoscope and aspirate any particulate meconium seen using a soft catheter under direct vision of the vocal cords.
Action points if no response:
![]() Is the baby in the neutral position?
Is the baby in the neutral position?
![]() Is there a good seal on the mask?
Is there a good seal on the mask?
![]() Do you need to perform a jaw thrust?
Do you need to perform a jaw thrust?
![]() Check for airway obstruction
Check for airway obstruction
![]() Consider Guedel airway.
Consider Guedel airway.
Breathing
If the baby is gasping or not breathing, immediately commence artificial ventilation.
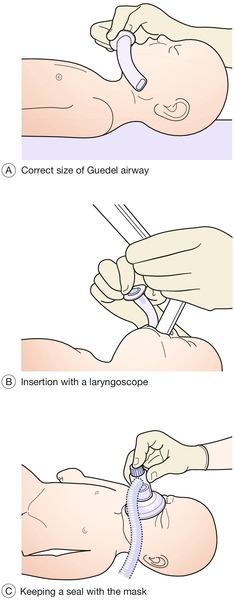
The first five breaths should be inflation breaths preferably using air in term babies. These should be 2- to 3-second sustained breaths using a bag valve mask. Use a transparent, soft, reformable mask big enough to cover the nose and mouth of the baby (Fig. 49.3).
The chest may not move during the first 1–3 breaths as fluid is displaced. Once the chest is inflated, reassess the heart rate. Assess air entry by chest movement, not by auscultation. In fluid-filled lungs, breath sounds may be heard without lung inflation. If the heart rate responds, it is safe to assume that the chest has been inflated successfully. A slow heart rate (< 100/min) will often improve with oxygenation. Once the chest is inflated, ventilation is continued at a rate of 30–40 ventilations/min. Continue to reassess that the airway is clear and that the chest is inflating.
A Guedel airway may be used to help maintain the airway (Fig. 49.4). It should be inserted under direct vision with a laryngoscope as shown. The correct size of airway should reach from the middle of the chin to the angle of the jaw.
If these techniques are unsuccessful in achieving adequate ventilation, the baby should be intubated (note that the most common reason for unsuccessful ventilation is poor positioning of the head). This is especially useful in prolonged resuscitations, pre-term babies and in those with meconium aspiration.
Circulation
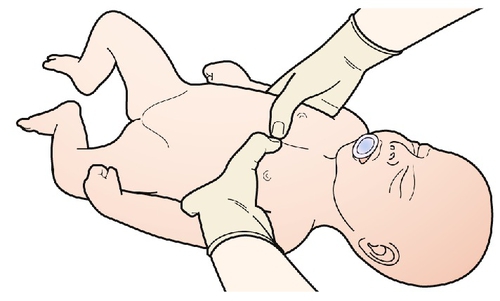
If the heart rate is not detectable or remains slow (< 60 bpm), once the lungs are inflated, chest compressions should be started immediately. The most efficient way of doing this in the neonate, is to encircle the chest with both hands, so that the fingers lie behind the baby and the thumbs are opposed on the sternum just below the inter-nipple line (Fig. 49.5). Compress the chest to one-third of its depth and perform three compressions for each breath.
The purpose of cardiac compression is to move a small amount of oxygenated blood to the coronary arteries in order to initiate cardiac recovery. There is therefore no point in cardiac compression before the lungs have been inflated. Similarly, compressions are ineffective unless interposed breaths are of good quality and inflate the chest. The emphasis must be upon effective ventilation and compressions. The most common reason for failure of the heart rate to respond, however, is failure to achieve lung inflation. Once the heart rate is above 60 bpm and rising, cardiac compression can be discontinued.
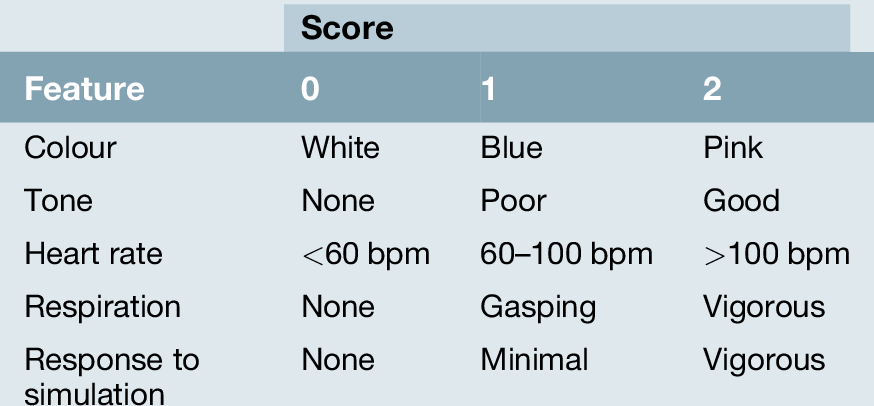
Apgar score
The Apgar score was proposed as a tool for evaluating a baby’s condition at birth and is recorded at 1 and 5 min (Table 49.1). Acute clinical assessment will categorize the baby into one of the three following colour groups:
![]() Pink – regular respirations, heart rate fast (> 100 bpm). These are healthy babies and they should be kept warm and given to their mothers.
Pink – regular respirations, heart rate fast (> 100 bpm). These are healthy babies and they should be kept warm and given to their mothers.
![]() Blue – irregular or inadequate respirations, heart rate slow (< 100 bpm). If gentle stimulation does not induce effective breathing, the airway should be opened. If the baby responds, no further resuscitation is needed. If not, progress to lung inflation.
Blue – irregular or inadequate respirations, heart rate slow (< 100 bpm). If gentle stimulation does not induce effective breathing, the airway should be opened. If the baby responds, no further resuscitation is needed. If not, progress to lung inflation.
![]() Blue/white – apnoeic, heart rate slow (< 60 bpm). Whether an apnoeic baby is in primary or secondary apnoea, the initial management is the same as above.
Blue/white – apnoeic, heart rate slow (< 60 bpm). Whether an apnoeic baby is in primary or secondary apnoea, the initial management is the same as above.
Drugs
If, after adequate lung inflation and cardiac compression, the heart rate has not responded, drug therapy should be considered. Airway and breathing must be reassessed as adequate before proceeding to drug therapy. Venous access will be required via an umbilical venous line, as drugs should be given centrally.
![]() Adrenaline (1:10 000) 0.1 mL/kg (epinephrine) can be given in the presence of profound unresponsive bradycardia or cardiac arrest
Adrenaline (1:10 000) 0.1 mL/kg (epinephrine) can be given in the presence of profound unresponsive bradycardia or cardiac arrest
![]() A bolus of 2.5 mls/kg of 10% dextrose can be used if there is hypoglycaemia
A bolus of 2.5 mls/kg of 10% dextrose can be used if there is hypoglycaemia
![]() Sodium bicarbonate 1–2 mmol/kg to reverse metabolic acidosis.
Sodium bicarbonate 1–2 mmol/kg to reverse metabolic acidosis.
Very occasionally, hypovolaemia may be present because of known or suspected blood loss (antepartum haemorrhage, placenta or vasa praevia, unclamped cord) or be secondary to loss of vascular tone following asphyxia. Volume expansion with normal saline (rather than albumin) may be appropriate. Most newborn or neonatal resuscitations do not require fluid unless there has been known blood loss or septicaemic shock.
Occasionally, a baby who has been effectively resuscitated and is pink, with a heart rate over 100 bpm, may not breathe because of the effects of maternal opiates. If respiratory depressant effects are suspected, the baby should be given naloxone intramuscularly. The effect will only last a few minutes.
Pre-term babies
The more pre-term a baby is, the less likely it is to establish adequate respirations. Pre-term babies (esp. < 32 weeks) are also likely to be deficient in surfactant. The effort required to breathe is greater and yet the muscles are less developed. One must anticipate that babies born before 32 weeks may need help to establish prompt aeration and ventilation. The paediatric or neonatal team should be called prior to delivery when possible.
Pre-term babies are more likely to become cold (higher surface area:mass ratio) and more likely to be hypoglycaemic (fewer glycogen stores). The temperature of very pre-term babies can be maintained if they are immediately placed in a plastic bag (without drying) under a radiant heater, leaving the face exposed and covering the head with a hat. The delivery room temperature should be maintained above 26°C (see also Chapter 50).
Discontinuation of resuscitation
The outcome for a baby with no cardiac output after 10 min of effective full resuscitation is likely to be very poor. The decision to discontinue resuscitation should be taken by a senior member of the team, ideally a consultant.