Neonatal and Pediatric Assessment
After reading this chapter, you will be able to:
1. Describe the type of information found in the pregnancy, labor, and delivery history and the clinical significance of common findings.
2. Explain the value of the Apgar scoring system and its interpretation.
3. Identify normal values for the vital signs in newborns and older children and the clinical implications of abnormalities.
4. Describe the clinical implications of retractions, nasal flaring, and grunting in neonates and infants.
5. Summarize the proper technique for auscultation of the infant.
6. Describe the clinical implications of abnormal breath sounds in the infant.
7. List potential causes of murmurs heard during auscultation of the infant precordium.
8. Identify the presence of a pneumothorax using a transilluminator.
9. Identify normal values for the white and red blood cell counts and partial differential for the infant at birth, 7 days of age, and 14 days of age.
10. List the possible causes of abnormalities in the white and red blood cell counts in the infant.
11. Describe the clinical implications of abnormalities in blood glucose, total protein and albumin, serum enzymes, and electrolytes.
12. Describe the limitations for sputum analysis in the infant and the child.
13. Identify normal values for arterial pH, Pao2, Paco2, HCO3−, and base excess at birth, 24 hours after birth, 2 days to 1 month, and 1 month to 2 years after birth.
14. Identify differences in blood gas parameters for capillary blood and arterial blood.
15. Describe the factors that can lead to misleading results from the transcutaneous oxygen monitor.
16. Describe the role of pulse oximetry assessment in the newborn for the detection of critical congenital heart disease.
17. Describe the lung volumes that can be measured in the newborn and the clinical value of such measurements.
18. Describe the lung mechanics that can be measured in the newborn and the clinical value of such measurements.
19. Describe the clinical findings that suggest the need for a chest radiograph in the infant.
20. Identify signs and symptoms of a compromised airway in infants and children with a tracheostomy.
21. List the indications and advantages of flexible bronchoscopy in infants and children.
bronchopulmonary dysplasia (BPD)
critical congenital heart disease (CCHD)
estimated date of confinement (EDC)
extremely low birthweight (ELBW)
interrupted aortic arch syndrome
intraventricular hemorrhage (IVH)
intrauterine growth retardation (IGR)
meconium aspiration syndrome (MAS)
neutral thermal environment (NTE)
patent ductus arteriosus (PDA)
pulmonary interstitial emphysema (PIE)
respiratory distress syndrome (RDS)
sudden infant death syndrome (SIDS)
Assessment of the Newborn
History
Maternal History
Other maternal factors that may indicate a high-risk pregnancy are listed in Table 12-1. Some of these factors will be discussed in the sections that follow.
TABLE 12-1
Common Maternal High-Risk Factors
| Classification | Factors |
| Medical history | History of hypertension and preeclampsia Pulmonary disease Cardiovascular disorders Seizure disorder Pregestational diabetes Smoking and drug use Infectious and venereal diseases |
| Obstetric history | Cervical insufficiency Absence of prenatal care Maternal anemia History of ectopic pregnancy Previous cesarean delivery History of miscarriage or ectopic pregnancy |
| Others | Low socioeconomic status Minority Malnutrition Maternal age < 18 years |
Labor and Delivery History
A healthy fetus is capable of withstanding the challenges of labor. However, when the fetus is compromised or the labor is dysfunctional, the fetus can be taxed beyond capacity. This stress can place the fetus at risk for further compromise, including but not limited to asphyxia and intrauterine death. Box 12-1 lists some of the more significant clinical manifestations signaling abnormal transition to extrauterine life.
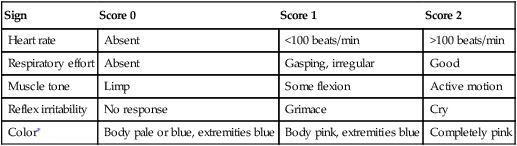
The most standard objective measurement of the newborn’s well-being during the perinatal period is the Apgar score.1,2 The Apgar score is a simple, quick, and reliable means to assess and document the newborn’s status immediately after birth. It assigns the infant points for the presence of five specific physical criteria (Table 12-2). Most infants are evaluated and assigned Apgar scores at 1 and 5 minutes. However, if the infant is having difficulty during the transition to extrauterine life, Apgar scores can be assigned more often and over a longer time span. For example, a sick infant may have 1-, 2-, 5-, 10-, 15-, and 20-minute Apgar scores. The process of assigning an Apgar score must not delay the initiation of resuscitative measures.
TABLE 12-2
| Sign | Score 0 | Score 1 | Score 2 |
| Heart rate | Absent | <100 beats/min | >100 beats/min |
| Respiratory effort | Absent | Gasping, irregular | Good |
| Muscle tone | Limp | Some flexion | Active motion |
| Reflex irritability | No response | Grimace | Cry |
| Color∗ | Body pale or blue, extremities blue | Body pink, extremities blue | Completely pink |
∗Skin pigmentation and race may affect this evaluation. In this case, assess oral mucosa and nail beds for a more accurate assessment. Beware of acrocyanosis in hands and feet, as explained later in this section.
Although the 1-minute Apgar score is a useful tool in screening infants who might require resuscitation, the 5-minute Apgar score is a better predictor of the infant’s neurologic outcome. For preterm and term infants, neonatal survival increases with increasing Apgar scores; low 5-minute scores (e.g., 0 to 3) are associated with the highest risk for neonatal morbidity and mortality.3
Fetal Assessment
• Genetic karyotyping during amniocentesis and biophysical profile to assess fetal growth and development
• Lecithin-to-sphingomyelin (L/S) ratio
• Presence of phosphatidylinositol (PI) and phosphatidylglycerol (PG) to assess lung maturity
• Fetal monitoring tracings and nonstress tests (NSTs) to assess for proper neurologic development
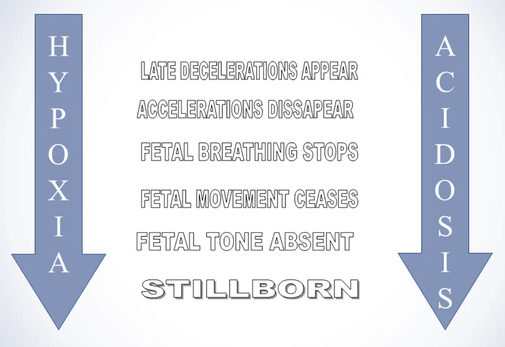
Fetal movement monitoring is easily accomplished using three widely available tools: maternal observation, fetal ultrasound, and fetal Doppler ultrasound. The simplest of these tools is having the mother keep a log of the timing, strength, and duration of the fetal movements for a period of time. Fetal ultrasound and Doppler ultrasound provide more quantifiable data but for shorter periods. Having a history of decreased fetal movement should alert the clinician of the possibility of the fetus being in trouble. This could indicate prenatal asphyxia and impending death or the possibility of severe neuromuscular disease, in which the newborn will be unable to support spontaneous independent respiration after birth. See Figure 12-1 for a representation of the events leading to neonatal death.
The biophysical profile is an ultrasound evaluation of fetal breathing, body movement, tone, reactive heart rate, and amniotic fluid volume that predicts the presence or absence of fetal asphyxia and, ultimately, the risk for fetal death. Like the Apgar score, each of these parameters has a maximal score of 2 and a minimal score of 0. The score for a normal fetus is 8 to 10. With lower biophysical profile scores, the chance of significant fetal and newborn problems increases (Table 12-3). These potential problems include IGR, significant fetal acidosis, stillbirth, and neonatal death (see Fig-12-1).
TABLE 12-3
| Biophysical Variable | Normal (Score 2) | Abnormal (Score 0) |
| Breathing | At least 30 sec of sustained FBMs observed over a 30-min period | Fewer than 30 sec of sustained FBMs observed over a 30-min period |
| Movements | At least three discrete body/limb movements in a 30-min period | Absent or less than three movements in a 30-min period |
| Tone | At least one movement of a limb from a position of flexion to one of extension, with a rapid return to flexion | Fetal limb in extension with no return to flexion with movement |
| FHR | Two or more episodes of acceleration of ≥15 beats/min and of >15 beats/min associated with fetal movement within 20 min | One or more episodes of acceleration of fetal heart rate or acceleration of <15 beats/min within 20 min |
| AFV | At least a single amniotic fluid pocket measuring 2 × 2 cm in two perpendicular planes | No amniotic fluid pocket that measures at least 2 × 2 cm in two perpendicular planes |
AFV, amniotic fluid volume; FBM, fetal breathing movements; FHR, fetal heart rate.
Adapted from Oyelese Y, Vintzileos AM: Uses and limitations of the fetal biophysical profile. Clin Perinatol 38(1):47-64, 2011.
Amniocentesis also allows for the evaluation of the L/S ratio to assess pulmonary lung maturity. The L/S ratio is the ratio of two surfactant phospholipids: lecithin and sphingomyelin. Increasing levels of lecithin indicate improving maturation of the lung’s surfactant system. Like lecithin, the presence of PI and PG is usually indicative of advancing lung maturation. In general, L/S ratios of less than 2:1 and the absence of PG are associated with high risks for RDS.4
The fetal NST is a method of evaluating the stability of the fetus’s physiology within the uterine environment. The NST monitors the acceleration of the fetal heart rate in response to fetal movement. A healthy fetus has a minimum of an increase in heart rate of at least 15 beats/minute in response to fetal movement. To be considered reactive, the fetus needs to have a minimum of two accelerations exceeding 15 beats/minute in 20 minutes for term pregnancies. A fetus is considered nonreactive when it fails to have heart rate response in two consecutive 20-minute periods. Nonreactivity may be associated with prolonged fetal sleep states, immaturity, maternal ingestion of sedatives, and fetal cardiac or neurologic anomalies.5 A fetus that is nonreactive is at greater risk for serious complications and fetal death. This will prompt the obstetrician to consider the possibility of an accelerated or operative delivery (cesarean). Knowing that a fetus has a nonreactive NST should alert the health care team that this infant may need a more extensive resuscitation and more careful evaluation after birth.
Physical Examination of the Newborn and Infant
Examination of a newborn is based on three of the four classic principles of physical examination as described in Chapter 5: inspection, palpation, and auscultation. Percussion is rarely used in examining newborns because of their small cavity and organ sizes and the possibility of injury. Therefore, percussion is not described in this chapter. Careful inspection reveals clues about the type and severity of respiratory disease. It is important to inspect the overall appearance of the infant carefully because respiratory pathology in the newborn is often manifested by extrapulmonary signs. Palpation is useful in assessing growth and gestational age and in determining the cause of respiratory distress and the severity of side effects from the lung disease and its treatment. As in the adult, auscultation is used to define characteristics of the disease process occurring in the lung. However, statements about the internal location of the pathologic process must be made with greater caution in newborns because localization by auscultation is difficult in the small chest cavity.
Growth and Gestational Age Assessment
Preterm infants are also classified based on their birthweight, as follows:
Based on their weight and gestational age, newborn infants are further classified as:
• Appropriate for gestational age (AGA): weight is appropriate for the gestational age
• Small for gestational age (SGA): smaller than expected, the weight falls below the 10th percentile for the gestational age
• Large for gestational age (LGA): heavier than expected, the birthweight is above the 90th percentile for the gestational age
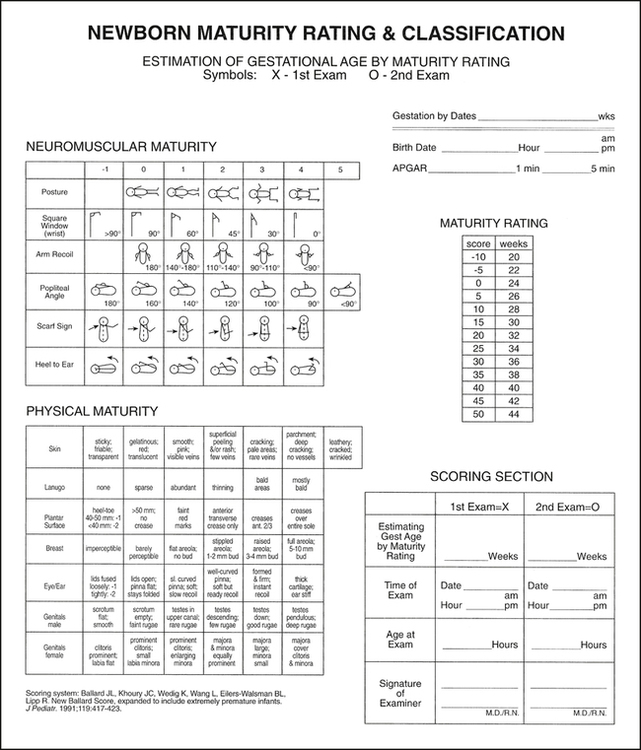
The original assessment tools were developed by Dubowitz and Dubowitz. These tools have been modified and validated over many years. Most nurseries currently use a Ballard examination (Fig. 12-2), which is a modification of the Dubowitz examination. Gestational age assessment should be performed for all newborns.
The Ballard examination is divided into two sections: neuromuscular maturity and physical maturity. The infant’s neuromuscular and physical characteristics are scored by matching the infant’s characteristics to the table’s descriptions and then marking the table. Each column of the table has a numerical value ranging from −1 to +5. The numerical values for all of the marked cells are added together. It is important that a cell is marked in each row. The sum is then compared with the maturity scale, and a gestational age is assigned. The Ballard examination is accurate to within 2 weeks of the gestational age.3
Vital Signs Assessment
Body Temperature
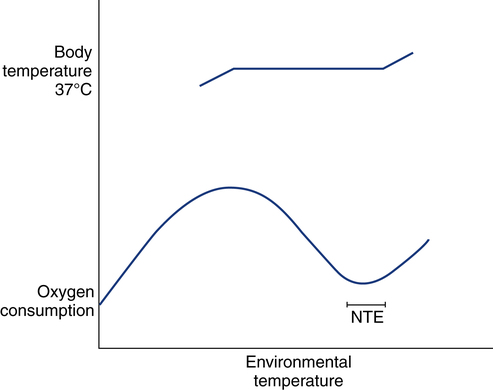
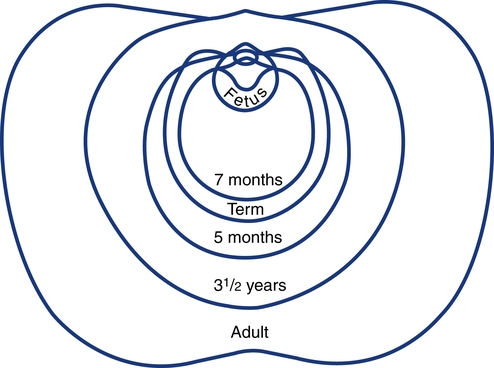
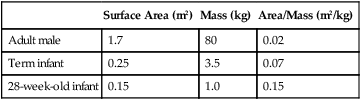
The range of normal body temperature in the newborn does not differ from that in the adult. Humans maintain body temperature by balancing heat production with heat loss. The newborn loses much more heat to the environment than the older child or adult, largely because heat loss is determined by the ratio of the surface area of the body to the total body mass (Table 12-4). The neonatal surface area-to-mass ratio is more than three times the surface area-to-mass ratio of an adult male. For premature neonates, the problem becomes even more significant owing to the lack of brown fat tissue and a very low surface area-to-mass ratio. Brown fat tissue, which is present in a full term neonate, is a major source of heat production for the newborn and helps to maintain internal body temperature. A 28-week gestational age neonate has a body surface area of approximately 0.15 m2 and a body mass of 1 kg. This results in a surface area to mass ratio of 0.15 m2/kg, which is more than six times greater than that of an adult male. Therefore, newborn term and preterm infants lose heat easily and are extremely dependent on the environment to help them maintain a neutral thermal environment (NTE). An NTE is the environmental temperature at which the infant’s metabolic demands and therefore oxygen consumption are the least (Fig. 12-3).
TABLE 12-4
Ratio of Surface Area to Body Mass
| Surface Area (m2) | Mass (kg) | Area/Mass (m2/kg) | |
| Adult male | 1.7 | 80 | 0.02 |
| Term infant | 0.25 | 3.5 | 0.07 |
| 28-week-old infant | 0.15 | 1.0 | 0.15 |
Assessment of Body Temperature
The most common methods to measure temperature are axillary and rectal temperatures. In addition to noting body temperature, the RT or other clinician should also note the temperature of the infant’s environment. Most sick infants are placed in an NTE (see Fig. 12-3). If the environmental temperature leaves the neutral thermal range, the infant usually can maintain a stable body temperature, but at the cost of a significant increase in oxygen consumption. NTEs are defined for an infant based on weight and gestational and chronologic age.
Pulse
Assessment of Pulse Rate
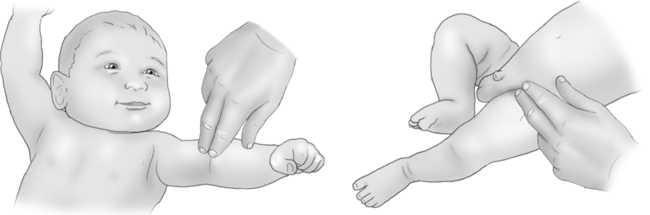
The pulse usually is evaluated at the brachial or femoral artery because of the small size of the radial arteries. To evaluate the brachial pulse, the clinician places his or her index finger pad over the brachial artery just above the elbow, with the baby in a supine position. The femoral artery pulse can be assessed at the groin, about halfway across the thigh (Fig. 12-4). On a newborn, the pulse can also be felt at the base of the umbilical cord. This is the preferred site in the L&D room during resuscitation of the neonate.
Blood Pressure
The normal values for blood pressure depend on the size of the infant or neonate, with pressures decreasing with lower weights (Table 12-5). Usually, a term neonate’s systolic blood pressure should be no higher than 70 mm Hg, with diastolic pressure no higher than 50 mm Hg. Normal pulse pressure (the difference between systolic and diastolic blood pressure) in a term infant is between 15 and 25 mm Hg.
TABLE 12-5
Normal Newborn Blood Pressures in the First Hours of Life
| Birthweight (g) | Systolic (mm Hg) | Diastolic (mm Hg) |
| 501-750 | 50-62 | 26-36 |
| 751-1000 | 48-59 | 23-36 |
| 1001-1250 | 49-61 | 26-35 |
| 1251-1500 | 46-56 | 23-33 |
| 1501-1750 | 46-58 | 23-33 |
| 1751-2000 | 48-61 | 24-35 |
| 2001-3000 | 59 | 35 |
| >3000 | 66 | 41 |
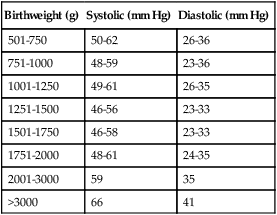
Adapted from Hegyi T, Carbone MT, Anwar M, et al: Blood pressure changes in premature infants. I. The first hours of life. J Pediatr 124:627-633, 1994.
Assessment of Blood Pressure
There are two common methods of determining blood pressure in newborns: use of a blood pressure cuff (sphygmomanometer) and direct arterial pressure monitoring. The more common method is to use a blood pressure cuff. The other common method for obtaining blood pressure in newborns is the direct measurement of pressure through an arterial cannula, also known as an arterial pressure catheter (see Chapter 15). In the newborn, it is important to measure the blood pressure in all four extremities after birth. Difference in blood pressure between upper and lower extremities can be an indication of a CCHD such as coarctation of the aorta (a narrowing of the ascending or descending aorta in a newborn).
Lung Topography
The infant’s lungs are situated in the chest much as in the adult, but the infant’s chest has a greater anteroposterior (AP) diameter than the adult’s chest. The AP diameter of the infant’s chest decreases proportionally and becomes more like the adult configuration with growth (Fig. 12-5). The imaginary lines and thoracic cage landmarks are the same in infants as in adults (see Chapter 5).
Techniques of Examination
Inspection
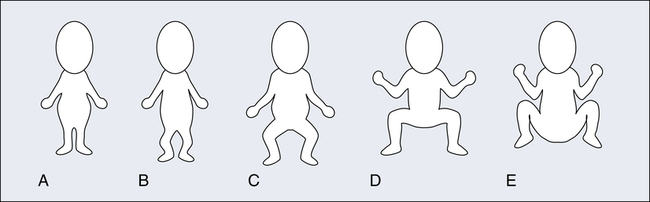
Inspection is probably the most important and often the most neglected portion of the physical examination of a newborn. The infant should be unclothed and in a supine position initially in a quiet environment. The RT or other clinician should look first at the infant’s overall appearance to identify level of illness, presence of malformations, and whether the infant’s body position is appropriate for the gestational age (Fig. 12-6). The full-term neonate at rest flexes the arms and legs into a fetal position. Premature infants at earlier gestational ages have less muscle tone, and their extremities are less flexed at rest.
Retractions
Retractions tend to be in different locations, depending on the cause of the respiratory distress. Three common points of collapse are the intercostal area (between the ribs), the subcostal area (below the lower rib margin), and the substernal area (below the bottom of the sternum). A fourth point of collapse is the supraclavicular area (above the clavicles) (Fig. 12-7).
Grunting
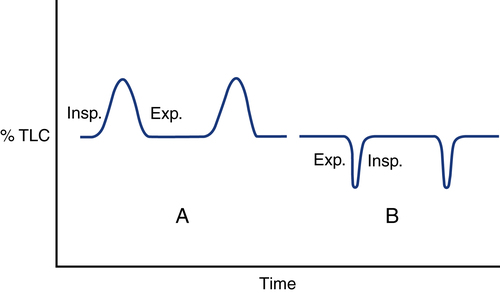
Grunting is a sound heard at the end of expiration just before rapid inspiration. Grunting is caused by closure of the glottis during expiration in an attempt to provide increased positive end-expiratory pressure and to maintain lung volume and functional residual capacity (FRC). The infant accomplishes this by occluding the airway with glottic closure and actively exhaling against the closed glottis after the end of inspiration. The grunting sound is produced when the infant suddenly opens the glottis and quickly exhales, inhales, and again closes the glottis (Fig. 12-8). Grunting is typically heard in infants with diseases that decrease lung volume (e.g., RDS).
Precordium
While observing the respiratory pattern and effort, the RT or clinician should look at the precordium (area over the heart) for any increase in motion. Increased motion is present if the chest wall is visibly lifting or moving as the heart contracts. This increase in motion, or hyperdynamic precordium, is an indication of increased volume load on the heart, usually secondary to a left-to-right shunt of blood through the ductus arteriosus or any other shunt.6 If a preterm newborn has a patent ductus arteriosus (PDA), the anatomic connection between the aorta and pulmonary artery remains open and blood from the aorta flows into the pulmonary artery, which can cause congestive heart failure and pulmonary edema. The presence of a hyperdynamic precordium is a clue that the infant’s respiratory distress may not be completely of pulmonary origin and requires further evaluation.