Multiple sclerosis I
Multiple sclerosis (MS, disseminated sclerosis) is a common disorder affecting about 1 in 1000 individuals in the UK. It is a major cause of disability in young adults. The diagnosis of MS requires two separate episodes of central nervous system demyelination separated in space and time.
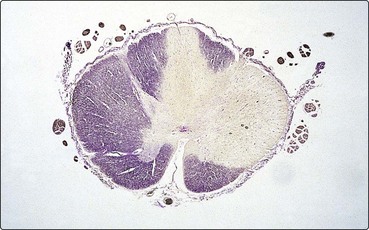
Pathology
The pathological hallmark of MS is the plaque. This is an area of demyelination, with loss of myelin and relative preservation of axons (Fig. 1). Active lesions may have an associated inflammatory response and oedema. In more chronic lesions, the oedema and inflammation have resolved and there is a demarcated area of gliotic scarring, with atrophy and axonal loss.
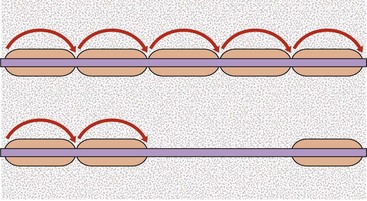
Pathophysiology
The area of demyelination disrupts the conduction of a nerve impulse (Fig. 2). This initially blocks conduction, but with recovery conduction is slowed and the refractory period is prolonged. Conduction along such segments is particularly sensitive to temperature changes and may fail if the temperature rises (which leads to Uhtoff’s phenomenon; see below).
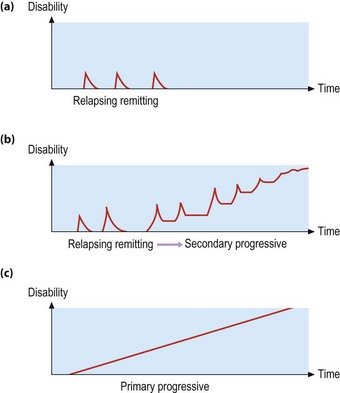
Clinical features
The peak age of onset of MS is 25–35 years. It is rare below 15 years and over 60 years. It is more frequent in women than men (about 1.5 : 1). There are essentially two patterns of disease (Fig. 3):
Symptoms and signs
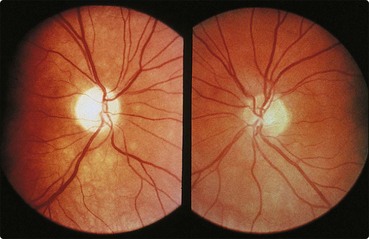
Visual
Optic neuritis is a common initial manifestation of MS. A visual disturbance evolves over a few days with distortion of the central vision and impairment of colour perception. There may be pain on eye movement. Visual loss can be mild to severe. Patients have a relative afferent pupillary defect and a central scotoma. The optic disc usually appears normal (retrobulbar optic neuritis) though may be swollen with papillitis. Vision improves over months, though may be incomplete, particularly if visual loss was severe initially. Optic atrophy may develop following an episode of optic neuritis (Fig. 4).
Spinal cord
Motor and sensory problems can be clearly localized to a single lesion in the spinal cord: myelitis. In MS this is usually incomplete, for example producing a hemicord lesion (Brown–Séquard syndrome; p. 60), though it can be complete – transverse myelitis. Some patients have a progressive spinal cord involvement.
Brain stem and cerebellum
Double vision is a common early symptom. This can be associated with a range of eye movement abnormalities (6th, 3rd or occasionally 4th nerve palsies), skew deviation and lateral gaze palsies and, most characteristic, an internuclear ophthalmoplegia (INO; p. 19).
Nystagmus is a common finding. Ataxic nystagmus is found with an INO.
Measuring disability
MS is a very variable disease. To try to assess treatment, it is imperative to have a reliable and valid measure of disability. This is straightforward for single components of disability, for example acuity and field, in assessing visual recovery after optic neuritis. A scale to cover the multiple possible disabilities found in MS will inevitably be less reliable: the most frequently used scale is the Kurtzke disability status scale (Box 1). This uses mobility as the major determinant. The scale is not linear (a one-point change means different things at different points on the scale) and has limited reliability. It is, however, the scale used in all recent major trials.