38
Multiple pregnancy
The nature of twinning and chorionicity
Antenatal problems specific to monochorionic twin pregnancies
Introduction
The natural incidence of twinning has a large geographical variation, ranging from 54/1000 in Nigeria, 12/1000 in the UK, to 4/1000 in Japan. This difference is almost entirely due to variations in the rate of non-identical twins, while the incidence of identical twins remains remarkably constant at around 3/1000. In developed countries, the actual incidence of twin pregnancies is significantly greater than the natural incidence, due to in vitro fertilization and ovulation induction techniques. Around 25% of twin pregnancies, 50–60% of triplet pregnancies, and 75% of quadruplet pregnancies are a result of assisted reproduction techniques. One in 64 pregnancies in the UK is now a twin pregnancy.
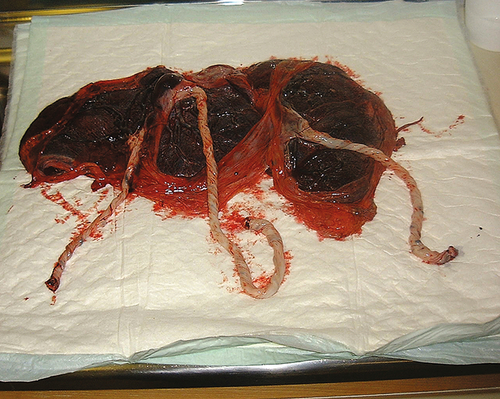
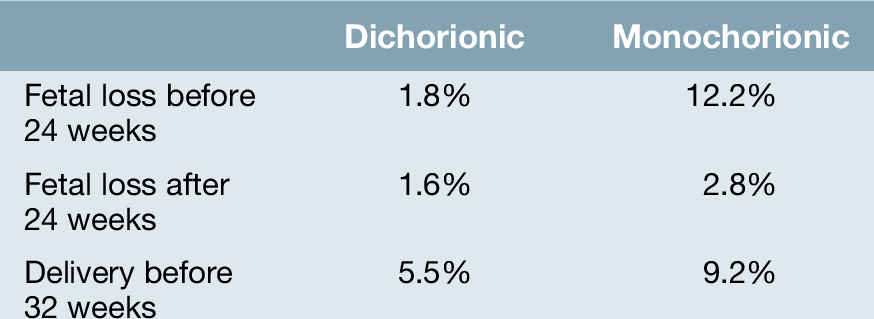
Overall, the perinatal mortality in twin pregnancies is four to five times higher than for singleton pregnancies, largely because of pre-term delivery, fetal growth restriction, twin-to-twin transfusion syndrome (TTTS), and a slightly increased incidence of congenital malformations. Perinatal mortality rates rise exponentially with fetal number in higher-order pregnancies. The outcome of any multiple pregnancy is also significantly affected by its chorionicity (whether each fetus has its own or shares a placenta) (Fig. 38.1).
The nature of twinning and chorionicity
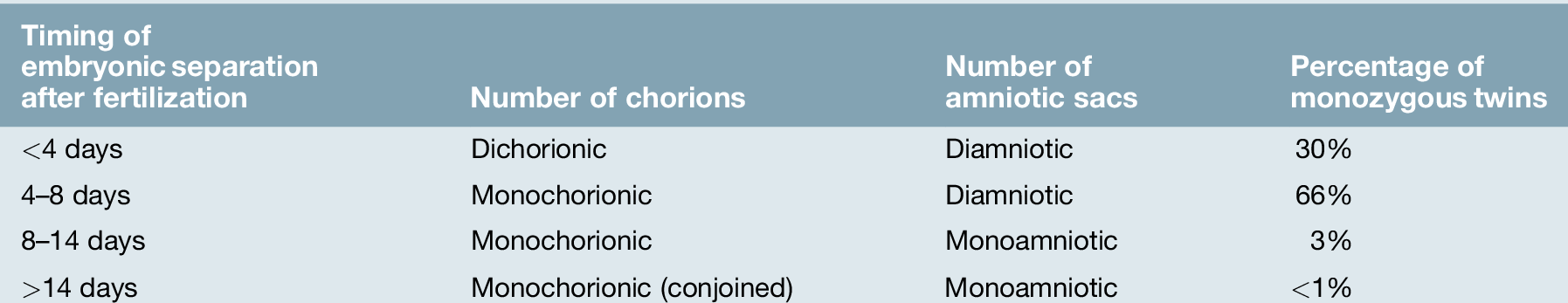
‘Zygosity’ refers to whether the twins have developed from a single ovum or from different ova – in other words, whether they are identical or non-identical. ‘Chorionicity’ refers to the number of placentae (Fig. 38.2).
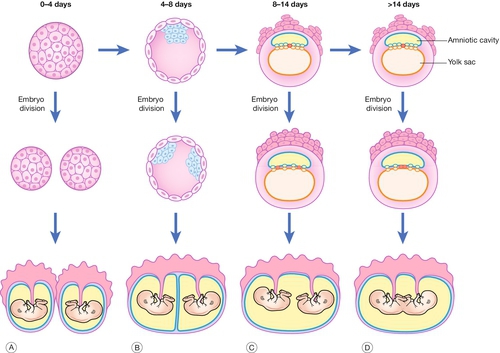
Fig. 38.2Diagram of chorionicity.
Monozygotic pregnancies may form any of the following combinations depending on the timing of embryo division: (A) dichorionic diamniotic; (B) monochorionic diamniotic; (C) monochorionic monoamniotic; (D) conjoined twins.
Dizygotic twinning (non-identical)
Dizygotic twins account for approximately 70% of twins. This process occurs when two ova are fertilized and implant separately into the decidua. Each developing embryo will form its own outer chorion (chorionic membrane and placenta) and its own inner amniotic membrane. Dizygotic twin pregnancies are described as dichorionic and diamniotic.
Monozygotic twinning (identical)
Monozygotic twins (30% of twins) are derived from the splitting of a single embryo and the exact configuration of placentation depends on the age of the embryo when the split occurs (Fig. 38.2). A split that occurs at or before the eight-cell stage (3 days post-fertilization) will occur before the outer chorion has differentiated and will therefore give rise to two separate embryos that will each proceed to form their own chorion. These twin pregnancies, like dizygotic twins, will therefore be diamniotic and dichorionic. Embryo splitting at the blastocyst stage (4–8 days post-fertilization) will occur after the chorion has started to differentiate and therefore the fetuses will share an outer chorion (placenta and outer chorionic membrane). This is the more common form of monozygotic twinning. Division of the embryo between 8 and 14 days will result in the inner amniotic cavity and membrane being shared (monochorionic monoamniotic twins). Splitting beyond 14 days following fertilization is extremely rare, giving rise to conjoined twins (Fig. 38.3); Table 38.1.
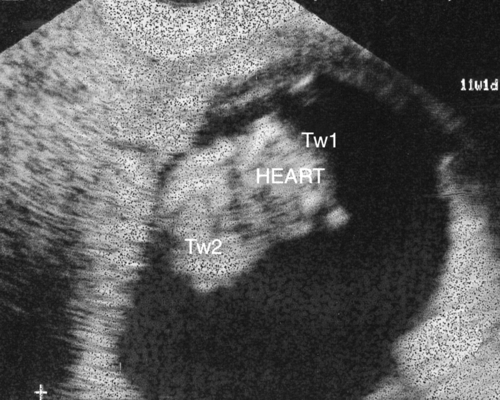
Diagnosed at 12 weeks’ gestation. This is a cross-sectional view through the thoraces of both of the twins. In view of the shared cardiac structures, management includes the option of termination of pregnancy.
In monochorionic twins, the shared placental mass inevitably contains a number of vascular anastomoses between the two fetal–placental circulations. The very presence of a shared vascular system dictates that the well-being of each twin is directly dependant on the well-being of the other. The number and nature of these vascular connections places monochorionic twins at risk of specific complications and an increased perinatal loss and morbidity rate.
Chorionicity determination is therefore essential to allow risk stratification (Table 38.2), and has key implications for prenatal diagnosis and antenatal monitoring. It is most easily determined in the first or early second trimester by ultrasound:
![]() widely separated first-trimester sacs or separate placentae are dichorionic
widely separated first-trimester sacs or separate placentae are dichorionic
![]() those with a ‘lambda’ or ‘twin-peak’ sign at the membrane insertion are dichorionic (Fig. 38.4A)
those with a ‘lambda’ or ‘twin-peak’ sign at the membrane insertion are dichorionic (Fig. 38.4A)
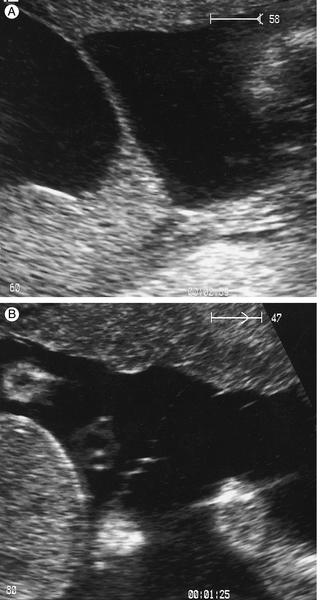
Fig. 38.4(A) Dichorionic twins – lambda sign. (B) Monochorionic twins – no lambda sign.
The two amniotic membranes form a ‘T-sign’ as they join the placenta.
![]() those with a ‘T’ sign at the membrane insertion are monochorionic (Fig. 38.4B)
those with a ‘T’ sign at the membrane insertion are monochorionic (Fig. 38.4B)
![]() different-sex fetuses are always dichorionic (and dizygous).
different-sex fetuses are always dichorionic (and dizygous).
Maternal complications
The incidence of all maternal complications is increased in multiple pregnancy.
Hyperemesis
The increased placental mass, and therefore increased maternal circulating human chorionic gonadotrophin (hCG) concentration, is associated with an increased and earlier incidence of hyperemesis.
Anaemia
There is an increase in the incidence of anaemia associated with multiple pregnancy, which is not completely explained by a haemodilutional effect of the increased plasma volume. The need for iron and folate supplementation should be assessed early in the pregnancy with a full blood count performed at 20–24 weeks’ gestation, in addition to the usual antenatal anaemia screen performed at 28 weeks in all pregnancies.
Pre-eclampsia
The incidence of pre-eclampsia in twin pregnancy is three to four times greater than that in singleton pregnancies. It tends to develop earlier and may be more severe. Women carrying a multiple pregnancy should be assessed for any additional risk factor for pre-eclampsia (first pregnancy; age ≥ 40 years; pregnancy interval of more than 10 years; BMI of ≥ 35 kg/m2 or family history of pre-eclampsia). If one or more additional risk factors exist, the women should be advised to take 75 mg of aspirin daily from 12 weeks until birth, as a measure aimed to reduce her overall risk of this complication.
Antepartum haemorrhage
Placenta praevia is more common with multiple gestations as a result of the larger placental surface. The management of this condition in multiple pregnancy is similar to that of a singleton pregnancy. Placental abruption also appears to be commoner in twin pregnancies.
Other maternal complications
The mother is also at increased risk of gestational diabetes, general discomfort, varicose veins and dependent oedema, delivery trauma, caesarean section, postpartum haemorrhage, psychological disorders, breastfeeding and parentcraft challenges.
Fetal complications
Chromosomal abnormalities
These are usually confined to one twin (i.e., non-concordant) in dizygotic twins and almost always concordant in monozygotic twins. The maternal age-related risk for carrying at least one fetus with Trisomy 21 (Down syndrome) is therefore approximately doubled in dichorionic twin pregnancies (the majority of which are dizygotic, i.e. the mother carries two individuals each with a risk), but remains unaltered in monochorionic (monozygotic) twins. Maternal serum screening for trisomy 21 performs poorly in twin pregnancy. Nuchal translucency measurement (with or without biochemistry) is a more useful screening test. If invasive diagnostic testing is indicated, amniocentesis of each amniotic sac is required in dichorionic pregnancies, and care must be taken to document which sample has come from which sac. Chorionic villous sampling is not usually appropriate for twin pregnancies as it may be difficult to be sure that both placentae have been sampled, particularly if they are lying close together. Before any screening or invasive diagnostic test is undertaken the parents should be comprehensively counselled about the psychological difficulties they may face if a risk or diagnosis of an anomaly is confined to a single fetus, and the physical and psychological risks associated with selective termination of one twin.
Structural defects
The incidence of structural fetal abnormality is no different per fetus in a dichorionic pregnancy from a singleton pregnancy, but it is two- to three-fold greater with monochorionicity. The mother therefore will have a two- to six-fold increased risk of carrying a fetus with a structural abnormality. In monochorionic twins, it is thought that it is the process of embryo division, which is inherently teratogenic. Characteristic abnormalities include cardiac defects, neural tube and other CNS defects, and gastrointestinal atresia. It is appropriate to offer all those with multiple pregnancies a detailed mid-trimester ultrasound scan. Monochorionic twin pregnancies should be offered an extended ultrasound assessment of fetal heart structure. The abnormalities are usually confined to one twin; for example, if there is a neural tube defect in one twin, the other twin is normal in 85–90% of cases. Selective termination with intracardiac KCl is possible in dichorionic pregnancies only, and is most safely carried out before 16–20 weeks. The procedure, however, carries a 5% risk of miscarriage of both twins. In monochorionic twins, specialized cord vessel occlusive techniques may be considered, but carry an increased risk of loss to the other twin due to the increased invasiveness of this procedure.
Premature birth
Approximately 60% of twin pregnancies result in spontaneous preterm birth before 37 + 0 weeks’ gestation. Triplet pregnancies typically result in spontaneous pre-term birth before 35 + 0 weeks’ gestation. Twins account for 25% of all premature births, despite accounting for only 3% of births per year. Pre-term delivery is higher in monochorionic compared to dichorionic twins (Table 38.2). Increased uterine distension, early myometrial contractility and TTTS may be causative factors in premature labour in multiple pregnancy. At present, there is no known effective treatment to prevent premature labour. Women should be advised to present early with any symptoms of suspected pre-term labour so that corticosteroids can be administered to accelerate fetal lung maturation.
Fetal growth restriction
Twins typically reflect singleton size charts until 28–30 weeks’ gestation and then growth slows. Approximately 30% of twins are small for gestational age by singleton standards and a significant difference in the growth of one twin compared to the other is seen in 12% of pregnancies. Placental dysfunction underlies fetal growth restriction in twin pregnancies, as in singleton pregnancies. Abdominal palpation is not reliable to monitor fetal growth in multiple pregnancy. Serial ultrasound should be performed to measure fetal abdominal circumferences. If diagnosed, growth restriction requires increased surveillance of fetal well-being with umbilical artery Doppler and cardiotocography (CTG) monitoring, so that delivery can be optimally timed. Monochorionic twins are at increased risk of growth restriction, and require a lower threshold for delivery owing to the adverse consequences of a single intrauterine death in these twins.
Twins with one fetal death
First-trimester intrauterine death in a twin has not been shown to have adverse consequences for the survivor. This probably also holds true for the early second trimester in dichorionic twins, but loss in the late second or third trimester commonly precipitates labour. The majority of affected pregnancies will deliver both fetuses before 34 weeks’ gestation, often within 3 weeks of the loss. Prognosis for a surviving dichorionic fetus is then influenced primarily by its gestation. When a monochorionic twin dies in utero, however, there are additional risks of death (approx. 20%) or cerebral damage (approx. 25%) in the co-twin as a result of the shared fetal-placental circulations. As these are probably related to acute hypotension in the co-twin at the time of the other’s death, early delivery of the surviving twin is unlikely to improve its outcome and may compound morbidity if performed at a premature gestation.
Antenatal problems specific to monochorionic twin pregnancies
Twin–twin transfusion syndrome (TTTS)
This complicates 10–15% of monochorionic multiple pregnancies and accounts for around 15% of perinatal mortality in twins. In this condition there is a net blood flow from one twin to the other through arterial to venous anastomoses in the shared placenta. The circulation of the recipient becomes hyperdynamic, with the risk of high-output cardiac failure and polyhydramnios. Conversely, the donor develops oliguria and oligohydramnios and often suffers growth restriction (Figs 38.5 and 38.6). The ultrasound finding of the oligohydramnios/polyhydramnios sequence is the key to establishing an antenatal diagnosis.
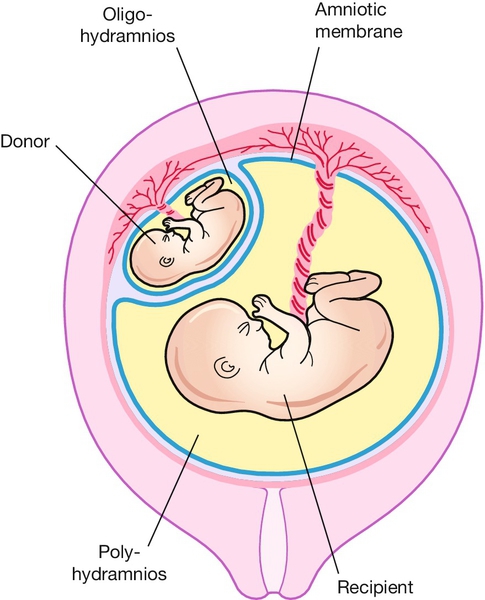
Fig. 38.5Monochorionic twins demonstrating twin-to-twin transfusion syndrome.
(Oligohydramnios–polyhydramnios sequence).
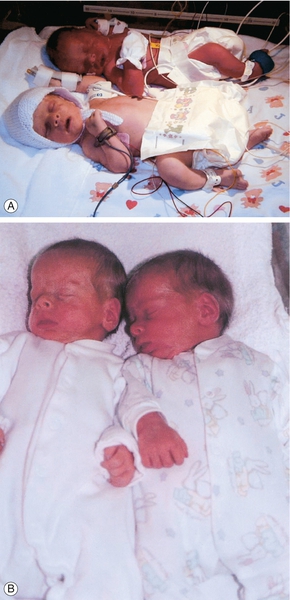
Fig. 38.6Twin anaemia polycythaemia sequence. (With permission.)
These monochorionic twins were born at 37 weeks’ gestation. Although their weights were almost identical, there was significant difference in haemoglobin concentrations at birth. This is a recently described (chronic) form of fetal to fetal transfusion. (A) At delivery. (B) Post corrective blood transfusion to the anaemic twin.
Without treatment, TTTS is associated with a > 80% pregnancy loss rate. Two interventions have proven useful: serial amniodrainage and laser ablation of the causative placental vascular anastomoses (Fig. 38.7). Evidence has emerged that laser ablation is the most effective intervention (70% survival vs 50% survival with amnioreduction) and therefore the treatment of choice in all but the mildest form of TTTS. Laser therapy is also associated with a lower rate of significant neurological morbidity in surviving twins compared with amnioreduction (5% vs 15%).
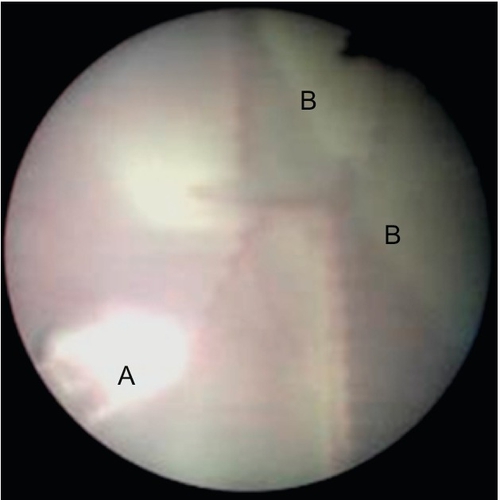
The laser fibre (A) is used to ablate vessels crossing the inter-twin membrane (B) from the donor twin as they anastomose with vessels from the recipient twin.
Monoamniotic twins
Twins who occupy a single amniotic sac are at risk of cord entanglement in utero. Frequent CTG monitoring is required once they reach viability. Delivery is electively planned for 32 weeks gestation, but indicated earlier if cord compression is suggested by abnormal fetal heart rate patterns on CTG analysis. Delivery should be performed by caesarean section, as the risk of a cord accident is particularly high during labour.
Twin reversed arterial perfusion sequence
If the heart of one monochorionic twin stops, it may continue to be partially perfused by the surviving twin, if large fetal arterial-to-arterial anastomoses exist in the shared placenta. The dead twin undergoes atrophy of its upper body and heart due to the especially poor oxygenation of these tissues, and becomes what has been described as an ‘acardiac monster’. The condition is very rare and there is a high incidence of mortality in the normal (‘pump’) twin due to intrauterine cardiac failure and prematurity. This risk increases with the relative size of the acardiac twin. Cord vessel occlusive techniques, when performed on large acardiac twins (> 50% size of the normal twin), appear to improve survival rates of the normal twin.
Management of pregnancy
Initial visit
It is important to ensure that chorionicity has been established at the first scan, as it becomes increasingly difficult to do so with advancing gestation.
The parents are often excited, and shocked, so initial counselling should be focused and include positive aspects. The parents should be counselled regarding their options for antenatal screening for fetal anomalies and should understand the potential dilemmas that may arise if one normal and one abnormal twin is diagnosed. It should be explained that more frequent antenatal visits will be required to monitor both the maternal and fetal well-being, and that ultrasound will play the key role in fetal assessments. The risk of premature delivery, the optimal timing of delivery in uncomplicated pregnancies and potential modes of delivery should be outlined.
Subsequent visits
These are ideally performed at a dedicated multiple pregnancy clinic and timed to coincide with the ultrasound assessments, the schedule of which will depend on chorionicity –
Monochorionic twins:
![]() every 2 weeks from 16 to 24 weeks to survey for TTTS
every 2 weeks from 16 to 24 weeks to survey for TTTS
![]() detailed structural survey at 18 weeks’ gestation
detailed structural survey at 18 weeks’ gestation
![]() detailed fetal cardiac scan at 20–22 weeks’ gestation
detailed fetal cardiac scan at 20–22 weeks’ gestation
![]() every 2 weeks from 24 weeks for fetal growth assessment
every 2 weeks from 24 weeks for fetal growth assessment
Dichorionic twins:
![]() detailed structural survey at 18 weeks’ gestation
detailed structural survey at 18 weeks’ gestation
![]() every 2–4 weeks from 24 weeks for fetal growth assessment.
every 2–4 weeks from 24 weeks for fetal growth assessment.
The mother should be monitored for complications such as pre-eclampsia and anaemia. Discussions about the risks and management of premature delivery and fetal growth problems are useful at 22–24 weeks’ gestation. In uncomplicated pregnancies, discussion around mode of delivery and management of twin labour is useful at 32 weeks’ gestation, when fetal presentations are unlikely to change. Tailored parentcraft advice or classes are worthwhile.
Management of twin delivery
In uncomplicated twin pregnancies delivery is planned for 37 weeks’ gestation in dichorionic twin pregnancies and for 36 weeks’ gestation (after antenatal steroids to ensure fetal lung maturation) in monochorionic pregnancies. This guidance is based on the increased risk of stillbirth in these populations after these gestations.
Presentations at term are typically:
![]() cephalic/cephalic (40%)
cephalic/cephalic (40%)
![]() cephalic/breech (40%)
cephalic/breech (40%)
![]() breech/cephalic (10%)
breech/cephalic (10%)
![]() other, e.g. transverse (10%).
other, e.g. transverse (10%).
In general, providing the presentation of the first twin is cephalic, the balance of current evidence would suggest that a trial of vaginal birth is appropriate. Significant growth discordance or any other concern of fetal well-being may be a reason to consider caesarean section. If the labour is pre-term (< 34 weeks) or if the mother has had a previous caesarean section, many clinicians would also consider delivery by caesarean section.
If labour is induced or spontaneous, the first stage is managed as for singleton pregnancies and care should be taken to ensure that both twins are being monitored with CTG, rather than one twin twice. This is best achieved by monitoring twin I with a fetal scalp electrode and twin II abdominally.
An experienced obstetrician, an anaesthetist, two paediatricians and two midwives should be present for delivery, and, if not already required, a syntocinon infusion should be ready in case uterine activity decreases after delivery of the first twin. After delivery of the first twin, it is often helpful to have someone ‘stabilize’ the lie of second twin to longitudinal by abdominal palpation while a vaginal examination is performed to assess the station of the presenting part. A portable, ultrasound machine is helpful to confirm the lie and presentation of the second twin. The membranes of twin II should not be broken until the presenting part has descended into the pelvis. If twin II lies transversely after the delivery of twin I, external cephalic or breech version is appropriate. If the lie is still transverse, the choice is between performing an internal podalic version (ideally keeping the membranes intact the obstetrician’s hand enters the uterus to identify, grasp and bring down a fetal foot), followed by subsequent breech extraction or performing a caesarean section. The CTG of twin II should be carefully monitored throughout and delivery expedited if suspected fetal distress is observed.
A maternal epidural is useful in the management of twin labour, owing to the increased risks of obstetric intervention, particularly assisted delivery of twin II.
Due to the enlarged uterine size the mother is at risk of atonic postpartum haemorrhage. This should be anticipated. Management of the third stage should be active with the administration of syntocinon or ergometrine. Rapid escalation to a postpartum haemorrhage protocol should follow if indicated by ongoing blood loss.
Triplets and higher multiples
In these cases, the perinatal mortality is high, mostly because of the high risk of premature labour, and it may be appropriate to discuss reducing the number of fetuses to twins at 12–14 weeks’ gestation. With quadruplets or higher-order pregnancies, there is likely to be a greater chance of at least one or two survivors if fetal reduction is carried out, despite the miscarriage risk associated with the procedure itself. Reduction of any monochorionic twin pairs will have the greatest positive effect on outcomes. For triplets, the situation is less clear. The emotional and ethical problems associated with these decisions are considerable.
Triplets and higher-order multiple pregnancies require intensive antenatal care. These pregnancies are best delivered by caesarean section due to the inability to effectively monitor all fetuses in labour and the higher risk of fetal malpresentation.