CHAPTER 49 Modified Brunelli Tenodesis for the Treatment of Scapholunate Instability
Rationale and Basic Science Pertinent to the Procedure
Scapholunate instability is the most common form of carpal instability. Injury to the scapholunate interosseous ligament leads to alterations in the kinematic loads passing through the radiocarpal joint and a progressive degeneration of the secondary stabilizers of the carpus.1 Eventual deterioration of these secondary stabilizers leads to fixed changes within the lunate and midcarpal joint leading to radiocarpal and midcarpal arthritis. Early within this process of scapholunate instability, pain is present over the dorsum of the wrist as overload to the remaining scapholunate ligament results in scaphoid subluxation, synovitis, and internal ligamentous strain.2,3
Despite its frequency, a standardized treatment protocol for scapholunate instability has not been established. Several surgical procedures have been recommended for the treatment of this disease process, including scaphotrapeziotrapezoidal and scaphocapitate fusion, capsulodesis alone, ligament repair in conjunction with dorsal capsulodesis, tenodesis, and bone-ligament-bone reconstruction.1,4–12
Tenodesis, in particular, attempts to re-establish the scapholunate relationship and scapholunate interosseous ligament through the use of various tendon weaves. Palmer and colleagues13 described the use of the extensor carpi radialis longus tendon, which is routed through the tuberosity of the scaphoid, brought out dorsally through the lunotriquetral ligament, and then buried into a hole in the capitate. Taleisnik14 used a strip of the flexor carpi radialis passed from palmar to dorsal through the lunate and into the scaphoid to recreate the dorsal scapholunate ligament. The graft is then introduced into a drill hole in the radius to create a deep radioscapholunate ligament. Many clinical series using similar tenodesis techniques have reported good results; however, because of the technical demands of these procedures and the complication associated with multiple bone tunnels, many of these procedures were abandoned in favor of scaphotrapeziotrapezoidal fusion or dorsal capsulodesis.13–15 Inherently, any tenodesis procedure has attendant difficulties in tensioning the carpal bones because the elastic modulus of tendon is much larger than that of ligament. A reconstructed ligament that is snug enough to restore the scapholunate relationship would often result in a significant restriction in wrist motion that may approximate that following a partial wrist fusion.
In 1995, Brunelli and Brunelli7 described a tenodesis technique using a slip of the flexor carpi radialis tendon that is tunneled through the distal portion of the scaphoid and attached to the distal radius to correct the abnormal scaphoid flexion deformity and to stabilize the scapholunate interval. Brunelli’s original assumption was that rotary subluxation of the scaphoid is best corrected by stabilization of the scaphotrapeziotrapezoid ligament, rather than by reinforcing the scapholunate interosseous ligament.7,16 Although this theory itself is still controversial, Brunelli’s results were encouraging. In addition, the procedure itself required less bone tunneling with minimal destruction of the volar carpal ligaments. The initial results with the Brunelli repair have been comparable to the results reported for dorsal capsulodesis.7,17,18
Modifications of Brunelli’s original procedure have been described by Van Den Abbeele and colleagues and Garcia-Elias and colleagues.3,18,19 This modified technique involves tunneling the flexor carpi radialis tendon through the scaphoid from the distal pole to the dorsal tuberosity, in contrast to Brunelli’s original description, in which the flexor carpi radialis is passed parallel to the scaphotrapeziotrapezoidal joint surface. The tendon is passed through the dorsal radiocarpal ligament, which also has been referred to as the dorsal radiolunotriquetral ligament. The distal end of the tendon is flipped back and secured to itself and the underlying lunate. This also is in contrast to Brunelli’s original description, in which the flexor carpi radialis graft was originally anchored to the dorsal distal radius. This modified technique (now termed the “three-ligament tenodesis” because the weave is believed to stabilize the scaphotrapeziotrapezoidal, scapholunate interosseous, and dorsal radiocarpal ligaments) has yielded encouraging medium-term results for chronic scapholunate instability.3,19
Pertinent Anatomy
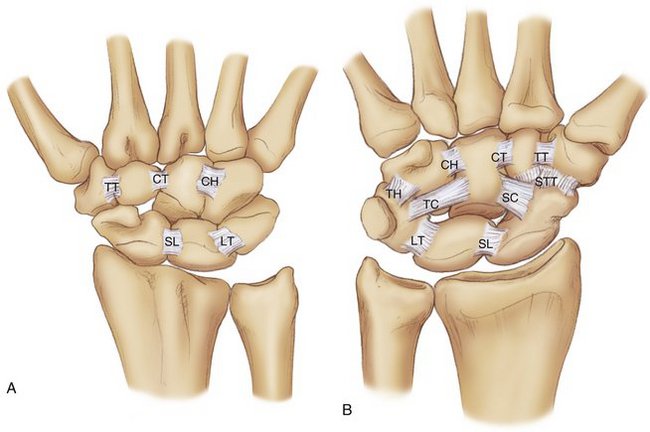
Adequate execution of the tenodesis procedure is predicated on a thorough understanding of wrist anatomy, including the secondary ligamentous constraints of scaphoid motion and the dorsal and volar wrist capsule. The ligaments of the wrist can be divided into two general categories. The first category includes the interosseous ligaments, which run between carpal bones and include the scapholunate and lunotriquetral interosseous ligaments (Fig. 49-1A). These two ligaments are the major stabilizers of the proximal carpal row and carpus.20,21 The scaphotrapeziotrapezoidal ligament, also an interosseous ligament, connects the scaphoid with the trapezium and trapezoid (Fig. 49-1B).22,23 Garcia-Elias and others24–26 characterized the distal ligament connections of the scaphoid further into two separated complexes—the mediolateral scaphotrapeziotrapezoidal ligament and the anteromedial scaphocapitate ligament; both ligaments provide distal support to the scaphoid.
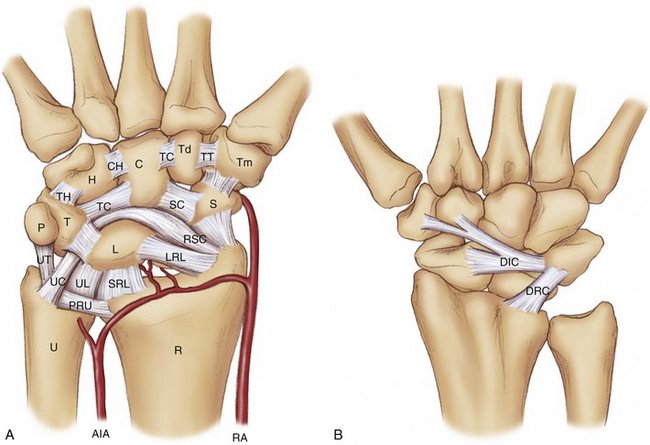
The second group of ligaments comprises the extrinsic wrist ligaments, which connect the forearm bones to the carpal bones. There are palmar and dorsal extrinsic wrist ligaments. These tend to serve as secondary stabilizers of carpal motion. The palmar extrinsic ligaments form a configuration of two “V”-shaped bands with a space between the bands. This space or gap, which has minimal ligamentous support and is an inherent point of weakness, is known as the space of Poirier (Fig. 49-2A). The dorsal carpal ligaments include the dorsal intercarpal and dorsal radiocarpal ligaments. These extrinsic ligaments are thinner and weaker than their palmar counterparts, but also provide structural support to the carpus (Fig. 49-2B).
The volar extrinsic ligaments, which act as major secondary constraints of scaphoid motion, include the radioscaphocapitate ligament, long radiolunate ligament, scaphotrapezial ligament, and scaphocapitate ligament (see Fig. 49-2A). The radioscaphocapitate ligament originates from the radial palmar rim of the radius and passes beneath the scaphoid waist to attach to the capitate. During its course, it gives off attachments to the lunate.27 These fibers interdigitate with fibers from the ulnocapitate ligament to form the so-called arcuate ligament of the wrist.28 The long radiolunate ligament lies ulnar to the radioscaphocapitate ligament and may also support the scapholunate relationship through its direct connections to the palmar component of the scapholunate interosseous ligament (see Fig. 49-2A).29,30 Short and coworkers31,32 showed that after disruption of the scapholunate interosseous ligament, division of the scaphotrapezial and radioscaphocapitate ligaments results in additional instability in scapholunate motion.
Important secondary dorsal stabilizers of the scapholunate joint include the dorsal intercarpal and dorsal radiocarpal ligaments. The dorsal intercarpal ligament originates from the dorsal ridge of the triquetrum and attaches to the dorsal distal aspect of the lunate and into the dorsal rim of the scaphoid. The ligament gives attachments to the scapholunate interosseous ligament and lunotriquetral interosseous ligament during its course.32 The dorsal radiocarpal ligament, or the dorsal radiolunotriquetral ligament, originates from the dorsal margin of the distal radius just ulnar and distal to Lister’s tubercle. The ligament extends obliquely with fibers inserting into the lunate, inserting into the lunotriquetral interosseous ligament, and finally inserting into the dorsal ridge of the triquetrum.32 The dorsal intercarpal and dorsal radiocarpal ligaments create a “V” shape over the dorsal wrist capsule and contribute to the stability of the scaphoid and lunate (see Fig. 49-2B). Viegas and others33,34 have noted that the dorsal portion of the scapholunate interosseous ligament is intertwined with portions of the dorsal capsule. Short and colleagues32 and Ruch and Smith35 have shown that injury to the dorsal intercarpal ligament can change carpal kinematics.
Finally, the flexor carpi radialis runs through a fibro-osseous canal at the scaphoid tuberosity and trapezial groove before inserting into the trapezial crest directly and then proceeding to the base of the second metacarpal.36 Its course may be easily palpated subcutaneously beneath the skin in the radial aspect of the forearm.
Indications
The primary goals of the treatment of scapholunate instability include pain relief, re-establishment of carpal alignment, and maintenance of wrist mobility. The use of the modified Brunelli procedure is reserved for patients with a history of wrist pain lasting longer than 2 to 3 months. Patients with scapholunate instability seen within 6 to 8 weeks of injury usually are treated with attempted primary open or arthroscopic repair.
Dynamic and static instability can be treated with this procedure. Dynamic and static instability refer to the radiographic appearance of the patient’s wrist at the time of presentation. Patients with static scapholunate instability present with a scapholunate diastasis greater than 3 mm and a scapholunate angle greater than 60 degrees. Patients also may present with radiographic signs of a dorsal intercalated segment instability pattern, which is manifested as an increased scapholunate angle greater than 60 degrees and an increased radiolunate and capitolunate angle. Patients with dynamic instability have normal static radiographs, but may show an increased scapholunate with stress radiographs (clenched fist view). The diagnosis of a dynamic scapholunate injury in these patients is often suspected on physical examination, but the definitive diagnosis is made at the time of arthroscopy. Patients presenting with wrist pain, normal radiographs, and only mild scapholunate instability, such as a Geissler grade 1 or 237 seen at the time of arthroscopy, may be better treated with an arthroscopic scapholunate interosseous ligament shrinkage or pinning versus an open repair combined with a dorsal capsulodesis, rather than a tenodesis procedure.9
The ideal patient for tenodesis is a patient with chronic scapholunate instability who has an easily reducible scaphoid and lunate, without evidence of chondrolysis in the radioscaphoid fossa or midcarpal joint.19 Concomitant ligamentous injuries, such as lunotriquetral injuries or triangular fibrocartilage complex injuries, can be repaired at the same time as the tenodesis procedure and are not a contraindication for this surgery.
Contraindications
At the time of surgery, Kirschner wires (K-wires) are placed into the dorsal aspect of the scaphoid and the lunate. These joysticks are used to correct the increased scaphoid flexion and dorsal angulation of the lunate. If it is difficult to restore the normal alignment of the scaphoid and lunate with the use of K-wires, long-term success with the tenodesis procedure is unlikely. Patients with an irreducible lunate or scaphoid are better treated with some form of salvage procedure. A percentage of irreducible scaphoids can be converted to reducible scaphoids by resection of the fibrous tissue that develops along the medial corner of the scaphoid tuberosity and the proximal edge of the lunate.3,7 If the scaphoid and lunate are easily reducible after resection of the fibrosis, one can proceed with the tenodesis procedure. Finally, if there is a repairable dorsal scapholunate interosseous ligament or an avulsed scapholunate interosseous ligament, one should attempt a primary repair before considering a tenodesis procedure.
Surgical Technique
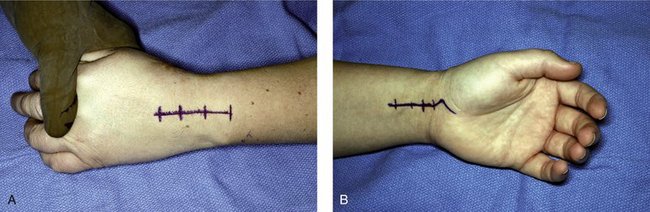
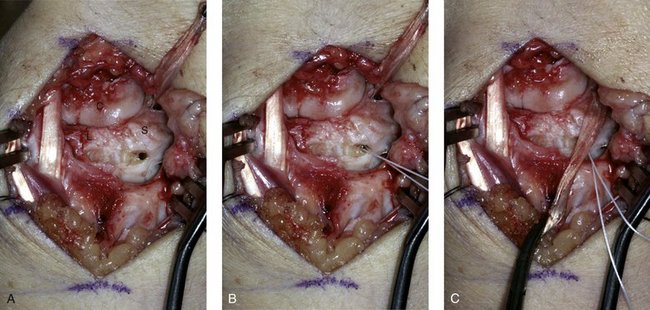
The modified Brunelli tenodesis technique is performed as described by Van Den Abbeele and colleagues18 and Talwalkar and associates19 using dorsal and volar approaches. A standard dorsal wrist incision is made, and the wrist capsule is opened using a ligament-sparing capsulotomy as described by Berger and Bishop38 (Fig. 49-3A). The radiocarpal and midcarpal joints are inspected for signs of degenerative arthritis. Any scar tissue within the joint is excised. At this point, the surgeon confirms that the scaphoid and lunate are easily reducible; if not, the procedure is abandoned, and an alternative procedure is chosen.
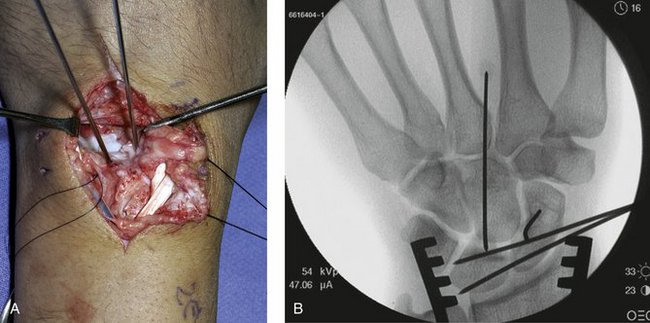
Volarly, an incision is made over the flexor carpi radialis, and dissection proceeds distally to the scaphoid tuberosity (Fig. 49-3B). A strip of the flexor carpi radialis tendon (about one third of its width) is cut proximally, preserving its distal attachment to the base of the second metacarpal. A K-wire is drilled dorsal to volar from the bare area of the scaphoid dorsally to the scaphoid tubercle palmarly. Fluoroscopy is used to verify the position of the wire (Fig. 49-4A and B). A 3.5-mm cannulated drill is passed over the K-wire to create a channel for the tendon slip. The slip of tendon is passed from volar to dorsal through the bone tunnel made in the scaphoid (Fig. 49-4C). Placing the tendon slip on tension reduces the scaphoid, although K-wire joysticks also may be used to aid in reduction. The reduced scaphoid is held with one to two K-wires (Fig. 49-5). A small trough is created in the dorsal portion of the scaphoid and lunate within which the tendon will lie (Fig. 49-6A). The flexor carpi radialis is secured onto the scaphoid and the lunate using one or two suture anchors (Fig. 49-6B and C).
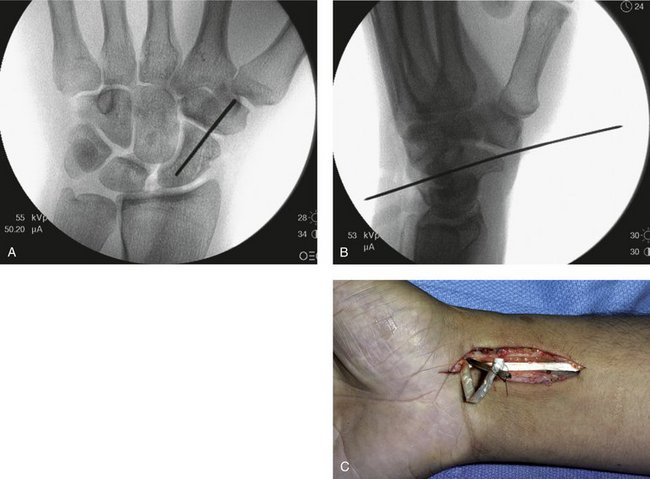
FIGURE 49-4 The initial guidewire is placed from a dorsal to palmar direction from the dorsal ridge or bare area of the scaphoid to the distal volar tuberosity. A and B, Intraoperative radiographs showing the ideal position of the guidewire in the anteroposterior (A) and lateral (B) planes. This wire is then used as the guide for a 3.5-mm cannulated drill, which creates the bone tunnel for the flexor carpi radialis. When the tunnel is created, a cannulated awl is passed from dorsal to proximal into the palmar incision. C, The flexor carpi radialis tendon slip is tied to the cannulated awl and withdrawn into the dorsal incision.
An additional wire is placed between the scaphoid and capitate to stabilize the midcarpal joint (Fig. 49-7). A long arm cast is worn for 2 weeks followed by a short arm cast until wire removal. Wires are left for 6 to 8 weeks, at which time gentle range of motion exercises are permitted. A splint is worn for an additional 6 weeks. Unrestricted activity is allowed at 5 to 6 months.
Results
Overall results of the tenodesis procedure are encouraging, but most patients can expect some reduction in wrist flexion, and 30% to 40% of patients may continue to have wrist pain with heavy exertion. Brunelli and Brunelli’s original report7 of 13 patients noted a reduction in wrist motion ranging from 30% to 60% of the contralateral wrist. Grip strength improved 50% over preoperative values, and all patients in this study were able to return to work during the follow-up period. In the study by Talwalkar and associates19 of 162 patients performed over 7 years, 62% of patients had no to mild pain at an average follow-up of 4 years. Range of motion was reduced by 26% compared with the contralateral side, and grip strength was 80% of the nonoperated side. Of patients, 79% were satisfied with the results of surgery, and 88% thought they would have had the same operation again.19 There was no significant difference in outcomes for patients presenting with dynamic or static instability. These results were comparable to earlier published results from the same institution.18
More recently, Garcia-Elias and colleagues3 have reported their 46-month results in 38 patients. In this group, 74% of patients noted pain relief at rest, and 76% were able to return to their normal vocational activities. Grip strength averaged 65% of the normal side, and postoperative wrist flexion and extension were approximately 75% of the contralateral side. None of these patients have required secondary surgery during the follow-up period.
Finally, Moran and colleagues17 reported on a retrospective comparison of 15 patients undergoing the modified Brunelli procedure and 14 patients undergoing dorsal capsulodesis for the treatment of chronic scapholunate instability with an average 3-year follow-up (Fig. 49-8). Final wrist range of motion was 63% to 64% of the normal side in both groups. The postoperative grip strength remained unchanged in both groups, measuring 91% of normal side in the capsulodesis group and 86.5% of normal side in the tenodesis group. There was one failure requiring wrist fusion in the tenodesis group. Motion decreased from 89% of the contralateral side preoperatively to 63% postoperatively. The preoperative scapholunate angle averaged 63 degrees (range 45 to 95 degrees) and was corrected to 54 degrees (range 35 to 95 degrees) on final follow-up.17 There was a statistical long-term improvement in the scapholunate angle in the tenodesis group that was not seen in the capsulodesis group, suggesting that the modified Brunelli procedure may provide a benefit over capsulodesis in controlling scaphoid flexion and preserving carpal dynamics; however, further prospective trials are required to determine the ideal long-term treatment for this difficult problem.
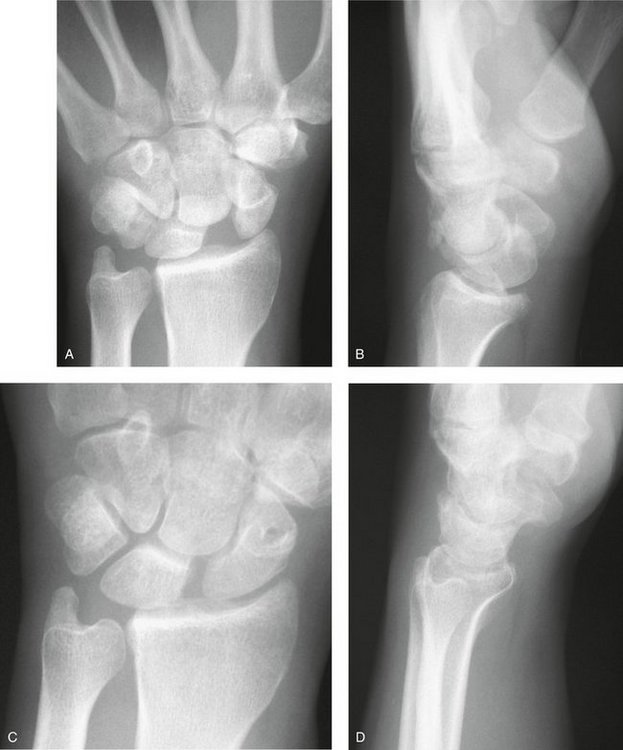
FIGURE 49-8 A and B, Preoperative anteroposterior (A) and lateral (B) radiographs of a patient with a chronic scapholunate dissociation and significant dorsal intercalated segment instability. C and D, The patient was treated with a tenodesis procedure with good restoration of the scapholunate gap (C) and scapholunate angle (D) at 2-year follow-up.
(From Moran SL, Ford KS, Wolfe CA, et al: Outcomes of dorsal capsulodesis and tenodesis for treatment of scapholunate instability. J Hand Surg. 2006; 31:1436-1438.)
1 Gelberman RH, Cooney WP, Szabo RM. Carpal instability. Instr Course Lect. 2000;82A:578-594.
2 Linscheid RL, Dobyns JH, Beabout JW, et al. Traumatic instability of the wrist: diagnosis, classification and pathomechanics. J Bone Joint Surg Am. 1972;54:1612-1632.
3 Garcia-Elias M, Lluch AL, Stanley JK. Three-ligament tenodesis for the treatment of scapholunate dissociation: indications and surgical technique. J Hand Surg [Am]. 2006;31:125-134.
4 Watson HK, Hempton RF. Limited wrist arthrodeses, I: the triscaphoid joint. J Hand Surg [Am]. 1980;5:320-327.
5 Kleinman WB, Carroll C. Scapho-trapezio-trapezoid arthrodesis for treatment of chronic static and dynamic scapho-lunate instability: a 10-year perspective on pitfalls and complications. J Hand Surg [Am]. 1990;15:408-414.
6 Davis CA, Culp RW, Hume EL, et al. Reconstruction of the scapholunate ligament in a cadaver model using a bone-ligament-bone autograft from the foot. J Hand Surg [Am]. 1998;23:884-892.
7 Brunelli GA, Brunelli GR. A new technique to correct carpal instability with scaphoid rotary subluxation: a preliminary report. J Hand Surg [Am]. 1995;20(3 Pt 2):S82-S85.
8 Blatt G. Capsulodesis in reconstructive hand surgery: dorsal capsulodesis for the unstable scaphoid and volar capsulodesis following excision of the distal ulna. Hand Clin. 1987;3:81-102.
9 Lavernia CJ, Cohen MS, Taleisnik J. Treatment of scapholunate dissociation by ligamentous repair and capsulodesis. J Hand Surg [Am]. 1992;17:354-359.
10 Wolf JM, Weiss AP. Bone-retinaculum-bone reconstruction of scapholunate ligament injuries. Orthop Clin North Am. 2001;32:241-246.
11 Wyrick JD, Youse BD, Kiefhaber TR. Scapholunate ligament repair and capsulodesis for the treatment of static scapholunate dissociation. J Hand Surg [Br]. 1998;23:776-780.
12 Wintman BI, Gelberman RH, Katz JN. Dynamic scapholunate instability: results of operative treatment with dorsal capsulodesis. J Hand Surg [Am]. 1995;20:971-979.
13 Palmer AK, Dobyns JH, Linscheid RL. Management of post-traumatic instability of the wrist secondary to ligament rupture. J Hand Surg [Am]. 1978;3:507-532.
14 Taleisnik J. Wrist: anatomy, function, injury. Instr Course Lect. 1978;27:61-68.
15 Almquist EE, Bach AW, Sack JT, et al. Four corner ligament reconstruction for treatment of chronic complete scapholunate separation. J Hand Surg. 1991;16:322-327.
16 Brunelli GA, Brunelli GR. Rotary subluxation of the scaphoid: correction using the flexor carpi radialis. In: Watson HK, Weinzweig J, editors. The Wrist. Philadelphia: Lippincott Williams & Wilkins, 2001.
17 Moran SL, Ford KS, Wolfe CA, et al. Outcomes of dorsal capsulodesis and tenodesis for treatment of scapholunate instability. J Hand Surg. 2006;31:1436-1438.
18 Van Den Abbeele KL, Loh YC, Stanley JK, et al. Early results of a modified Brunelli procedure for scapholunate instability. J Hand Surg [Br]. 1998;23:258-261.
19 Talwalkar SC, Edwards AT, Hayton MJ, et al. Results of tri-ligament tenodesis: a modified Brunelli procedure in the management of scapholunate instability. J Hand Surg [Br]. 2006;31:110-117.
20 Berger RA, Blair WF, Crowinshield RD, et al. The scapholunate ligament. J Hand Surg [Am]. 1982;7:87-91.
21 Landsmeer JM. Studies in the anatomy of the carpus and its bearing on some surgical problem. Acta Morphol Neederlando-Scand. 1960;3:304-321.
22 Drewniany JJ, Palmer AK, Flatt AE. The scaphotrapezial ligament complex: an anatomic and biomechanical study. J Hand Surg. 1985;10:492-498.
23 Moritomo H, Viegas SF, Nakamura K, et al. The scaphotrapezio-trapezoidal joint, part I: an anatomic and radiographic study. J Hand Surg. 2000;25:899-910.
24 Garcia-Elias M. Kinetic analysis of carpal stability during grip. Hand Clin. 1997;13:151-158.
25 Masquelet AC, Strube F, Nordin JY. The isolated scapho-trapezio-trapezoid ligament injury: diagnosis and surgical treatment in four cases. J Hand Surg [Br]. 1993;18:730-735.
26 Garcia-Elias M, Geissler WB. Carpal instability. In: Green DP, Hotchkiss RN, Pederson WC, et al, editors. Green’s Operative Hand Surgery. Philadelphia: Elsevier Churchill Livingstone, 2005.
27 Berger RA, Landsmeer JM. The palmar radiocarpal ligaments: a study of adult and fetal human wrist joints. J Hand Surg [Am]. 1990;15:847-854.
28 Patterson R, Moritomo H, Yamaguchi S, et al. Scaphoid anatomy and mechanics: update and review. Atlas Hand Clin. 2004;9:129-140.
29 Berger RA. The anatomy of the ligaments of the wrist and distal radioulnar joints. Clin Orthop. 2001;383:32-40.
30 Berger RA. The gross and histologic anatomy of the scapholunate interosseous ligament. J Hand Surg [Am]. 1996;21:170-178.
31 Short WH, Werner FW, Green JK, et al. Biomechanical evaluation of the ligamentous stabilizers of the scaphoid and lunate, part II. J Hand Surg. 2005;30:24-34.
32 Short WH, Werner FW, Green JK, et al. The effects of sectioning the dorsal radiocarpal ligament and insertion of a pressor sensor into the radiocarpal joint on scaphoid and lunate kinematics. J Hand Surg. 2002;27:68.
33 Viegas SF, Yamaguchi S, Boyd NL, et al. The dorsal ligaments of the wrist: anatomy, mechanical properties, and function. J Hand Surg. 1999;24:456.
34 Mizuseki T, Ikuta Y. The dorsal carpal ligaments: their anatomy and function. J Hand Surg [Br]. 1989;14:91.
35 Ruch DS, Smith BP. Arthroscopic and open management of dynamic scaphoid instability. Orthop Clin North Am. 2001;32:233.
36 Bishop AT, Gabel G, Carmichael SW. Flexor carpi radialis tendinitis, part I: operative anatomy. J Bone Joint Surg Am. 1994;76:1009-1014.
37 Geissler WB, Freeland A, Savoie FHIII, et al. Intraarticular soft-tissue lesions associated with an intraarticular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78:357-365.
38 Berger RA, Bishop AT. A fiber-splitting capsulotomy technique for dorsal exposure of the wrist. Tech Hand Upper Extrem Surg. 1997;1:2-10.