Impression on CHD is often concave to the right
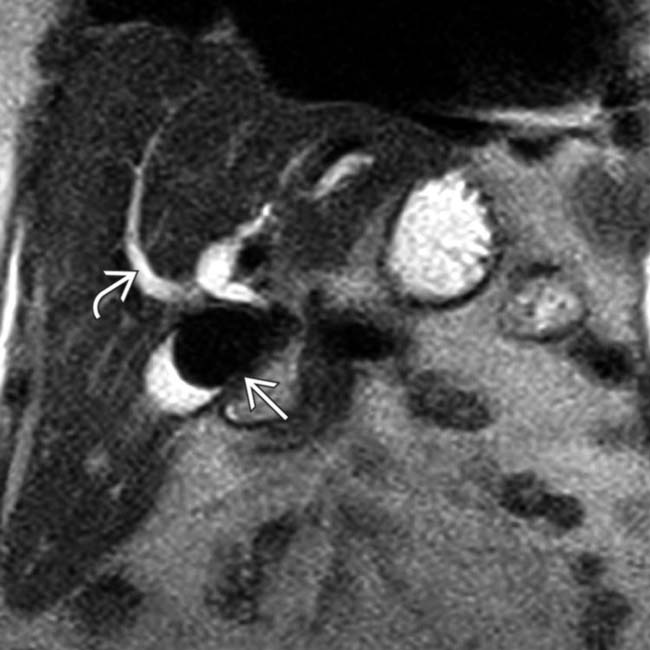
• MR: Dilated CHD and intrahepatic ducts with stricture at level of stone (signal void on all pulse sequences)
• US: Large, immobile gallstone impacted in cystic duct or infundibulum with dilated intrahepatic ducts
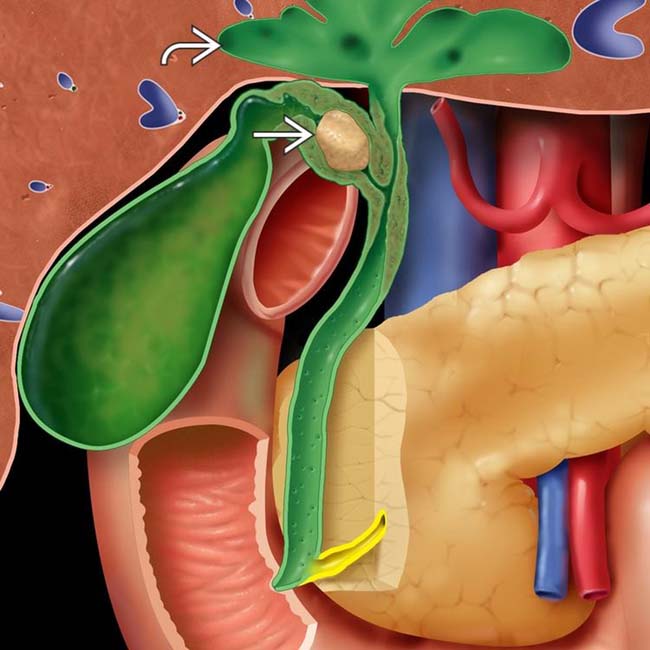
 causing extrinsic compression of the common hepatic duct (CHD) and dilation of the intrahepatic bile ducts
causing extrinsic compression of the common hepatic duct (CHD) and dilation of the intrahepatic bile ducts  .
.
 and a large gallstone
and a large gallstone  impacted within the neck of the gallbladder (GB), causing extrinsic narrowing of the common duct.
impacted within the neck of the gallbladder (GB), causing extrinsic narrowing of the common duct.
 that causes extrinsic compression of the CHD
that causes extrinsic compression of the CHD  . The intrahepatic ducts were dilated, which was better seen on axial sections (not shown).
. The intrahepatic ducts were dilated, which was better seen on axial sections (not shown).
 in the GB neck compressing the adjacent CHD
in the GB neck compressing the adjacent CHD  , resulting in mild intrahepatic biliary dilatation (not shown). Note the dilated GB with multiple stones
, resulting in mild intrahepatic biliary dilatation (not shown). Note the dilated GB with multiple stones  and mild wall thickening.
and mild wall thickening.IMAGING
General Features
CT Findings
• Imaging findings similar to MR or US, with large stone in cystic duct, focal narrowing of CHD at level of stone, and biliary dilatation upstream from level of stone
DIFFERENTIAL DIAGNOSIS
Choledocholithiasis
PATHOLOGY
General Features
• Etiology
 Impaction of stone in cystic duct, infundibulum, or Hartmann pouch compressing bile duct at same level
Impaction of stone in cystic duct, infundibulum, or Hartmann pouch compressing bile duct at same level
 Obstruction caused by either direct mass effect (extrinsic compression or erosion into bile duct) or secondary development of stricture in CHD due to inflammation from stone
Obstruction caused by either direct mass effect (extrinsic compression or erosion into bile duct) or secondary development of stricture in CHD due to inflammation from stone
 Impaction of stone in cystic duct, infundibulum, or Hartmann pouch compressing bile duct at same level
Impaction of stone in cystic duct, infundibulum, or Hartmann pouch compressing bile duct at same level
 Obstruction caused by either direct mass effect (extrinsic compression or erosion into bile duct) or secondary development of stricture in CHD due to inflammation from stone
Obstruction caused by either direct mass effect (extrinsic compression or erosion into bile duct) or secondary development of stricture in CHD due to inflammation from stone
Staging, Grading, & Classification
• Csendes classification (1989)
 Type II (∼ 25% of cases): Cholecystocholedochal fistula involving < 1/3 circumference of ductal wall
Type II (∼ 25% of cases): Cholecystocholedochal fistula involving < 1/3 circumference of ductal wall
 Type III (∼ 13% of cases): Cholecystocholedochal fistula involving 1/3-2/3 circumference of ductal wall
Type III (∼ 13% of cases): Cholecystocholedochal fistula involving 1/3-2/3 circumference of ductal wall
 Type II (∼ 25% of cases): Cholecystocholedochal fistula involving < 1/3 circumference of ductal wall
Type II (∼ 25% of cases): Cholecystocholedochal fistula involving < 1/3 circumference of ductal wall Type III (∼ 13% of cases): Cholecystocholedochal fistula involving 1/3-2/3 circumference of ductal wall
Type III (∼ 13% of cases): Cholecystocholedochal fistula involving 1/3-2/3 circumference of ductal wallCLINICAL ISSUES
Presentation
Treatment
• Stent placement during ERCP may be temporary option prior to surgery but is not definitive therapy
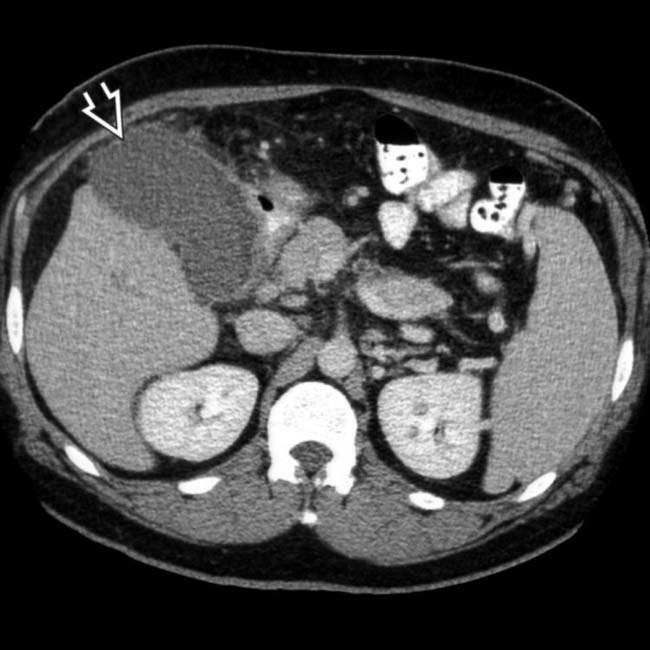
 with a thickened wall and pericholecystic stranding, suggesting acute cholecystitis.
with a thickened wall and pericholecystic stranding, suggesting acute cholecystitis.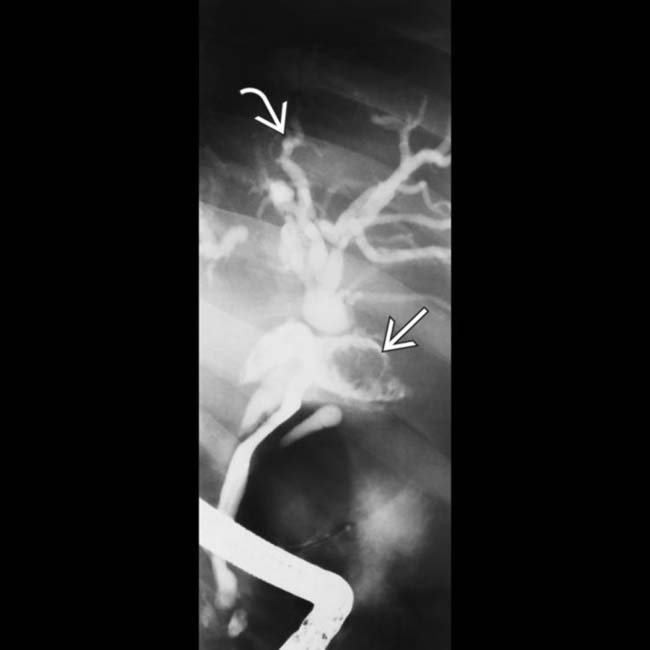
 (not visualized by CT). In addition, mass effect from the large cystic duct stone on the adjacent CHD causes intrahepatic biliary dilation
(not visualized by CT). In addition, mass effect from the large cystic duct stone on the adjacent CHD causes intrahepatic biliary dilation  , in keeping with Mirizzi syndrome.
, in keeping with Mirizzi syndrome.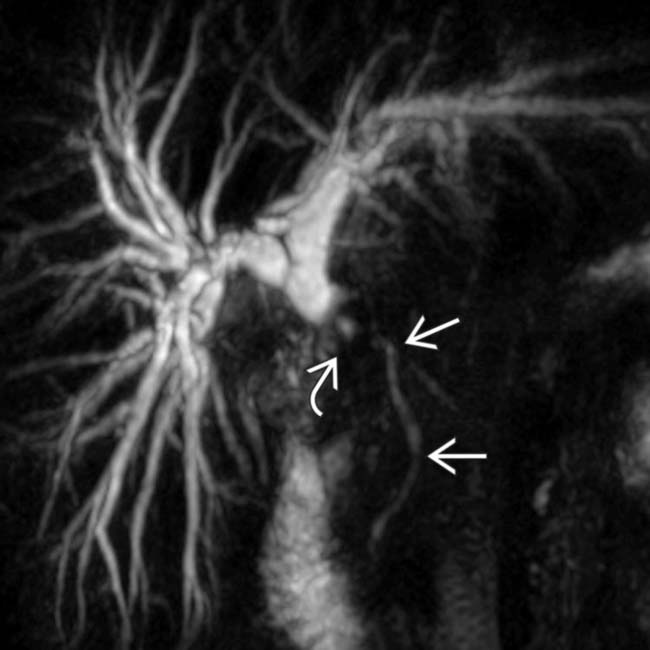
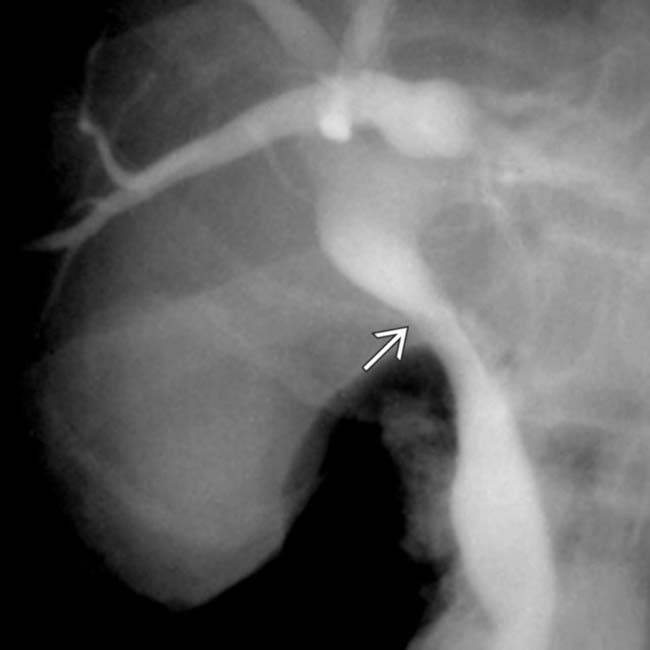
 . There is the suggestion of a discrete filling defect
. There is the suggestion of a discrete filling defect  in the CHD at the site of transition.
in the CHD at the site of transition.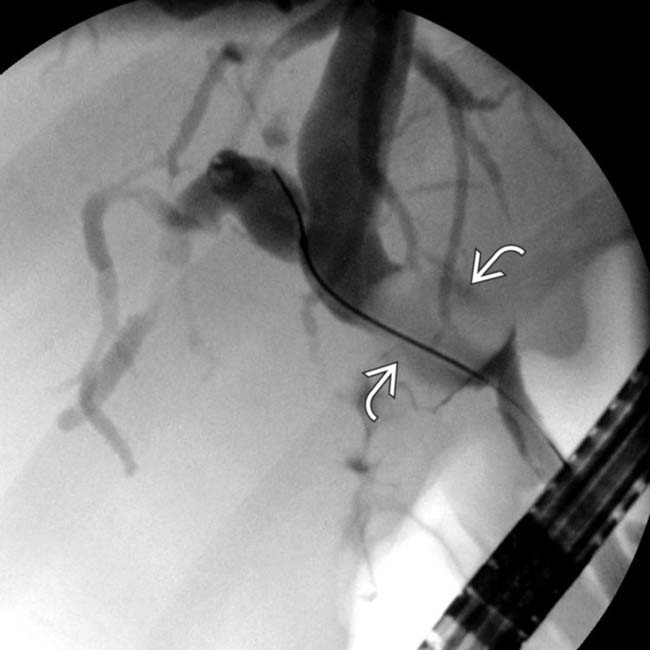
 . Note nonfilling of the GB. A cholecystocholedochal fistula and a large stone at the cystic duct-CD junction were shown at surgery, in keeping with Mirizzi syndrome.
. Note nonfilling of the GB. A cholecystocholedochal fistula and a large stone at the cystic duct-CD junction were shown at surgery, in keeping with Mirizzi syndrome.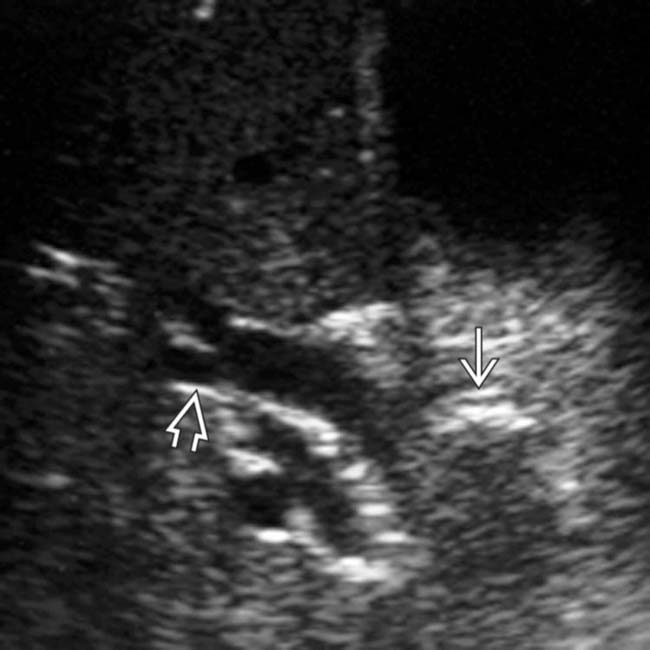
 with dilation of the adjacent CHD
with dilation of the adjacent CHD  , compatible with Mirizzi syndrome.
, compatible with Mirizzi syndrome.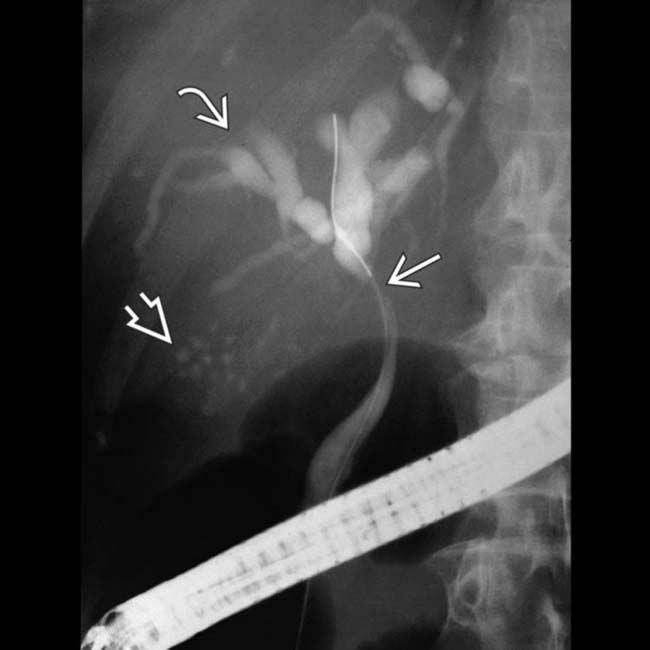
 due to a stricture of the CHD
due to a stricture of the CHD  . Note the presence of multiple gallstones within the GB
. Note the presence of multiple gallstones within the GB  . Although not visible on this image, a stone was found impacted in the cystic duct, resulting in Mirizzi syndrome.
. Although not visible on this image, a stone was found impacted in the cystic duct, resulting in Mirizzi syndrome.








































 .
.


