60 Minimally Invasive Scoliosis Treatment
Introduction
The degenerative cascade can occur in a variety of ways. When the disc degenerates and loses its height, shortening of the anterior spinal column occurs. In most cases, the collapse of the disc space occurs symmetrically, leading to loss of lumbar lordosis and accentuation of thoracic kyphosis. However, the disc may collapse asymmetrically, which in turn can lead to a lateral bending of the spine. When this occurs over multiple segments, a degenerative scoliosis may develop, causing imbalance in posture, often in both the coronal and the sagittal planes.1
As our population increases in age, the prevalence of symptomatic degenerative scoliosis will increase concomitantly. The incidence of complications is high for this type of surgery.2 The risk of these complications increases with advanced age and other medical comorbidities. The goal of minimally invasive surgery is to decrease the soft tissue trauma associated with large midline posterior and thoracoabdominal approaches, which require take-down of the diaphragm. This chapter addresses the key indications for surgical treatment, minimally invasive strategies for scoliosis treatment, contraindications to minimally invasive surgery, and potential pitfalls of MIS treatment.
Basic Science of Minimally Invasive Spine Surgery
The posterior paraspinal muscles provide dynamic stability to the spinal column.3 Numerous studies have investigated the anatomic, histologic, and radiographic properties of many of these muscles with the goal of understanding pathologic changes associated with spinal abnormalities such as chronic low back pain, disc herniation, scoliosis, and degenerative lumbar kyphosis. Paradoxically, some operations designed to treat these various spinal disorders actually disrupt these muscles and, in turn, may lead to substantial functional deficits, various pain syndromes, or both. Minimally invasive spine surgery techniques strive to minimize surgical trauma to these muscles, thereby preserving their function. Architectural studies show that the multifidus muscle stands out among all other lumbar muscles, and indeed many extremity muscles, as a most extreme example of a muscle designed to stabilize the lumbar spine against flexion. This functional design was elucidated by means of intraoperative laser diffraction and quantitative architecture measurements that demonstrated (1) an extremely large physiologic cross-sectional area, greater than that of any other lumbar spine muscle, and (2) a sarcomere length range exclusively on the ascending portion of the length–tension curve.4 The large physiologic cross-sectional area and relatively short fibers indicate that the multifidus muscle is architecturally designed to produce large forces over a narrow range of lengths. This design allows the multifidus muscle to function more to stabilize the spine and less to provide motion of the spine. As a stabilizer, it acts to maintain optimal joint forces throughout the spine as the body assumes various positions requiring prolonged flexion (such as assembly-line work) or extension (such as standing).
Clinical Practice Guidelines
Pain also occurs because of the degenerative arthritis that develops within the disc and facet joints. Bone-on-bone movement between motion segments can cause pain in a manner analogous to degenerative joint disease in the knee and hip. Furthermore, a malalignment will create focal areas of increased stress. Finally, postural imbalance can lead to fatigue-related muscle pain. Much as in flat back syndrome, early muscle fatigue and pain can develop as the patient tries to compensate for coronal and/or sagittal imbalance. In contrast to adolescent scoliosis, the concern for curve progression is relatively low. The pain associated with stenosis, radiculopathy, and early muscle fatigue drives surgical decision-making. It is rare to perform surgical correction of deformity in the absence of pain in adults with degenerative scoliosis.
Endoscopic Transforaminal Decompression for Unilateral Radiculopathy
Occasionally, a patient with degenerative scoliosis will complain mainly of leg pain, with only minor back pain. In most cases, the pain is due to neuroforaminal stenosis. Traditionally, this has been treated with hemilaminectomy and foraminotomy. However, there is risk of worsening deformity due to loss of stability when excessive bony resection is necessary and when the activity of the multifidus muscle is disrupted. An extraforaminal approach has been used with good success via a Wiltse-type paramedian approach. A minimally invasive modification of this technique utilizes tubular retractors that dilate the soft tissue and minimize retraction pressures. Although this is still performed with the patient under general anesthesia, the accessibility of the neuroforamen is sufficient. However, it is technically challenging to use the operating microscope because of the angle of the approach.
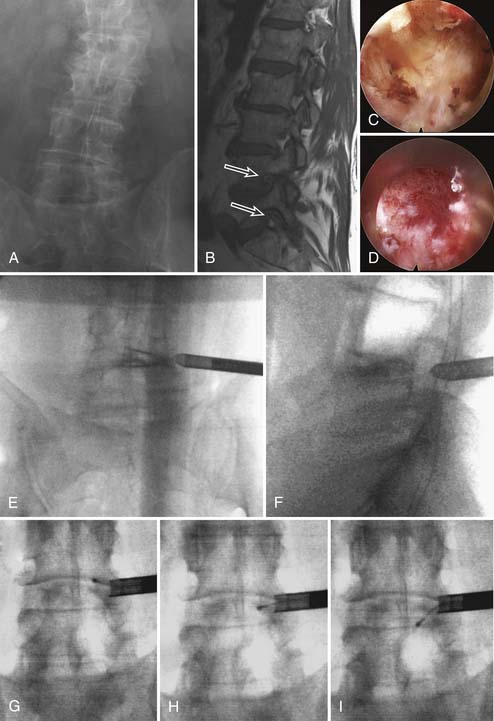
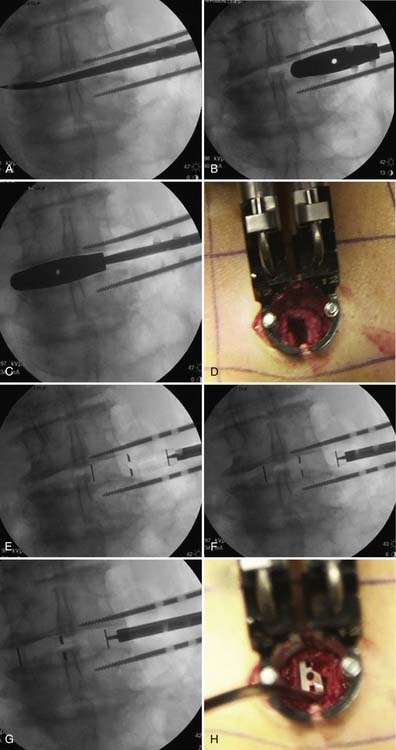
The endoscopic technique provides another avenue of treatment and it can be performed using local anesthesia.5 This is advantageous for patients with significant medical comorbidities that make general anesthesia risky. Furthermore, the endoscopic technique allows a more lateral trajectory to the spine, facilitating deeper entry into the neuroforamen (Figure 60-1).
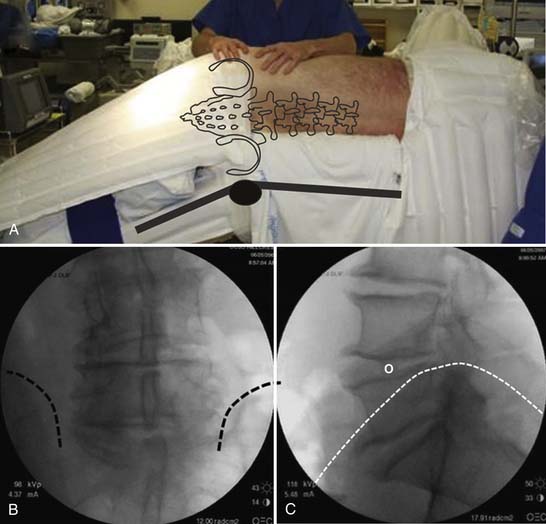
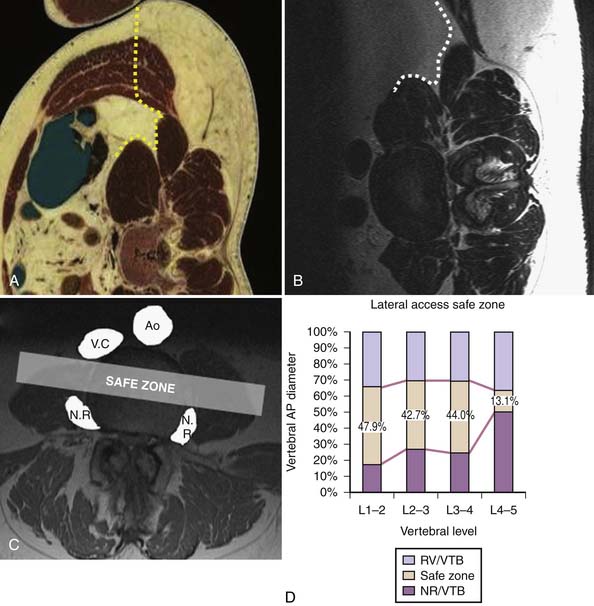
Deformity Correction via Direct Lateral Anterior Interbody Fusion
A powerful method of deformity correction is the direct lateral interbody fusion (DLIF) technique (Figures 60-2 through 60-5). This technique was best described by Ozgur and colleagues6 using the XLIF system (Nuvasive, San Diego, Calif.). The key feature of the technique is the ability to rest the interbody spacer along the strongest portion of the vertebra endplate, namely, the cortical rim or apophyseal ring. The annulus inserts at this location and the cortex of the vertebral body acts as a vertical support. Because the interbody spacer is placed from the lateral position, the implant may overhang past the edge of the disc space, ensuring that the implant fully rests on the strongest portion of the endplate. If placed from an anterior or anterolateral position, the interbody spacer would enter the canal or the neuroforamen. In addition, the DLIF technique preserves the anterior longitudinal ligament. It is presumed that by keeping the integrity of this structure, the spine maintains a pivot point from which to correct an asymmetrically collapsed disc.
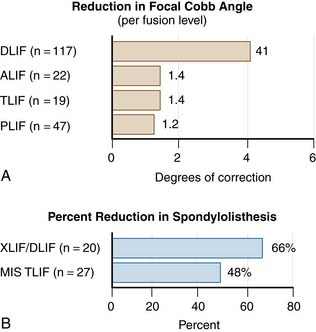
A comparison of interbody fusion techniques shows that the direct lateral interbody technique allows for greater deformity correction than anterior lumbar interbody fusion (ALIF), transforaminal lumbar interbody fusion (TLIF) or posterolateral fusion without interbody fusion. A radiographic comparison of various treatment groups showed that the focal Cobb angle for DLIF was two to four times that for the other treatment methods (Figure 60-6). The main drawback of this technique is approach-related nerve root irritation, which occurs in 3.4% of patients.7
Minimally Invasive Posterior-Only Approaches
The most common minimally invasive posterior approach is the minimally invasive transforaminal lumbar interbody fusion (MIS TLIF). Utilizing a paramedian approach, a unilateral facetectomy may be performed on the side requiring maximum correction.8 Interbody fusion allows for a high fusion rate and provides additional soft tissue release needed for deformity correction. The MIS TLIF strategy is particularly attractive if there is a large disc herniation, facet cyst, and/or severe stenosis requiring a direct decompression.
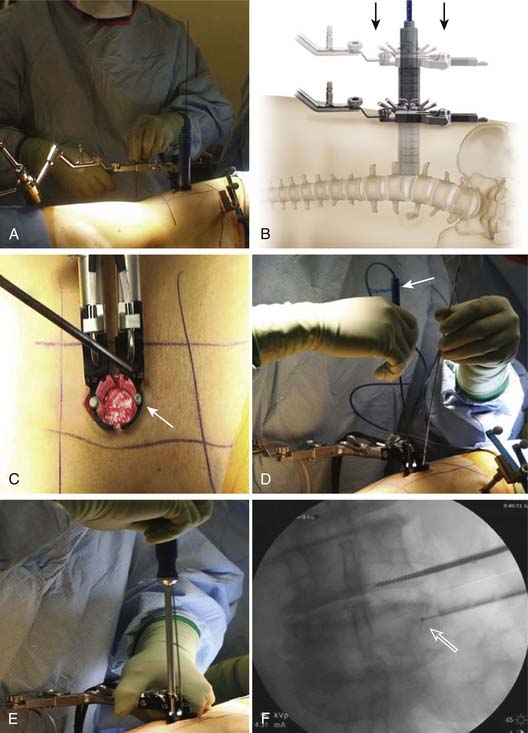
Percutaneous Pedicle Screw Fixation
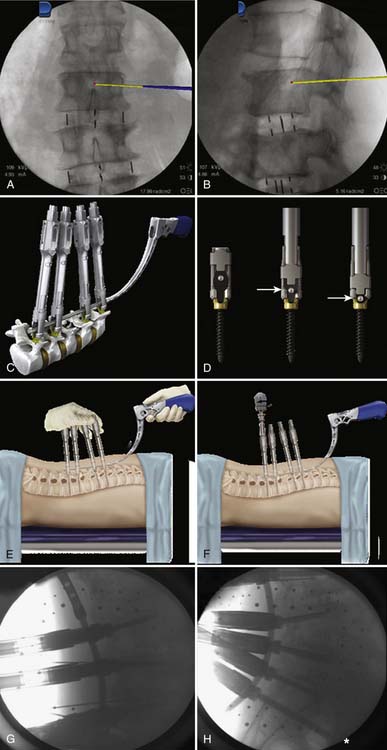
Multilevel fixation with pedicle screws and rods remains one of the most significant challenges in the minimally invasive treatment of degenerative scoliosis. In contrast to open techniques, the percutaneous rods cannot be reduced into the tulip of the pedicle screws, nor can a rotation maneuver be performed. The method of bringing the rod to the screw relies on screw extension sleeves that serve to guide the rods through each tulip and thereafter reduces the rod into the seat of the tulip so that a fixation nut can be applied (Figure 60-7). The greatest challenge occurs at the lumbosacral junction, where there is a sudden curvature due to the lordotic angle between L4 and S1 (See Figure 60-7H). Extreme care must be exercised to align the height of the tulips. With osteoporotic bone, misalignment can lead to screw pullout during the reduction maneuver. The use of bone cement injected into the pedicles immediately before screw insertion greatly improves fixation strength.9
MIS Iliac Fixation
The use of iliac screws improves fusion rates at L5-S1 when the construct is long. An important technique in posterior deformity correction is insertion of iliac screws in a minimally invasive fashion.10 By placing the insertion point of the iliac screws on the medial wall of the posterior superior iliac spine (PSIS) about 2 cm distal to the S1 screw, the tulips of the screws can be aligned so that a rod can be passed through both the S1 screw tulip and the iliac screw tulip (Figure 60-8). Meticulous attention to rod contouring is required to ensure that the construct is not under undue stress.
Case Studies
Minimally invasive scoliosis surgery relies on three main technologies: (1) DLIF/XLIF, (2) posterior MIS TLIF, and (3) percutaneous pedicle screw instrumentation. Using a combination of these techniques, deformities of the thoracolumbar spine spanning T10 to the pelvis can be treated. The most common and most straightforward problem is a degenerative scoliosis from L2 to L5 with back pain and neurogenic claudication (Figure 60-8). Using a lateral interbody approach, much of the stenosis can be addressed by correcting the Cobb angle and reestablishing the disc space height. In doing so, an indirect decompression can be achieved in some cases without the need for a posterior laminectomy.
In cases in which there is an oblique takeoff of L5 from the sacrum, L5-S1 fusion can be achieved using an MIS TLIF (see Figure 60-9). A novel and promising strategy for L5-S1 fusion is the use of a transsacral fixation device (Figure 60-10). Added construct stability can be achieved with additional pelvic fixation using the L5-S1 surgical corridor to expose the medial wall of the posterior-superior iliac spine (PSIS) as the entry point for the pelvic screw. This allows the tulip of the pelvic screw to align with the S1 screw so that a single rod can be used (see Figures 60-9 and 60-10).
1. Ploumis A., Transfledt E.E., Denis F. Degenerative lumbar scoliosis associated with spinal stenosis. Spine J.. 2007;7:428-436.
2. Cho K.J., Suk S.I., Park S.R., Kim J.H., Kim S.S., Choi W.K., Lee K.Y., Lee S.R. Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine (Phila Pa 1976). 2007;32:2232-2237.
3. Bogduk N., Macintosh J.E., Pearcy M.J. A universal model of the lumbar back muscles in the upright position. Spine (Phila Pa 1976). 1992;17:897-913.
4. Ward S.R., Kim C.W., Eng C.M., Gottschalk L.J., Tomiya A., Garfin S.R., Lieber R.L. Architectural analysis and intraoperative measurements demonstrate the unique design of the multifidus muscle for lumbar spine stability. J. Bone Joint Surg. Am.. 2009;91:176-185.
5. Yeung A.T., Yeung C.A. In-vivo endoscopic visualization of patho-anatomy in painful degenerative conditions of the lumbar spine. Surg. Technol. Int.. 2006;15:243-256.
6. Ozgur B.M., Aryan H.E., Pimenta L., Taylor W.R. Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J.. 2006;6:435-443.
7. Knight R.Q., Schwaegler P., Hanscom D., Roh J. Direct lateral lumbar interbody fusion for degenerative conditions: early complication profile. J. Spinal Disord. Tech.. 2009;22:34-37.
8. Schwender J.D., Holly L.T., Rouben D.P., Foley K.T. Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J. Spinal Disord. Tech.. 2005;18(Suppl.):S1-S6.
9. Burval D.J., McLain R.F., Milks R., Inceoglu S. Primary pedicle screw augmentation in osteoporotic lumbar vertebrae: biomechanical analysis of pedicle fixation strength. Spine (Phila Pa 1976). 2007;32:1077-1083.
10. Wang M.Y., Ludwig S.C., Anderson D.G., Mummaneni P.V. Percutaneous iliac screw placement: description of a new minimally invasive technique. Neurosurg. Focus. 2008;25:E17.