CHAPTER 19 Menopausal Health
PERIMENOPAUSE AND MENOPAUSE: AN OVERVIEW
In other cultures women do not report severe symptoms of menopause and menopause is not managed medically. Relying solely on a medical perspective (or disease model) of menopause does not account for the impact of culture and other social influences and may ignore the variety of patient perspectives on the menopausal transition.1
It is estimated that by the year 2015, 50% of all women in the United States will be menopausal. Women’s opinions and experience of menopause are changing. Until recent decades, menopause was a hushed topic for the 40 million American women going through “the change.” Times have changed and women today are openly looking for strategies to maintain their health and minimize discomforts. Women are also concerned about preventing the problems that commonly arise during and after menopause; for example, cardiovascular disease and osteoporosis, which may occur partly as a result of the decline in estrogen that is the hormonal hallmark of menopause. Although perimenopause—the commonly symptomatic phase leading to the permanant cessation of the menses—may be associated with varying degrees of discomfort from mild to severe, it is important to remember that this can be the beginning of a welcomed new phase of life for women. Social factors are sometimes more predictive than biologic factors of whether women will develop symptoms. A number of studies have found that women who report increased freedom, social status, and mobility after menopause are less likely to report negative symptoms. 2 3 4 5 6 In the United States, fear of aging and higher socioeconomic status are more frequently associated with negative menopausal symptoms than are body mass index or history of bilateral oophorectomy. A definition of menopause must take into account the impact of “social/cultural factors in order to encompass the range of experiences that women experience at the menopause transition. This biocultural definition permits exploration of the worldwide differences in menopause within the framework of the human life cycle and appropriately accounts for the influence of medico-cultural definitions of the menopausal transition.”1
WHAT IS MENOPAUSE?
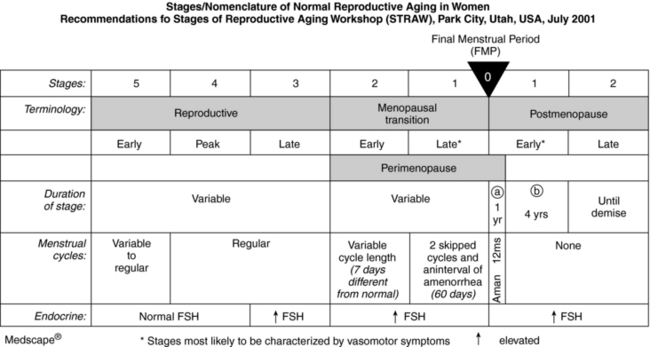
The term menopause is typically used to refer to what are actually three distinct phases: perimenopause, menopause, and postmenopause (Fig. 19-1). Perimenopause refers to the period of 2 to 8 years before the cessation of menstruation, during which regular cycles of ovulation and menses become irregular prior to terminating, a natural result of declining hormone levels, until one year after the cessation of menstruation. An elevated follicle stimulating hormone (FSH) level of 60 to 100 mIU/L on two tests done at least 1 month apart is considered indicative of menopause, although not definitive. Other hormonal indicators of the perimenopause are a luteinizing hormone (LH) level greater than 50 mIU/L and an estradiol level <50 pg/mL. The complete termination of menstrual bleeding for 12 months in the absence of another cause of amenorrhea heralds menopause and indicates that reproductive capabilities have ceased. Postmenopause is the time after complete cessation of menses. Despite ethnic, racial, and cultural variations, the median age around the world of 51 years for menopause indicates there are some common biological elements, although individuals range from ages 40 to 58 years old. However, there is a great deal of cultural disparity related to symptoms that arise during this period. For example, according to the World Health Organization (WHO), menopausal vasomotor symptoms are not as problematic for women worldwide as they are for women in the United States and other Westernized nations. Along with diet and exercise patterns, cultural attitude differences toward menopause may play some role in these epidemiologic differences.7
HERBAL STRATEGIES: AN OVERVIEW
Botanical treatments must also be placed in the context of a holistic approach that recognizes and addresses social, emotional, psychological, and other factors that can impact women, and must be proactive in helping women to prevent the development of symptoms during this time in their lives, especially heart disease and osteoporosis.
Depression and Anxiety
Hormonal changes, worries about aging, personal concerns, loss of sleep, inadequate nutrition, memory problems, and other physical complaints can fuel feelings of frustration and depression, and new concerns about health can lead to anxiety. Botanical therapies commonly used include adaptogens [see Chapter 6 Stress, Adaptation, the Hypothalamic-Pituitary-Adrenal-Axis (HPA) and Women’s Health], ashwagandha (Withania somnifera), eleuthero (Eleutherococcus senticosus), ginkgo (Ginkgo biloba), ginseng (Panax ginseng), dong quai (Angelica sinensis), motherwort (Leonurus cardiaca), St. John’s wort (Hypericum perforatum), and blue vervain (Verbena officinalis).
REFRAMING MENOPAUSE: THE WISE WOMAN PERSPECTIVE
The joy of menopause is the world’s best-kept secret. Like venturing through the gateway to enter an ancient temple, in order to claim that joy a woman must be willing to pass beyond the monsters who guard its gate… as thousands of women from all cultures throughout history have whispered to each other, it is the most exciting passage a woman ever makes.22
[Menopause] is not a natural condition; it is an endocrine disorder and should be treated medically with the same seriousness we treat other endocrine disorders, such as diabetes or thyroid disease.8
The medical definition of menopause is the end of menstruation. However, this definition fails to recognize women’s experience: that menopause, like puberty, is not a moment, not an end, but a metamorphosis that may take 5 to 10 years.1 Many practitioners—from both the scientific and alternative communities—define menopause as a state of loss, or an abnormal state. Menopause is described in disease terms as an endocrine disorder, estrogen deficiency, or simply hormonal imbalance. “This insistence on viewing menopause as a disease…defines older women as aberrant.”9 In contrast, the Wise Woman Tradition (woman-centered herbal medicine based on principles of nourishing the whole woman) defines menopause as a natural event occurring over several years, and during which the hormonal and nervous systems undergo cumulative and profound changes. In this woman-centered view, the menopausal years are an opportunity for conscious change and increased personal power, not a time of failure.
…the conventional view of menopause as a scary transition heralding ‘the beginning of the end’ couldn’t be farther from the truth.10
THE MEDICALIZATION OF MENOPAUSE
During the 1960s, with the popularization of hormone replacement, menopause became a treatable medical problem—and big business. Hormones became “the cure,” enabling women to remain “forever female.” The norm of care for middle- and upper-class white menopausal women in the United States from the mid-1960s to the present has been some form of hormonal supplementation: a combination of estrogen and progesterone for women who still have their uterus, estrogen for those without. It is now recognized that HRT increases the risk of endometrial and breast cancer. 11 12 13 15 16
Given the volumes of press devoted to HRT, one might assume that most US women use hormonal therapies at menopause; however, this is not the truth. One survey found that 52% of women wanted to avoid the use of hormones and 58% preferred alternative therapies for menopausal symptoms.17 Even before the recent cancellation of one large double-blind study of HRT, only half of all women over 50 had ever filled a prescription for estrogen or hormone replacement, and only one-third of those ever refilled the prescription. It is estimated that as many as 85% of the 37 million postmenopausal women [in the United States] do not want to use HRT.18 With growing concerns over the safety of HRT, many women—and even some physicians—are turning to alternatives. An understanding of the appropriate use of herbal medicines to nourish women during this transitional time and address common complaints associated with menopause, can ease this transition and promote health for women entering their “wisdom years.”
REFRAMING MENOPAUSE: WOMEN’S MYSTERY STORIES
Menopause is not simply an artifact of technology that has allowed us to expand our life expectancy and outlive our usefulness. Kristen Hawkes of the University of Utah studies hunter-gatherer cultures. Her “grandmother hypothesis,” based on observing the vigor and effectiveness of postmenopausal women in these cultures, demonstrates that postmenopausal women were critical to the health of their grandchildren, their community members, and the culture as a whole, and suggests that the presence of menopausal women in a society provides a survival advantage.19 The most industrious members of the Hazda culture are women in their fifties, sixties, and seventies says Dr. Hawkes. “The older woman knows the land, and its water, the seasons, the movements of the game, and the time to harvest each plant, she is not a sentiment, she is a requirement.”19 “Among many non-Western groups, the older woman enjoys increased status in the family and greater freedom in society at large. Menopause and the cessation of childbearing become positive events in a woman’s life. …“20 Reframing menopause from a “problem” to a “gift” is a direct help to most women. Women in cultures in which menopause is regarded as a gift have fewer problems with the physical and emotional changes that accompany it.21 A vigorous life keeps women vital. Vigorous exercise and a whole foods diet can help us live longer; reframing menopause can help us enjoy each passing year: gray hair, wrinkles, and all.
We have come to believe, patient and practitioner alike, that normal aging is a failure of our glands and that hormones—not just estrogen, but progesterone, testosterone, DHEA, and melatonin—are fountains of youth that will provide for us when our bodies fail. Reframing our view leads not only to a different attitude about normal menopausal symptoms, but to radically different treatments, in which herbs are not used as natural hormones, but as sources of the rich variety of helpful phytochemicals available from nature. Reframing menopause gives women a greater sense of self-worth. We reframe “loss of fertility” into “acquisition of postmenopausal zest.” This gives women something to look forward, a reward for passing through the gates of menopause. One manifestation of this reframing is the “Crone’s Crowning Ceremony.” This honoring ceremony, which celebrates a woman’s passage through the menopausal years, has become increasingly popular in the United States, especially among “the culturally creative” and women engaged in natural lifestyles. 2 23
A WHOLE FOODS DIET FOR MENOPAUSE AND BEYOND
Adequate, high-quality fat intake is essential; human steroid hormones are synthesized from cholesterol. Interestingly, studies have shown an inverse correlation between milk consumption and breast cancer. After tracking 4,697 Finnish women ages 15 to 90 for 25 years, researchers discovered that those “women who habitually drank the most milk had only half the breast cancer risk of those who drank the least.”25 A recent study done in the United States came to the same conclusion: Women who drank milk as children and continued to drink at least three glasses a day as adults had half the rate of breast cancer as those who drank little or no milk.26 Is it possible that cholesterol-rich foods, eaten as part of a healthy whole foods diet are health promoting, and that hydrogenated and partially hydrogenated vegetable fats are the real culprits in heart disease?27 A study of 61,000 Swedish women between the ages of 40 and 76 found that consumption of the monounsaturated fats, even from meat, milk, cheese, and butter, lowered the risk of breast cancer. For each 10 grams of monounsaturated fat [from dairy products and meat], the risk of breast cancer fell by 55%. For each 5 grams of polyunsaturated fat [from vegetable oil], the risk rose by 70%.28 Studies on the relationship between dairy and cancer, however, are often conflicting, with other studies demonstrating a direct correlation between dairy consumption and ovarian cancer.
The healthiest women in the world may be the women of Greece. They have some of the lowest rates of heart disease and breast cancer in the world.29 Their diets contain lavish amounts of olive oil, goat cheese, nuts, fresh vegetables, and meat. There is an inverse correlation between the amount of olive oil a Greek woman eats and her risk of breast cancer.30
HERBAL MEDICINES FOR THE MENOPAUSAL YEARS
Goals for helping women experience a healthy menopausal transition may include:
Nourishing Herbal Infusions
Nourishing herbal infusions provide nutritional, phytochemical support for menopausal and postmenopausal women with low cost and little effort. There is generally a high acceptance and follow-through rate among women of many ethnicities, cultures, education levels, and economic abilities.3 When amply extracted into boiling water, herbs such stinging nettle, oat straw, and red clover release generous amounts of vitamins, minerals, proteins, phytoestrogens, and other important constituents. 31 32 33 If the menopausal and postmenopausal diet is not mineral-rich, the entire woman suffers, not just her bones, but her heart, blood vessels, and immune and nervous systems. Minerals may be difficult to get, even in an adequate diet.32 Mineral values in commercial foodstuffs have decreased dramatically since the early part of the twentieth century.32 Regular use of nourishing herbal infusions can help to close this gap. 32 34 35 36
Cooked greens are also a rich source of minerals, as are edible seaweeds. Herbal vinegars are another great source of minerals and a way to encourage women to consume herbs daily, along with a healthful salad. Minerals are poorly absorbed from encapsulated herbs, and the amount taken is very small. Mineral-rich herbs are more like foods than medicines or drugs, and need to be consumed in dietary quantities—1 to 4 cups of infusion, not tea, or 1 to 3 tablespoons of infused vinegar daily. One cup of nourishing herbal infusion, prepared by steeping 35 g of dried herb in a liter of boiling water overnight, provides 100 to 400 mg of calcium. A tablespoon of medicinal herbal vinegar, prepared by macerating fresh herbs in vinegar for six weeks, may provide up to 50 to 100 mg of calcium.37
Supporting the Adrenals
Adrenal stress is often overlooked as a factor possibly contributing to a number of menopausal complaints including increased stress and irritability, panic attacks, emotional lability, fatigue, night waking, and possibly even night sweats. 38 39 Stinging nettle (Urtica dioica) is an excellent herbal ally. Fresh nettle leaves are eaten in soups, or as a cooked green or fresh or dried herb; 2 to 4 cups is a daily nourishing infusion. There is no scientific evidence exploring the effects of nettle on the adrenals; however, many herbalists corroborate the observation that nettle improves many symptoms associated with chronic stress and has rapid, reliable effects. Other adaptogenic herbs are also important for providing adrenal support. See Chapter 8 for a comprehensive discussion of adaptogens, as well as elsewhere throughout this book.
Supporting the Liver, Nourishing the Blood: A Vital Component of Menopausal Health
Traditional Chinese medicine (TCM) sees menopausal symptoms such as night sweats, hot flashes, memory loss, sleep disturbances, emotional swings, and even sometimes heart disease, as a result of liver qi stagnation, excess liver fire, and blood and yin deficiency.40 Many herbs are used in TCM to treat these “imbalances.” Among the most commonly used by Western herbalists as analogues for the Chinese herbs for moving liver qi and cooling heat are dandelion (Taraxacum officinale), yellow dock root (Rumex crispus), burdock root (Arctium lappa), motherwort (Leonurus cardiaca), and bupleurum (Bupleurum falcatum). Dong quai (Angelica sinensis) is perhaps the most popularly used herb for nourishing the blood. For use of traditional Chinese herbs, women can be referred to acupuncturists and TCM herbalists.
Phytoestrogens and Menopause
Phytoestrogens are hormones made by plants for their own biological needs. They weakly activate estrogen receptors in mammals and are found in ordinary foodstuffs such as whole grains, many legumes (not just soy), root vegetables including carrots and yams, seeds (e.g., flax), and nuts, as well as in herbs. 42 43 A diet rich in phytoestrogens confers benefits such as reduction of breast cancer risk, with little effect on premenopausal women’s cycles. 44 45 46 47 Phytoestrogens may also help prevent osteoporosis, high blood pressure, heart disease, and senility. 48 49 Phytoestrogens are ubiquitous in plants; only a totally plant-free diet would prevent exposure to them. Thus, phytoestrogenic foods are generally considered safe for long-term, daily use. Phytoestrogenic herbs and supplements, however, may not be safe for daily or long-term use for women at risk of developing estrogen-dependent cancers.50
A FEW WORDS ON EXERCISE
Although exercise alone is not sufficient to prevent heart attacks, osteoporosis, or fractures, it is vitally and tremendously important in their prevention and for the promotion of healthy hearts, healthy bones, and longevity.51 Exercise not only strengthens bone, it also increases muscular flexibility and improves balance. A broken bone can cause a fall, but poor balance leads to more falls and more broken bones. Plus, of course, exercise improves the functioning of the heart, counters depression, and may even help prevent breast cancer. The amount of exercise needed varies, but 30 minutes daily is a goal most women can easily achieve and maintain. Any kind of exercise helps, but best results are found with a mix of strength building (such as weight training), simple walking—brisk if possible, and flexibility improvement with tai chi and yoga. Best of all, we are never too old and never too unfit to begin benefiting from some form of exercise.
SUMMARY
HORMONE REPLACEMENT THERAPY: RISKS, BENEFITS, ALTERNATIVES
Today, the main reasons for prescribing HRT are relief of menopausal symptoms and prevention or management of osteoporosis. Strong evidence from both observational studies and RCTs show estrogen to be highly effective for controlling hot flashes and genitourinary symptoms.54 Urogenital atrophy and vasomotor instability are improved with HRT.
CONVENTIONAL TREATMENT APPROACHES
Until relatively recently, the allopathic gold standard of treatment for menopause has been HRT. Approximately 38% of postmenopausal women in the United States in 1995 used HRT, estrogen with or without progestin, to treat symptoms of menopause and prevent chronic conditions such as cardiovascular disease and osteoporosis.55 In 2000, 46 million prescriptions were written for Premarin (conjugated equine estrogens), making it the second most frequently prescribed drug in the United States.56 HRT was indicated for the classic symptoms of hot flashes and night sweats, which related to declining estrogen levels and are reported by 85% of US menopausal women. 57 58 HRT can effectively treat menopausal symptoms such as vasomotor instability (hot flashes), mood swings, concentration difficulties, dyspareunia, and vaginal irritation caused by dryness.59
For women with an intact uterus, HRT includes both an estrogenic agent and a progestin. Progestins are generally indicated to offset the increased risk of endometrial cancer with the use of unopposed estrogen. For women using both an estrogenic agent and a progestin, there is a choice between cyclic and continuous dosing regimens. With the cyclic dosing regimens (intermittent high-dose progestin and estrogenic withdrawal), women can anticipate resuming a predictable (but artificial) menstrual cycle. With the continuous regimens (continual estrogen and low-dose progestin, without withdrawal), women can anticipate amenorrhea with occasional erratic spotting. Progestins are usually not recommended for women who have had a hysterectomy.60
The preventive effects of HRT on long-term health outcomes are now challenged by new data from clinical studies. In terms of beneficial effects, randomized clinical trials have proved that HRT is effective for vasomotor and urogenital symptoms.61 A meta-analysis of estrogen treatment (oral or intravaginal) for urinary incontinence revealed a significant improvement in subjective symptoms, but no improvement in objective measures such as urodynamic testing.62 It is unclear if HRT helps directly with depression and other nervous system disorders. A “domino” effect may occur; for example, relieving hot flashes may improve sleep, which may improve mood.63
Osteoporosis
Another area where HRT was found to be helpful was for the treatment of osteoporosis. In the United States, 4 to 6 million women have osteoporosis. The consequence is that more than 250,000 hip fractures occur annually, with a health care cost of approximately $14 billion per year. Hip fracture carries a 10% to 20% risk of death within a year and a 25% chance of institutionalization.64 After age 35 men and women start to lose approximately 1% of bone mass each year. However, bone loss is accelerated during the first 3 to 4 years after menopause. Estrogen therapy inhibits age-related bone loss after menopause by acting on osteoclasts (bone resorbing cells) and osteoblasts (bone-building cells) to decrease bone resorption. Estrogen also helps calcium to be absorbed in the gut. The daily dosage required to prevent bone loss is 0.625 mg of conjugated estrogen, but even 0.3 mg may suffice if taken with adequate calcium supplements.59 Estrogen must be taken for at least 7 years to provide significant benefit and the risk of osteoporosis reverts back to baseline once the estrogen is discontinued.54 Bone loss resumes within a year after stopping HRT, however, and bone turnover rises to the level of that in untreated women within 3 to 6 months.65 Randomized controlled trials have shown that HRT reduces bone loss at clinically relevant sites such as the spine and neck of the femur.66 The Women’s Health Initiative (WHI) study was the first randomized controlled trial to show a reduction in hip fracture with HRT.67 No herbal product studied has been proven effective in the prevention or treatment of osteoporosis.68
Nonhormonal therapies such as bisphosphates (e.g., Fosamax) and selective estrogen receptor modulators (SERMS) are as effective as HRT for preventing fractures. Bisphosphates inhibit osteoclast activity in the bone. Randomized controlled trials have demonstrated Fosamax efficacy increasing BMD and reducing fractures.69 Etidronate (Didronel) is another bisphosphate. It is FDA-labeled for the treatment of Paget’s disease, but has had an off-label use as a treatment for osteoporosis in patients who cannot tolerate Fosamax. Intranasal calcitonin is a polypeptide hormone that also inhibits osteoclastic activity; an intranasal form is now available for treatment of established osteoporosis. A selective estrogen receptor modulator, raloxifene (Evista), has been FDA labeled for prophylactic treatment of osteoporosis. For women whose main interest is prevention of osteoporosis, this agent offers an alternative to traditional HRT. Other selective estrogen receptor modulators pending FDA labeling include droloxifene and idoxifene.59
Colorectal Cancer
Observational studies have consistently suggested that HRT reduces the risk of colorectal cancer. The WHI study, however, was the first randomized controlled trial to confirm this, reporting six fewer colorectal cancers each year in every 10,000 women taking HRT compared with the placebo group.67
Cardiac Disease
Recent studies have cast doubt on the cardioprotective effects of HRT, the most frequently cited reason for starting women on HRT—further undermining conventional recommendations. Today, the results of the WHI have radically changed the way doctors are prescribing HRT. The WHI, the largest randomized trial of HRT, showed that long-term use of HRT poses more risks than benefits for healthy postmenopausal women. The WHI studied the use of estrogen plus progestin for prevention of coronary heart disease in 16,608 postmenopausal women age 50 to 79 years. After 5 years of follow-up, this arm of the study was stopped because of the adverse effects of the intervention. The researchers found that HRT increases the risk of several events: coronary heart disease events, invasive breast cancer, stroke, venous thromboembolic events, and pulmonary embolism.67
The Heart and Estrogen/Progestin Replacement Study (HERS) examined the effects of HRT in postmenopausal women with coronary artery disease. HERS was a large randomized controlled trial of 2763 women with an average follow-up time of 4.1 and 6.8 years. It showed no statistically significant difference between the HRT (estrogen plus medroxyprogesterone) group compared with the placebo group in either the primary outcomes (nonfatal myocardial infarction or coronary heart disease death) or in the secondary outcomes (coronary revascularization, unstable angina, congestive heart failure, resuscitated cardiac arrest, stroke or transient ischemic attack, and peripheral arterial disease). However, further analysis showed a significant time trend, with more coronary heart disease events in the hormone group than in the placebo group during the first year of treatment and fewer in years 3 to 5. The recommendation after the HERS study was that postmenopausal HRT should not be used for reducing risk of coronary heart disease.70 Thus, the WHI and HERS trials have shown that continuous treatment with 0.625 mg of conjugated equine oestrogens plus 2.5 mg of medroxyprogesterone increases the risk of heart disease events by 29% (37 vs. 30 per 10,000 person years) and stroke by 41% (29 vs. 21 per 10,000 person years). 67 70
Thromboembolic Disease
Studies generally show an increased risk of deep venous thrombosis and pulmonary embolus in women taking HRT. 71 72 History of or risk factors for these conditions are contraindications to the use of HRT.
Endometrial Cancer
More than 30 observational studies have shown that unopposed estrogen therapy increases the risk of endometrial cancer. Progestin use in women with a uterus mitigates the risk of cancer associated with estrogen.54
Breast Cancer
A large meta-analysis of data from 51 observational studies reported that the risk of breast cancer increased by 2.3% for every year of use of HRT.11 This increased risk does not become significant unless HRT is taken for more than 5 years. The risk of breast cancer falls after stopping HRT and returns to baseline within 5 years.
Because the WHI study stopped early, it could not examine the risk of death from breast cancer. However, it did confirm the excess risk of breast cancer with HRT. There was a 15% increase in invasive breast cancer in women taking estrogen plus progestogen for less than 5 years and a 53% increase in those taking it for more than 5 years. The study concluded that for every 10,000 women taking estrogen and progestogen, there would be eight more cases of invasive breast cancer a year. 11 67
Mood and Cognitive Changes
Studies have also indicated that many cases of depression relate more to life stresses or “mid-life crises” than to the hormonal changes of menopause.60 Menopause is not only a physical change but also a social transition. These transitions include an alteration in family roles, grown children leaving home; a changing social support network; a changing relationship with one’s partner; parents or other close relative die; and changes in finances as one looks to retirement. Dysphorias, irritability, anger, memory loss, and losses of clarity of thought are among the most frequent symptoms reported by menopausal women, although the research data on the role of estrogen loss to depression and cognitive changes are mixed.60 It is often the presence of mood- or memory-related symptoms that motivates a woman to request HRT. Physicians are now prescribing SSRIs to help women with these symptoms.
SIDE EFFECTS OF HRT
There are many reasons for noncompliance with HRT, but the most commonly cited include thrombotic complications, side effects on mood, and changes in the breasts.60 Only about one in three women stay on HRT after a year, secondary to side effects. Adverse effects attributed to HRT include breast tenderness, breakthrough bleeding, and thromboembolic disorders. In addition, there are relative and absolute contraindications to the use of HRT (Box 19-1).
WOMEN’S OPINIONS OF HRT
Women’s experiences of menopausal symptoms vary widely and have been found to relate to factors such as social class, ethnicity, and culture. The most common reason motivating women to take HRT is the relief of menopausal symptoms. Prior to the WHI, women who were trying HRT were having serious concerns about its use, and discontinuation was a major issue. 73 74 In 1995, a survey of women aged 50 to 80 found that 50% of women who had never used HRT believed that hormones were unnecessary, and 18% believed that menopause was a natural event not requiring medication. Safety concerns were expressed by nearly 30% of women who never used HRT, including fear of cancer (15.3%) and fear of side effects (12.9%).75 Only a third to a half of women who leave their physician’s office with a prescription for HRT are still taking it 1 year later. Women express concerns about the prospect of having menses indefinitely, the potential side effects of HRT, and the increased risk of cancer. 76 77 Forty percent of women discontinue HRT within 8 months of initial therapy or never fill the prescription.78 Women who are currently using HRT are more likely to have had a hysterectomy than women who have never used HRT. In one survey of women who had undergone a hysterectomy, 50% of women were using HRT, 37% of women had used it in the past, and 24% of women never used HRT.75
NATURAL HORMONES
The most frequently prescribed estrogen in the traditional HRT regimen is conjugated equine estrogen (CEE). As public awareness of the source of CEE has grown, more women find this choice objectionable, whether out of concern for animal rights or out of an aversion to ingesting hormones that come from horse urine.79 There has been a demand for natural sources of estrogen.
The three most common forms of estrogen produced by the body are estradiol (E2), estrone (E1), and estriol (E3). Estradiol, produced by the ovaries, is the most potent. Estrone becomes the most plentiful estrogen after menopause. Estriol is the weakest and is the estrogen that becomes more plentiful during pregnancy.80 Estradiol can be produced from plants, and there is a growing market for such products. These estrogens are referred to as “natural” or “bioidentical” hormones, and are formulated by compounding pharmacies. There is little in the medical literature about these hormones. Additionally, among the lay public, there has been a growing demand for individually compounded hormone regimens. This demand is in response to the work of Wright and others who argue that HRT should mimic the ratios of E1, E2, and E3 naturally found in the body, or roughly 3%, 7%, and 90%, respectively. 80 81 This combination is known by the name of triestrogen or Tri-Est, which may consists of 1 mg estriol (E3), 0.125 mg estrone (E1), and 0.125 mg estradiol (E2) taken twice daily. This is equivalent to 0.625 mg CEE. There is also a product on the market called Bi-Est or biestrogen, which is estriol and estradiol. Bioidentical estrogens are compounded into sublingual troches, transdermal creams, and gels. Although only recently gaining popularity in the United States, these products have been used extensively in Europe where they are very popular. Although these estrogens are compounded in doses equivalent to prescription estrogens, and appear to have equivalent effects in regards to stimulation of the endometrium, there are, thus far, no studies that look at their safety or efficacy, particularly in regard to preventing or treating osteoporosis.80 Although these are “natural” products, the safety of this estrogen and progesterone is being questioned following the publication of results from the Women’s Health Initiative.
PROGESTERONE
Progesterone plays a very important role in the shedding of the endometrium to avoid endometrial hyperplasia in postmenopausal women after they are exposed to estrogen in HRT. Therefore, it is now standard care to prescribe some form of progesterone with HRT in women with intact uteri. It is also believed that progesterone has additional benefits and risks. Synthetic progestins such as medroxyprogesterone and norethindrone have been shown to decrease vasomotor symptoms. 82 83 Reported androgenic effects of synthetic progestins include fluid retention, glucose metabolism, reduction of HDL cholesterol levels, headaches, and mood disturbance.84 Furthermore, it was recently reported that women who were given HRT using a synthetic progestin had an increased rate of breast cancer compared with women who took estrogen alone.15
Natural progesterone taken by mouth is inactivated in the gastrointestinal tract. However, micronizing progesterone is a process designed to increase the half-life of progesterone and reduce its destruction in the gastrointestinal tract. Micronization decreases particle size and enhances the dissolution of progesterone.84 Unlike synthetic progestins, micronized progesterone has not been shown to affect mood or lipid profile (or adversely affect pregnancy outcome). 84 85 The most commonly reported side effects are fatigue and sedation. Extensive use in Europe has shown that the micronized form can be taken once daily and is as effective as the synthetic progestins in controlling endometrial growth, while displaying significantly fewer metabolic side effects. 80 86
A number of compounding pharmacies make natural progesterone products as alternatives to medroxyprogesterone acetate. Certain plants, including wild yam and soybeans, produce sterols called saponins that have chemical structures similar to progesterone. These sterols can be used as precursors for progesterone in the pharmacy. Most preparations that contain bioidentical progesterone contain United States Pharmacopeia (USP) grade progesterone, formulated from these plant sterols and manufactured by Pharmacia Upjohn (Peapack, NJ) and sold in bulk.80 The hormone is not available from any natural source without extraction and synthesis. The body is not able to convert plants such as wild yam into progesterone on its own. Contrary to popular understanding, wild yam creams provide no active hormones because the sterols in plants cannot be converted into active steroidal compounds.87 Only wild yam creams to which bioidentical progesterone has been added will exert a progesterogenic effect. Bioidentical progesterone is sold as a topical cream, a vaginal gel, and rectal or vaginal suppositories. The transdermal cream is formulated to contain 400 mg progesterone/oz and is easily absorbed into the skin. The usual dose is ¼ and ½ tsp once or twice a day. Recent research has cast doubt on whether the transdermal creams, even in prescription strengths, provide serum levels sufficient to protect the endometrium.88
In a double-blind placebo-controlled trial, 102 healthy women within 5 years of menopause applied 20 mg transdermal progesterone cream or placebo daily for 1 year. Each woman received daily multivitamins and 1200 mg of calcium and was seen every 4 months for review of symptoms. Improvement or resolution of vasomotor symptoms, as determined by review of weekly symptom diaries, was noted in 83% of treatment subjects and 19% placebo subjects. However, the number of women who showed gain in bone mineral density exceeding 1.2% did not differ.89
BOTANICAL ALTERNATIVES TO HRT
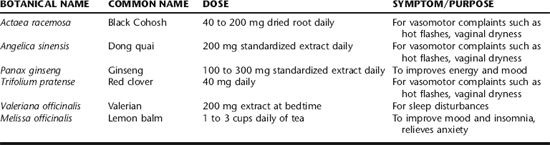
In the past several years, more than 100 OTC products targeted for menopausal women have reached the market, and women spend an estimated $600 million per year on these products. For nearly 70% of women, the transition into menopause is smooth;90 however, many women seek advice for management of symptoms such as hot flashes or vaginal dryness. Women also seek information on the prevention of associated long-term health problems such as osteoporosis and coronary artery disease. It is essential that the practitioner address the whole woman. An individual assessment of her health risk factors and preferences for supportive care are chosen based on the symptoms she experiences, her risk of heart disease, breast cancer, and osteoporosis. This section addresses the clinical findings for botanicals commonly used as substitutes for HRT, or as treatments for menopausal concerns (Table 19-1). Specific menopausal concerns are also addressed in individual chapters.
Red Clover
Red clover was not traditionally used on a long-term basis for hot flashes, but today it is commonly used as an “estrogen substitute” for menopausal symptoms and the prevention of osteoporosis. Red clover contains phytoestrogenic isoflavones such as formononetin, biochanin A, daidzein, and genistein. Red clover has estrogenic properties on endometrial and breast cancer cells in vitro. 91 92 It is unknown whether long-term use has an estrogenic effect on the breast or endometrium. One small double-blind, randomized controlled pilot study looked at the effect of a 3-month course of a 33 mg red clover isoflavone supplement on endometrial cells taken between days 8 and 11 of the menstrual cycle. In this study of 30 late-reproductive age and perimenopausal women, there was no difference in endometrial index or thickness compared with the placebo groups.93 Red clover extract is marketed as Promensil™ in Europe; it contains 40 mg isoflavones per tablet, which is approximately equivalent to the isoflavone content of a cup of soy milk and 5 cups of chickpeas. Promensil, a red clover isoflavone preparation, showed significant estrogenic activity, equivalent to 10 to 8 mol/L estradiol.94 A 30-week small double-blind, randomized crossover trial of 43 perimenopausal and menopausal women with three hot flashes daily found no significant difference between Promensil (40 mg) or placebo to manage hot flashes.95 A randomized, double-blind placebo-controlled prospective trial of 37 postmenopausal women with symptoms of estrogen deficiency was performed over a 12-week period. The women were randomized to three treatment groups: placebo, 40 mg, or 160 mg (isoflavone extract containing red clover isoflavones). There was no significant difference in the incidence of flashes among the three groups. There was no difference between the groups in Greene Menopause Symptom Scores, vaginal pH, levels of follicle stimulating hormone (FSH), sex hormone binding globulin (SHBG) or total cholesterol, liver function, or blood parameters. A statistically significant increase in high-density lipoprotein (HDL) cholesterol of 18.1% (p = 0.038) occurred in the 40-mg group.96 Isoflavones have been found to increase arterial compliance in postmenopausal women,97 thus presumably reducing heart disease risk. In another double-blind, randomized study, 60 postmenopausal women received either a commercially available red clover isoflavone supplement (80 mg/day) or placebo for 90 days. In this trial, red clover isoflavone supplementation significantly decreased the rate of menopausal symptoms and had a positive effect on vaginal cytology.98 A recent meta-analysis and systematic review showed mixed benefits in reducing hot flashes compared to placebo. 99 100
Although clinical research is lacking, the phytoestrogenic effects of red clover may, in theory, produce undesirable or unpredictable effects in the face of hormone-dependent tumors. Therefore, caution is advised in patients with estrogen receptor–positive neoplasia,101 and patients taking hormonal or antihormonal medications such as tamoxifen. 101 102 Use with caution in patients susceptible to bleeding problems or those taking anticoagulants.101
Dong Quai
For the past 3 years, sales of Rejuvex™, the most popular health remedy containing dong quai, have been extensive among hundreds of thousands of users in the United States.103 In the Chinese Materia Medica, dong quai is indicated for disorders of the women’s reproductive system, including menopausal symptoms, dysmenorrhea and irregular periods, and menstrual cramps, and is used to “strengthen the blood.” The symptoms of “deficient blood” listed in Chinese texts are similar to those that Western medicine associates with menopause: menstrual flow abnormalities, nervousness, dizziness, insomnia, and forgetfulness.60 Dong quai, traditionally prescribed as a tonic for women, is most commonly used as part of a mixture. It is sold in the United States for use alone or as part of newly formulated, nontraditional herbal combinations.
Its chemical constituents include furocoumarins, beta-sitosterol, flavonoids, and others. However, its presumed mechanism of action remains unknown. In a double-blind, randomized controlled study, 71 post-menopausal women age 40 to 65, were instructed to take three capsules three times daily, equivalent to taking 4.5 g of dong quai root daily (standardized to 0.5 mg/kg ferulic acid). There was no difference in Kupperman index scores, number of hot flashes, or endometrial thickness and vaginal maturation. A recent systematic review found dong quai to be ineffective in ameliorating menopausal symptoms at the dosages and preparation in the clinical trials reviewed.99
It would be valuable to study TCM formulas prescribed in accordance with TCM diagnostic methods. Dong quai does not contain the typically reported phytoestrogens, and the data on stimulation of estrogen receptor-positive breast cancer cells or binding to estrogen receptors are conflicting. 91 92 104 Dong quai contains coumarins and can cause bleeding when administered concurrently with warfarin; the furocoumarins contained in dong quai can cause photosensitization.
Black Cohosh
Black cohosh (Fig. 19-2) is widely used in Europe and has become increasingly popular in the United States as a treatment for menopausal symptoms (e.g., hot flashes and vaginal dryness). Since 1956, over 1.5 million women in Germany have used black cohosh extract, and in 1994 menopausal women in Germany, Scandinavia, and Austria used over 6.5 million monthly dosages of black cohosh extract.105 It is an indigenous North American plant long used by Native American populations. Black cohosh contains several triterpenes and isoflavinoids. Other constituents are ascorbic acid, beta-carotene, butyric acid, calcium, chromium, selenium, thiamine, zinc, and salicylic acid. The German Commission E recommends it for premenstrual discomfort and dysmenorrheic as well as climacteric neurovegetative complaints.106
Studies of black cohosh’s physiologic effects have had mixed results. Originally, it was believed that black cohosh had estrogenic effects, but now there is evidence to dispute this claim. 91 104 107 108 Data that suggest a nonestrogenic, or estrogen-antagonistic effect of the herb on human breast cancer cells may lead to the conclusion that treatment may be a safe natural remedy for menopausal symptoms in breast cancer, but the data are mixed. 109 110 111 There are no long-term safety studies using black cohosh in women who have had breast cancer.112
In numerous case studies, standardized black cohosh monodrug preparations have been used to treat menopausal symptoms, menstrual disorders (amenorrhea, oligomenorrhea, dysmenorrhea, polymenorrhea, PMS), and complaints during pregnancy. The literature describes the efficacy of black cohosh in approximately 1500 patients with menopausal disorders, citing distinct and clear improvements in the clinical picture and good to very good therapeutic responses. 107 113 By 1960, 1256 case reports in 111 published studies by gynecologists, general practitioners, internists, and neurologists had evaluated the use of black cohosh for the treatment of menopausal symptoms with positive effects and few side effects.113 Most of the clinical trials assessing the use of black cohosh for menopausal complaints have been carried out using Remifemin® [Schaper & Brummer Gmb & Co., Salzgitter-Ringelheim, Germany]. Remifemin is standardized with respect to triterpene glycoside content, with each 20-mg tablet containing 1 mg of 27 deoxyactein; it is also available in a standardized liquid extract. Remifemin is the most clinically studied black cohosh product and has been the subject of more than 20 trials over the last 40 years. For an assessment tool, many studies have used the Kupperman Menopausal Index, which is a weighted sum of 10 individual symptoms: hot flashes, outbreaks of sweating, sleep disorders, nervousness, irritability, dizziness, difficulty in concentration, joint pains, headaches, and palpitations.114 The clinical trials are generally of poor methodically quality, small, and lack a control group. The results are mixed but most studies show benefit. 115 116 117 118 119 120 121 122 123 124 Recent systematic reviews demonstrate that majority of studies indicate that extract of black cohosh (Actaea racemosa L.) improves menopause-related symptoms. 99 125 126
Black cohosh is not usually used on a long-term basis, and no clinical trials have lasted for more than 6 to 12 months. However, the safety profile is reassuring and black cohosh is well tolerated. 127 128 Tolerability of Remifemin appears to be good, with mild GI symptoms being the only significant adverse effect. Although black cohosh may be useful for menopausal symptoms, long-term use cannot be presumed to be safe until appropriate safety studies are conducted. Research by the German manufacturer has shown that black cohosh supplements have no effect on follicle-stimulating hormone, luteinizing hormone, estrone and estradiol, progesterone, sex hormone binding globulin, the vaginal maturation index, or endometrial thickness.129 To date, four case reports of possible hepatotoxicity have been published, although previous safety reviews suggest that black cohosh is well tolerated and adverse events are rare when it is used appropriately. 99 126 130 Additionally, there is one case report of a woman with severe asthenia and very high blood levels of creatine phosphokinase and lactate dehydrogenase after using black cohosh.131 (See Plant profiles: Black cohosh for a safety discussion.)
Evening Primrose Oil
Evening primrose oil, borage oil, and black currant seed oil produce seeds that contain gamma linolenic acid (GLA). A 6-month randomized double-blind placebo controlled trial was conducted with 56 menopausal women who reported having hot flashes three or more times a day. Participants were randomized to receive evening primrose oil 2000 mg with 40 mg vitamin E twice daily or placebo. Twenty-one women discontinued the study caused by a poor clinical response to the treatment, 10 taking evening primrose oil and 11 taking placebo. This study showed that evening primrose oil had no benefit over placebo in the alleviation of vasomotor symptoms.132 A recent systematic review found no benefit.99
Panax Ginseng
Ginseng is reputed to be an aphrodisiac and to have estrogenic actions that improve menopausal symptoms. The Ginsana Corporation in Switzerland, the largest manufacturer of ginseng products worldwide, conducted a 16-week placebo-controlled trial in almost 400 postmenopausal women. 1 333 Although vasomotor complaints were not reduced, improvements were noted on scales used to rate depression and general health and well-being. Assessments of estrogenic effects, including the maturation index and measurement of plasma follicle-stimulating hormone and estradiol over a 16-week period, showed that there was no difference between the effects of ginseng and those of placebo.133 A randomized, multicenter, double-blind, parallel study on symptomatic postmenopausal women assessed the effects of 16 weeks’ treatment of standardized ginseng extract or placebo on quality of life and on physiologic parameters. To assess the efficacy of ginseng on postmenopausal symptoms, physiologic parameters [follicle-stimulating hormone (FSH) and estradiol levels, endometrial thickness, maturity index, and vaginal pH] were recorded at the same time points. Of the 384 randomized patients (mean age 53.5 ± 4.0 years), the questionnaires were completed by 193 women treated with ginseng and 191 treated with placebo. No differences were found between treatment subjects and placebo control is vasomotor symptoms, but significant improvements were reported on the quality measures for depression and well-being in favor of ginseng compared with placebo. Physiologic parameters such as FSH and estradiol levels, endometrial thickness, maturity indexes, and vaginal pH was not affected by the treatment.134 In a double-blind placebo controlled study, 57 postmenopausal women were randomly assigned to 12 weeks treatment with Gincosan (320 mg/day), containing 120 mg Ginkgo biloba, and 200 mg Panax ginseng or placebo. The researchers found no significant effects of Gincosan treatment on ratings of mood, bodily symptoms of somatic anxiety, menopausal symptoms, or sleepiness or on any of the cognitive measures of attention, memory or frontal lobe function. Additionally, a recent systematic review found no benefit to using ginseng for menopause symptoms.99 Ginseng’s adverse reactions include nervousness, gastrointestinal upset or diarrhea, insomnia, dizziness, headache, euphoria, blood pressure effects, and vaginal bleeding.135 Case reports link ingestion of ginseng with postmenopausal bleeding. 136 137 One case of postmenopausal bleeding occurred after topical use of a ginseng-containing face cream.138
Soy
Lower estrogen levels and longer menstrual cycles have been reported with soy-rich diets. Menopausal symptoms are reported to be less problematic in cultures (particularly Asian cultures) in which the diet is predominantly plant based and contains a lot of soy. Soy protein appears to be effective in reducing hot flashes, bone loss, and total and LDL cholesterol level.139 The consumption of soy may reduce the frequency, severity, and incidence of hot flashes, but clinical studies and systematic reviews have showed mixed results. 140 141 142 143 144 145 14 The majority of phytoestrogens found in human diets are divided into two classes: isoflavones and lignins. Isoflavones are found predominantly in soy foods and other legumes such as chickpeas, pinto beans, and lima beans. Lignins are found in whole grains, seeds (particularly flax), and some fruits and vegetables. Soy supplement products are not recommended; whole food sources are optimal.
ADDITIONAL THERAPIES
For women with mild to moderate menopausal complaints, simple lifestyle modifications (Table 19-2) may be enough to cope with the discomforts of this change without medications of any kind. Diet, exercise, and comfort measures can reduce hot flashes and other discomforts mildly to significantly.
| TREATMENT | HOW IT HELPS |
|---|---|
| Diet | |
| High fiber | Decreases heart disease, decreases constipation, helps maintain weight |
| Low fat | Improves cholesterol, helps maintain weight |
| Rich in antioxidants | May decrease hot flashes and other menopausal symptoms |
| Increase soy | May decrease hot flashes, part of a heart-healthy diet |
| Exercise | |
| Cardiovascular | Decreases CAD risk, improves mood, aids sleep, helps maintain weight |
| Weight-bearing and strengthening | Improves bone health, may decrease hot flashes, helps maintain weight |
| Smoking cessation | Decreases heart disease, decreases smoking-related cancers, decreases osteoporosis risk, may decrease hot flashes |
| Decrease alcohol consumption | May decrease hot flashes, decreases osteoporosis risk |
| Maintain regular sexual activity | May decrease vaginal dryness (use it or lose it), may improve depressive symptoms |
Key dietary recommendations include the following:
Some have suggested that regular aerobic exercise lessens the frequency and severity of hot flashes.147 Studies show that women who regularly exercise are less likely than their counterparts to experience severe hot flashes. In one observational study of 1323 women in Sweden, 15% of sedentary women experienced “severe” hot flashes, compared with only 5% of the subjects who exercised.148
There are many simple lifestyle changes women can make to help with hot flashes. The practice of wearing light, “breathable” cotton clothing helps, as does layering clothing. Other suggestions include keeping the ambient temperature of a room low; and avoiding hot, spicy foods, caffeine, and alcohol. Women also can benefit from stress reduction. In one study, women were taught “paced breathing,” a biofeedback technique that lowered their rate of hot flashes.149 Diet and exercise also decrease bone loss. Other benefits can be derived from stopping smoking, decreasing soda and alcohol consumption, and improving dietary calcium intake.
Several studies have shown a benefit of calcium on improving bone density in both adults and children. There is no definitive evidence, however, that it lowers fracture risk. Calcium remains an important adjunct to the prevention and treatment of osteoporosis. Women should be encouraged to get their calcium through dietary intake of calcium-rich or fortified foods, but most women have trouble getting enough through diet. The aim for postmenopausal women should be a daily intake of 1000 to 1500 mg. Vitamin D supplementation should be a part of any osteoporosis prevention program. Studies have shown a decrease in fracture rates in older people treated with vitamin D, compared with those on placebo. 150 151 Present evidence suggests a daily dose of 400 to 800 IU may be required. Research has shown that people whose diets are rich in both magnesium and potassium have denser bones.152
CASE HISTORY:
The following herbal protocol was recommended for anxiety and insomnia:
A follow-up in 3 months found Clare with symptoms much improved, and still taking the Remifemin.
HOT FLASHES AND NIGHT SWEATS
Bhaswati Bhattacharya and Aviva Romm
Approximately 75% of women in the United States experience hot flashes, one of the most common vasomotor symptoms of perimenopause. Hot flashes and night sweats typically accompany the onset of menstrual irregularity, as estrogen levels begin to decline. Women report a feeling of (sometimes intense) heat on the face, neck, and upper chest, which quickly progresses to a generalized feeling of being overheated. The sensation lasts for 2 to 4 minutes and may be accompanied by sweating and palpitations. The episode is often followed by chills and shivering, particularly when episodes occur at night. Hot flashes may occur several times daily. Rarely, extremely frequent hot flashes occur—as often as hourly throughout the day and night.
Night sweats are a common source of significant sleep disturbance. Women may awake soaked from a night sweat. Sometimes, they are severe enough to necessitate a change of bedding, requiring the woman to wake fully, which further interrupts sleep. Severe sleep disturbance may be accompanied by daytime symptoms such as irritability, fatigue, depression, memory loss, and other disturbances in mental acuity. Sleep deprivation decreases functioning at daily tasks, increases the risk of accidents and injuries, and is an often-unrecognized source of marital tension, particularly when the partner’s sleep also becomes disturbed by the woman’s waking.153
Studies show that 72% to 80% of perimenopausal women consider hot flashes one of the most disturbing and disruptive symptoms they experience.154 Addressing hot flashes in the history intake is pertinent, as not all women report hot flashes, sleep disturbances, and related symptoms unless specifically queried about their presence. Because not all women identify vasomotor symptoms as “hot flashes,” with descriptions of the symptoms varying based on education and cultural background, careful inquiry and creative questioning is important.
HOT FLASHES AROUND THE WORLD
According to the World Health Organization, menopausal vasomotor symptoms are not as problematic for women worldwide as they are for women in the United States and other Westernized nations.155 Reported percentages are: Mayan women 0%, Hong Kong women 10% to 22%, Japanese women 17%, Thai women 23%, US women 45%, and Dutch women 80%. Cultural differences in attitudes toward menopause play a role in these epidemiologic differences; it is also postulated that the common denominator in reduced vasomotor symptoms also may result in part from disparities in phytoestrogen content of the diet and variations in amounts of exercise.155
HOT FLASH PHYSIOLOGY
Nonhormonal Treatments for Hot Flashes
Since the WHI study raised concerns about the safety of estrogen, women have been increasingly requesting nonhormonal treatments for menopausal symptoms. 156 157 Alpha-adrenergic agents such as clonidine have been used to relieve hot flashes and night sweats (especially at nighttime, as they may cause drowsiness). Its hypotensive effects also may limit its use for normotensive patients during the day.158 Patients often experience edema and weight gain with continued use; rebound hypertension upon discontinuation is a potentially serious medical problem. Other nonhormonal treatments that are currently used and considered effective with relatively good safety profiles include SSRIs and gabapentin, a combination of ergotamine, belladonna alkaloids, and phenobarbital that has been used for many years to relieve climacteric symptoms, and “off-label” use of megestrol acetate, which also may help control hot flashes. 157 159 160 161 SSRIs have shown a 19% to 65% reduction in hot flashes, whereas clonidine has shown a reduction of 15% to 20%.157 Gabapentin has been found to be more effective when combined with SSRIs than when used alone.162
Hormone Replacement Therapy
Estrogen and progestins are clearly effective in the reduction of hot flashes and have been a mainstay in the medical management of vasomotor symptoms; however, the use of HRT is accompanied by significant health risks. Should other alternative and conventional therapies prove ineffective in alleviating symptoms, and HRT be desired, some authors suggest that some of the personalized HRT prescriptions available through compounding pharmacies may minimize the risks associated with hormonal supplementation with equivalent efficacy.163
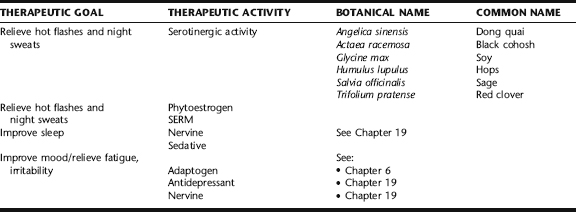
THE BOTANICAL PRACTITIONER’S PERSPECTIVE
It is estimated that 50% to 75% of women use alternative therapies for the management of menopausal symptoms (Table 19-3), and the prevalence may be even higher in breast cancer patients. 164 165 Among the most commonly used botanical products are phytoestrogen-rich soy supplements, isoflavone-rich red clover products (e.g., Promensil), and black cohosh products (e.g., Remifemin). Herbal practitioners recommend herbs to “regulate” hormones and herbs for their “cooling” effects. Herbs rich in phytoestrogens and volatile oils, which may themselves exert estrogen-like or directly estrogenic effects (e.g., soy, red clover, sage, and hops), are highly favored for hot flashes and night sweats. Herbs are also used to treat concurrent symptoms (e.g., insomnia, irritability, or depression), an essential component in improving a woman’s overall sense of well-being while treating hot flashes. Holistic practitioners also encourage a variety of general comfort measures (see General Recommendations) to reduce the incidence of hot flashes and night sweats. Adaptogens can play a major role in hormonal regulation, as well as mediation of the sympathetic response, thereby providing underlying support to the system that can help to correct dysregulation. Important adaptogens to consider include ashwagandha (Withania somnifera), American ginseng (Panax quinquefolim), and eleuthero (Eleutherococcus senticosus), among others. Readers are directed to Chapter 8 for a complete discussion of adaptogens.
Phytoestrogens
The most commonly discussed plant compounds associated with perimenopausal therapies are the phytoestrogens. With a steroid ring structure similar to the estrogens, phytoestrogens are naturally occurring plant compounds that weakly bind to human estrogen receptors. Phytoestrogens are classified chemically into three main categories: isoflavones found in legumes such as soy, alfalfa, lentils, chickpeas, pinto beans, and lima beans; phytosterols such as coumestans, found in red clover, sunflower seeds, and bean sprouts; and lignins, found in flax seeds, fruits, vegetables, and whole grains. Lignins are converted by bacteria in the gut to enterodiol and enterolactone, and absorbed by the body to use for synthesizing the isoflavone subtypes: genistein, daidzein, and equol. Because they bind receptors weakly, phytoestrogens act as competitive agonists, blocking stronger estrogens from binding except at high concentrations. Genistein is clearly a bioactive molecule. It displays characteristics of a selective estrogen receptor (ER) modulator (SERM) rather than an estrogen, showing affinity for ERβ.166
Japanese women consuming a traditional Japanese diet, which is typically rich in soy products and vegetables, were found to have between 100 and 1000 times higher levels of urinary phytoestrogens than US and Finnish women eating omnivorous diets.167 It has been proposed that phytoestrogens are a factor in the report of fewer hot flashes by Japanese women. However, trials evaluating the effects of soy supplements on hot flashes have not consistently found benefit. There is speculation that it is lifetime exposure to soy, as would occur in a traditional diet, that confers protective effects.168 Of 12 clinical trials evaluating soy or soy isoflavones for the treatment of menopausal hot flashes, only four showed improvements.163 A recent meta-analysis of evidence on phytoestrogen consumption and menopausal symptoms from 1966 to 2004 concluded that there is no benefit to phytoestrogens.145 These inconsistent results may be related to methodologic issues with dietary monitoring or great variation in products used in the trials. 169 170 It should be noted that most of the clinical research on soy has involved the use of commercially processed soy proteins and not traditional soy foods, yet traditional soy foods are considered to be more effective than supplements. 168 169 171 Genistein, with few exceptions, is not a major isoflavone in most soy foods and products unless these have been fermented, as in traditional foods such as tempeh, natto, and to some extent, miso.166 Further, only 30% to 50% of the adult population possesses the intestinal bacteria capable of converting the soybean isoflavone daidzein into the isoflavonoid equol.169
Although soy products (soy, miso, tempeh, natto) may only minimally reduce hot flashes, they do so in the context of providing other health benefits, including a beneficial effect on cholesterol and possible prevention of osteoporosis. Caused by the long-term, large-scale exposure of humans to dietary soy without deleterious effects, regular consumption of fermented soy products is considered safe. Soy isoflavone supplementation has been recommended at a dose of 60 to 100 mg/day.163 Whether to use phytoestrogens in women with estrogen-positive breast cancer is controversial and a legitimate concern. At this time, it is impossible to give a definitive recommendation. According to phytoestrogen expert Kenneth Setchell:
findings for the prophylactic effect of the SERM raloxifene on breast cancer may offer some promise for soy in the latter group. To expect that soy and its constituent isoflavones will reverse or arrest chronic disease is asking too much of this small bean. The greatest potential for soy lies not in using it to treat pathologic changes that are usually irreversible, but in including it in the diet early in life, which will, by whatever mechanism, offer the potential for preventing chronic diseases.166
It should be remembered that many legumes are rich sources of phytoestrogens, and a varied diet is optimal.
Black Cohosh
Indigenous to North America, black cohosh has long been used for the treatment of menopause symptoms, mild depression, and its sedative and muscle-relaxant properties. Modern herbalists widely use this herb for the treatment of vasomotor symptoms, reporting positive results. The German Commission E approves the use of black cohosh for climeractic complaints associated with menopause, including hot flashes. It is the most widely studied herbal medicine for the treatment of menopausal complaints.171 The bulk of clinical research on black cohosh for menopausal symptoms has used the isopropanolic extract Remifemin. Clinical trials have found noteworthy beneficial effects in the relief of hot flashes, night sweats, and other menopausal complaints, even comparable with the effects of conjugated estrogens, and statistically significant over the effects of placebo. 172 173 174 Unfortunately, the methodologic quality of the black cohosh trials is purportedly weak.163 It was postulated that black cohosh is a selective estrogen receptor modulator (SERM); however, new data suggest a lack of estrogenic effects, with recent studies showing no changes in FSH, LH levels, SHBG, or estradiol levels, and a lack of endometrial proliferation, change in vaginal cytology, or increased risk development of breast cancer regrowth in survivors taking the herb for hot flashes. 91 172 175 176 177 It is now thought that perhaps black cohosh is working through a nonestrogenic, central mechanism, possibly through serotonergic or dopaminergic pathways; however, the exact mechanisms are unknown. 147 178 Clinically, black cohosh is used in a range from 20 to 80 mg twice daily of isopropanolic extract. There appears to be little risk of women with a history of ER+ breast cancer taking black cohosh; however, one study demonstrated an increased incidence of lung metastases in mice that developed breast cancer than in controls.179 Recently raised concerns about possibly hepatotoxicity associated with black cohosh ingestion are discussed in Plant Profiles: Black Cohosh.
Dong Quai
The only randomized, double-blind placebo-controlled study of dong quai for hot flashes evaluated 71 postmenopausal women (mean age, 52 years) using 4.5 g/day dong quai root for 6 months. During the study, the hot flash incidence decreased by approximately 25% to 30% from baseline in the dong quai group, which was not significantly different from placebo.103 Dong quai is commonly used in TCM for treating gynecologic conditions. However, unlike in this trial, it is never used singly; rather, it is included in individually tailored herbal formulae. Further, it is considered a warming herb, and in some women, may actually exacerbate hot flashes. Therefore, it is prescribed only for women in whom it is appropriate based on a TCM diagnosis, and used in combination with what are considered “heat-clearing herbs” (e.g., gardenia, Gardenia jasminoides).180 Dong quai is contraindicated in women using warfarin. The herb may lead to increased vaginal or other bleeding. [This author (AR) managed the case of a menopausal woman taking a dietary supplement prescribed by an acupuncturist, consisting predominantly of dong quai, who experienced severe bleeding gums that ceased with 2 days of discontinuation of the product she had been on for 6 months and restarted on retrial.]
Hops
Hops, long used as a sedative by herbalists, is approved by the German Commission E for restlessness and sleep disorders. This, combined with its known estrogenic effects, which are considered greater than established phytoestrogens in vitro, caused by the presence of 8-prenylnaringenin, makes it an important herb to consider for treating hot flashes and night sweats. 91 163 Used in tea and tincture, often combined with herbs such as sage, passion flower, lavender, or other herbs to promote sleep, it is considered safe when used in moderate doses, although theoretically it may interfere with barbiturates and is thought by herbalists to exacerbate depression in some patients, although this is not a universally held concern.181 There are no human clinical trials evaluating the efficacy or safety of this herb. With repeated consecutive doses, it will cause drowsiness; smaller single doses promote relaxation without drowsiness.
Red Clover
Red clover (Fig. 19-3) is a rich source of phytoestrogens: formononetin, biochanin A, genistein, coumestans, and daidzein. It has demonstrated estrogenic and progestational activity in ruminants as well as in in vitro receptor binding and cell proliferation studies.91 Based on its constituents, it has been investigated for use in the treatment of menopausal symptoms. Promensil, a popular red clover product, is widely sold for its purported beneficial effects on hot flashes and other symptoms. To date, however, red clover clinical trials using 40 to 160 mg/day of red clover isoflavones have largely failed to provide evidence in favor of its use for reducing hot flashes or other menopausal symptoms. 96 181 182 One clinical trial that did demonstrate positive results was a randomized, double-blind placebo-controlled trial of 30 women with more than 12 months amenorrhea and experiencing more than five hot flashes per day. All received single blind placebo tablets for 4 weeks and were subsequently randomized to either placebo or Promensil (80 mg isoflavones) for a further 12 weeks. Efficacy was measured by the decrease in number of hot flashes per day and changes in the Greene Climacteric Scale Score. During the first 4 weeks of placebo, the frequency of hot flashes decreased by 16%. During the subsequent double-blind phase, a further, statistically significant decrease of 44% was seen in the isoflavones group, whereas no further reduction occurred within the placebo group. The Greene score decreased in the active group by 13% and remained unchanged in the placebo group.184
Sage
Sage (Fig. 19-4) is loved by herbalists for its ability to inhibit excessive sweating, and thereby finds its way into the materia medica of treatments for hot flashes and night sweats.185 It is commonly recommended as a
Protocol and Formulas for Hot Flashes and Night Sweats
Protocol 1: Hot Flashes and Night Sweats with No Other Accompanying Symptoms
Cool Down Tincture
| Hops | (Humulus lupulus) | 30 mL |
| American ginseng | (Panax quinquefolium) | 30 mL |
| Lemon balm | (Melissa officinalis) | 20 mL |
| Blue vervain | (Verbena officinalis) | 10 mL |
| Lavender | (Lavandula officinalis) | 10 mL |
| Total: 100 mL | ||
Cool Down Tea
| Sage leaf | (Salvia officinalis) | 1 tsp |
| Spearmint leaf | (Mentha spicata) | ½ tsp |
| Lavender flower | (Lavandula officinalis) | ½ tsp |
Protocol 2: Hot Flashes and Night Sweats with Anxiety
Take 3 mL black cohosh* (or equivalent) bid with the tea or tincture.
Cool and Calm
| Hops | (Humulus lupulus) | 20 mL |
| Skullcap | (Scutellaria lateriflora) | 20 mL |
| Kava kava | (Piper methysticum)† | 20 mL |
| Ashwagandha | (Withania somnifera) | 20 mL |
| Licorice | (Glycyrrhiza glabra)‡ | 20 mL |
| Total: 100 mL | ||
Protocol 3. Hot Flashes, Night Sweats, and Insomnia/Irritability
| Hops | (Humulus lupulus) | 30 mL |
| Passionflower | (Passiflora incarnata) | 30 mL |
| Bupleurum | (Bupleurum falcatum) | 15 mL |
| Ashwagandha | (Withania somnifera) | 15 mL |
| Cramp bark/black haw | (Viburnum opulus/prunifolium) | 10 mL |
| Total: 100 mL | ||
† Kava kava has been associated with hepatotoxicity in rare cases and should not be used by those with liver disease.
‡ Licorice is contraindicated for patients with renal disease, hypertension, or hyperaldosteronism (see Plant Profiles).
* Recent concerns have been raised about black cohosh and rare cases of hepatotoxicity. The validity of the concern about black cohosh has not been corroborated by the FDA. See Plant Profiles: Black Cohosh.
tea, alone or with other herbs such as chamomile and lavender to also promote relaxation, to be taken 1 to 2 hours before bed, as well as 1 to 2 cups during the day. Only one trial of unknown quality was identified looking at sage specifically for hot flashes. In this study, the efficacy of a combination of Salvia officinalis and Medicago sativa (alfalfa) was tested in 30 menopausal women with hot flashes and night sweats. Symptoms completely disappeared in 20 women; of the remaining 10 women, four showed good improvement and the other six showed a reduction in symptoms. GnRH and TRH tests were performed in eight women to evaluate TSH and Prl responses before and after 3 months of therapy. The plants product induced a significant increase in Prl and TSH response to TRH. Basal levels of estradiol, LH, FSH, Prl, and TSH were unchanged. The authors concluded that the product seemed to have a slight central antidopaminergic action without side effects and is an effective agent in the treatment of menopausal symptoms. In an open study of two groups (n = 40, no control), given sage infusion (2.6 g or 4.5 g herb/day), the herb inhibited pilocarpine-induced sweating.186 Herbalists also may encourage a perimenopausal patient to keep a spray bottle of sage tea on hand to use as a cooling spritz during the day and at night just before bed. Sage essential oil, 3 to 4 drops, diluted in 2 ounces of a lavender aromatherapy spray is also effective and pleasant for a quick cool down. Sage essential oil should never be taken internally!
ADDITIONAL THERAPIES
Nutritional Considerations
In spite of popular use, vitamin E (400 IU/4 weeks) has not been shown to be significantly more effective than placebo in the reduction of hot flashes. The study has been criticized for using too low a dose, with vitamin E proponents suggesting 800 IU to be a more appropriate dose for a trial.163