Medical emergencies
Respiration
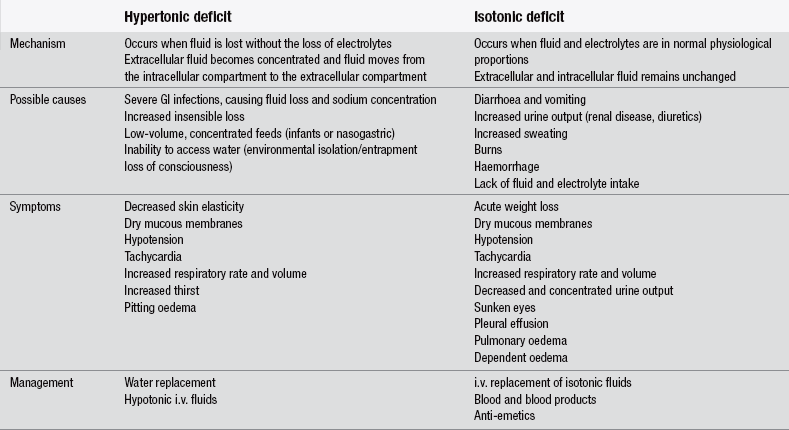
Respiration is a process that is fundamental to life itself. In the absence of external respiration, oxygen is not absorbed into the circulation and carbon dioxide is not removed from it. Such a state is clearly incompatible with life and is of an importance few would fail to acknowledge. The process of respiration is considerably more complex than external respiration alone (Fig. 28.1). Respiration also takes place at a cellular level, known as internal respiration, where oxygen plays a fundamental part in cell energy production, or metabolism, with one of the by-products of this process being carbon dioxide. Internal and external respiration cannot sustain life without the existence of an adequate transport system that enables the oxygen absorbed by external respiration to be delivered to the cells to support internal respiration, and the removal of carbon dioxide produced by internal respiration to the lungs for excretion by means of external respiration.
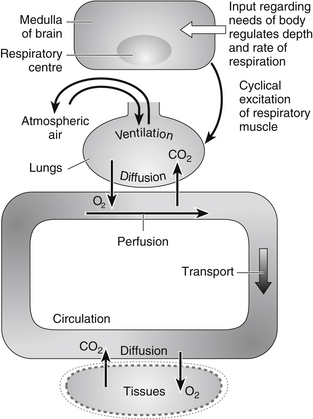
Figure 28.1 Process involved in respiration. (After Hinchliff S, Montague S, Watson R (1996) Physiology for Nursing Practice, 2nd edn. London: Bailliére Tindall.)
The mechanics of respiration
Inspiration occurs when intrathoracic pressure falls below atmospheric pressure. This fall in intrathoracic pressure is caused by an increase in the intrathoracic volume, which occurs when muscle contraction causes the rib cage to move upwards and outwards at the same time as the diaphragm is flattening. During normal inspiration it is the movement of the diaphragm that accounts for the greatest change in intrathoracic volume and not the expansion of the rib cage (Ganong 2003). The fall in intrathoracic pressure causes air to be drawn into the lungs. This generally occurs at approximately −4 to −8 mmHg.
Hypoxia
Hypoxia is regarded as being one of the leading causes of preventable death in the trauma patient, but it is often overlooked as a potential threat to life in the many patients who attend ED for reasons other than having sustained an injury. Hypoxia, or inadequate tissue oxygenation, falls broadly into four broad groups (Box 28.1):
Assessment of gas exchange
In recent years there has been an increased reliance upon pulse oximetry in respiratory assessment. In many cases, this technology is helpful in identifying hypoxia. However, pulse oximetry must be used with caution as it has the potential to mislead (Moyle 2002). Pulse oximetry gives an indication of the degree to which the available haemoglobin is saturated with oxygen. However, oximetry must only be trusted in situations where a correlation can be made to other assessments of hypoxia and it is strongly recommended to use an oximeter device that has ‘photoplethysmograph’ (PPG) capability (or ‘pleth’ as it is more commonly known). It can measure the change in the volume of arterial blood with each pulse beat and therefore can be useful in comparing to a peripheral pulse rate, and watching for signs of cardiac insufficiency (especially when ectopics occur) and, of course, prove that you have a strong enough signal and can trust the percentage reading. The relationship between oxygen saturation and the amount of oxygen within the circulation is illustrated in graphical format as the oxygen dissociation–haemoglobin dissociation curve. Assuming that the relationship on this curve is normal for a given patient, Gibson (2003) suggests that an oxygen saturation of 90 % represents a blood oxygen tension of 8 kPa. The normal range for arterial blood gases is shown in Box 28.2.
A patient with carbon monoxide poisoning may well have an anaemic hypoxia whilst still presenting what appears to be a normal oxygen saturation on the pulse oximeter. Similarly, patients with other forms of hypoxic anaemia may have normal pulse oximetry readings because the pulse oximeter is a reflection of the degree of saturation of each red blood cell and not of the total oxygen content of the blood. Again pulse oximetry must be used with caution when there is probe movement or when peripheral perfusion is low, as recorded saturation may be inaccurate (Levine & Fromm 1995).
Asthma
Asthma is a complex disorder characterized by variable and recurring symptoms, airflow obstruction, bronchial hyperresponsiveness, and an underlying inflammation (National Institutes of Health 2007). While many of the 10 % of children and 5 % of adults in the population who have asthma are asymptomatic or are well controlled with medication, approximately 1500 people per year die from asthma (Newman-Taylor 2003). Acute asthma is characterized by an acute attack of bronchospasm in which the airways become swollen, constricted and plugged with mucus. The airflow obstruction, which characteristically fluctuates markedly, causes a mismatch of alveolar ventilation and perfusion and increases the work of breathing. Being more marked during expiration it also causes air to be ‘trapped’ in the lungs.
Asthma can be broadly divided into two main types: allergic and non-allergic. Allergic asthma, as the name suggests, is triggered by allergens such as the house dust mite and others previously identified. This condition generally appears in childhood and may improve as the child reaches adolescence. Conversely, non-allergic asthma is triggered by factors such as anxiety or cold weather, first presenting in middle age. The symptoms of non-allergic asthma tend to intensify in both severity and frequency as the individual becomes older (Axford 1996).
Attendance at the ED is usually precipitated by one of two events:
1. an acute event in the individual who has episodic asthma, i.e., symptom-free between distinct acute episodes; or
2. an acute increase in the severity of symptoms in the individual who has chronic asthma, where tightness and wheezing are present most of the time, if not controlled by regular medication.
Initially, the most obvious sign of asthma may be noisy respiration in the form of a wheeze, which is generally expiratory but can also be inspiratory. One must be cautious not to make false assumptions based upon this symptom, for, as Axford (1996) notes, ‘all that wheezes is not asthma’. Wheezing is a sign of airway obstruction that may or may not be asthmatic in origin.
Assessment
 medication history; beta blockers, aspirin and non-steroidal anti-inflammatory drugs (NSAIDs) may precipitate a severe asthma attack in some patients with asthma
medication history; beta blockers, aspirin and non-steroidal anti-inflammatory drugs (NSAIDs) may precipitate a severe asthma attack in some patients with asthma
 previous admissions, especially to intensive care units (British Thoracic Society 2012)
previous admissions, especially to intensive care units (British Thoracic Society 2012)
 skin colour and appearance, such as sweating
skin colour and appearance, such as sweating
 respiratory rate, rhythm and depth
respiratory rate, rhythm and depth
 temperature (episode may have been precipitated by a chest infection)
temperature (episode may have been precipitated by a chest infection)
• percussion – resonance of the chest
 measured against predicted and actual normal for that individual
measured against predicted and actual normal for that individual
 should not be done if the patient has signs of severe or life-threatening asthma (i.e., is unable to speak a complete sentence)
should not be done if the patient has signs of severe or life-threatening asthma (i.e., is unable to speak a complete sentence)
• pulse oximetry – use with caution; remember it will not tell you the amount of carbon dioxide the patient is retaining
From the assessment it will be possible to identify those patients with severe and life-threatening asthma who need immediate intervention (Tables 28.1 and 28.2).
Table 28.1
| Adult | Child |
| Cannot complete sentences | Cannot talk or feed |
| Pulse >110 beats/min | Pulse >140 beats/min |
| Respiratory rate >25 min | Respiratory rate >50 min |
| Peak flow rate <50 % of predicted |
(After Greaves I, Hodgetts T, Porter K (2005) Emergency Care: A Textbook for Paramedics, 2nd edn. London: WB Saunders.)
Table 28.2
Features of life-threatening asthma
| Adult | Child |
| Exhaustion Cyanosis Bradycardia Hypotension Silent chest Peak flow <33 % of predicted Coma |
Reduced conscious level Agitation Cyanosis Silent chest Coma |
(After Greaves I, Hodgetts T, Porter K (2005) Emergency Care: A Textbook for Paramedics, 2nd edn. London: WB Saunders.)
Management
Position the patient to sit upright to maximize ventilation. Patients may need high concentrations of oxygen or medication nebulized by an oxygen-driven system. The drug regimen recommended by the British Thoracic Society and Scottish Intercollegiate Guidelines Network (British Thoracic Society 2012) includes nebulized or i.v. salbutamol, and oral or i.v. steroids depending upon the mechanism and severity of the attack. In life-threatening asthma, ipratropium should be added to the nebulizer and expert advice must be sought, which may include progression to non-invasive intermittent positive pressure ventilation (IPPV) with pressure support (PS) and positive end expiratory pressure (PEEP) (such as CPAP or BiPap). This can be done on the spontaneously breathing patient, via a face mask and a ventilator that is capable of delivering the non-invasive positive support safely, but is a skill that requires extra knowledge and training as there is risk of barotrauma. For children with moderate to severe exacerbation, bronchodilators can be given by inhaler using a spacer device. ED nurses must be familiar with the current British Thoracic Society and Scottish Intercollegiate Guidelines Network guidelines on asthma (British Thoracic Society 2012) and in particular the flow charts relating to the management of acute asthma in adults in ED and the management of acute asthma in children in ED. In addition to continued reassessment based upon the initial assessment, monitor the cardiac rhythm. Provide psychological care for patient and family in dealing with their stress and anxiety. The use of spacers for adult asthma patients as well as children is currently being evaluated.
It is important to differentiate asthma from hyperventilation, as the presenting symptoms of both are dramatic and can easily be confused by the inexperienced nurse (Yeh & Schwartzstein 2010). A hyperventilating patient will be tachypnoeic but not tachycardic and will usually have oxygen saturation levels of 100 %. Hyperventilation is associated with anxiety and responds quickly to rebreathing through a paper bag. Hyperventilating patients generally do not have a history of asthma.
Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease (COPD) is a collective term for a number of chronic respiratory diseases, the most common of which are chronic bronchitis and emphysema and is characterized by airflow obstruction that is not fully reversible (National Institute for Health and Clinical Excellence 2010). Airflow obstruction has profound effects on cardiac function and gas exchange with systemic consequences (Barnes & Celli 2009, MacNee 2011).
Chronic bronchitis
Assessment
• a full history, including past history as well as the history of the current episode
 signs of chronic respiratory disease, e.g., clubbing of the fingers, barrel chest
signs of chronic respiratory disease, e.g., clubbing of the fingers, barrel chest
• percussion – resonance of the chest
• pulse oximetry – use with caution; remember many of these patients retain carbon dioxide which can result in fatal respiratory acidosis, even in the presence of adequate oxygen saturation. Pulse oximetry will not provide any information about elevated levels of carbon dioxide
• arterial blood gas analysis – will be abnormal given the chronic respiratory disease and should be viewed in the light of the individual’s actual or predicted normal
• sputum sample – for microbiological examination (microscopy, culture and sensitivity)
Assessment of the patient is likely to reveal the following clinical features:
Management
Position the patient sitting upright to maximize ventilation. Oxygen should be given at a low concentration, initially no more than 28 %; increased concentrations may be necessary if improvement does not occur, but this should be based on the results of arterial blood gas analysis. Whilst on oxygen the patient must be closely monitored for signs of respiratory depression. Antibiotics, bronchodilators and steroids should be given if asthma is an element in the acute episode. Where nebulized medication is indicated the British Thoracic Society (2012) recommend that a compressed air nebulizer should be used and the patient given supplemental oxygen by nasal prongs. In addition to continued reassessment based upon the initial assessment, the cardiac rhythm should be monitored. Arterial blood gas analysis must be carried out within the first hour of admission to the ED and results used to inform on-going management of the patient. Psychological care for patient and family should be provided in dealing with their stress and anxiety. Progression to invasive, or non-invasive positive pressure ventilation may also be needed if the condition deteriorates and there is a clinical need, however the medical staff will need to take into consideration all aspects of the individual’s medical history including their normal functioning state and any advanced health directives. Discussions with family members will also be valuable in deciding the next appropriate step in resuscitation.
Pulmonary oedema
Other possible causes of pulmonary oedema
• inhalation of toxic or irritant substances
• airway burns/inhalation injury
Assessment
• a full history (past history as well as the history of the current episode)
 signs of possible underlying mechanisms, e.g., inhalation injury, substance misuse
signs of possible underlying mechanisms, e.g., inhalation injury, substance misuse
• percussion – resonance of the chest
Assessment is likely to reveal:
Management
Management of the patient is dependent upon the underlying pathology, but will include securing the airway and positioning the patient upright to maximize ventilation. Provide high-concentration oxygen through a Hudson mask with reservoir bag at a flow rate of 10–15 L/min. Diuretics may reduce the fluid load from the circulation. Morphine/diamorphine, if not contraindicated, causes venous pooling, thus reducing venous return on loading on the heart. Opiates will also help in the reduction of anxiety, but one must be vigilant for signs of respiratory depression. Vasodilators in the form of nitrates, if indicated, sublingual or i.v. infusion also cause venous pooling. Catheterization should be considered and the patient’s fluid output should be carefully monitored. A 12-lead ECG should be performed to monitor any cardiac changes. Progression to non-invasive IPPV with PS and PEEP (such as CPAP or BiPap). This can be done on the spontaneously breathing patient, via a face mask and a ventilator that is capable of delivering the non-invasive positive support safely, but is a skill that requires extra knowledge and training as there is a risk of barotrauma. In addition to continued reassessment based upon the initial assessment, monitor the cardiac rhythm and raise the back of the trolley to sit the patient up and support with pillows if necessary (Wyatt et al. 2012). Psychological care should be provided for patient and family in dealing with their stress and anxiety.
Pulmonary embolism
Venous thromboembolism (VTE) is a common cause of death in Europe. The total estimated number of VTE-related deaths for 2004 across six EU countries (UK, France, Germany, Italy, Spain and Sweden) was 370 012. Of these deaths, 7 % (26 473) were expected to have resulted from diagnosed (and presumably treated) VTE, 34 % (126 145) from sudden fatal pulmonary embolism (PE), and 59 % (217 394) from PE-related deaths following undiagnosed (untreated) VTE (Cohen et al. 2007). Pulmonary embolism is a common cause of respiratory-related death in the UK, with an estimated 60 000 deaths each year (Cohen et al. 2007). It is a commonly associated complication of deep vein thrombosis (DVT), where a fragment detaches from the thrombus to form an embolus (Fig. 28.2). The embolus flows through the circulation until it wedges in narrow branches of the arterial system, classically branches of the pulmonary artery. The pulmonary circulation becomes obstructed, which consequently reduces the efficacy of gas exchange and ventilation−perfusion mismatch occurs.
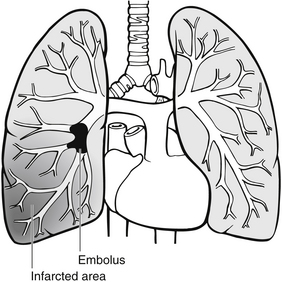
Figure 28.2 Pulmonary embolism.
Predisposition to pulmonary embolism, generally speaking, is determined by a predisposition to DVT:
Emboli may arise from other mechanisms such as air, fat or amniotic fluid entering the circulatory system, but these are less common. Symptoms are related to the size of the area of lung affected, the rate of onset and the severity of the symptoms being determined by the size and number of emboli:
• small emboli – these wedge in smaller vessels, close to the alveolar–capillary interface, and affect only a small area of lung
• medium emboli – these wedge in the larger branches of the pulmonary artery some distance from the alveolar–capillary interface; they affect a larger area of lung than do smaller emboli and result in a greater ventilation–perfusion mismatch
• large emboli – these wedge in the largest branches of the pulmonary artery, furthest away from the alveolar–capillary interface; they affect very large areas of the lung and result in a massive ventilation–perfusion mismatch.
Assessment
• a full history, considering predisposition to and evidence of DVT, as well as the history of the current episode
• percussion – resonance of the chest
Table 28.3 outlines the features of emboli of different sizes. An ECG may reveal an S wave in lead I, a Q wave in lead II and an inverted T wave in lead III. The ECG may also be useful in excluding other diagnoses such as myocardial infarction and pericardial disease.
Table 28.3
| Small emboli | Medium emboli | Large emboli |
| Slow onset Mild to moderate dyspnoea Fatigue |
Rapid onset Pleuritic chest pain Dyspnoea Haemoptysis |
Sudden onset Dyspnoea Chest pain Haemoptysis Tachycardia Compromised circulation Hypotension Cyanosis Reduced level of consciousness Unconsciousness |
Management
Position the patient sitting upright to maximize ventilation. Administer high-concentration oxygen using a Hudson mask with reservoir bag at a flow rate of 10–15 L/min. Bloods should be taken for clotting screen. Anticoagulants, such as heparin, are often the only form of treatment given for massive pulmonary embolism. A thrombolytic, such as alteplase, may be indicated primarily in patients who are haemodynamically unstable (British Thoracic Society 2003). Silent pulmonary embolisms have also been found to be present in 1665 of 5233 patients (32 %) with deep venous thrombosis so routine screening may be advantageous (Stein et al. 2010).
Anaphylaxis
Anaphylaxis is an acute, life-threatening systemic reaction with varied mechanisms, clinical presentations, and severity that results from the sudden systemic release of mediators from mast cells and basophils. The more rapidly anaphylaxis develops, the more likely the reaction is to be severe and potentially life-threatening. The prevalence of anaphylaxis is increasing and the number of cases of fatal anaphylaxis appears to be rising (Nasser 2012). Prompt recognition of signs and symptoms of anaphylaxis is crucial (Lieberman et al. 2010). Symptoms will usually occur rapidly within minutes of exposure to the causative allergen, especially if given parenterally. Repeated administration of parenteral or oral therapeutic agents may also precipitate an anaphylactic reaction.
Commonly cited riggers include:
Clinical features
The clinical features of anaphylactic shock may occur singly or in combination and may include respiratory distress, cyanosis, bronchospasm, laryngeal obstruction, circulatory collapse, hypotension, tachycardia, generalized erythema, urticaria, nausea, vomiting, abdominal pain and diarrhoea. Generally, the faster the onset of symptoms, the more life-threatening is the reaction.
Near drowning
There are about 700 drowning deaths in the UK each year and many times that number of near drowning (Joint Royal Colleges Ambulance Liaison Committee 2006). Worldwide, over 175 000 children under 20 years of age died from drowning in 2004. For each fatal event it is estimated that there are 1–4 non-fatal submersions (Taneja et al. 2008).
Near drowning following submersion in water results from one of two main mechanisms: ‘dry’ drowning and ‘wet’ drowning. Dry drowning occurs in 10–20 % of cases following immersion in cold water, where the cold water causes intense and persistent laryngospasm and vagal stimulation leading to asphyxiation, hypoxia and cardiac arrest. Little or no water enters the lower airways or lungs and death is secondary to airway obstruction rather than pulmonary oedema (Morris 2003). More commonly, drowning and near drowning occur as a result of wet drowning. After a period of breath-holding following immersion, the individual is forced to inhale by reflex mechanism. Water is aspirated into the lungs along with the large volumes of water which have been swallowed. This causes pulmonary vasoconstriction and hypertension with ventilation/perfusion mismatch, aggravated by surfactant destruction and washout and atelectasis. Consequently, the individual rapidly becomes hypoxic, which leads to unconsciousness and cardiac arrest (Wyatt et al. 2012).
Near drowning is often associated with other factors which complicate the individual’s condition. In adults, as much as 25 % of cases have been documented as being associated with alcohol use (Mills et al. 1995). Hypothermia is common in UK waters. This is inevitable when the water is below 10°C as body heat is lost despite the individual actively exercising (Greaves et al. 2005). Near drowning is frequently associated with head and neck injury, when individuals dive into shallow water or water that contains submerged objects.
Occasionally, near-drowning victims can be asymptomatic; however, most present with mild dyspnoea, a deathlike appearance with blue or grey colouring, apnoea or tachypnoea, hypotension, heart rate as slow as 4 to 5 beats per minute or pulselessness, cold skin, dilated pupils known as fish eyes, hypothermia and vomiting (Morris 2003). Significant neurological impairment occurs in up to 25 % of near-drowning patients. Neurological injury results from hypoxia and can lead to cerebral oedema and brain stem herniation. Approximately 20 % of comatose patients recover completely. Secondary drowning, which is a deterioration in a previously apparently well patient following successful resuscitation after submersion, may occur in 5–10 % of initial survivors (Wyatt et al. 2012). Hypothermia is an important clinical feature in determining outcome as it decreases the metabolic demands of the body, and severe cerebral hypoxia may be prevented or delayed. Acidosis is a common finding in near-drowning patients. Metabolic acidosis is primarily due to tissue hypoxia, but a respiratory component may be present following aspiration. Hypoxia and acidosis act as myocardial depressants and precipitate circulatory collapse.
Assessment
 signs of possible underlying factors; head and neck trauma, alcohol use
signs of possible underlying factors; head and neck trauma, alcohol use
• percussion – resonance of the chest
The presentation of the individual following near drowning may be diverse, but is likely to include at least some of the following:
Symptoms may be delayed. Apparently well patients must be observed and reviewed over the subsequent 48 hours due to the risk of secondary drowning.
Management
• airway management with cervical spine control
• high-concentration oxygen, with intermittent positive pressure ventilation if indicated
• rewarming if indicated (see hypothermia)
• continued reassessment based upon the initial assessment
• psychological care for the patient and family in dealing with their stress and anxiety.
Good prognostic factors include patients who are alert on admission, hypothermia, older children adults, brief submersion time, and those who receive rapid on-scene basic life support and respond to initial resuscitation measures (Wyatt et al. 2012).
Carbon monoxide poisoning
Carbon monoxide poisoning is the most common cause of poisoning in the UK, and is thought to cause approximately 50 deaths per year. Carbon monoxide is a colourless, odourless, tasteless gas produced by incomplete combustion of organic material. Poisoning is usually associated with inhalation of smoke from fires in confined spaces, engine exhausts and faulty heating systems. Because its earliest symptoms are vague and mimic a viral illness, carbon monoxide has been coined ‘the great masquerader’ (Sivilotti & Abu-Laban 2012). It is often referred to as the silent killer as victims of accidental exposure often have no idea they are being poisoned, even when they develop severe symptoms. Consequently, victims are likely to remain in a life-threatening environment without realizing the dangers. Carbon monoxide combines more readily with haemoglobin than oxygen does – its affinity is more than 200 times that of oxygen. Once combined with carbon monoxide, haemoglobin is unable to bind with oxygen, resulting in a fall in PO2 and an anaemic hypoxia.
Assessment
 airway – soot, carbonaceous sputum as evidence of an inhalation injury
airway – soot, carbonaceous sputum as evidence of an inhalation injury
 skin colour – may look pink or flushed in the later stages (cherry red appearance may not be evident)
skin colour – may look pink or flushed in the later stages (cherry red appearance may not be evident)
• pulse oximetry – can be extremely misleading, giving high readings even though the patient is hypoxic
Presentation will depend upon the percentage of carboxyhaemoglobin present (Table 28.4).
Table 28.4
Presentation of carbon monoxide poisoning
| Carboxyhaemoglobin | Symptoms |
| <10 % | No symptoms |
| 10–20 % | Headache Nausea Vomiting Loss of manual dexterity |
| 21–40 % | Confusion Lethargy ST depression on ECG Apathy – loss of interest in leaving dangerous environment, and therefore may be fatal |
| 41–60 % | Ataxia Convulsions Apnoea Coma |
| >60 % | Usually fatal |
Management
A carboxyhaemoglobin level greater than 3 % in non-smokers or greater than 10 % in smokers confirms exposure to carbon monoxide, but the level does not correlate with the presence or absence of initial symptoms (Weaver 2009). The patient should be given high-concentration oxygen, with intermittent positive pressure ventilation if indicated. In the presence of 100 % oxygen there is a 50 % reduction of carboxyhaemoglobin in the first 20 minutes. Consider hyperbaric oxygen, which forces oxygen onto the haemoglobin and reduces the half-life of carbon monoxide as well as decreasing intercranial pressure and cerebral oedema. The indications for hyperbaric oxygen (Axford 1996) are:
Renal disorders
Maintenance of blood pressure
• acts directly on arterioles to cause vasoconstriction
• stimulates the circulation centre in the central nervous system resulting in vasoconstriction
• stimulates the thirst mechanism in the hypothalamus
• influences renal blood flow and the glomerular filtration rate by renal vasoconstriction
• stimulates the adrenal cortex to secrete aldosterone, which increases sodium reabsorption by the kidney and so causes water retention.
Excretion of by-products of metabolism
Assessment of the renal system
The renal system gives an insight into many physiological processes and should not be underestimated when making a patient assessment. Likewise, an assessment of the renal system should not be restricted to those patients with renal conditions. The assessment of these processes and of renal function is via the urine output in terms of volume, frequency and content. This may be achieved by accurate fluid balance measurement and recording at intervals appropriate to the patient’s condition. Routine urine testing using reagent strips offers a wealth of information, as does a visual inspection of the urine, which is frequently undervalued in assessment.
Urinary tract infection
Of the many conditions which are of renal or urinary tract origin, few are seen in the ED. Where the patient does attend with an underlying renal or urinary tract pathology, it is generally because of pain rather than any other symptom, the most common conditions being urinary tract infection (UTI) and renal colic. Escherichia coli is associated with 80–90 % of UTIs (Ejernæs 2011). Other organism groups that cause UTI include Proteus, Pseudomonas, Streptococcus, Staphylococcus epidermidis and Klebsiella (Cetti & Venn 2012). Following inoculation, organisms rapidly multiply in the ideal culture material of the urine. The individual will generally present at the ED complaining of pain on micturition. Recurrent UTIs (RUTIs) are reported in 25 % of women within six months of an acute UTI episode and pose a major problem (Ejernæs 2011).
Renal colic
Renal colic is the most common presentation of renal calculi. It occurs most frequently between 20 and 50 years of age with a male:female ratio of 3:1. About 50 % of patients have a single episode but the remaining 50 % have recurrences within 5 years (Nicholson 2004). Renal calculi are predominantly calcium in origin, although they may be calcium/ammonium phosphate, urate or cysteine. The calculi form in the kidney when the urine is saturated with the given solute and the kidney is unable to excrete it. The solute, in its crystalline form, deposits in the kidney causing pain. Pain is at its most intense when the calculi pass through the urinary tract.
Assessment
• a full history and pain assessment
 urine – colour, opacity, odour, laboratory stick test; urine should be filtered through filter paper to identify evidence of grit from the calculi
urine – colour, opacity, odour, laboratory stick test; urine should be filtered through filter paper to identify evidence of grit from the calculi
• midstream specimen of urine – for microscopy, culture and sensitivity.
The main feature identified by the assessment is likely to be pain; however, other features may be present:
Management
• Increase fluid intake – orally or i.v.
• Patient education – advise patient to increase fluid intake especially at night when urine normally concentrates.
NSAIDs provide excellent analgesia in renal colic, but should be used with care in patients at risk of renal impairment, cardiac failure and gastric ulceration (Davenport & Waine 2010).
Dehydration – fluid volume deficit
The mechanisms leading to dehydration are many and varied. It is likely that the patient will attend the ED with a condition resulting in dehydration rather than with dehydration perse. It is important to consider the processes involved in the underlying illness to identify the potential for dehydration. There are two main types of dehydration, depending on the type of fluid deficit, i.e., hypertonic, isotonic (Table 28.5).
In an effort to correct dehydration, patients may inadvertently overhydrate, leading to subsequent physiological disturbance. This is covered in Table 28.6.
Table 28.6
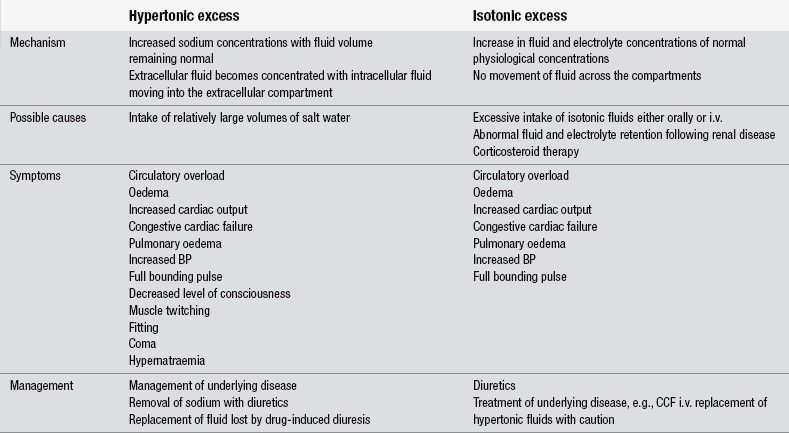
(After Paradiso C (1995) Fluids and Electrolytes. Philadelphia: JB Lippincott.)
Thermoregulation
The control of body temperature takes place in the hypothalamus in response to changes in core temperature, detected by thermoreceptors in the hypothalamus, skin and spinal cord. When the body temperature rises, the hypothalamus responds by increasing sweating, respiration and blood flow to the skin, via the autonomic nervous system. Normal human body temperature displays a circadian rhythm, ranging from 35.8°C (96.4°F) in the predawn hours to 37.3°C (99.1°F) in the late afternoon (Bickley & Szilagyi 2009) and body temperatures that exceed the norm of 37.0°C (98.6°F) are often observed in healthy people. Abnormal elevation of temperature (pyrexia) is categorized as hyperthermia or fever. Hyperthermia is the result of a failure of thermal control mechanisms. In fever, the thermal control mechanisms are intact.
Heat illness
• high humidity (humidity reduces effective evaporation through sweating)
• clothing which reduces the skin surface area available for evaporation.
Assessment
• a full history, including past history as well as the history of the current episode
From the assessment, two conditions may be identified. These are heat exhaustion and heat stroke.
Management
• place in a cool environment, with gentle air flow
• remove clothing preventing heat loss
• replace isotonic fluid – orally if conscious and oriented and not vomiting; otherwise by the intravenous route
• tepid sponging and the use of a fan is not advocated as this causes peripheral vasoconstriction, pooling the blood to the core with a consequential rise in core temperature.
• secure the airway if indicated
• administer high-concentration oxygen and assisted ventilation if required
• carry out active cooling – consider immersion in cool water, taking into account potential airway and breathing problems. Spraying the skin with cool water in the presence of air flow may be a more practical intervention to reduce body temperature through evaporation
• carry out intravenous fluid replacement and correction of electrolyte imbalance.
Nervous system
Headaches
Headaches of non-traumatic origin account for approximately 0.5 % of ED attendances and 10–15 % have serious underlying pathology (Wyatt et al. 2012). Headaches with no other neurological signs fall broadly into three main groups: tension, migraine and cluster. In order to differentiate between the three and to identify any serious underlying conditions, a full assessment is essential, with great emphasis being placed upon the history:
• a full history, including past history as well as the history of the current episode
 what exacerbates or relieves pain
what exacerbates or relieves pain
 other associated neurological symptoms
other associated neurological symptoms
 health history – has the individual experienced these headaches previously?
health history – has the individual experienced these headaches previously?
 current medication – especially over-the-counter medications taken for symptom relief, vasodilators or caffeine-containing drugs
current medication – especially over-the-counter medications taken for symptom relief, vasodilators or caffeine-containing drugs
Subarachnoid haemorrhage
Spontaneous subarachnoid haemorrhage (SAH) generally results from the rupture of an intercranial aneurysm on a major artery in the circle of Willis. The occurrence of SAH is 3 % of all strokes and one third of haemorrhagic strokes and has a mortality ranging between 32–67 % (Taqi & Torbey 2012). The patient generally presents with sudden onset of an intense headache which may initially be frontal or occipital, but eventually becomes generalized. The blood in the subarachnoid space leads to irritation and neurological signs such as drowsiness, confusion, neck stiffness, photophobia, convulsions and loss of consciousness. Depending upon the location of the bleed, the individual may have aphasia, hemiparesis or hemiplegia.
Management is focused on supporting the vital functions in terms of airway, breathing and circulation. Particular attention should be given to the monitoring of the blood pressure, as a raised blood pressure may increase the degree of bleeding. Preventing and managing the secondary insults on the brain are also important, e.g., hypo-/hyperglycaemia, seizures, hypo-/hyperthermia, hypoxia, irregular respiratory patterns.
Cerebrovascular accident and transient ischaemic attacks
The most frequently observed types of brain ischaemia seen in the ED are transient ischaemic attacks and ischaemic stroke. In both cases, ischaemia leads to focal loss of cerebral function. As the name suggests, the symptoms of the ischaemia are short-lived, lasting less than 24 hours, the actual ischaemia being shorter in duration than this. When symptoms last more than 24 hours, death occurs from what is thought to be a cerebral vascular event alone. A person who has had one or more transient ischaemic attacks is almost ten times more likely to have a stroke than someone of the same age and gender who has not had one. Those who have had a myocardial infarct are also at increased risk for having a stroke (Bergman et al. 2012).
More than 85 % of strokes are ischaemic in origin leading to infarction; haemorrhagic brain injuries account for the remaining cases (Wang et al. 2009). These mainly result from either a primary intercerebral bleed or a subarachnoid haemorrhage. A quick way to triage stroke is to use the FAST acronym, based on the Cincinnati Stroke Scale that was developed to raise public recognition of stroke. FAST stands for Face, Arm, Speech, and Time, and time is brain is a key concept in the management of those who have had a stroke (Arto et al. 2012, Bergman et al. 2012).
Assessment
The modes of presentation of both transient ischaemia and stroke differ little other than in the duration of the symptoms. Symptoms vary depending upon the area of brain affected:
Management
As with subarachnoid haemorrhage, management is focused upon supporting the vital functions in terms of airway, breathing and circulation. Particular attention should be given to monitoring of the blood pressure, as a raised blood pressure may increase the degree of bleeding. Patients should be screened for intravenous thrombolytic drugs such as Alteplase/recombinant tissue plasminogen activator which should be given within 3–4.5 hours after acute ischaemic stroke. Exclusion criteria include >80 years of age, taking oral anticoagulant drugs, and/or combined history of diabetes and stroke (ECASS III 2008, Bergman et al. 2012).
Epilepsy
Epilepsy in itself is not a medical emergency; however, there are a number of mechanisms that may make it so, the most common being injury sustained during a convulsion and several seizures following on from the previous in quick succession – status epilepticus. This is more common at the extremes of age, with over 50 % of all cases occurring in children and a disproportionately high incidence in those over 60 years of age. It also occurs most commonly in patients with no previous history of epilepsy (Wilkes 2004).
Normally when convulsions cease, the individual is drowsy, confused and may have a headache. The main danger for the individual in such circumstances is from injury when falling to the ground or colliding with objects or from having objects forced into the mouth by unwitting ‘helpers’. It is important to establish if the fit is related to epilepsy or if it is a symptom of some other condition such as head injury or subarachnoid haemorrhage. Status epilepticus, where one seizure ends and another immediately commences, is a potentially life-threatening condition requiring immediate intervention to break the cycle. Status epilepticus has a significant mortality (2–4 %) and morbidity (10 %) with irreversible neurological damage (Appleton 1994). The mainstay of management is securing the airway, administration of oxygen, assessment of respiratory and cardiac function and the administration of either lorazepam or diazepam intravenously (Scottish Intercollegiate Guidelines Network 2003).
Glucose regulation
Diabetes mellitus
Three main conditions occur in diabetes which may present a threat to life: hypoglycaemia, diabetic ketoacidosis (DKA) and hyperglycaemic hyperosmolar state (HHS) also known as hyperosmolar non-ketotic state (HONK). HHS replaces the older terms, ‘HONK coma’ and ‘HONK’, because mild to moderate ketosis is commonly present in this state and alterations of sensoria may be present without coma (English & Williams 2004).
Assessment
Hypoglycaemia
Symptoms and signs of hypoglycaemia include:
• blood glucose of less than 3.0 mmol/L
• rapid in onset in IDDM, where synthetic insulin intake oversupplies glucose intake or where there is an increased glucose demand
Early signs:
Later signs:
All individuals with a reduced level of consciousness, especially if associated with alcohol, should routinely have blood glucose measured by use of a reagent lab stick.
• glucagon by injection – converted into glucose by the body; benefits are temporary and so it must be followed up with oral long-acting sugar when consciousness returns and the individual is able to protect his own airway
• 50 % glucose intravenous infusion – must be into a large vein as hypertonic fluids are highly irritant.
Haematology
Collectively these cells form the basis of the body’s defence system. Platelet formation also takes place in the bone marrow; 60–75 % of platelets stay in the circulation and the bulk of the remainder are found in the spleen (Waugh & Grant 2010). Platelets are predominantly involved in clotting processes.
Sickle cell disease
While 70 % of those with sickle cell disease are of African ethnic origin, it is also seen in Mediterranean, Middle Eastern and Indian communities (Rees et al 2010). Sickle cell disease is thought to have evolved over a considerable time in malaria-endemic areas, as a defence against malaria. The evolutionary changes have resulted in a change in the structure of the haemoglobin, which in sickle cell disease can lead to a change in the shape of the red blood cell to form the classically sickle-shaped blood cell, and these changes are at a genetic level, accounting for the hereditary element of sickle cell disease.
Assessment
Management
This includes rapid and adequate analgesia, usually requiring opiate analgesics. These should not be delayed by undertaking a detailed examination. Intravenous fluids are particularly important for patients with renal involvement and the aim should be to generate urine output in excess of 100 mL/h (McLaren 2004). Seek specialist advice from the haematologist. As well as pain relief, ensure the patient is warm and able to rest. Oxygen therapy should be given if indicated; however, oxygen will be of little or no benefit to most individuals in sickle cell crisis as the problem is associated with obstructed blood flow and not oxygenation of that blood. Sickle cell disease is associated with an increased risk of cerebral infarction (Verduzco & Nathan 2009). It is highly recommended that each department has a policy for managing individuals with sickle cell disease and information on where to access specialist advice and support locally.
Neutropaenic pyrexia
One of the major causes of fevers in cancer patients is infection, especially in relation to neutropaenia. Fever in the neutropaenic cancer patient represents an absolute emergency, since undetected and untreated infections in neutropaenic patients can progress quickly (Bosnjak 2004). Fever in a neutropaenic cancer patient may signify a life-threatening infection and in a cancer patient should be considered indicative of infection until proven otherwise and appropriate assessments should be instituted immediately.
Management
All neutropaenic cancer patients should be considered to be at risk for infection and, once febrile, should be treated immediately with antimicrobials, without waiting for clinical and/or microbiological documentation of infection (Bosnjak 2004): this is known as empirical antibiotic therapy. Empirical antibiotic treatment of all neutropaenic patients at the onset of fever continues to be controversial. However, it also remains the key aspect of infection management. The specific composition of the empirical antibiotic regimen also remains subject to change, which is due to the changing pattern of pathogens, the emergence of antibiotic-resistant organisms, the appearance of the new clinical entities, the availability of new drugs and the improved models for patient’s infection risk categorization (Bosnjak 2004). While there is a general consensus that empirical therapy is appropriate, there is no consensus as to which antibiotics or combinations of antibiotics should be used.
Conclusion
In the modern ED, a ‘medical emergency’ can range from a full cardiac arrest to a GP referral patient with an exacerbation of a chronic condition. This chapter has considered the more common medical conditions which may result in ED attendances. The ED nurse plays an important role in identifying and alleviating symptoms and conditions which can be debilitating for the patient. While many medical conditions are chronic, the exacerbation of these conditions may require the patient to attend ED for subsequent admission. The provision of supportive care can alleviate the suffering and disruption caused by these medical emergencies.
References
Appleton, R. The Nursing Times Guide to Epilepsy. Basingstoke: Macmillan; 1994.
Arto, V., Putaala, J., Strbian, D., et al. Stroke mimics and intravenous thrombolysis. Annals of Emergency Medicine. 2012;59(1):27–32.
Axford, J. Medicine. Oxford: Blackwell Science; 1996.
Barnes, P.J., Celli, B.R. Systemic manifestations and comorbidities of COPD. European Respiratory Journal. 2009;33(5):1165–1185.
Bergman, K., Kindler, D., Pfau, L. Assessment of stroke: A review for ED nurses. Journal of Emergency Nursing. 2012;38(1):36–42.
Bickley, L.S., Szilagyi, P.G. Bates’ Pocket Guide to Physical Examination and History Taking, sixth ed. Philadelphia: Lippincott, Williams & Wilkins; 2009.
Bosnjak, S. Treatment of a febrile neutropenic patient. Archives of Oncology. 2004;12(3):179–181.
British Thoracic Society. British guidelines on the management of suspected acute pulmonary embolism. Thorax. 2003;58:470–484.
British Thoracic Society. The British Guideline on the Management of Asthma: A National Clinical Guideline. Edinburgh: BTS & SIGN; 2012.
Cetti, R., Venn, S. The management of acute urinary tract infection. In Dawson C., Nethercliffe J., eds.: ABC of Urology, third ed, London: John Wiley & Sons, 2012.
Cohen, A.T., Agnelli, G., Anderson, F.A., et al. Venous thromboembolism (VTE) in Europe: The number of events and associated morbidity and mortality. Thrombosis and Haemostasis. 2007;98:756–764.
Davenport, K., Waine, E. The role of non-steroidal anti-inflammatory drugs in renal colic. Pharmaceuticals. 2010;3:1304–1310.
ECASS, III. Thrombolysis with Alteplase 3 to 4.5 hours after acute ischaemic stroke. New England Journal of Medicine. 2008;359:1317–1329.
Ejernæs, K. Bacterial characteristics of importance for recurrent urinary tract infections caused by Escherichia coli. Danish Medical Bulletin. 2011;58(4):B4187.
English, P., Williams, G. Hyperglycaemic crises and lactic acidosis in diabetes mellitus. Postgraduate Medical Journal. 2004;80:253–261.
Ganong, W.F. Review of Medical Physiology, twenty-first ed. Connecticut: Appleton & Lange; 2003.
Gibson, G.J. Respiratory function tests. In: Warrel D.A., Cox T.M., Firth J.D., eds. Oxford Textbook of Medicine. Oxford: Oxford University Press, 2003.
Greaves, I., Hodgetts, T., Porter, K. Emergency Care: A Textbook for Paramedics, second ed. London: WB Saunders; 2005.
Hinchliff, S., Montague, S., Watson, R. Physiology for Nursing Practice, second ed. London: Bailliere Tindall; 1996.
Joint Royal Colleges Ambulance Liaison Committee. The Immersion Incident. Warwick: JRCALC; 2006.
Lieberman, P., Nicklas, R.A., Oppenheimer, J., et al. The diagnosis and management of anaphylaxis practice parameter: 2010 update. The Journal of Allergy and Clinical Immunology. 2010;126(3):477–480.
Levine, R.L., Fromm, R.E. Critical Care Monitoring: From Pre-hospital to the ICU. St Louis: Mosby; 1995.
MacNee, W. Pathology and pathogenesis. In Currie G.P., ed.: ABC of COPD, second ed, Oxford: Wiley-Blackwell, 2011.
McLaren, H. Anaemia. In Cameron P., Jelinek G., Kelly A.M., Murray L., Brown A.F.T., Heyworth J., eds.: Textbook of Emergency Medicine, second ed, Edinburgh: Churchill Livingstone, 2004.
Mills, K., Morton, R., Page, G. Colour Atlas and Text of Emergencies, second ed. London: Mosby-Wolfe; 1995.
Morris, J. Environmental emergencies. In Newberry L., ed.: Sheehy’s Emergency Nursing: Principles and Practice, fifth ed, St Louis: Mosby, 2003.
Moyle, J. Pulse Oximetry, second ed. London: British Medical Journal Publishing Group; 2002.
Nasser, S. Anaphylaxis: current state of knowledge for the modern physician. Postgraduate Medical Journal. 2012;88:458–464.
National Institute for Health and Clinical Excellence. Chronic Obstructive Pulmonary Disease: Management of Chronic Obstructive Pulmonary Disease in Adults in Primary and Secondary Care. London: NICE; 2010.
National Institutes of Health. Guidelines for the Diagnosis and Management of Asthma: National Asthma Education and Prevention Program Expert Panel Report 3. Bethseda, MD: NIH; 2007.
Newman Taylor, A.J. Endocrine disorders. In: Warrel D.A., Cox T.M., Firth J.D., eds. Oxford Textbook of Medicine. Oxford: Oxford University Press, 2003.
Nicholson, P. Renal colic. In Cameron P., Jelinek G., Kelly A.M., Murray L., Brown A.F.T., Heyworth J., eds.: Textbook of Emergency Medicine, second ed, Edinburgh: Churchill Livingstone, 2004.
Paradiso, C. Fluids and Electrolytes. Philadelphia: JB Lippincott; 1995.
Rees, D.C., Williams, T.N., Gladwin, M.T. Sickle-cell disease. The Lancet. 2010;376(9757):2018–2031.
Scottish Intercollegiate Guidelines Network. Diagnosis and Management of Epilepsy in Adults: A National Clinical Guideline. Edinburgh: Scottish Intercollegiate Guidelines Network; 2003.
Sivilotti, M.L.A., Abu-Laban, R.B. Inhaling smoke causes smoke inhalation: put that in your hookah pipe!. Canadian Journal of Emergency Medicine. 2012;14(1):3.
Stein, P.D., Matta, F., Muzammil, H.M., et al. Silent pulmonary embolism in patients with deep vein thrombosis: A systematic review. The American Journal of Medicine. 2010;123(5):426–431.
Taqi, M.A., Torbey, M.T. Subarachnoid haemorrhage. In: Manno E., ed. Emergency Management in Neurocritical Care. London: John Wiley & Sons, 2012.
Taneja, G., Van Beeck, E., Brenner, R. Drowning. In: Peden M., Oyebgite K., Ozanne-Smith J., et al, eds. World Report on Child Injury Prevention. Geneva: World Health Organization, 2008.
Verduzco, L.A., Nathan, D.G. Sickle cell disease and stroke. Blood. 2009;114:5117–5125.
Waugh, A., Grant, A. Ross and Wilson’s Anatomy and Physiology in Health and Illness, eleventh ed. Edinburgh: Churchill Livingstone; 2010.
Wang, C.X., Stroink, A., Casto, J.M., et al. Hyperthermia exacerbates ischaemic brain injury. International Journal of Stroke. 2009;4:274–284.
Weaver, L.K. Carbon monoxide poisoning. New England Journal of Medicine. 2009;360:1217–1225.
Wilkes, G.J. Seizures. In Cameron P., Jelinek G., Kelly A.M., Murray L., Brown A.F.T., Heyworth J., eds.: Textbook of Emergency Medicine, second ed, Edinburgh: Churchill Livingstone, 2004.
Wyatt, J.P., Illingworth, R.N., Graham, C.A., et al. Oxford Handbook of Accident & Emergency Medicine, fourth ed. Oxford: Oxford University Press; 2012.
Yeh, S.Y., Schwartzstein, R. Asthma: Pathophysiology and diagnosis. In: Harver A., Kotses H., eds. Asthma, Health and Society: A Public Health Perspective. New York: Springer, 2010.