Chapter 1 Medial and Anterior Knee Anatomy
MEDIAL ANATOMY OF THE KNEE
The medial anatomy of the knee consists of several layers of structures that work together to provide stability and function. Authors have used a variety of anatomic terms and descriptions that, unfortunately, have created ambiguity and confusion regarding this area of the knee. Two anatomic classifications or descriptions have been proposed to aid in the understanding of the relationships of the medial knee structures. These include a layered approach,46 which describes the qualitative relationship of each medial structure, and a more quantitative description,28 which details the exact attachment site and origin of each structure. In this chapter, both approaches are presented; however, emphasis is on the precise anatomic relationships that provide a more thorough understanding of the structures compared with the layered approach.
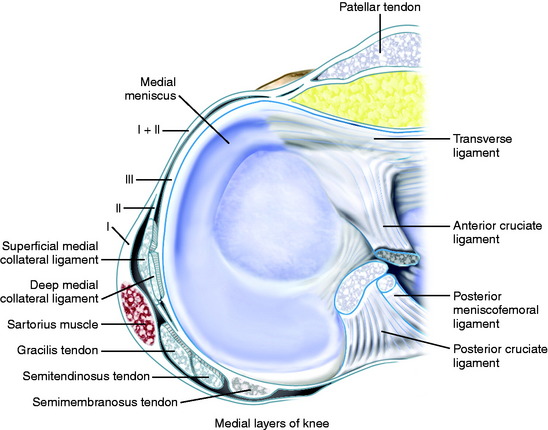
Medial Layers of the Knee
The three-layer description of the medial anatomy of the knee was proposed by Warren and Marshall.46 In this approach, layer 1 consists of the deep fascia or crural fascia; layer 2 includes the superficial medial collateral ligament (SMCL), medial retinaculum, and the medial patellofemoral ligament (MPFL); and layer 3 is composed of the deep medial collateral ligament (DMCL) and capsule of the knee joint (Fig. 1-1). For this chapter, the term medial collateral ligament (MCL) has been selected instead of tibial collateral ligament because it represents the term most commonly used in the English literature. The medial structures identified as important in preventing lateral patellar subluxation are the MPFL and the medial patellomeniscal ligament, which inserts onto the inferior third of the patella to the anterior portion of the medial meniscus and runs adjacent to the medial fat pad. The medial parapatellar retinaculum and so-called medial patellotibial ligament (thickening of the anterior capsule inserting from the inferior aspect of the patella to the anteromedial aspect of the tibia) are retinacular tissues that have been described; however, these structures are not believed important to providing patellar stability.
The layered approach is important because the ligaments and soft tissues on the medial side of the knee are not discrete, individual structures like the SMCL, but rather, fibrous condensations within tissue planes.46 This qualitative description of anatomy assists in understanding the spatial relationships of these structures and how they function to support the knee.48 It is equally important to understand the quantitative anatomy from precise measurements of the attachments and origins of each individual structure. The complex medial anatomy of the knee has been illustrated in the past with oversimplification of the soft tissue attachments to bone and other structures, which makes it difficult to compare the origins, insertions, and courses of the many separate structures among studies.3,4,12,15,30,41,46 LaPrade and coworkers28 recently published detailed quantitative measurements that provide a better understanding of the medial knee anatomy.
Layer 1: Deep Fascia
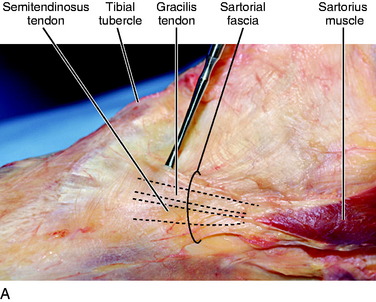
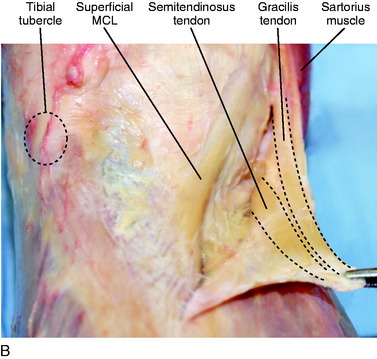
Layer 1 (see Fig. 1-1) consists of the deep fascia that extends proximally to invest the quadriceps, posteriorly to invest the two heads of the gastrocnemius and cover the popliteal fossa, and distally to involve the sartorius muscle and sartorial fascia. Anteriorly, layer 1 blends with the anterior part of layer 2, approximately 2 cm anterior to the SMCL.46 Inferiorly, the deep fascia continues as the investing fascia of the sartorius and attaches to the periosteum of the tibia. Layers 1 and 2 are always distinct at the level of the SMCL unless extensive scarring has occurred.46 The gracilis and semitendinosus tendons are discrete structures that lie between layers 1 and 2 and are easily separated from these two layers. However, according to Warren and Marshall,46 these tendons will occasionally blend with the fibers in layer 1 anteriorly before they insert onto the tibia. As depicted in Figure 1-2, dissections and clinical experience of the authors of this chapter concur in that there is a blending of layer 1 with a confluence of the semitendinosus and gracilis tendons at their common insertion onto the tibia; however, they are easily found as discrete structures more posteriorly. Thus, it is the recommendation of the authors of this chapter that when attempting to harvest the semitendinosus and gracilis tendons for an anterior cruciate ligament reconstruction, these tendons initially be identified 2 to 3 cm posterior and medial to the anterior tibial spine. This will allow for easier visualization of the tendons, which can then be traced to their insertions on the anterior tibia to allow for maximal tendon length at the time of harvest.
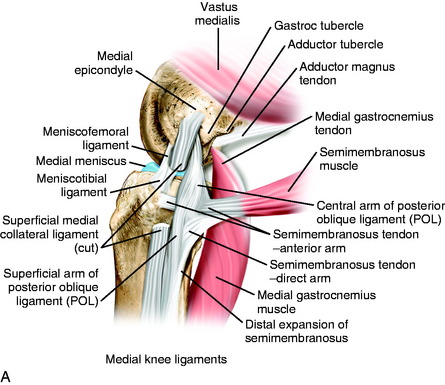
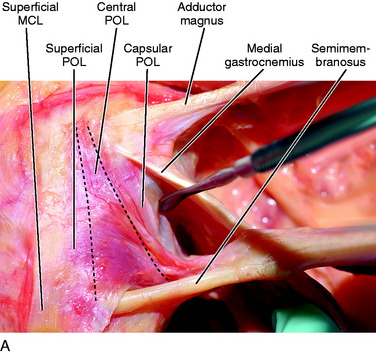
Layer 2: SMCL and Posterior Oblique Ligament
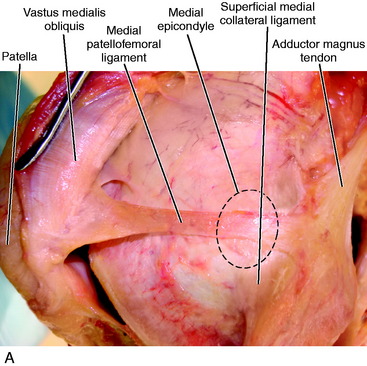
The SMCL is a well-defined structure that spans the medial joint line from the femur to tibia. According to LaPrade and coworkers,28 the SMCL does not attach directly to the medial epicondyle of the femur, but is centered in a depression 4.8 mm posterior and 3.2 mm proximal to the medial epicondyle center. Other studies have described the MCL attaching directly to the medial epicondyle of the femur.* The confusion lies in the confluence of fibers that reside in the area of the medial epicondyle that make it difficult to identify the precise attachment site of the SMCL. As shown in Figure 1-3, the authors agree with LaPrade and coworkers28 that the main fibers of the SMCL attach to an area just posterior and proximal to the medial epicondyle; but the origin of the SMCL is rather broad and, thus, there are also superficial fibrous strands attaching anterior on the medial epicondyle and posterior in a depression on the medial femoral condyle.
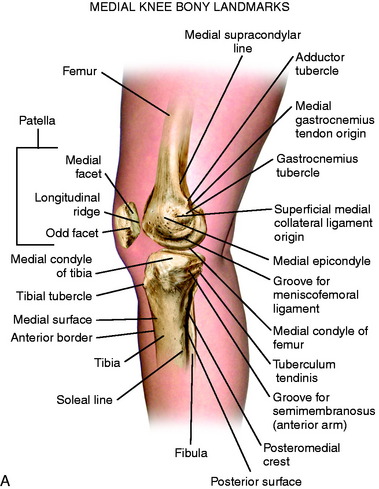
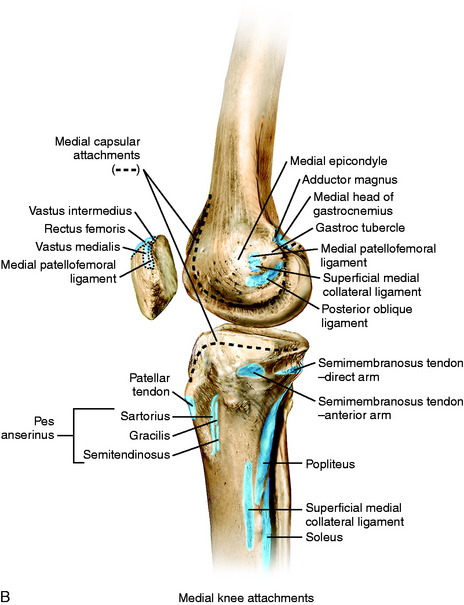
FIGURE 1-3 A, Osseous landmarks of the knee (medial view). B, Soft tissue attachments to bone (medial knee).
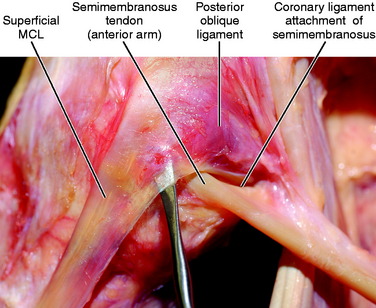
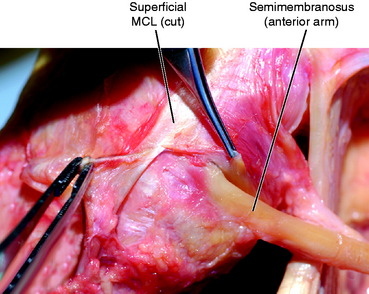
The posterior fibers of the SMCL overlying the medial joint line, both above and below the joint, change orientation from vertical to a more oblique pattern that forms a triangular structure with its apex posterior,4,30 eventually blending with the fibers of the posterior oblique ligament (POL; Fig. 1-4). LaPrade and coworkers28 described two anatomic attachment sites of the SMCL on the tibia. The first is located proximally at the medial joint line and consists mainly of soft tissue connections over the anterior arm of the semimembranosus. The second attachment site is further distal on the tibia, attaching directly to bone an average of 61.2 mm from the medial joint line. In the authors’ experience, there is a consistent attachment of the proximal portion of the SMCL to the soft tissues surrounding the anterior arm of the semimembranosus, but a discrete attachment to bone is found only distally (see Fig. 1-4).
The gracilis and semitendinosus lie between layers 1 and 2 at the knee joint. The sartorius drapes across the anterior thigh and into the medial aspect of the knee invested in the sartorial fascia in layer 1. The insertion of the sartorius, as described by Warren and Marshall,46 consists of a network of fascial fibers connecting to bone on the medial side of the tibia, but does not appear to have a distinct tendon of insertion such as the underlying gracilis and semitendinosus. However, LaPrade and coworkers28 located the gracilis and semitendinosus tendons on the deep surface of the superficial fascial layer, with each of the three tendons attaching in a linear orientation at the lateral edge of the pes anserine bursa.
In the authors’ experience, the sartorial fascia has a broad insertion onto the anteromedial border of the tibia and, with sharp dissection at its insertion, the underlying distinct tendons of the gracilis and semitendinosus are easily visualized (see Fig. 1-2). At the level of the joint, layers 1 and 2 are easily separated from each other over the SMCL. However, farther anteriorly, layer 1 blends with the anterior part of layer 2 along a vertical line 1 to 2 cm anterior to the SMCL.46
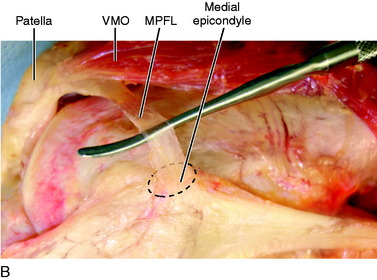
Also within layer 2 is the MPFL that courses from the medial femoral condyle to its attachment onto the medial border of the patella. This is a flat, fan-shaped structure that is larger at its patellar attachment than at its femoral origin, with a length averaging 58.3 mm (47.2–70.0 mm).38 Controversy exists regarding where the MPFL attaches at the medial femoral condyle. LaPrade and coworkers28 noted that the MPFL attaches primarily to soft tissues between the attachments of the adductor magnus tendon and the SMCL, with an attachment to bone 10.6 mm proximal and 8.8 mm posterior to the medial epicondyle. Steensen and associates,40 from a dissection of 11 knees, believed the MPFL attaches along the entire length of the anterior aspect of the medial epicondyle. Smirk and Morris38 described a variable origination of the MPFL on the femur. In dissections of 25 cadavers, the MPFL attached solely to the posterior aspect of the medial epicondyle, approximately 1 cm distal to the adductor tubercle in 44% of specimens. The adductor tubercle was included in the origin in 4%, the adductor magnus tendon in 12%, the area posterior to the adductor magnus tendon in 20%, and a combination of these in 4%. In 16% of the specimens, the MPFL attached anterior to the medial epicondyle.
In the authors’ experience, the MPFL attaches in a depression posterior to the medial epicondyle and blends with the insertion of the SMCL (Fig. 1-5). The anterior attachment of the MPFL consists of both attachments to the undersurface of the vastus medialis obliquus (VMO) and the proximal medial border of the patella. The work of Steensen and associates40 demonstrated that the VMO does not overlap the MPFL, with the exception in 3 of 11 knees in which only 5% of the width of the MPFL was deep to the VMO. However, LaPrade and coworkers28 reported that the distal border of the VMO attaches along the majority of the proximal edge of the MPFL before inserting onto the superomedial border of the patella. The midpoint of the MPFL attachment is located 41% of the length from the proximal tip of the patella along the total patellar length. The experience of the authors of this chapter is that the MPFL attaches to the proximal third of the patella, with the majority of the ligament connected to the distal portion of the VMO with fibrous bands (see Fig. 1-5).
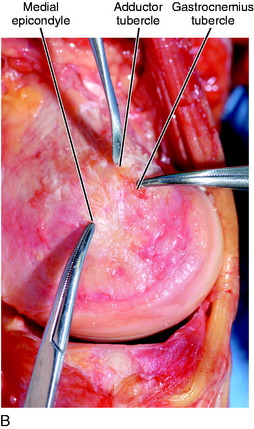
The adductor magnus and medial gastrocnemius tendons also contribute to the medial anatomy of the knee; both attach on the medial femoral condyle. Similar to the SMCL attachment, the confluence of fibers over the medial femoral condyle makes it difficult to precisely identify the exact location of each attachment (Fig. 1-6). The adductor magnus tendon is a well-defined structure attaching just superior and posterior to the medial epicondyle near the adductor tubercle. LaPrade and coworkers28 reported the adductor magnus does not attach directly to the adductor tubercle, but rather to a depression located an average of 3.0 mm posterior and 2.7 mm proximal to the adductor tubercle. The adductor magnus also has fascial attachments to the capsular portion of the POL and medial head of the gastrocnemius.
The medial gastrocnemius tendon inserts in a confluence of fibers in an area between the adductor magnus insertion and the insertion of the SMCL (Fig. 1-7A). LaPrade and coworkers28 described a gastrocnemius tubercle on the medial femoral condyle in this region; however, these authors stated that the tendon does not attach to the tubercle, but to a depression just proximal and posterior to the tubercle. In addition, fascial expansions from the lateral aspect of the medial gastrocnemius tendon form a confluence of fibers with the distal extent of the adductor magnus tendon in addition to the capsular arm of the POL (see Fig. 1-7A).
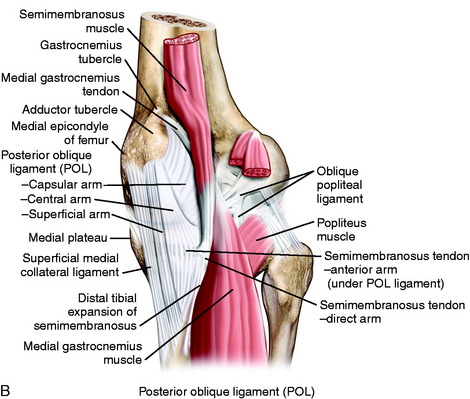
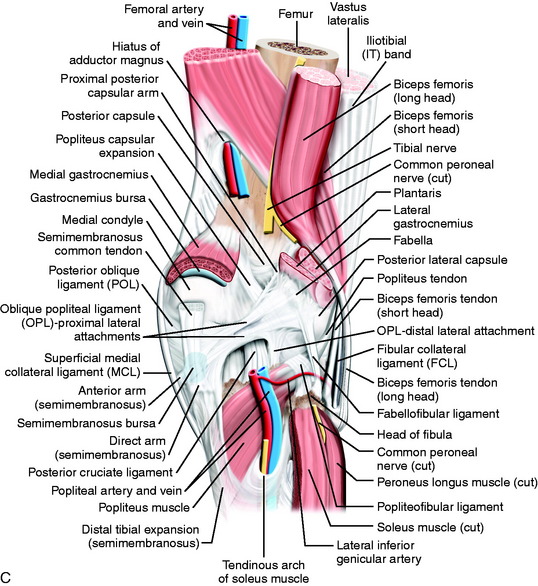
Layers 2 and 3 blend together in the posteromedial corner of the knee along with additional fibers that extend from the semimembranosus tendon and sheath that form the posteromedial capsule (see Fig. 1-7). LaPrade and coworkers28 used the term posterior oblique ligament (POL) for this same structure and described each of the three fascial attachments similar to Hughston and colleagues’ original description.21,22 The superficial arm of the POL runs parallel to both the more anterior SMCL and the more posterior distal expansion of the semimembranosus. Proximally, the superficial arm blends with the central arm; distally, it blends with the distal expansion of the semimembranosus as it attaches to the tibia.28
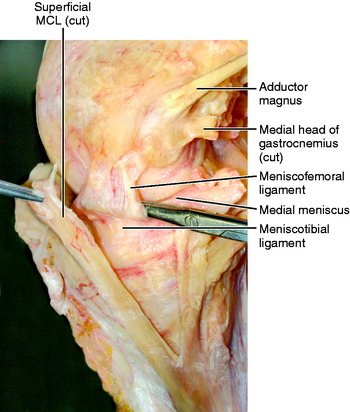
The central arm is the largest and thickest portion of the POL,28 running posterior to both the superficial arm of the POL and the SMCL. It courses from the distal portion of the semimembranosus and is a fascial reinforcement of the meniscofemoral and meniscotibial portions of the posteromedial capsule. LaPrade and coworkers28 noted that this structure has a thick attachment to the medial meniscus. As the central arm courses along the posteromedial aspect of the joint, it merges with the posterior fibers of the SMCL and can be differentiated from the SMCL by the different directions of the individual fibers. The distal attachment of the central arm is primarily to the posteromedial portion of the medial meniscus, the meniscotibial portion of the capsule, and the posteromedial tibia.28
The capsular portion of the POL is thinner than the other portions of this structure and fans out in the space between the central arm and the distal portions of the semimembranosus tendon. The capsular portion blends posteriorly with the posteromedial capsule of the knee and the medial aspect of the oblique popliteal ligament (OPL).28 It attaches proximally to the fibrous bands of the medial gastrocnemius tendon and fascial expansions of the adductor magnus tendon, with no osseous attachment identified.
The superficial portion of the POL is rather thin and appears to represent a confluence of fibers from the SMCL and the semimembranosus more distally. The capsular portion appears to represent a confluence of fibers from the semimembranosus, adductor magnus, and medial gastrocnemius (see Fig. 1-7). The central arm appears more robust, having contributions from the semimembranosus and medial gastrocnemius.
Controversy remains on whether three separate distinct anatomic structures make up the POL. Other authors36 have not found three distinct structures and note that with tibial rotation, different portions of the posteromedial capsule appear under tension but are not anatomically separate structures.
Semimembranosus
Controversy exists with respect to the exact number of attachments of the semimembranosus tendon at the knee joint.5,6,8,22,24,25,27,34,46 However, it appears that three major attachments have been consistently identified. The common semimembranosus tendon bifurcates into a direct and anterior arm just distal to the joint line. LaPrade and coworkers28,29 described the direct arm attaching to an osseous prominence called the tuberculum tendinis, approximately 11 mm distal to the joint line on the posteromedial aspect of the tibia. These authors also noted a minor attachment of the direct arm that extends to the medial coronary ligament along the posterior horn of the medial meniscus (see Fig. 1-4). A thinning of the capsule or capsular defect may be identified just distal to the femoral attachment of the medial head of the gastrocnemius and proximal to the direct arm of the semimembranosus. This is often the site of the formation of a Baker cyst.
Warren and Marshall46 believed the semimembranosus tendon sheath and not the tendon itself extends distally over the popliteus muscle and inserts directly into the posteromedial aspect of the tibia, with some fibers coalescing with SMCL fibers inserting in the same region. These authors contend that these fibers do not have functional significance, because no change was found in the position or tension of the MCL when those fibers were transected. LaPrade and associates29 separated the distal tibial expansion into a medial and a lateral division. Both divisions originating on the coronary ligament of the posterior horn of the medial meniscus are located on either side of the direct arm of the semimembranosus. The divisions then course distally to cover the posterior aspect of the popliteus muscle and insert onto the posteromedial aspect of the tibia, forming an inverted triangle. These authors noted that the medial division attaches just posterior to the SMCL, whose fibers coalesce with the superficial arm of the POL (as previously noted by Hughston and colleagues22) rather than the MCL.
In the authors’ experience, as shown in Figure 1-8, the semimembranosus tendon sheath and not the tendon itself comprises the distal tibial expansion, which includes a medial and a lateral division with a central raphae separating the two. The anterior arm of the semimembranosus courses deep to the SMCL and attaches directly to bone just distal to the medial joint capsule on the tibia (Fig. 1-9). There are fibrous connections between the SMCL and the anterior arm of the semimembranosus, but only the anterior arm of the semimembranosus has an osseous attachment in this region. Because both the direct and the anterior arms of the semimembranosus anchor directly to bone and attach distal to the tibial margin of the medial joint capsule, these are not considered part of either layer 2 or layer 3 as described by Warren and Marshall.46
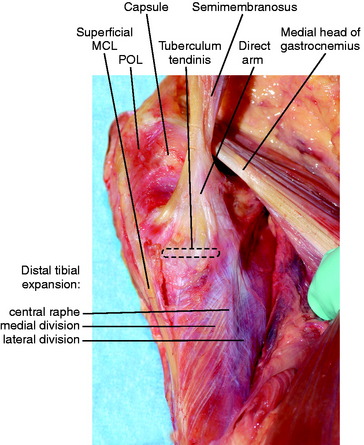
FIGURE 1-8 Distal tibial expansion of the semimembranosus tendon sheath with its medial and lateral divisions.
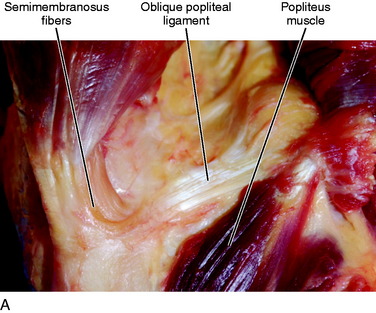
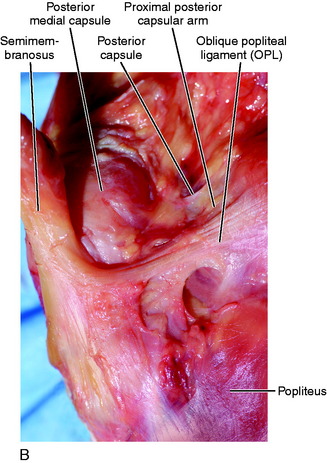
The third major attachment of the semimembranosus is the OPL. Warren and Marshall46 described the semimembranosus tendon sheath as forming fiber tracts that make up the OPL, although they admit some collagen fibers may come from the tendon itself. LaPrade and associates29 described a lateral expansion off the common semimembranosus tendon, just proximal to its bifurcation into the direct and anterior arms, that coalesces to form a portion of the OPL, in addition to the capsular arm of the POL. As shown in Figure 1-10A–B, it is difficult to appreciate distinct structures making up the origin of the OPL because of the significant confluence of fibers in the region. However, there are fibers originating from both the semimembranosus tendon and its sheath that contribute to its origin.
The OPL is described as a broad fascial band that courses laterally and proximally across the posterior capsule. LaPrade and associates29 noted two distinct lateral attachments of the OPL (proximal and distal). The proximal attachment is broad, extending to the fabella, the posterolateral capsule, and the plantaris (see Fig. 1-10). It does not attach directly to the lateral femoral condyle. The distal attachment is on the posterolateral aspect of the tibia, just distal to the posterior root of the lateral meniscus, but not directly attaching to the lateral meniscus as described by Kim and coworkers.27 It is theorized that this may serve a functional role limiting hyperextension, but this has not been demonstrated in any biomechanical study to date.
LaPrade and associates29 also described a proximal capsular arm of the semimembranosus as a thin aponeurosis that traverses medially to laterally along the superior border of the OPL. As it courses laterally, it blends with the posterolateral capsule and inserts on the distal lateral femur just proximal to the capsular insertion while at the same time extending fibers to the short head of the biceps femoris tendon (see Fig. 1-10B–C).
Layer 3: DMCL and Knee Capsule
The capsule of the knee joint is thin anteriorly and envelopes the fat pad. In this area, the capsule is easily separated from the overlying superficial retinaculum until it reaches the margin of the patella, where it is difficult to separate the capsule from the overlying superficial structures.46 Under the SMCL lies a vertical thickening of the knee capsule known as the distal medial collateral ligament (DMCL). The DMCL crosses the joint from the distal femur to the medial meniscus and inserts into the proximal tibia at sites adjacent to the articular surfaces of the femur and tibia. These separate divisions of the DMCL are named the meniscofemoral and meniscotibial ligaments. Warren and Marshall46 noted that the meniscofemoral portion of the DMCL had a discrete attachment onto the distal femur at its articular margin. Similarly, the meniscotibial portion of the DMCL, also known as the coronary ligament, is easily separated from the overlying SMCL in layer 2 before attaching to the tibia at its articular margin (Fig. 1-11).
The deepest structure on the medial side is the capsule of the knee, which envelopes the entire joint and extends proximally up to the suprapatellar pouch and distally to the attachment site of the meniscotibial ligament on the tibia–articular cartilage border.46
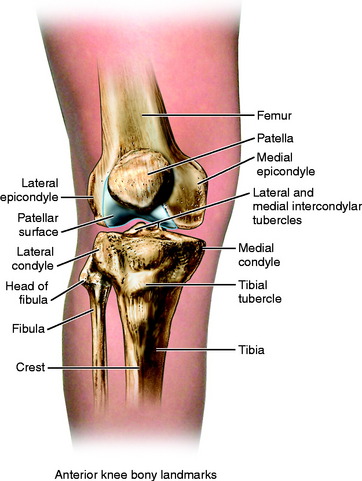
ANTERIOR ANATOMY OF THE KNEE
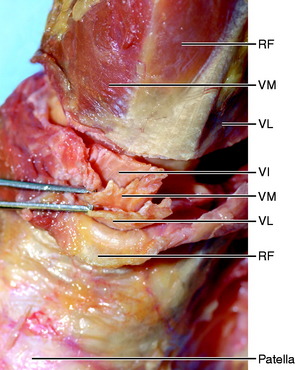
Quadriceps Mechanism
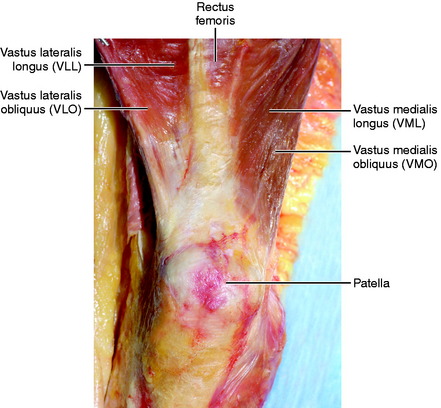
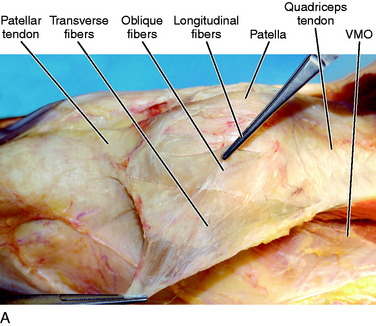
The quadriceps consists of the rectus femoris, adjacent to the vastus medialis and lateralis on either side, and the vastus intermedius deep (Fig. 1-12). The rectus femoris is located centrally and superficially in the quadriceps mechanism and widens distally as it approaches the superior aspect of the patella. Reider and colleagues35 found the width of the rectus femoris tendon to be 3 to 5 cm at the proximal pole of the patella. Some of the rectus tendon fibers insert into the superior aspect of the patella, but the majority continue over the anterior surface of the patella and are continuous with the patellar tendon distally. This is in contrast to the other components of the quadriceps mechanism that do not commonly contribute directly to the patellar tendon. The vastus medialis has fibers that run parallel to the rectus femoris fibers, called the vastus medialis longus, and others that run obliquely in relation to the rectus, termed the vastus medialis obliquus (VMO) according to Lieb and Perry.31 Conlan and coworkers7 described the VMO originating from the medial intermuscular septum and the adductor longus tendon proximal to the adductor tubercle. The angle of the obliquity of the VMO fibers varies considerably. Reider and colleagues35 found a range of 55° to 70° in a cadaveric study. This variability in obliquity has been implicated in patellar maltracking.
The muscle of the vastus medialis extends distally and often becomes tendinous only millimeters from its patellar insertion. Reider and colleagues35 noted that some fibers insert directly into the patella, whereas others course more distally and contribute to the medial retinaculum. Conlan and coworkers7 contended that some fibers of the VMO extend more distally and actually contribute to the patellar tendon. As shown in Figure 1-12, the vast majority of the VMO fibers either attach directly onto the patella or extend more distally to make up the medial retinaculum. The most medial fibers of the medial retinaculum converge into the medial border of the patellar tendon, but do not provide a significant contribution to the patellar tendon fibers.
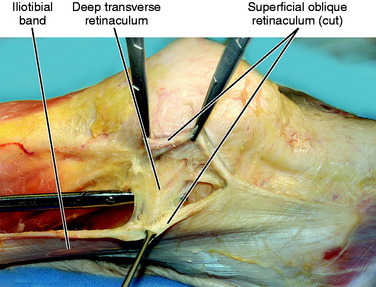
The vastus lateralis muscle is divided similarly to the vastus medialis with a longus and an obliquus portion. The insertions of the longus and obliquus tendons are quite variable, according to Hallisey and associates.16 These authors contended that the amount of vastus lateralis tendon that travels over the anterior cortex of the patella and contributes to the patellar tendon distally is variable. In some cases, the lateralis tendon fibers remain lateral to the patella and interdigitate with the fibers of the iliopatellar tract without contributing to the patellar tendon (Fig. 1-13). The insertion of the obliquus fibers is also variable according to Hallisey and associates.16 These authors found that in some specimens, the obliquus tendon fibers insert into the vastus lateralis longus fibers proximal to the patella; in others, they blend into the iliopatellar tract before inserting on the patella. As shown in Figure 1-13, it is the experience of the authors of this chapter that the most medial fibers of the lateralis obliquus tend to coalesce with the fibers of the longus, whereas the most lateral obliquus fibers coalesce with the iliopatellar tract. The vastus lateralis does not provide a significant contribution to the patellar tendon.
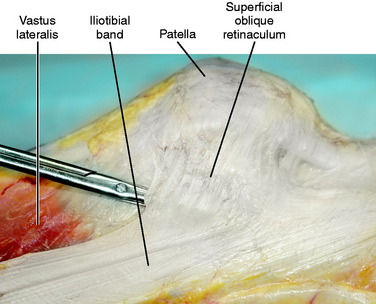
FIGURE 1-13 Longitudinal fibers of the vastus lateralis blend with fibers of the superficial oblique retinaculum.
The fibers of the lateralis run more parallel to the rectus femoris fibers than to the vastus medialis (see Fig. 1-12). The average obliquity of the lateralis fibers is 31°, according to Reider and colleagues.35 The lateralis fibers also become tendinous more proximally than the medialis, an average of 2.8 cm proximal to the patella.35 The angle of insertion of the obliquus fibers is rather variable, with an average of 48.5° in men and 38.5° in women.30
The vastus intermedius is deep to the rectus femoris, inserts directly into the proximal pole of the patella, and blends with the fibers of the medialis and lateralis that insert in similar fashion. Previous descriptions of the quadriceps tendon insertion depict a trilaminar arrangement of fibers, with the rectus femoris contributing the most superficial fibers, the medialis and lateralis contributing the middle layer, and finally, the intermedius contributing the deepest fibers. Reider and colleagues35 described the inserting fibers as more of a coalescence rather than distinct layers as previously described. It is the authors’ experience that the quadriceps tendon is a coalescence of fibers at the proximal pole of the patella, but as one travels a few centimeters proximal, four distinct layers to the quadriceps tendon can be identified and separated from one another (Fig. 1-14). When harvesting a quadriceps tendon graft, it is important that all layers are identified.
Fascial Layers
Lateral
The most superficial layer laterally, termed the aponeurotic layer by Terry and colleagues,43 is composed of the superficial fascia of the vastus lateralis and biceps femoris. These fibers, termed arciform fibers, travel transversely across the anterior aspect of the patella to blend at the midline with the superficial fascia of the sartorius, which begins medially.
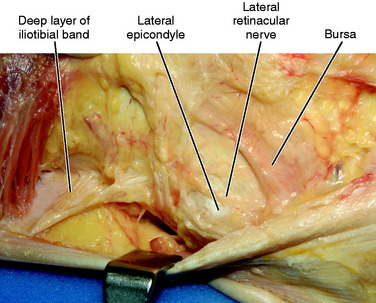
The next layer is termed the superficial layer by Terry and colleagues.43 It is made up of the iliopatellar tract, which connects the iliotibial band to the patella.13,45 The iliopatellar tract has been further subdivided into a superficial and a deep layer by Fulkerson and Gossling13 who described two different fiber orientations. The most superficial is termed the superficial oblique retinaculum because its fiber orientation is oblique. This tract inserts along the lateral border of the patella (see Fig. 1-13). In addition, there are deep transverse fibers that also connect the iliotibial band with the lateral aspect of the patella (Fig. 1-15). In this deeper, more transverse tract is the patellotibial ligament, which originates just proximal to Gerdy’s tubercle on the tibia and inserts on the inferior portion of the lateral aspect of the patella.13 Just deep to this ligament is the lateral meniscopatellar ligament, which runs between the anterior horn of the lateral meniscus and the inferior aspect of the patella. It is a thickening of the anterolateral capsule. The deepest layer on the lateral side is the capsular-osseous layer, which anchors the iliotibial band to the femur through the lateral intermuscular septum and travels anteriorly to the patella. Some authors26,43,45 contended that it includes the lateral patellofemoral ligament, but the experience of the authors of this chapter is that a distinct ligament is not present.
As shown in Figure 1-16, the capsular-osseous layer of the iliotibial tract has a femoral attachment proximal to the lateral epicondyle. At the level of the lateral epicondyle is a bursa deep to the iliotibial tract. It is the authors’ experience that there commonly is an identifiable nerve, which is called the lateral retinacular nerve, within this bursa that may play a role in pain associated with runner’s knee. During an iliotibial tract lengthening procedure for recalcitrant runners’ knee, it is the authors’ belief that while the iliotibial bursa is excised, the lateral retinacular nerve should be identified and cut posterior to the lateral epicondyle to prevent recurrence of this painful condition.
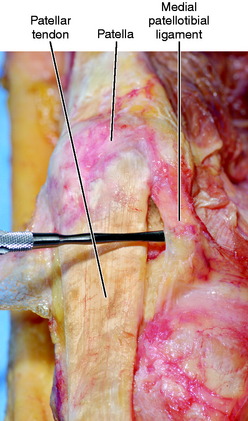
Medial
The next layer is considered to be the same as layer 2 as described by Warren and Marshall.46 This is composed of the MPFL and the SMCL. In this layer is the medial retinaculum, which is defined as the VMO fibers running transversely from the anterior border of the SMCL to the medial aspect of the patella. The medial patellotibial ligament is also found in this middle layer (Fig. 1-17). According to Conlan and coworkers,7 it originates on the inferior portion of the medial aspect of the patella and travels distally and posteriorly to insert on the anteromedial aspect of the tibia. The deepest structure found on the anteromedial aspect of the knee is the medial meniscopatellar ligament, which is a thickening of the capsule that runs between the anterior horn of the medial meniscus and the inferior portion of the medial border of the patella7 (Fig. 1-18).
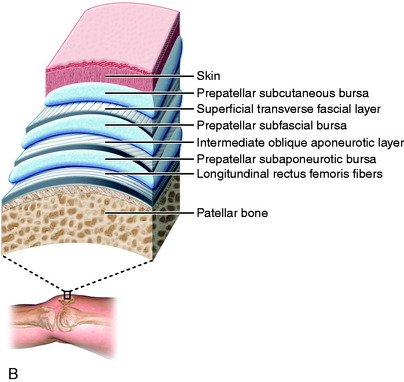
Prepatellar
The fascial layer covering the quadriceps is termed the fascia lata. Dye and coworkers11 noted that the fascia lata extends distally as the most superficial layer overlying the patella after the skin and subcutaneous tissue. These authors described the fascia lata as an extremely thin layer that has little structural integrity, but visible transverse fiber orientation. This is in contrast to the intermediate layer overlying the patella, which has an oblique fiber orientation proximally and becomes more transverse distally over the patellar tendon. Dye and coworkers11 described the intermediate layer consisting of tendinous fibers from the vastus medialis and lateralis, in addition to the superficial fibers of the rectus femoris that extend over the anterior aspect of the patella.
The deepest layer anterior to the patella is composed of the deeper fibers of the rectus femoris that extend distal to the proximal pole of the patella and are intimately associated with the anterior cortex of the patella as they continue to contribute to the fibers of the patellar tendon (Fig. 1-19).
Dye and coworkers11 noted that these layers form three separate bursae superficial to the patella. The most superficial is termed the prepatellar subcutaneous bursa (between the skin and the superficial fascia lata). The middle bursa is termed the prepatellar subfascial bursa (between the superficial fascia lata and the oblique intermediate layer). Finally, the deepest bursa is called the prepatellar subaponeurotic bursa (between the intermediate and the deep aponeurotic layers). It should be noted that no bursa exists between the deepest aponeurotic layer and the anterior cortex of the patella, as others have suggested.23a
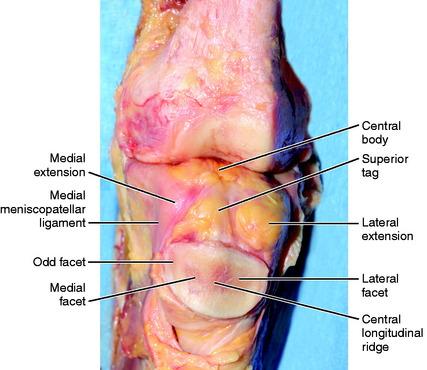
Patella
The patella is a sesamoid bone deeply associated with the quadriceps tendon, as previously described (Fig. 1-20). The articular surface of the patella is often divided into facets based on longitudinal ridges. The major longitudinal ridge divides the medial and the lateral facets of the patella. A second longitudinal ridge near the medial border of the patella separates the medial facet from a thin strip of articular surface known as the odd facet (see Fig. 1-18). Wiberg47 classified the morphology of patellae into three major types based upon the position of the longitudinal ridges. Type I patella have medial and lateral facets that are equal in size. Type II patella have a medial facet slightly smaller than the lateral facet. Type III patella have a very small and steeply angled medial facet, whereas the lateral facet is broad and concave. According to Dye and coworkers,11 type II patella are the most common (present in 57% of knees) followed by type I (24%), and type III (19%).
Patellar Tendon
The patellar tendon courses between the inferior pole of the patella and the tibial tubercle (see Fig. 1-17). This tendon consists mostly of fibers from the rectus femoris, as previously mentioned. The structure inserts on the proximal tibia, just distal to the most proximal portion of the tibial tubercle. It blends medially and laterally with the fascial expansions of the anterior surface of the tibia and the iliotibial band. Dye and coworkers11 reported an average length of 46 mm, with a range of 35 to 55 mm.
Infrapatellar Fat Pad
The infrapatellar fat pad is an intracapsular, but extrasynovial structure; the deepest portion is covered by a synovial layer. This structure has been consistently identified to have a thick central body, with thinner medial and lateral extensions (see Fig. 1-18). It has attachments to the inferior pole of the patella proximally, the patellar tendon and anterior capsule anteriorly, the anterior horns of the medial and lateral menisci plus the proximal tibia inferiorly, and the intercondylar notch posteriorly via the ligamentum mucosum.14 The ligamentum mucosum is an embryonic remnant separating the medial and lateral compartments of the knee. It has two alar folds that attach to the infrapatellar fat pad, allowing it to maintain its position in the joint.17
Gallagher and associates14 identified two clefts in the infrapatellar fat pad: a horizontal cleft, found just inferior to the ligamentum mucosum, and a vertical cleft, located anterior to the superior tag of the central body. It has been postulated that these clefts may play a role in reducing the friction between the anterior capsule and the femoral condyles, but they also may be a location for loose bodies to hide.
Inflammation in the infrapatellar fat pad has been implicated as a source of anterior knee pain. Hoffa’s disease is characterized by inflammation and hypertrophy, with subsequent trapping of the fat pad between the patellar tendon and the femoral condyles.14 The treatment frequently consists of resection of the fat pad, but this has been associated with a decrease in patellar blood supply.20 The fat pad may also become inflamed after arthroscopic surgery because of portal placement. This may lead to fibrous scarring, which can limit motion and serve as a source for residual pain.10 Fibrous scars that occur after arthroscopy have a 50% resolution rate after one year.42 It is recommended that portal placement be well medial and lateral to the patellar tendon borders so that damage to the central body and superior tag can be minimized in order to limit this potential complication.14
Superficial Neurovascular Structures
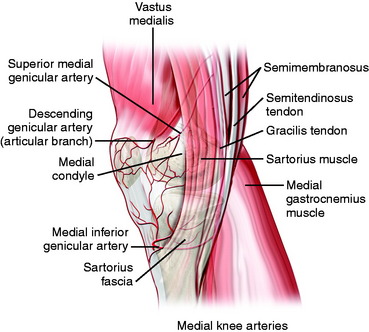
The medial inferior genicular artery traverses beneath the SCML after branching from the popliteal artery (Figs. 1-21 and 1-22). It can be visualized on the anterior border of the SMCL as it courses toward the patellar tendon and medial meniscus. This vascular structure may be encountered during any dissection on the medial aspect of the knee, most notably, during a posteromedial approach for meniscal repair. If identified in the approach, it must be retracted or cauterized to provide a clear approach to the medial meniscus.
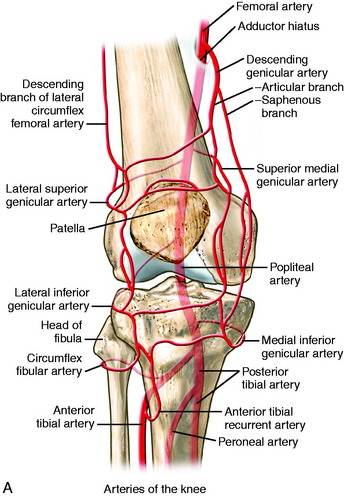
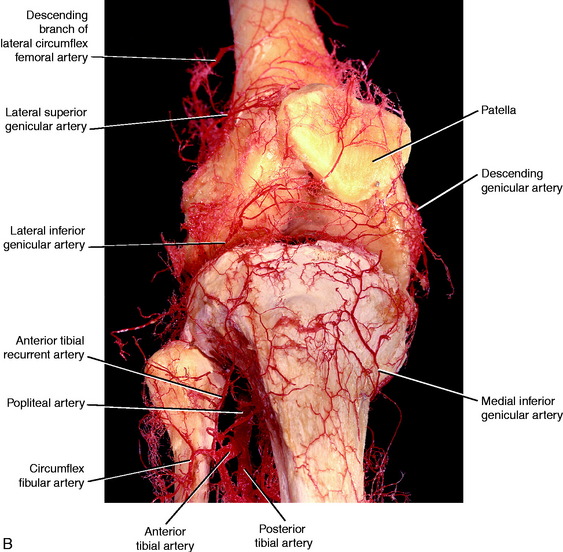
FIGURE 1-21 A, Arterial vasculature of the knee. B, Detailed vascularity shown after specialized injection technique.
(Unpublished from Kaderly RF, Butler DL, Noyes FR, Grood ES: The three-dimensional vascular anatomy of the human knee joint.)
Other important structures located on the medial side of the knee are the saphenous nerve with its sartorial and infrapatellar branches, the medial femoral cutaneous nerve, and the medial retinacular nerve (Fig. 1-23). These nerves may be easily injured with medial dissection of the knee. It has been reported that injury to the saphenous nerve occurs in 7% to 22% of patients during arthroscopic meniscal repair.2 According to Dunaway and colleagues,9 cadaver dissections in 42 knees revealed that the sartorial branch of the saphenous nerve consistently became extrafascial between the sartorius and the gracilis. However, this location varied between 37 mm proximal to the joint line to 30 mm distal to the joint line, with the nerve being extrafascial at the joint only 43% of the time and deep to the sartorius fascia in 66% of specimens. Dunaway and colleagues9 noted that only 2.8% of the specimens dissected had a sartorial branch anterior to the sartorius fascia. These authors recommend that during an inside-out medial meniscus repair, staying anterior during dissection minimizes the risk of injury to the sartorial branch. Horner and Dellon18 described the sartorial branch as the terminal branch of the saphenous nerve that passes 3 cm posterior to the central point of the medial condyle of the femur and continues to the medial aspect of the foot alongside the saphenous vein.
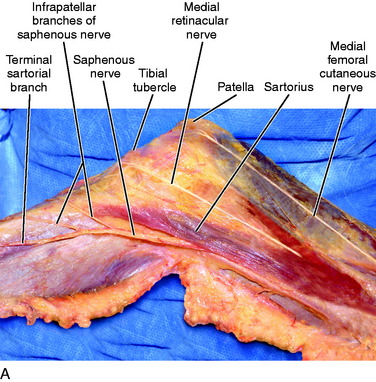
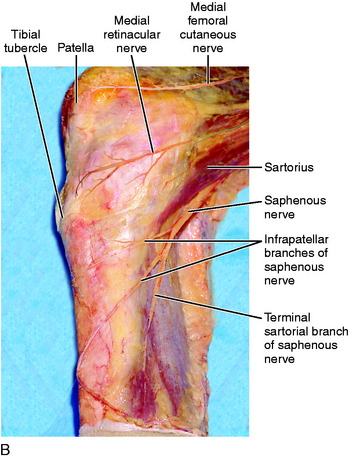
FIGURE 1-23 A, Anteromedial view of the superficial nerves. B, Medial view of the superficial nerves.
The infrapatellar branch of the saphenous nerve may also be easily damaged with indiscriminate dissection on the medial aspect of the knee, leading to postoperative pain and paresthesia. Postoperative numbness, paresthesia, or hypersensitivity in the distribution of the infrapatellar branch of the saphenous nerve has been reported in the literature38: 21% in the Mayo Clinic series, 51.5% in the Iowa series,and 40% in the Alberta series.19 The risk of damage is increased by the varying course of the nerve. The infrapatellar branch of the saphenous nerve may have four different courses at the level of the medial joint line, which are described by the nerve’s relationship to the sartorius muscle. The nerve may be posterior, penetrating, parallel, or anterior to the sartorius, with the most common type being posterior (62.2%).1 Arthornthurasook and Gaew-im1 reported that the infrapatellar branch of the saphenous nerve is an average distance of 40.6 mm from the medial epicondyle when the nerve exits and travels posterior to the sartorius. Horner and Dellon18 described the infrapatellar branch separating from the saphenous nerve in the proximal third of the thigh in 17.6% of specimens, in the middle third in 58.8%, and in the distal third of the thigh in 23.5%. This nerve innervates not only the patella but also the anterior-inferior capsule.18
Horner and Dellon18 described the medial femoral cutaneous nerve traveling superficially to the sartorius muscle in 39.1% of knees. However, this nerve often travels in Hunter’s canal and perforates the sartorius (30.4% of knees) or continues in Hunter’s canal and exits deep to the sartorius (30.4% of knees). The termination of this nerve is the most superficial constant branch that eventually bisects the patella to form a prepatellar plexus before continuing to the lateral aspect of the knee and pairing with the infrapatellar branch of the saphenous nerve proximal to the knee joint.
The medial retinacular nerve has also been described as residing on the medial aspect of the knee near the vastus medialis. The vastus medialis is innervated by branches from the femoral nerve. The terminal branch of the nerve to the vastus medialis ends as the medial retinacular nerve. According to Horner and Dellon,18 this nerve may traverse within the vastus medialis (90% of knees) or lie superficial to its fascia (10% of knees). The nerve enters the knee capsule beneath the medial retinaculum, 1 cm proximal to the adductor tubercle, and sends a branch to the MCL.18 This nerve was not identified in dissections performed by the authors of this chapter.
Indiscriminate dissection on the medial side of the knee could easily damage any one of these described nerves, leading to the pathology already noted. Painful neuromas and complex regional pain syndrome can turn a successful operation into a complicated pain syndrome. Horner and Dellon18 advised that the surgeon be aware of these pitfalls and recognize the possibility that symptomatology may result from damage to one or more nerves that require diagnostic nerve blocks at multiple sites to identify the pathology. Unnecessary subsequent surgeries for postoperative pain may be prevented by identifying the true cause of pain, which may very well be the result of nerve damage. A neurectomy may be required when a nerve block provides only temporary relief of pain.18
1 Arthornthurasook A., Gaew-Im K. Study of the infrapatellar nerve. Am J Sports Med. 1988;16:57-59.
2 Austin K.S., Sherman O.H. Complications of arthroscopic meniscal repair. Am J Sports Med. 1993;21:864-869.
3 Brantigan O.C., Voshell A.F. The mechanics of the ligaments and menisci in the knee joint. J Bone Joint Surg. 1941;23A:44-61.
4 Brantigan O.C., Voshell A.F. The tibial collateral ligament: its function, its bursae, and its relation to the medial meniscus. J Bone Joint Surg Am. 1943;25:121-131.
5 Cave A.E., Porteous C.J. A note on the semimembranosus muscle. Ann R Coll Surg Engl. 1959;24:251-256.
6 Cave A.E., Porteous C.J. The attachments of m. semimembranosus. J Anat. 1958;9Z(Pt 4):638.
7 Conlan T., Garth W.P., Lemons J.E. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg. 1993;75:682-693.
8 Cross M.J. Proceedings: the functional significance of the distal attachment of the semimembranous muscle in man. J Anat. 1974;118(pt 2):401.
9 Dunaway D.J., Steensen R.N., Wiand W., Dopirak R.M. The sartorial branch of the saphenous nerve: its anatomy at the joint line of the knee. Arthroscopy. 2005;21:547-551.
10 Duri Z.A., Aichroth P.M., Dowd G. The fat pad. Clinical observations. Am J Knee Surg. 1996;9:55-66.
11 Dye S.F., Campagna-Pinto D., Dye C.C., et al. Soft-tissue anatomy anterior to the human patella. J Bone Joint Surg Am. 2003;85:1012-1017.
12 Fischer R.A., Arms S.W., Johnson R.J., Pope M.H. The functional relationship of the posterior oblique ligament to the medial collateral ligament of the human knee. Am J Sports Med. 1985;13:390-397.
13 Fulkerson J.P., Gossling H.R. Anatomy of the knee joint lateral retinaculum. Clin Orthop Relat Res. 1980;153:183-188.
14 Gallagher J., Tierney P., Murray P., O’Brien M. The infrapatellar fat pad: anatomy and clinical correlations. Knee Surg Sports Traumatol Arthrosc. 2005;13:268-272.
15 Haimes J.L., Wroble R.R., Grood E.S., Noyes F.R. Role of the medial structures in the intact and anterior cruciate ligament-deficient knee. Limits of motion in the human knee. Am J Sports Med. 1994;22:402-409.
16 Hallisey M.J., Doherty N., Bennett W.F., Fulkerson J.P. Anatomy of the junction of the vastus lateralis tendon and the patella. J Bone Joint Surg Am. 1987;69:545-549.
17 Hardaker W.T., Whipple T.L., Bassett F.H.3rd. Diagnosis and treatment of the plica syndrome of the knee. J Bone Joint Surg Am. 1980;62:221-225.
18 Horner G., Dellon A.L. Innervation of the human knee joint and implications for surgery. Clin Orthop Relat Res. 1994;301:221-226.
19 Huckell J.R. Is meniscectomy a benign procedure? A long-term follow-up study. Can J Surg. 1965;8:254-260.
20 Hughes S.S., Cammarata A., Steinmann S.P., Pellegrini V.D.Jr. Effect of standard total knee arthroplasty surgical dissection on human patellar blood flow in vivo: an investigation using laser Doppler flowmetry. J South Orthop Assoc. 1998;7:198-204.
21 Hughston J.C. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the anterior cruciate ligament. Results of long-term follow-up. J Bone Joint Surg Am. 1994;76:1328-1344.
22 Hughston J.C., Andrews J.R., Cross M.J., Moschi A. Classification of knee ligament instabilities. Part I. The medial compartment and cruciate ligaments. J Bone Joint Surg Am. 1976;58:159-172.
23 Hughston J.C., Eilers A.F. The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. J Bone Joint Surg Am. 1973;55:923-940.
23a International Anatomical Nomenclature Committee. Nomina anatomica. Authorized by the 12th International Congress of Anatomists in London, 1985. 6th ed. Edinburgh: Churchill Livingstone; 1989.
24 Kaplan E.B. Factors responsible for the stability of the knee joint. Bull Hosp Joint Dis. 1957;18:51-59.
25 Kaplan E.B. Some aspects of functional anatomy of the human knee joint: an integral part of the deep capsular layer (layer III). Clin Orthop Relat Res. 1962;23:18-29.
26 Kaplan E.B. The iliotibial tract. J Bone Joint Surg. 1958;40A:817-832.
27 Kim Y.C., Yoo W.K., Chung I.H., et al. Tendinous insertion of semimembranosus muscle into the lateral meniscus. Surg Radiol Anat. 1997;19:365-369.
28 LaPrade R.F., Engebretsen A.H., Ly T.V., et al. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89:2000-2010.
29 LaPrade R.F., Morgan P.M., Wentorf F.A., et al. The anatomy of the posterior aspect of the knee. An anatomic study. J Bone Joint Surg Am. 2007;89:758-764.
30 Last R.J. Some anatomical details of the knee joint. J Bone Joint Surg Br. 1948;30:683-688.
31 Lieb F.J., Perry J. Quadriceps function. An anatomical and mechanical study using amputated limbs. J Bone Joint Surg. 1968;50A:1535-1548.
32 Loredo R., Hodler J., Pedowitz R., et al. Posteromedial corner of the knee: MR imaging with gross anatomic correlation. Skeletal Radiol. 1999;28:305-311.
33 Moore K.L., Dalley A.F. Clinically oriented anatomy. In: Lower Limb. New York: Williams & Wilkins; 1999:503-663.
34 Muller W., editor. The Knee: Form, Function and Ligament Reconstruction. New York: Springer-Verlag, 1983.
35 Reider B., Marshall J.L., Koslin B., et al. The anterior aspect of the knee joint. An anatomical study. J Bone Joint Surg. 1981;63A:351-356.
36 Robinson J.R., Sanchez-Ballester J., Bull A.M., et al. The posteromedial corner revisited. An anatomical description of the passive restraining structures of the medial aspect of the human knee. J Bone Joint Surg Br. 2004;86:674-681.
37 Sims W.F., Jacobson K.E. The posteromedial corner of the knee: medial-sided injury patterns revisited. Am J Sports Med. 2004;32:337-345.
38 Smirk C., Morris H. The anatomy and reconstruction of the medial patellofemoral ligament. Knee. 2003;10:221-227.
39 Standring S., editor. Gray’s Anatomy: The Anatomical Basis of Clinical Practice, 39th ed, New York: Churchill Livingstone, 2005.
40 Steensen R.N., Dopirak R.M., McDonald W.G.3rd. The anatomy and isometry of the medial patellofemoral ligament: implications for reconstruction. Am J Sports Med. 2004;32:1509-1513.
41 Sullivan D., Levy I.M., Sheskier S., et al. Medial restraints to anterior-posterior motion of the knee. J Bone Joint Surg. 1984;66A:930-936.
42 Tang G., Niitsu M., Ikeda K., et al. Fibrous scar in the infrapatellar fat pad after arthroscopy: MR imaging. Radiat Med. 2000;18:1-5.
43 Terry G.C., Hughston J.C., Norwood L.A. The anatomy of the iliopatellar band and iliotibial tract. Am J Sports Med. 1986;14:39-45.
44 Thompson J.C., editor. Netter’s Concise Atlas of Orthopaedic Anatomy. Teterboro, NJ: Icon Learning Systems, 2002.
45 Vieira E.L., Vieira E.A., da Silva R.T., et al. An anatomic study of the iliotibial tract. Arthroscopy. 2007;23:269-274.
46 Warren L.F., Marshall J.L. The supporting structures and layers on the medial side of the knee: an anatomical analysis. J Bone Joint Surg Am. 1979;61:56-62.
47 Wiberg G. Roentgenographic and anatomic studies on the femoro-patella jont. Acta Orthop Scand. 1941;12(3):319-410.
48 Yoshiya S., Kuroda R., Mizuno K., et al. Medial collateral ligament reconstruction using autogenous hamstring tendons: technique and results in initial cases. Am J Sports Med. 2005;33:1380-1385.