Chapter 2 Mechanisms of Noncontact Anterior Cruciate Ligament Injuries
As in the prevention of other injuries in sports, understanding injury mechanisms is a key component of preventing noncontact anterior cruciate ligament (ACL) injuries.1 The research effort to determine risk factors of sustaining noncontact ACL injuries is increasing as the concerns of increased incidents and cost for treatment, as well as serious consequences of noncontact ACL injuries, are growing. Prospective cohort studies are commonly used in epidemiological research designs for determining risk factors of injuries and diseases2 and are being used to determine risk factors of sustaining noncontact ACL injuries.3 The results of epidemiological studies with cohort designs, however, are descriptive in nature and lack cause-and-effect relationship between identified risk factors and the injury.2 Without a good understanding of the injury mechanisms, the risk factors of sustaining noncontact ACL injuries identified from epidemiological studies could be misinterpreted and could lead to the selection of nonoptimal injury prevention programs.
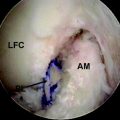
Mechanically, ACL injury occurs when an excessive tension force is applied on the ACL. A noncontact ACL injury occurs when a person self-generates great forces or moments at the knee that applied excessive loading on the ACL. An understanding of the mechanisms of ACL loading during active human movements, therefore, is crucial for understanding the mechanisms of noncontact ACL injuries and risk factors of sustaining noncontact ACL injuries. Berns et al4 investigated the effects of combined knee loading on ACL strain on 13 cadaver knees. The strain of the anteromedial (AM) bundle of the ACL was recorded using liquid mercury strain gauges at 0 and 30 degrees knee flexion. The results of this study showed that anterior shear force on the proximal end of the tibia was the primary determinant of the strain in the AM bundle of the ACL, whereas neither pure knee internal-external rotation moment nor pure knee valgus-varus moment had significant effects on the strain of the AM bundle of the ACL. The results of this study further showed that anterior shear force at the proximal end of the tibia combined with a knee valgus moment resulted in a significantly greater strain in the AM bundle of the ACL than did the anterior shear force at the proximal end of the tibia alone.
Markolf et al5 also investigated effects of anterior shear force at the proximal end of the tibia and knee valgus, varus, internal rotation, and external rotation moments on the ACL loading of cadaver knees. A 100N anterior shear force and 10-Nm knee valgus, varus, internal rotation, and external rotation moments were added to cadaver knees. The ACL loading was recorded as the knee was extended from 90 degrees flexion to 5 degrees hyperextension. The results of this study showed that an anterior shear force on the tibia generated significant ACL loading, whereas the knee valgus, varus, and internal rotation moments also generated significant ACL loading only when the ACL was loaded by the anterior shear force at the proximal end of the tibia. The results of this study further showed that the ACL loading due to the anterior shear force combined with either a valgus or a varus moment to the knee was greater than that due to the anterior shear force alone, whereas the ACL loading due to the anterior shear force combined with a knee external rotation moment was lower than that due to anterior shear force alone. The knee valgus and external rotation moment loading are elements of dynamic valgus that many current ACL injury prevention programs are trying to avoid.3 The results of the study by Markolf et al5 also showed that ACL loading due to the combined knee varus and internal rotation moment loading was greater than that due to either knee varus moment loading or internal rotation moment loading alone and that the ACL loading due to combined knee valgus and external rotation moment loading was lower than that due to either knee valgus or external rotation moment loading alone. Finally, the results of this study showed that the ACL loading due to the anterior shear force and knee valgus, varus, and internal rotation moments increased as the knee flexion angle decreased.
Fleming et al6 studied the effects of weight bearing and tibia external loading on ACL strain. They implanted a differential variable reluctance transducer to the AM bundle of the ACL of 11 subjects. ACL strains were measured in vivo when a subject’s leg was attached to a knee loading fixture that allowed independent application of anterior-posterior shear force, valgus-varus moments, and internal-external rotation moments to the tibia and simulation of weight-bearing conditions. The anterior shear force was applied on the proximal end of the tibia from 0N to 130N in 10-N increments. The valgus-varus moments were applied to the knee from −10 Nm to 10 Nm in 1-Nm increments. The internal-external rotation moments were applied to the knee from −9 Nm to 9 Nm in 1-Nm increments. The knee flexion angle was fixed at 20 degrees during the test. The results of this study showed that ACL strain significantly increased as the anterior shear force at the proximal end of the tibia and the knee internal rotation moment increased, whereas knee valgus-varus and external rotation moments had little effects on ACL strain under the weight-bearing condition.
Quadriceps muscles are the major contributor to the anterior shear force at the proximal end of the tibia through the patella tendon. DeMorat et al7 demonstrated that a 4500-N quadriceps muscle force could create ACL injuries at 20 degrees knee flexion. Eleven cadaver knee specimens were fixed to a knee simulator and loaded with 4500-N quadriceps muscle force. Quadriceps muscle contraction tests at 400 N (Q-400 tests) and KT-1000 tests were performed before and after the 4500-N quadriceps muscle force loading. Tibia anterior translations were recorded during the Q-400 and KT-1000 tests. All cadaver knee specimens were dissected after all tests to determine the ACL injury states. Six of the 11 specimens had confirmed ACL injuries (three complete ACL tears and three partial tears). All specimens showed increased tibia anterior translation in Q-400 and KT-1000 tests. The result of this study also showed that quadriceps muscle contraction caused not only tibia anterior translation but also tibia internal rotation.
Decreasing knee flexion angle increases the anterior shear force at the proximal end of the tibia by increasing the patella tendon–tibia shaft angle. With a given quadriceps muscle force, the anterior shear force at the proximal end of the tibia is determined by the patella tendon–tibia shaft angle, defined as the angle between the patella tendon and the longitudinal axis of the tibia.8 With a given quadriceps muscle force, the greater the patella tendon–tibia shaft angle, the greater the anterior shear force on the tibia. Nunley et al8 studied the relationship between the patella tendon–tibia shaft angle and knee flexion angle with weight bearing. Ten male and 10 female university students without known history of lower extremity injuries were recruited as the subjects. Sagittal plane x-ray films were taken for each subject at 0, 15, 30, 45, 60, 75, and 90 degrees knee flexion, bearing 50% of body weight. Patella tendon–tibia shaft angles were measured from the x-ray films. Regression analyses were performed to determine the relationship between patella tendon–tibia shaft angle and knee flexion angle and to compare the relationship between genders. The results showed that the patella tendon–tibia shaft angle was a function of the knee flexion angle, with the patella tendon–tibia shaft angle increasing as the knee flexion angle decreased, and that on average the patella tendon–tibia shaft angle was 4 degrees greater in females than in males. The relationship between the patella tendon–tibia shaft angle and knee flexion angle obtained by Nunley et al8 was consistent with those from other studies on the patella tendon–tibia shaft angle under non–weight-bearing conditions.9–11
Decreasing the knee flexion angle also increases ACL loading by increasing the ACL elevation angle and deviation angle, defined as the angle between the longitudinal axis of the ACL and the tibia plateau and the angle between the projection of the longitudinal axis of the ACL on the tibia plateau and the posterior direction of the tibia, respectively.12 The resultant force along the longitudinal axis of the ACL equals the anterior shear force on the ACL divided by the cosines of the ACL elevation and deviation angles. The greater the ACL elevation and deviation angles, the greater the ACL loading with a given anterior shear force on the ACL. Li et al12 determined the in vivo ACL elevation and deviation angles as functions of the knee flexion angle with weight bearing. Five young and healthy volunteers were recruited as the subjects. The ACL elevation and deviation angles at 0, 30, 60, and 90 degrees knee flexion with weight bearing were obtained using individualized dual-orthogonal fluoroscopic images and magnetic resonance imaging (MRI)-based, three-dimensional (3D) models. The results of this study showed that both the ACL elevation and deviation angles increased as the knee flexion angle decreased.
Several studies show that ACL loading increases as the knee flexion angle decreases. Arms et al13 studied the biomechanics of ACL rehabilitation and reconstruction and found that quadriceps muscle contraction significantly strained the ACL from 0 to 45 degrees knee flexion but did not strain the ACL when knee flexion was greater than 60 degrees. Beynnon et al14 measured the in vivo ACL strain during rehabilitation exercises and found that isometric quadriceps muscle contraction resulted in a significant increase in ACL strain at 15 and 30 degrees knee flexions but resulted in no change in ACL strain relative to the relaxed muscle condition at 60 and 90 degrees knee flexion. Li et al15,16 investigated the quadriceps and hamstring muscle loading on ACL loading and showed that the in situ ACL loading increased as the knee flexion angle decreased when quadriceps muscles were loaded, regardless of the hamstring muscle loading conditions.
Literature also shows that individuals at high risk of sustaining noncontact ACL injuries have a smaller knee flexion angle during athletic tasks than do individuals at low risk. Epidemiological studies show that female athletes are at higher risk of sustaining noncontact ACL injuries than their male counterparts.17–24 Recent biomechanical studies demonstrated that female recreational athletes exhibited small knee flexion angles in running, jumping, and cutting tasks.25,26 Studies also demonstrate that female adolescent athletes had a sharply increased ACL injury rate after age 13 years.27,28 A recent biomechanical study showed that female adolescent soccer players started decreasing their knee flexion angle during a stop-jump task after age 13 years.29 Taken together, these results suggest that small knee flexion angle during landing tasks may be a risk factor of sustaining noncontact ACL injuries.
Increasing peak posterior ground reaction forces during athletic tasks increases ACL loading by inducing an increased quadriceps muscle contraction. A posterior ground reaction force creates a flexion moment relative to the knee, which needs to be balanced by a knee extension moment generated by the quadriceps muscles.30 As previously described, the quadriceps muscle contraction adds an anterior shear force on the proximal end of the tibia through the patella tendon. The greater the posterior ground reaction force, the greater the quadriceps muscle force and the greater the ACL loading.30 Cerulli et al31 and Lamontagne et al32 recently recorded in vivo ACL strain in a hop-landing task. A differential variable reluctance transducer was implemented on the middle portion of the AM bundle of the ACLs of three subjects through surgical procedures. Subjects then performed the hop-landing task in a biomechanics laboratory. Force plate, electromyography (EMG), and in vivo ACL strain were recorded simultaneously. The results of this study showed that the peak ACL strain occurred at the impact peak vertical ground reaction force shortly after initial contact between foot and ground. Yu et al30 demonstrated that peak impact vertical and posterior ground reaction forces occurred essentially at the same time. Taken together, these results suggest that a hard landing with a great impact posterior ground reaction force may be a risk factor of sustaining noncontact ACL injuries.
Literature shows that individuals at a high risk of sustaining noncontact ACL injuries have greater peak posterior ground reaction forces in athletic tasks. Chappell et al26 studied the lower extremity kinetics as well as kinematics of university-age recreational athletes during landings of stop-jump tasks. Their results showed that female recreational athletes had greater peak resultant proximal tibia anterior shear force and knee joint resultant extension moment during landings of stop-jump tasks than did male recreational athletes. Yu et al studied the immediate effects of a newly designed knee brace with a constraint to knee extension during a stop-jump task.29–29b Their results showed that the university-age female recreational athletes had greater peak posterior ground reaction force during the landing of the stop-jump task than did their malecounterparts. Yu et al30 showed that the resultant peak proximal tibia anterior shear force was positively correlated to the peak posterior ground reaction force.
Hamstring co-contractions protecting the ACL have been a longstanding clinical concept because hamstring muscles provide a posterior shear force on the tibia that is supposed to reduce the anterior shear force on the tibia from the patellar tendon and thus unload the ACL. Recent scientific studies, however, did not support this concept. Li et al15 showed in a cadaver study that hamstring co-contraction did not significantly decrease tibia anterior translation when the knee flexion angle was less than 30 degrees. Beynnon et al14 found that the isometric hamstring co-contraction of the hamstring muscles did reduce in vivo ACL strain between 15 and 60 degrees knee flexion. Kingma et al33 found that hamstring muscle activation increased only 1.3 to 2.0 times, whereas knee extension moment increased 2.7 to 3.4 times with a knee flexion angle between 5 and 50 degrees, which did not suggest a hamstring recruitment pattern to reduce the ACL loading. O’Connor,34 Pandy et al,35 and Yu et al29 all studied ACL loading using a modeling and computer simulation approach and showed that the hamstring muscles did not reduce ACL loading at all when the knee flexion angle was small.
Although biomechanical studies showed that the knee valgus moment was not a major mechanism of ACL loading, a recent epidemiological study by Hewett et al3 reported that external knee valgus moment in a vertical drop landing–jump task was a predictor of ACL injuries. A total of 205 high school soccer, basketball, and volleyball players were followed for three competition seasons. Knee flexion and valgus angles at initial foot contact with the ground and the maximum knee flexion and valgus angles and maximum moments during the stance phase of the vertical drop landing–jump task were recorded prospectively for every subject. A total of nine subjects sustained ACL injuries after three competition seasons. The results of this study showed that knee abduction angle at landing was 8 degrees greater in ACL-injured than in uninjured athletes and that ACL-injured athletes had a 2.5 times greater peak external knee valgus moment and 20% higher peak vertical ground reaction force than did uninjured athletes. The results further showed that peak external knee valgus moment predicted ACL injury status with 73% specificity, 78% sensitivity, and a predictive R2 value of 0.88. The results of this study appear to suggest an association between knee valgus angle and moment with ACL injuries.
However, we may have to be cautious when interpreting the association of knee valgus angle and moment with noncontact ACL injuries observed in the study by Hewett et al.3 The observed preinjury knee valgus moments of the nine subjects who suffered ACL injuries in this study were less than 0.12 Nm/body weight/standing height. The average body weight and stranding height of the injured subjects in this study were 62 kg and 1.68 m, respectively. This means that the preinjury knee valgus moments of the nine injured subjects in this study were less than 12.5 Nm. These knee valgus moment loadings were similar to those in the studies by Berns et al,4 Markolf et al,5 and Fleming et al,6 which demonstrated that knee valgus loading did not significantly affect ACL loading unless a significant proximal tibia anterior shear force was applied. Furthermore, several other studies in the current literature demonstrate that knee valgus moment loading alone cannot injure the ACL when the MCL is intact. Bendjaballah et al36 studied the effects of knee valgus-varus moment loading on cruciate and collateral ligament loadings using a finite element model. Their results suggest that cruciate ligaments are not major valgus-varus moment loading bearing structures when collateral ligaments are intact. Matsumoto et al37 investigated the roles of the ACL and MCL in preventing knee valgus instability using cadaver knees. Their results demonstrate that the MCL is the major structure to stop medial knee space opening. Mazzocca et al38 tested the effect of knee valgus loading on MCL and ACL injuries. They found that the response of the ACL strain to knee valgus moment loading was minimal when the MCL was intact but significantly increased after the MCL rupture began due to knee valgus moment loading. Their results show that the ACL still had about 60% of its original strength after complete MCL ruptures with medial knee space openings greater than 15 mm due to knee valgus moment loading. This study clearly demonstrates that a complete ACL rupture due to knee valgus moment loading without a complete MCL rupture (grade III injury) is unlikely, whereas clinical observations show that the majority of noncontact ACL injuries do not have significant MCL injuries. A recent study by Fayad et al39 showed that only 5 of a total of 84 contact and noncontact ACL injuries had complete MCL ruptures. Taken together, these studies suggest that knee valgus moment loading alone is not likely to be a major ACL loading mechanism that can result in ACL rupture or a major risk factor of sustaining noncontact ACL injuries. More scientific studies are needed before we can confidently interpret the association of knee valgus angle and moment with noncontact ACL injuries as a sole risk factor of sustaining noncontact ACL injuries.
1 Bahr R, Krosshaug T. Understanding injury mechanisms: a key component of preventing injuries in sport. Br J Sports Med. 2005;39:324-329.
2 Portney LG, Watkins MP. Foundations of clinical research: applications to practice, ed 2, Upper Saddle River, NJ: Prentice Hall Health, 2000.
3 Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33:492-501.
4 Berns GS, Hull ML, Paterson HA. Strain in the anterior medial bundle of the anterior cruciate ligament under combined loading. J Orthop Res. 1992;10:167-176.
5 Markolf KL, Burchfield DM, Shapiro MM, et al. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13:930-935.
6 Fleming BC, Renstrom PA, Beynnon BD, et al. The effect of weightbearing and external loading on anterior cruciate ligament strain. J Biomech. 2001;34:163-170.
7 DeMorat G, Weinhold P, Blackburn T, et al. Aggressive quadriceps loading can induce noncontact anterior cruciate ligament injury. Am J Sports Med. 2004;32:477-483.
8 Nunley RM, Wright D, Renner JB, et al. Gender comparison of patellar tendon tibial shaft angle with weight bearing. Res Sports Med. 2003;11:173-185.
9 Smidt JG. Biomechanical analyses of knee flexion and extension. J Biomech. 1973;6:79-82.
10 Buff HU, Jones LC, Hungerford DS. Experimental determination of forces transmitted through the patella-femoral joint. J Biomech. 1988;21:17-23.
11 vanEijden TMGJ, De Boer W, Weijs WA. The orientation of the distal part of the quadriceps femoris muscle as a function of the knee flexion-extension angle. J Biomech. 1985;18:803-809.
12 Li G, DeFrate LE, Rubash HE, et al. In vivo kinematics of the ACL during weight-bearing knee flexion. J Orthop Res. 2005;23:340-344.
13 Arms SW, Pope MH, Johnson RJ, et al. The biomechanics of anterior cruciate ligament rehabilitation and reconstruction. Am J Sports Med. 1984;12:8-18.
14 Beynnon BD, Fleming BC, Johnson RJ, et al. Anterior cruciate ligament strain behavior during rehabilitation exercises in vivo. Am J Sports Med. 1995;23:24-34.
15 Li G, Rudy TW, Sakane M, et al. The importance of quadriceps and hamstring muscle loading on knee kinematics and in-situ forces in the ACL. J Biomech. 1999;32:395-400.
16 Li G, Zayontz S, Most E, et al. In situ forces of the anterior and posterior cruciate ligaments in high knee flexion: an in vitro investigation. J Orthop Res. 2004;22:293-297.
17 Ferretti A, Papandrea P, Conteduca F, et al. Knee ligament injuries in volleyball players. Am J Sports Med. 1992;20:203-207.
18 Paulos LE. Why Failures Occur Symposium: revision ACL surgery. American Orthopaedic Society for Sports Medicine Eighteenth Annual Meeting, San Diego, CA, July 1992. 1992.
19 Malone TR, Hardaker WT, Garrett WE, et al. Relationship of gender to anterior cruciate ligament injuries in intercollegiate basketball players. J South Orthop Assoc. 1993;2:36-39.
20 Pearl AJ. The athletic female. Champaign, IL: Human Kinetics, 1993;302-303.
21 Irelan ML. Special concerns of the female athlete. Sports injuries: mechanism, prevention, and treatment, ed 2, Philadelphia: Williams & Wilkins; 1994:153-187.
22 Lindenfeld TN, Schmitt DJ, Hendy MP, et al. Incidence of injury in indoor soccer. Am J Sports Med. 1994;22:354-371.
23 Woodford-Rogers B, Cyphert L, Denegar CR. Risk factors for anterior cruciate ligament injury in high school and college athletes. J Athl Train. 1994;29:343-346.
24 Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. Am J Sports Med. 1995;23:694-701.
25 Malinzak RA, Colby SM, Kirkendall DT, et al. A comparison of knee joint motions patterns between men and women in selected athletic maneuvers. Clin Biomech. 2001;16:438-445.
26 Chappell JD, Yu B, Kirdendall DT, et al. A comparison of knee kinetics between male and female recreational athletes in stop-jump tasks. Am J Sports Med. 2002;30:261-267.
27 Yu B, Kirkendall DT, Taft TN, et al. Lower extremity motor control-related and other risk factors for noncontact anterior cruciate ligament injuries. Instruct Course Lect. 2002;51:315-324.
28 Shea KG, Pfeiffer R, Wang JH, et al. Anterior cruciate ligament injury in pediatric and adolescent soccer players: an analysis of insurance data. J Pediatr Orthop. 2004;24:623-628.
29 Yu B, McClure SB, Onate JA, et al. Age and gender effects on lower extremity kinematics of youth soccer players in a stop-jump task. Am J Sports Med. 2005;33:1356-1364.
29a Yu B, Herman D, Preston J, et al. Immediate effects of a knee brace with a constraint to knee extension on knee kinematics and ground reaction forces in a stop-jump task. Am J Sports Med. 2004;32:1136-1143.
29b Yu B, Lin CF, Garrett WE. Lower extremity biomechanics during the landing of a stop-jump task. Clin Biomech. 2006;21:297-305.
30 Yu B, Chappell JD, Garrett WE. Authors’ response to letter to the editor. Am J Sports Med. 2006;34:312-315.
31 Cerulli G, Benoit DL, Lamontagne M, et al. In vivo anterior cruciate ligament strain behavior during a rapid deceleration movement: case report. Knee Surg Sports Traumatol Arthrosc. 2003;11:307-311.
32 Lamontagne M, Benoit DL, Ramsey DK, et al. What can we learn from in vivo biomechanical investigation of lower extremity? Proc XXIII Int Symp Biomech Sports. 2005:49-56.
33 Kingma I, Aalbersberg S, van Dieen JH. Are hamstrings activated to counteract shear forces during isometric knee extension efforts in healthy subjects? J Electromyogr Kinesiol. 2004;14:307-315.
34 O’Connor JJ. Can muscle co-contraction protect knee ligaments after injury or repair? J Bone Joint Surg Br. 1993;75(1):41-48. Jan;
35 Pandy MG, Garner BA, Anderson FC. Optimal control of non-ballistic muscular movements: a constraint-based performance criterion for rising from a chair. J Biomech Eng. 1995;117(1):15-26. Feb;
36 Bendjaballah MZ, Shirazi-Adl A, Zukor DJ. Finite element analysis of human knee joint in varus-valgus. Clin Biomech. 1997;12:139-148.
37 Matsumoto H, Suda Y, Otani T, et al. Roles of the anterior cruciate ligament and medial collateral ligament in preventing valgus instability. J Orthop Sci. 2001;6:28-32.
38 Mazzocca AD, Nissen CW, Geary M, et al. Valgus medial collateral ligament rupture causes concomitant loading and damage of the anterior cruciate ligament. J Knee Surg. 2003;16:148-151.
39 Fayad LM, Parellada JA, Parker L, Schweitzer ME. MR imaging of anterior cruciate ligament tears: is there a gender gap? Skeletal Radiol. 2003;32:639-646.
Boden BP, Dean GS, Feagin JA, et al. Mechanisms of anterior cruciate ligament injury. Ortho. 2000;23:573-578.
Caraffa A, Cerulli G, Projetti M, et al. Prevention of anterior cruciate ligament injuries in soccer. A prospective controlled study of proprioceptive training. Knee Surg Sports Traumatol Arthrosc. 1996;4:19-21.
Chappell JD, Herman DC, Knight BS, et al. Effect of fatigue on knee kinetics and kinematics in stop-jump tasks. Am J Sports Med. 2005;33:1022-1029.
Kanamori A, Woo SLY, Ma CB, et al. The forces in the anterior cruciate ligament and knee kinematics during a simulated pivot shift test: a human cadaveric study using robotic technology. J Arthroscop Relat Surg. 2000;16:633-639.
Li G, Rudy TW, Sakane M, et al. The importance of quadriceps and hamstring muscle loading on knee kinematics and in-situ forces in ACL. J Biomech. 1999;32:395-400.
Myklebust G, Engebretsen L, Braekken IH, et al. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sports Med. 2003;13:71-78.
Olsen O-E, Myklebust G, Engebretsen L, et al. Injury mechanisms for anterior cruciate ligament injuries in team handball. Am J Sports Med. 2004;32:1002-1012.
Petersen W, Braun C, Bock W, et al. A controlled prospective case control study of a prevention training program in female team handball players: the German experience. Arch Orthop Trauma Surg. 2005;125:614-621.
Soderman K, Werner S, Pietila T, et al. Balance board training: prevention of traumatic injuries of the lower extremities in female soccer players? A prospective randomized intervention study. Knee Surg Sports Traumatol Arthrosc. 2000;8:356-363.