Mastectomy
Partial Mastectomy
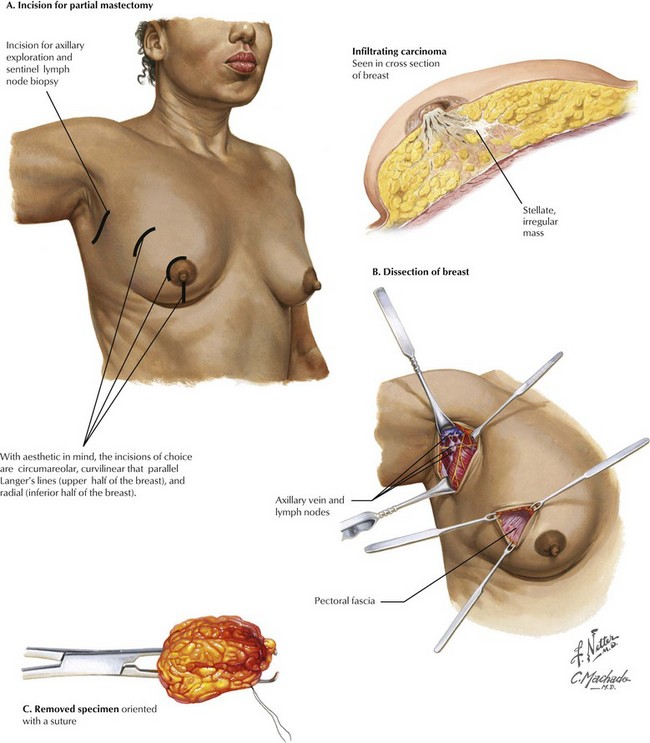
With breast conservation and aesthetics the focus of partial mastectomy, the choice of incision is of great importance (Fig. 46-1, A). Circumareolar incisions provide good cosmesis. Curvilinear incisions that parallel Langer’s lines of tension in the upper half of the breast also work well. In the inferior half of the breast, radial incisions provide good cosmesis. For palpable lesions, the incision should be made directly over the tumor. For nonpalpable tumors localized with a wire, care should be made to make the incision over the expected location of the tumor and not necessarily at the insertion of the wire.
Small skin flaps are raised, and then dissection can be performed sharply or with electrocautery. Breast tissue can be grasped with an Allis forceps to facilitate dissection, but care should be used to avoid tearing the tissues (Fig. 46-1, B).
Although currently no consensus exists on margins to obtain for breast-conserving surgery, it is important that the entire lesion is removed with negative margins. Once removed, the specimen must be oriented so that if a margin is positive, another more localized excision can be done (Fig. 46-1, C).
Total Mastectomy
Modified Radical Mastectomy
For most breast cancer patients in whom mastectomy is indicated, the procedure of choice is the modified radical mastectomy. This approach combines total mastectomy (discussed below) with axillary lymph node dissection (see Chapter 49). In the case of prophylactic mastectomy, the typical procedure is the total mastectomy.
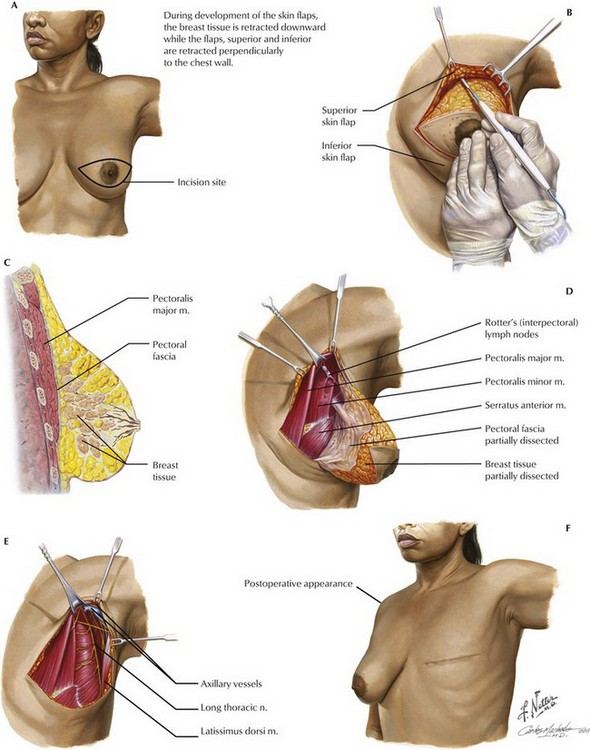
The incision for the procedure is typically an ellipse centered on the areola (Fig. 46-2, A). This incision should encompass previous biopsy and excision scars. Methylene blue dye is injected along the superior border of the nipple for SLNB (see Chapter 48).
Skin flaps are then raised, typically with the use of skin hooks or rakes to provide tension (Fig. 46-2, B). The skin flaps should be approximately 7 to 10 mm and thick enough to avoid necrosis and buttonholes, but thin enough to resect all breast tissue. These flaps are carried superiorly to the level of the clavicle and inferiorly to the inframammary fold. The flaps should reach the lateral border of the sternum medially and the latissimus dorsi muscle laterally.
Figure 46-2, C, shows a lateral view of the breast with the correct plane of dissection for mastectomy being deep to the pectoral fascia.
The breast is then dissected off the chest wall, starting superiorly at the clavicle (Fig. 46-2, D and E). This dissection continues inferiorly deep to the retromammary fascia and investing fascia of the pectoralis major muscle. The breast tissue is retracted inferiorly as electrocautery is used to dissect the tissue and investing fascia of the pectoralis from the underlying muscle.
Breast Removal and Reconstruction
For a total mastectomy, once the dissection has reached the inframammary fold, the breast can be removed and the overlying skin closed with drains in place (Fig. 46-2, F). If a modified radical mastectomy is performed, the lateral border of the breast that is attached to the axilla should be left in place, and the axillary lymph node dissection is completed. This approach will remove a single specimen containing the breast and contents of the axilla.
Clarke, M, Collins, R, Darby, S, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;366(9503):2087–2106.
Kuerer, HM. Kuerer’s breast surgical oncology. New York: McGraw-Hill Medical; 2010.
National Institues of Health (NIH) consensus conference. Treatment of early-stage breast cancer. JAMA. 1991;265(3):391–395.
Salhab, M, Bismohun, S, Mokbel, K. Risk-reducing strategies for women carrying BRCA1/2 mutations with a focus on prophylactic surgery. BMC Womens Health. 2010;10:28.
Soltanian, H, Okada, H. Understanding genetic analysis for breast cancer and its implications for plastic surgery. Aesthet Surg J. 2008;28(1):85–91.
Van Dongen, JA, Voogd, AC, Fentiman, IS, et al. Long-term results of a randomized trial comparing breast-conserving therapy with mastectomy. European Organization for Research and Treatment of Cancer 10801 trial. J Natl Cancer Inst. 2000;92(14):1143–1150.