Chapter 225 Management of Traumatic Unilateral Jumped Cervical Facet Joint without Myelopathy
Closed Traction Reduction Then Surgery
Description and Mechanism
The most common activities associated with this type of injury include motor vehicle accidents, falls, and sports injuries. These injuries typically occur in the cervical spine due to the anatomy of the facet joints, which allow them to be very mobile. The mechanism of these injuries has been attributed to combined flexion and rotation. Some authors have postulated that the unilateral facet dislocation is mainly due to a flexion load with a rotational component.1–3 The rotational component of the injury is often evident on plain radiographs, with the superior segment of the spine rotated. The patient often appears to be looking to the side. The diagnostic accuracy is enhanced by a review of the anteroposterior projection on plain radiographs of the cervical spine. These often reveal malalignment or offset of the spinous processes. Unilateral cervical facet dislocation and fracture-dislocations of the cervical spine are relatively uncommon injuries that can result in spinal cord or nerve root injury. They represent approximately 12% to 16% of all cervical spine injuries.4 The goal of treatment is to prevent further injury, attempt to restore normal neurologic function, and reduce axial and radicular pain.
Diagnosis
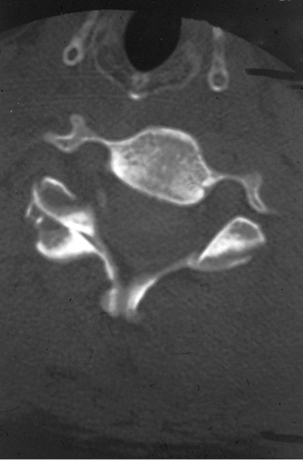
Plain radiographs demonstrate a characteristic appearance on the lateral radiograph, demonstrating anterolisthesis of the upper vertebra, usually measuring less than 25% of the anteroposterior dimension of the body (Fig. 225-1). This differs from bilateral facet dislocations, in which there commonly is a 50% subluxation (Fig. 225-2). On the anteroposterior view, the spinous processes above the level of the injury rotate to the same side as the dislocated facet. On the lateral radiograph, instead of the facets being in a superimposed position, they are seen individually and separately at the level of the injury. This creates the so-called bow-tie sign seen on CT. The lateral radiograph may also show increased distance between adjacent spinous processes at the level of the injury, which may be due to a disruption in the dorsal ligamentous complex. Oblique radiographs may reveal obstruction of the neuroforamen by the dislocated facet. A CT scan may reveal that the articular surface of the facet is observed to be without the appropriate articulating mate or that the appropriate articulating mate may be on the wrong side of the facet (the so-called naked facet sign or reversed hamburger bun sign) (Fig. 225-3).
Treatment
The primary goal in the treatment of this injury is to prevent further damage to the spinal cord and neural elements. The secondary goal is to relieve neural compression. This may be achieved by directly decompressing and removing the compressing elements or restoring the normal alignment of the cervical spine with distraction. The treatment of this injury with cervical traction was popularized by Crutchfield. It now includes attempted awake closed reduction with Gardner-Wells tongs5,6 (Fig. 225-4). The use of cervical traction is also referred to as closed reduction, because a skin incision is not made. Once the spine is aligned with a closed reduction, there remains a need to fuse the unstable segments, which requires an open procedure. Fixation and fusion can be performed either through an anterior or posterior approach.7 If closed reduction fails, open reduction may be achieved via either an anterior or posterior approach, followed by fixation and fusion.8–11 A preoperative MRI can provide information about the presence of a disc herniation and spinal cord compression. If disc herniation is present, a ventral decompression should be considered to decompress the spinal cord before manipulation. In addition, the spinal column can be manipulated and reduced through a ventral approach.
The initial weight used for traction should not be greater than 10 pounds (4.6 kg) to avoid overdistraction at the level of injury. The weight may be increased by 5- to 10-pound (2.3–4.6 kg) increments, usually at 10- to 15-minute intervals, until the desired alignment is achieved. It is important that with each increase in the traction weights, the patient is examined both neurologically and with plain radiographs. Under most circumstances, the total weight should not exceed 10 pounds per vertebral level. Gentle manual torsion toward the side of the jumped facets (straightening the head) may also aid reduction. In addition the use of paraspinal muscle relaxation using IV diazepam and/or narcotics may provide an easier reduction. The downside to muscle relaxants and narcotics is that they may mask results of the neurologic examination and as such should be used judiciously.
An initial attempt at closed reduction using skeletal traction is not without risk. The most serious complication of cervical traction and closed reduction is the retropulsion of disc fragments into the spinal canal and resultant spinal cord compression. Several reports of neurologic deterioration after closed reduction in the setting of concurrent disc herniation have been described.12 This deterioration, however, is rare and a permanent major neurologic deficit has not been documented with closed reduction in an awake, alert patient without distraction injuries. The aforementioned has led to a debate as to whether MRI should be obtained before closed reduction of dislocated facets.13 In addition, late instability is relatively common in patients treated with closed reduction alone without arthrodesis because of the concomitant presence of significant ligamentous disruption associated with these injuries. When traction is sufficient, the facets are usually distracted or perched and they reduce spontaneously.
The natural history of most spinal cord injuries after a unilateral jumped facet seems to consist of some improvement, with or without reduction—typically in the form of return of the impaired nerve root at the level of the injury or the next caudal level. In the past, controversy surrounding the best method of obtaining and maintaining reduction of unilateral facet dislocation was commonplace. Bohler,14 Crutchfield,15 and Ramadier and Bombart16 recommended that a patient with such an injury be treated with skull-tong traction, with progressively increased weights to obtain reduction. Failure of this procedure to achieve reduction was considered an indication for open reduction and posterior cervical fusion by Bohlman,9,10 Jacobs,11 and Bailey.8 In the past, Galibert,17 Evans,18 and Burke and Berryman19 described considerable success with gentle head and neck manipulation under general anesthesia in patients with unilateral facet dislocation. Bailey8 and Durbin20 condemned this act and pointed out that it was hazardous and should not be undertaken. Several studies have demonstrated that closed reduction with Gardner-Wells tongs is very difficult, because axial traction alone is often insufficient. In situations in which closed reduction is possible, internal or external stabilization should follow. Sonntag reported success in four patients with bilateral dislocated facets treated with reduction and external fixation.21 In contrast, some authors feel that a patient with an acute unilateral facet dislocation, with or without fracture of the superior articular facet, may have a stable injury and, as such, rarely require open reduction and fusion after a failed reduction with traction.3,22 Miller et al.23 have demonstrated biomechanically that increased weights are needed for reduction of a true unilateral dislocated facet joint without fracture as a result of the strength of the intact posterior longitudinal ligament. Unilateral facet dislocation, whether reduced or nonreduced, is an injury for which the indications for surgical stabilization remain somewhat cloudy. White et al.,24 Beatson,3 and Bohlman9,10 have written extensively on this subject and believe that patients who present with this type of injury with neurologic deficit have indications for reduction with surgical stabilization. Patients who are neurologically intact at the time of their injury pose more of a dilemma in terms of management strategies.
Once closed reduction has been achieved, operative stabilization should be undertaken. The use of internal fixation allows for more rapid mobilization of the patient, aids in maintaining stability, and reduces the potential for late deformity associated with closed reduction and immobilization alone.25 Beatson3 initially postulated that unilateral dislocated facet injuries that remained unreduced were stable injuries that did not displace further. Thus, they could be observed, with persistent root symptoms being the only indications for surgery. Cheshire26 did not agree with this theory, noting re-dislocation in patients who were treated with closed reduction and bracing. Surgical treatment of dislocated facets includes open reduction in patients in whom closed reduction failed and stabilization, both in patients who underwent closed reduction and in those treated with open reduction. Surgical treatment can be performed via a dorsal approach,20,26–31 a ventral approach,32–37 or a combined approach.36,38,39 Those who favor the ventral approach cite minimal blood loss, the familiarity of the region, and the technical ease associated with this approach as critical decision-making considerations.32–35 It is easier to decompress the spinal cord via a ventral approach if the offending agents are the dorsal vertebral osteophytes or disc fragments.27,36,38 Another indication for a ventral approach is the presence of lamina fractures.33 An argument can be made for a dorsal approach, because this can easily restore the posterior tension band in the spine, which is rendered inadequate as a result of disruption of the interspinous and supraspinous ligaments and the facet capsules. Also, if a neuroforamen needs to be decompressed, this can also be easily achieved via a dorsal approach. In situations in which the injury leads to disruption of the dorsal tension band and spinal cord impingement by a herniated disc or osteophyte, a combined ventral and dorsal approach may be warranted to achieve adequate decompression and stabilization of the injured regions, as advocated by Rizzolo et al.38 Ventral decompression and fusion may sometimes suffice in the management of these injuries. In patients who are myelopathic and require dorsal fusion, ventral decompression should be performed first. Andreshak and Dekutoski25 have postulated that any unilateral facet dislocation with or without a fracture should initially be managed with attempted closed reduction in the awake, alert, and cooperative patient. If the patient’s neurologic status changes during the reduction, the procedure should be aborted and an MRI should be obtained immediately. In a patient who is not cooperative or obtunded, an MRI should be considered before closed reduction is attempted. If reduction is unsuccessful, an MRI should be obtained to evaluate for a disc herniation. If present, an anterior cervical discectomy and fusion should be performed, but if no herniated disc is identified, a posterior open reduction and fusion should be considered.
Summary
The management of traumatic unilateral dislocated facets in the cervical spine has always been controversial because of the variability of management strategies among surgeons. It is, however, important to understand that the injury fundamentally results from disruption of the supraspinous and interspinous ligaments, as well as the facet capsule. This results in disruption of the posterior tension band. Occasionally, the injury may involve the vertebral body and the disc. Because the injury is primarily a result of a disruption of the dorsal elements, it can be argued that management strategies should primarily involve restoration of the posterior ligamentous complex via a dorsal approach. In myelopathic patients who have a disc herniation, ventral decompression should, perhaps, be performed before dorsal fusion and stabilization.
Aebi M., Mohler J., Zach G.A. Indications, surgical techniques and results of 100 surgically treated fractures and fracture dislocations of the cervical spine. Clin Orthop. 1986;203:244-257.
Braakman R., Vinken P.J. Unilateral facet interlocking in lower cervical spine. J Bone Joint Surg [Br]. 1967;49:249-257.
Crutchfield W.G. Skeletal traction in the treatment of injuries of the cervical spine. JAMA. 1954;155:29-32.
Evans D.K. Reduction of cervical dislocations. J Bone Joint Surg [Br]. 1961;43:552-555.
Holdsworth F.H. Fractures, dislocations, fracture-dislocations of the spine. J Bone Joint Surg [Br]. 1963;45:6-26.
Kwon B.K., Fisher C.G., Boyd M.C., et al. A prospective randomized controlled trial of anterior compared with posterior stabilization for unilateral facet injuries of the cervical spine. J Neurosurg Spine. 2007;7:1-12.
Savini R., Parisini P., Cervellati S. The surgical treatment of late instability of flexion rotation injuries in the lower cervical spine. Spine (Phila Pa 1976). 1987;12:178-182.
1. Holdsworth F.H. Fractures, dislocations, fracture-dislocations of the spine. J Bone Joint Surg [Br]. 1963;45:6-26.
2. Roaf R. A study of the mechanics of spinal injuries. J Bone Joint Surg [Br]. 1960;12:810-823.
3. Beatson T.R. Fracture and dislocations of the cervical spine. J Bone Joint Surg [Br]. 1963;45:21-35.
4. Berquist T.H., Cabanela M.E. The spine. In: Berquist T.H., editor. Imaging of orthopedic trauma and surgery. Philadelphia: WB Saunders; 1986:121-124. 144–154
5. Crutchfield W.G. Skeletal traction in treatment of injuries to the cervical spine. JAMA. 1954;155:29-32.
6. Crutchfield W.G. Skeletal traction for dislocation of the cervical spine: report of a case. South Surg. 1993;2:156.
7. Kwon B.K., Fisher C.G., Boyd M.C., et al. A prospective randomized controlled trial of anterior compared with posterior stabilization for unilateral facet injuries of the cervical spine. J Neurosurg Spine. 2007;7:1-12.
8. Bailey R.W. Fractures and dislocations of the cervical spine. Surg Clin North Am. 1961;41:1357-1366.
9. Bohlman H.H. Pathology and current treatment concepts of cervical spine injuries. Instructional Course Lectures, The American Academy of Orthopaedic Surgeons. St Louis: C.V. Mosby, 1972;vol 21. 108–115
10. Bohlman H.H. Acute fractures and dislocations of the cervical spine. J Bone Joint Surg [Am]. 61, 1979. 1119–1942, 1979
11. Jacobs B. Cervical fractures and dislocations (C3-C7). Clin Orthop. 1975;109:18-32.
12. Robinson R.A., Southwick W.O. Surgical approaches to the cervical spine. Instructional Course Lectures: The American Academy of Orthopaedic Surgeons. St Louis: C.V. Mosby, 1960;vol 17. pp 299–330
13. Doran S.E., Papadopoulos S.M., Ducker T.B., Lillehei K.O. Magnetic resonance imaging documentation of coexistent traumatic locked facets of the cervical spine and disc herniation. J Neurosurg. 1993;79:341-345.
14. Bohler L. Die Technik doc knochenbruchbehandlung. Vierk Auflage. Wien: Wilhelm Maudrich; 1933.
15. Crutchfield W.G. Further observations on the treatment of fracture-dislocation of the cervical spine with skeletal traction. Surg Gynecol Obstet. 1936;63:513-517.
16. Ramadier J.O., Bombart M. Fractures et luxations du rachis cervical sans lesions medullaries 2eme partie. Lesions des 5 dernieres vertebres cervicales. Rev Chir Orthop. 1964;50:3.
17. Galibert P. Une methode de traitment des luxations du rachis cervical compliquees de lesions medulaires ou radiculaires. Lille Chir. 1962;17:172-180.
18. Evans D.K. Reduction of cervical dislocations. J Bone Joint Surg [Br]. 1961;43:552-555.
19. Burke D.C., Berryman D. The place of closed manipulation in the management of flexion-rotation dislocations of the cervical spine. J Bone Joint Surg [Br]. 1971;53:165-182.
20. Durbin F.C. Fracture dislocation of the cervical spine. J Bone Joint Surg [Br]. 1957;39:23-38.
21. Sonntag V. Management of bilateral locked facets of the cervical spine. Neurosurgery. 1981;8:150-152.
22. Braakman R., Vinken P.J. Unilateral facet interlocking in lower cervical spine. J Bone Joint Surg [Br]. 1967;49:249-257.
23. Miller L.S., Cotler H.B., DeLucia F.A., et al. Biomechanical analysis of cervical distraction. Spine. 1987;12:831-837.
24. White A.A., Southwick W.O., Panjabi M.M. Clinical instability in the lower cervical spine: a review of past and current concepts. Spine (Phila Pa 1976). 1976;1:15-27.
25. Andreshak J.L., Dekutoski M.B. Management of unilateral facet dislocations: a review of the literature. Orthopedics. 1997;20(10):917-926.
26. Chesire D.J. The stability of the cervical spine following the conservative treatment of fracture and fracture dislocations. Paraplegia. 1969;7:193-203.
27. Bohlman H.H. Acute fractures and dislocations of the cervical spine. Analysis of 300 hospitalized patients and review of the literature. J Bone Joint Surg [Am]. 1979;61:1119-1142.
28. Bucholz R., Cheung C. Halo vest versus spinal fusion for cervical injury: evidence from an outcome study. J Neurosurg. 1989;70:884-892.
29. Beyer C.B., Cabanela M.E. Unilateral facet dislocations and fracture-dislocations of the cervical spine: a review. Orthopedics. 1992;15:311-315. [erratum in Orthopedics 15:545, 1992]
30. Beyer C.A., Cabanela M.E., Berquist T.H. Unilateral facet dislocations and fracture dislocations of the cervical spine. J Bone Joint Surg [Br]. 1991;73:977-981.
31. Shapiro S.A. Management of unilateral locked facet of the cervical spine. Neurosurgery. 1993;33:832-837.
32. Argenson C., Lovet J., Sanouiller J.L., de Peretti F. Traumatic rotatory displacement of the lower cervical spine. Spine (Phila Pa 1976). 1998;13:767-773.
33. Lukhele M. Fractures of the vertebral lamina associated with unifacet and bifacet cervical spine dislocations. South Afr J Surg. 1994;32:112-114.
34. Goffin J., Plets C., Van den Bergh R. Anterior cervical fusion and osteosynthetic stabilization according to Caspar: a prospective study of 41 patients with fractures and/or dislocations of the cervical spine. Neurosurgery. 1989;25:865-871.
35. De Oliveira J.C. Anterior reduction of interlocking facets in the lower cervical spine. Spine (Phila Pa 1976). 1979;4:195-202.
36. Cloward R.B. Treatment of acute fractures and fracture-dislocations of the cervical spine by vertebral body fusion. A report of 11 cases. J Neurosurg. 1961;18:201-209.
37. Savini R., Parisini P., Cervellati S. The surgical treatment of late instability of flexion rotation injuries in the lower cervical spine. Spine (Phila Pa 1976). 1987;12:178-182.
38. Rizzolo S.J., Vaccaro A.R., Cotler J.M. Cervical spine trauma. Spine (Phila Pa 1976). 1994;19:2288-2298.
39. Aebi M., Mohler J., Zach G.A. Indications, surgical techniques and results of 100 surgically treated fractures and fracture dislocations of the cervical spine. Clin Orthop. 1986;203:244-257.
Open Reduction
Open reduction should be strongly considered in patients with an additional cervical injury rostral to the unilateral jumped facet. Overdistraction at the rostral site of injury and resultant neurologic deterioration may occur with closed traction. Traction resulting in neurologic deterioration secondary to a missed rostral injury is a well-known complication that has been previously reported in the literature.1,2 This would most likely occur with a rostral distraction injury such as a type II atlanto-occipital dislocation injury or an Effendi type II hangman’s fracture (traumatic spondylolisthesis of the axis). The safest treatment for these patients is open reduction and stabilization. When managing these patients, the surgeon needs to formulate a surgical strategy that addresses both injuries. For example, a patient with an unstable hangman’s fracture and a unilateral C5-6 jumped facet could undergo anterior cervical discectomies and reduction/fusion at C2-3 and at C5-6. A patient with atlanto-occipital dislocation and a unilateral C5-6 jumped facet would probably be best served with posterior reduction and occiput-to-C6 instrumented fusion.
Open reduction should also be considered in patients who cannot be examined during closed reduction. This includes unconscious patients, intoxicated patients, developmentally delayed patients who cannot communicate, and aphasic patients. In these situations, the patient is unable to inform the physician of an evolving neurologic deficit. The physician also may not be able to perform a proper neurologic examination during the reduction process because of the patient’s inability to cooperate. In this situation, an MRI should be considered. If the MRI demonstrates a large herniated disc in close proximity to or compressing the thecal sac at the level of the jumped facet, a ventral decompression may be warranted. Reduction and stabilization can be achieved via a ventral approach by using an interbody spreader or by using the vertebral body post technique (see Chapter 94). The patient and family, however, should be counseled that a combined ventral/dorsal approach would be necessary if ventral reduction cannot be achieved.
1. Rosenfeld J.F., Vaccaro A.R., Albert T.J., et al. The benefits of early decompression in cervical spinal cord injury. Am J Orthop. 1998;27:23-28.
2. Schaefer D.M., Flanders A., Northrup B.E., et al. Magnetic resonance imaging of acute cervical spine trauma. Spine (Phila Pa 1976). 1989;14:1090-1095.