CHAPTER 53 Management of Lost Pronosupination
Pronosupination is important in most activities of daily living. A loss of forearm rotation may be compensated by internally or externally rotating the humerus with the elbow semiextended, but this implies a high risk of developing degeneration of the rotator cuff. Without pronosupination, numerous common tasks, such as pouring water from a pitcher into a glass, or fastening a brassiere, are extremely difficult. A forearm with limited pronosupination is a substantial handicap, almost as serious as an unstable distal radioulnar joint (DRUJ).
For a full forearm rotation, not only do proximal and distal radioulnar joints need to be well aligned, with matching lengths and congruent cartilages, but also the soft tissue stabilizing structures must function properly.1–3 Pronosupination is a multifactorial phenomenon that can be affected in many different ways, the more common being distal radius misalignment, radioulnar length discrepancy, joint incongruity, and soft tissue (capsule or muscle or both) contracture.4
Frequently, the loss of supination is secondary to a dorsally malunited distal radial fracture. In such instances, if the triangular fibrocartilage complex (TFCC) has been stretched out or avulsed off the basistyloid fovea, the ulnar head is forced into a dorsally subluxed position relative to the sigmoid notch. Such joint incongruity prevents the normal combination of joint spinning and gliding necessary for a full forearm rotation. Treatment in these cases consists of a radial corrective osteotomy.5
In other circumstances, the ulna may be excessively long as a result of trauma (shortened distal radial fracture) or a congenital defect, and may impinge the lunate during supination and wrist extension, producing pain. Such an abutment may explain a reduced range of forearm rotation. In these cases, any form of ulnar length reduction (i.e., ulnar shortening osteotomy or wafer procedure) is mandatory.6
If the lack of rotation is due to joint incongruity secondary to trauma or cartilage degeneration, many different options exist2: (1) total ulnar head resection,7 (2) “matched ulna” resection,8 (3) hemiresection and fibrous interposition,9 (4) DRUJ fusion plus creation of a metaphyseal pseudarthrosis,10 (5) ulnar head implants,11,12 and (6) total DRUJ prosthesis.13 All of these options are discussed elsewhere in this book, so they are not covered here. This chapter concentrates on the loss of forearm rotation secondary to soft tissue (capsular or muscle or both) contracture.
Pathomechanics
Supination Constraints
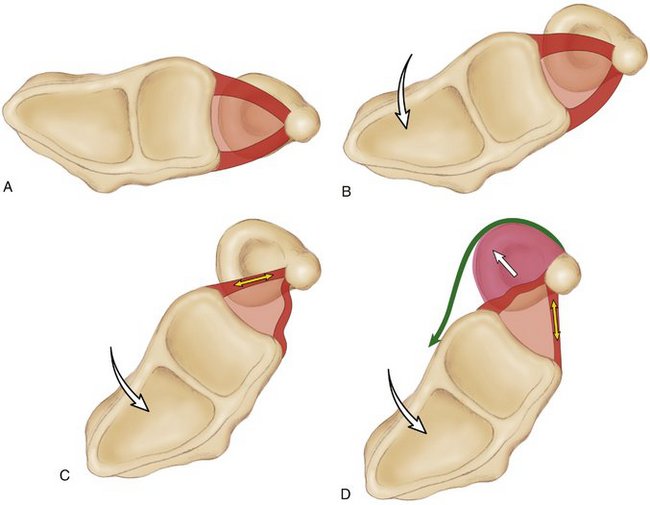
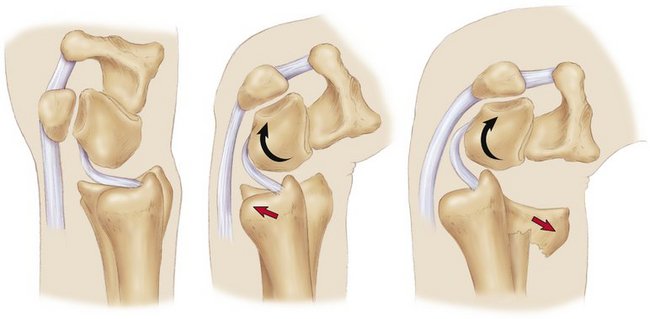
As the radius rotates from neutral toward supination, very few changes in ligament tension appear in either the palmar or the dorsal radioulnar ligaments. The horizontal portion of the TFCC, consisting of the articular disc (central zone) and the two peripheral radioulnar ligaments, moves as a unit (Fig. 53-1A and B).3,14 Tension in the palmar radioulnar ligament does not increase until a certain degree of supination is reached (Fig. 53-1C). At this point, the distance between the two ends of the ligament (fovea and palmar corner of the radius) starts increasing until the palmar radioulnar ligament is fully taut, at about 70 degrees of supination.14 If the palmar capsule was not elastic, that would be the limit of supination. The capsule is very lax, however,15 and allows some degree of dorsal subluxation of the radius, with the ulnar head displacing palmarward, decreasing tension in the anterior radioulnar ligament (Fig. 53-1D). This decrease in tension allows further supination up to about 80 degrees, until the dorsal radioulnar ligament becomes fully taut.1
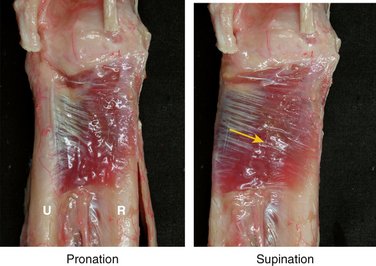
An important dynamic control of the final stages of supination is the pronator quadratus, which in supination becomes stretched and promotes coaptation of the joint, avoiding its subluxation (Fig. 53-2).3,16,17 The palmar radioulnar ligament can be thought of as the primary stabilizer of the early stages of supination,1 whereas the dorsal radioulnar ligament,14 the palmar capsule,15 and the pronator quadratus muscle16,17 are secondary stabilizers avoiding dorsal dislocation of the radius relative to the ulna.
Pronation Constraints
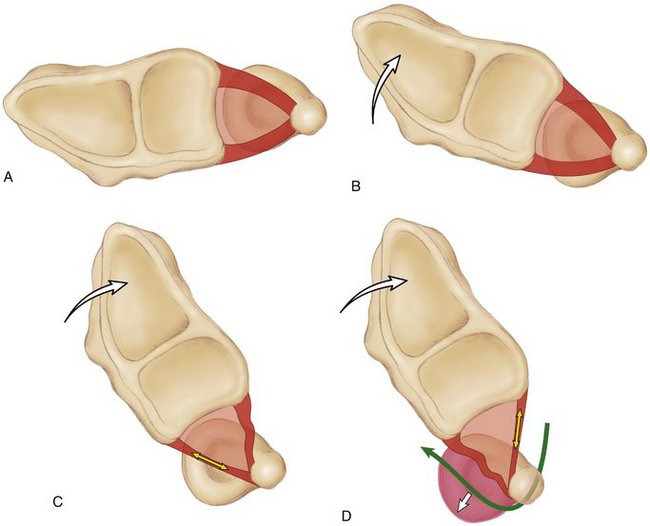
A similar phenomenon occurs during pronation: No substantial changes in tension develop in the two radioulnar ligaments until a certain degree of pronation is achieved (Fig. 53-3A, B). At about 60 degrees of pronation, the dorsal ligament becomes maximally taut (Fig. 53-3C).14 This would stop pronation if it were not for the elastic dorsal capsule, which allows some palmar subluxation of the radius relative to the ulna. As the ulna glides dorsally, there is increasing tensioning of the anterior radioulnar ligament and the dorsal capsule, the two ultimate constraints of pronation (Fig. 53-3D).1
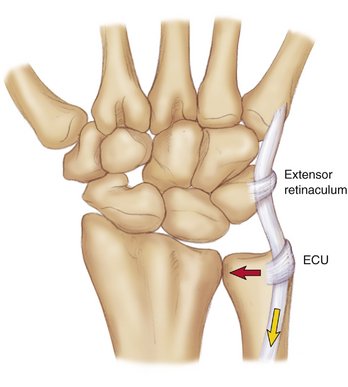
The extensor carpi ulnaris muscle has a similar role to that of the pronator quadratus in that it is an effective dynamic stabilizer of the DRUJ during pronation. As emphasized by Spinner and Kaplan,18 the extensor carpi ulnaris tendon is maintained in a close relationship with the head of the ulna by a fibrous tunnel, independent from the rest of the extensor retinaculum. Because of this, at full pronation, the extensor carpi ulnaris tendon lies medial to the ulnar head and promotes coaptation of this bone against the dorsal rim of the sigmoid cavity, maximizing stability (Fig. 53-4).3,18 The dorsal radioulnar ligament can be thought of as the primary stabilizer of the early stages of pronation,14 whereas the palmar radioulnar ligament,1 the dorsal capsule,15 and the extensor carpi ulnaris muscle18 are secondary stabilizers avoiding palmar dislocation of the radius relative to the ulna.
Clinical Forms of Soft Tissue Contractures around the Distal Radioulnar Joint
Contractures around the DRUJ may cause three forms of forearm limitation: (1) loss of pronation, (2) loss of supination, and (3) combined pronation and supination loss. The third form of forearm limitation, combining pronation and supination losses, usually falls into the category of intra-articular stiffness (arthrofibrosis), and often results from complex trauma or inflammatory disease generating intra-articular cartilage destruction and invasion by scarring fibrotic tissue.2 This is a difficult condition to treat effectively and most often requires a salvage intervention.4 It is rarely seen after a common distal radial fracture. If releasing an arthrofibrotic joint is believed to be necessary, however, a double palmar and dorsal approach following the guidelines proposed by Kleinman and Graham15 is recommended (see later).
Loss of Pronation
Of the four structures the scarring or contracture of which may theoretically affect pronation (see Fig. 53-3D), only the dorsal capsule is shown to be directly involved in the rare cases where there is truly an isolated lack of pronation owing to soft tissue contracture.15 The dorsal capsule may disrupt, lose its elasticity, and become thick in several ways; most often, this occurs as the consequence of an extra-articular, palmarly angulated distal radial fracture (Smith type), or in Galeazzi’s fracture-dislocation.4 If the fracture is not properly reduced and stabilized, and particularly if the forearm is immobilized in an above-elbow cast for too long, these injuries may induce a deficit of pronation. Plate fixation and early mobilization of these types of fractures is common practice because the need for a secondary dorsal capsular release is almost anecdotic.
Permanent scar retraction of a partial injury to the radioulnar ligaments producing limitation of forearm rotation is very rare. When they fail, these ligaments tend to avulse or disrupt creating instability, but seldom stiffness.19 Detaching the radioulnar ligaments to achieve increased pronosupination should be considered only exceptionally.
Extensor carpi ulnaris tendinitis may result in muscle contracture and slight limitation of pronation.20 Reduction of forearm rotation is not static, but most often the result of pain produced by the synovitic tendon when stretched during pronation. Proper treatment of the condition (e.g., splinting, glucocorticoid injections, eventually a synovectomy) is all that is needed to recover full pronosupination.
Loss of Supination
Post-traumatic palmar capsular thickening inducing a supination deficit is common.15 Distal radial fractures with mild dorsal displacement are particularly prone to create DRUJ capsular defects in the palm, which may eventually cause this problem. The reason for it is as follows.
The hyperextended carpus pulls the ulnar head anteriorly by means of the strong ulnocarpal ligaments (Fig. 53-5).3 As the distal radius displaces dorsally, a shear stress in the DRUJ is created. If the TFCC, including the ulnocarpal ligaments, does not fail, the ulnar head promotes tearing of the palmar capsule in its attempt to sublux palmarly relative to the dorsally angulated distal radius. If, in addition, there is a supination moment involved in the injury, the fully stretched pronator quadratus muscle may be unable to resist the palmar push of the ulna, and may sustain substantial elongation. Such muscle injury would not have major consequences, however, if not for the fact that this muscle is contained in its own small compartment,21,22 which the fracture fills with abundant hematoma, creating the conditions for a localized compartment syndrome.23,24 Increased pressure on the muscle may seriously affect its contractability, inducing its later fibrotic retraction and subsequent limitation of supination.
Management of Distal Radioulnar Joint Soft Tissue Contracture
The management of a patient with reduced pronosupination depends on the chronicity of the problem and the location of the structures involved. As stated earlier, if there is bone deformity or joint incongruity, this needs to be resolved first. No soft tissue release would ever correct a bone-related stiffness problem. If this problem has been ruled out, an aggressive supervised therapy program is always recommended. The aim is to recover progressively the elasticity of all retracted structures through deep massage, gentle passive mobilization, and application of passive splints with progressive rotation angles. Dynamic splinting also may be considered. Failing this, surgery is indicated.
Distal Radioulnar Joint Capsular Release
A volar approach to the DRUJ capsule is usually performed through a 5-cm longitudinal or zigzag incision along the medial border of the flexor carpi ulnaris tendon. Alternatively, the joint may be approached through a longitudinal incision along the interval between the ulnar neurovascular bundle and the flexor digitorum tendons (see Fig. 53-6D). In the first case, a careful dissection and protection of the dorsal branch of the ulnar nerve is mandatory. Gentle retraction of the neurovascular bundle allows exposure of the deep fascia that covers the pronator quadratus muscle. Complete fasciectomy of the area covering the DRUJ is recommended. Excision of the volar capsule is accomplished, as described by Kleinman and Graham,15 by first incising its insertion on the radius. A second transverse incision paralleling the proximal margin of the palmar edge of the TFCC is then made. The proximal border of the capsule is cut, circumscribing the area of the ulna covered by cartilage. With this, a volar “silhouette” resection of the DRUJ capsule is excised, while protecting the articular surfaces of the distal ulna and sigmoid notch of the radius (see Fig. 53-6F).15 At this point, if the only problem is capsular thickening, full passive supination should be obtained. If there is still a lack of supination, the procedure needs to address the associated pronator quadratus muscle problem.
When there is a true pronator quadratus muscle contracture owing to muscle disruption, its distal and ulnar fibers usually appear whitish and fibrotic (see Fig. 53-6E). By contrast, when contracture is the consequence of a localized compartment syndrome, the entire muscle looks fibrotic and does not contract when stimulated with the scalpel.23,24 In the first instance, the superficial belly of the muscle is detached off the ulna, and its fibrotic portion is excised. In the second case, the entire muscle needs to be released and extracted.
Aside from capsular and muscle contracture, the joint may have developed arthrofibrosis (intra-articular adhesions) requiring further arthrolysis (see Fig. 53-6G). A blunt Freer elevator is used to unblock the joint until full passive supination is achieved, and the ulnar head can be passively displaced back and forth on the sigmoid notch. Detachment of the foveal insertion of the TFCC is seldom indicated. If liberation of all intra-articular adhesions does not allow full forearm rotation, a dorsal approach is preferred.
The dorsal DRUJ capsule is approached by retracting the extensor digiti quinti from the fifth extensor compartment.25 An ulnar retinacular flap is elevated from the underlying dorsal capsule. The thickened and adhesive capsule is excised following the “silhouette” method of capsulectomy described for the palmar side.15 After passive intraoperative assessment of forearm rotation and translation of the ulnar head within physiological limits, the dorsal retinaculum is repaired, and all wounds are closed. A bulky compression dressing with an above-elbow supination splint is placed for 1 week, after which patients are encouraged to pursue active hand therapy. Night splints in full supination may be used eventually.
Results
We have recently reviewed six patients (five women and one man, average 36 years old [range 20 to 51 years old]) who had undergone a DRUJ capsular release for a loss of forearm rotation. Three of the six patients had sustained mildly displaced fractures of the distal radius, all having been treated nonoperatively in a cast. One had had a radial head fracture treated with internal plate fixation, one had a direct blow to the palmar surface of his wrist, just proximal to the palmar crease, and the last one had an episode of intense wrist pain after a racket ball game. All patients with a radial fracture had acceptable radial length and congruent articular surfaces at the DRUJ (see Fig. 53-6B).
The average interval between injury and surgery was 16 months (range 4 to 30 months). At an average follow-up of 15 months (range 7 to 52 months), patients were evaluated for pain relief, range of motion, and grip strength. Pain relief at rest was obtained in all patients, with two complaining of mild discomfort during strenuous activity. All patients resumed their normal activities except one who had to downgrade the strength level of her job. Average ranges of forearm rotation at follow-up were for supination 68 degrees (84% of contralateral) and pronation 80 degrees (95%). Average grip strength relative to the contralateral normal side improved from 45% to 65%. A case example of the technique and the results obtained is shown in Figure 53-6.
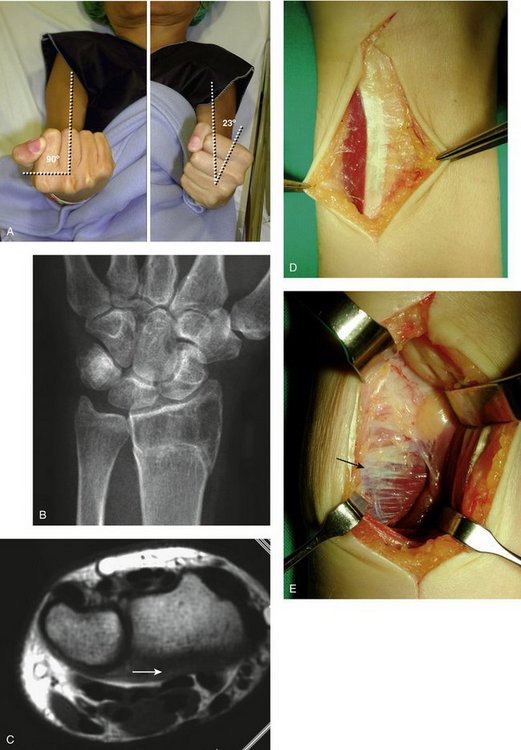
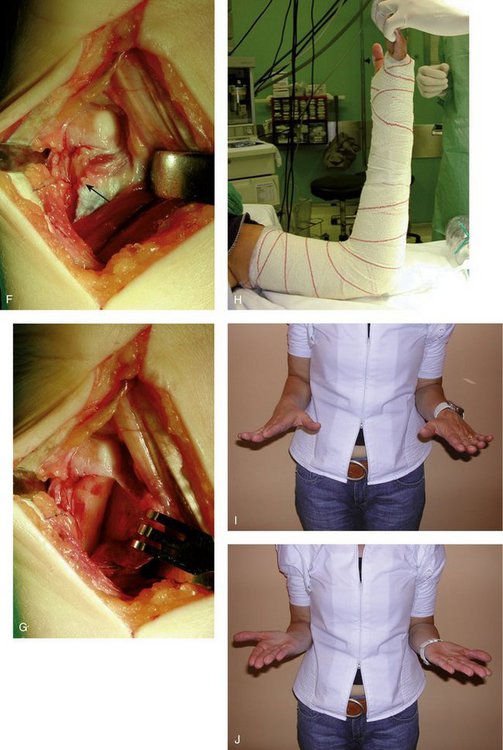
FIGURE 53-6 Illustrative case of a 52-year-old woman who presented with lack of supination 6 months after a mildly displaced distal radius fracture treated conservatively. The patient recalled having had intense pain at the palmar aspect of the wrist after the fracture (possibly pronator quadratus compartment syndrome). A, Clinical photographs of the maximum range of active supination that was present before surgery. Passive motion was identically reduced. B, Neither joint incongruity nor length discrepancy could be blamed for the lack of rotation. C, Transverse magnetic resonance imaging showed retraction of the pronator quadratus muscle. D, The joint was approached palmarly along the lateral border of the flexor carpi ulnaris tendon, taking care to protect the ulnar neurovascular bundle that courses behind the tendon. E, Appearance of the pronator quadratus muscle, with a whitish distal medial corner (arrow) as a result of fibrosis.F, Despite excision of the volar distal radioulnar joint capsule and detachment of the pronator quadratus muscle (arrow), supination was still blocked. G, Elevation of the pronator quadratus muscle disclosed the existence of fibrotic bands within the joint, excision of which allowed recovery of full supination. H, The arm was immobilized in an above-elbow supination splint for 1 week followed by an active program of supervised physiotherapy. In this case, it took 5 months to obtain full active pronosupination. I and J, At 1 year, the range of forearm rotation was still normal and painless.
Our results are similar to the results published by Kleinman and Graham in 1998.15 In their series, six patients with recalcitrant limited forearm rotation required a palmar capsulectomy, whereas three had a combined palmar and dorsal capsulectomy. Their range of forearm rotation improved from an average 54 to 21 degrees of pronation-supination to 82 to 72 degrees at follow-up.
1. Hagert CG. The distal radioulnar joint in relation to the whole forearm. Clin Orthop. 1992;275:56-64.
2. Lichtman DM, Ganocy TK, Kim DC. The indications for and techniques and outcomes of ablative procedures of the distal ulna. Hand Clin. 1998;14:265-277.
3. Garcia-Elias M. Soft-tissue anatomy and relationships about the distal ulna. Hand Clin. 1998;14:165-176.
4. Bowers WH. Instability of the distal radioulnar articulation. Hand Clin. 1991;7:311-327.
5. Prommersberger KJ, Van Schoonhoven J, Lanz UB. Outcome after corrective osteotomy for malunited fractures of the distal end of the radius. J Hand Surg. 2002;27:55-60.
6. Chun S, Palmer AK. The ulnar impaction syndrome: Follow-up of ulnar shortening osteotomy. J Hand Surg [Am]. 1993;18:46-53.
7. Darrach W. Forward dislocation at the inferior radio-ulnar joint, with fracture of the lower third of the shaft of the radius. Ann Surg. 1912;56:801-802.
8. Watson HK, Gabuzda GM. Matched distal ulnar resection for posttraumatic disorders of the distal radioulnar joint. J Hand Surg. 1992;17:724-730.
9. Bowers WH. Distal radioulnar joint arthroplasty: the hemiresection-interposition technique. J Hand Surg. 1985;10:169-178.
10. Kapandji IA. The Kapandji-Sauvé operation: its techniques and indications in non-rheumatoid diseases. Ann Chir Main. 1986;5:181-193.
11. van Schoonhoven J, Fernandez DL, Bowers WH, et al. Salvage of failed resection arthroplasties of the distal radio-ulnar joint using a new ulnar head prosthesis. J Hand Surg [Am]. 2000;25:438-446.
12. Berger RA, Cooney WP. Use of an ulnar head endoprosthesis for treatment of an unstable distal ulnar resection: review of mechanics, indications, and surgical technique. Hand Clin. 2005;21:603-620.
13. Scheker LR, Babb BA, Killion PE. Distal ulnar prosthetic replacement. Orthop Clin North Am. 2001;30:365-376.
14. Schuind F, An KN, Berglund L, et al. The distal radioulnar ligaments: a biomechanical study. J Hand Surg [Am]. 1991;16:1106-1114.
15. Kleinman WB, Graham TJ. The distal radioulnar joint capsule: clinical anatomy and role in posttraumatic limitation of forearm rotation. J Hand Surg [Am]. 1998;23:588-599.
16. Johnson RK. Stabilization of the distal ulna by transfer of the pronator quadratus origin. Clin Orthop. 1992;275:130-132.
17. Stuart PR. Pronator quadratus revisited. J Hand Surg [Br]. 1996;21:714-722.
18. Spinner M, Kaplan EB. Extensor carpi ulnaris: its relationship to the stability of the distal radioulnar joint. Clin Orthop. 1970;68:124-129.
19. Szabo RM. Distal radioulnar joint instability. J Bone Joint Surg. 2006;88:884-894.
20. Allende C, Le Viet D. Extensor carpi ulnaris problems at the wrist—classification, surgical treatment and results. J Hand Surg. 2005;30:265-272.
21. Sotereanos DG, McCarthy DM, Towers JD, et al. The pronator quadratus: a distinct forearm space? J Hand Surg [Am]. 1995;20:496-499.
22. Gerber A, Masquelet AC. Anatomy and intracompartmental pressure measurement technique of the pronator quadratus compartment. J Hand Surg [Am]. 2001;26:1129-1134.
23. Summerfield SL, Folberg CR, Weiss APC. Compartment syndrome of the pronator quadratus: a case report. J Hand Surg [Am]. 1997;22:266-268.
24. Schumer ED. Isolated compartment syndrome of the pronator quadratus compartment: a case report. J Hand Surg [Am]. 2004;29:299-301.
25. Garcia-Elias M, Smith DE, Llusá M. Surgical approach to the triangular fibrocartilage complex. Tech Hand Upper Extrem Surg. 2003;7:134-140.