Management of clinical problems of children with cerebral palsy*
CLAUDIA R. SENESAC, PT, PhD, PCS
After reading this chapter the student or therapist will be able to:
1. Identify the parameters of the diagnosis of cerebral palsy including motor, family, and psychosocial components.
2. Analyze the multifaceted aspects of the clinical problem and appreciate a multifaceted approach to evaluation and treatment.
3. Analyze treatment strategies and their application to clinical problems.
4. Identify and critique current research for the pediatric client with cerebral palsy.
5. Identify the therapist’s role in the treatment of the child with cerebral palsy, with family involvement, in different settings, and with other health professionals.
Overview
Historical perspective
Cerebral palsy is a misnomer at best. Little1 suggested the name in the mid-1800s, but there is still no established direct relationship between the identifiable state of the brain and the distortions in posture and movement control that we are able to observe in the individual.2,3 The condition is not always evident at birth, although the work of Prechtl4 statistically supports the possibility of a link between the quality of spontaneous movements in the first months of life and later difficulties in coordinated movement expression. In only a small number of children has a specific lesion been identified that corresponds to the observed motor responses of the child, and this elite group includes children with porencephaly and other early developmental malformations of the brain. Whether there is a biochemical element in the brain of a child that distorts the actual motor learning process has not been established. There is a shocking variability in the age at which intervention is initiated for individual children and a wide variety of programs that do not necessarily take into account the current information available from clinical studies on efficient motor development and brain function. This confusion has led us astray in understanding the process of movement and postural distortion that characterizes children who carry the label of “cerebral palsy.”
Historically, the evolution of diagnosis and treatment intervention or management is clear and relates to the recognition of the special needs of this minority of society. The British physician Little identified the condition on the basis of observable characteristics of movement and posture, or—in other words—the external features of the condition, so the initial efforts at remediation fell to orthopedists such as Deaver and Phelps.3,5,6 Deaver placed importance on external bracing that was periodically reduced in the hope that the child would take over control of increasing parts of his or her own body.5 Phelps used bracing and surgery and was a significant force in obtaining schooling for these children in the United States.6 He pointed out that they did not belong in academic classes with children diagnosed as retarded or mentally handicapped and that children with cerebral palsy should be exposed to a traditional academic curriculum. In his Children’s Rehabilitation Institute in Reisterstown, Maryland, he also advocated restriction of a more functional limb to encourage use of the one less used, particularly in work with the upper extremities.
In the 1950s and 1960s there simultaneously emerged new theories of neuromotor behavior that redefined the clinical characteristics of cerebral palsy and permitted clinicians to orient their intervention strategies to the principles of motor development and motor learning. Kabat in conjunction with Knott introduced proprioceptive neuromuscular facilitation (PNF), which was applied to children with movement disorders and to adults with a history of trauma.7 The use of diagonal patterns of movement in this approach changed the customary postures of the child and introduced more functional movement patterns in logical learning sequences. Physical and occupational therapist Margaret Rood added the more specific sensory components of ice and light quick brushing of the skin surface to guide the desired motor response.8 She spoke of the need to focus attention on both “heavy work” and “light work” during the early development of movement skills. These terms referred to the central body moving over limb support and limb movement with central stability. Bobath was working in London at this same time and observed the need to have a dynamic interaction between stability and mobility, after finding that inhibition of the reflexive movements was not sufficient to change the functional outcome of the child with cerebral palsy.9 They pointed out that the areas of the child’s body that appeared to be spastic changed when the body was placed in a different relationship to gravity. This observation held up for reexamination the prevailing view of the time, namely, that spasticity existed in a tendon or muscle, a specific structure.
When the birth process is prolonged for any of many reasons, the physiological timing of these changes is interrupted. Unique combinations of pressure may make it difficult for the membranous structures to maintain their structural alignment. That lack of structural alignment may persist long after birth and affect future movement and development. Rapid changes of pressure, with minor misalignments of the head and body during the birth process, result in sufficient trauma to affect the nervous system and the delicate fascia and in a small percentage of infants to affect the expression of spontaneous movements. In the majority of healthy infants born at term the spontaneous movements seem to assist in the activation of the central body and the limbs so that physiological changes in the fascia are sufficient to permit a typical expression of developmental movement responses after birth. Body movement and respiration are coordinated with the infant’s physiological rhythms in this initial adaptation to the world of gravity. With complications of the pregnancy or the birth process, these spontaneous movements that are so easily made by the healthy infant become laborious and sometimes impossible, affecting motor actions, postural mechanisms, and the basic physiological rhythms. Cerebral palsy is a heterogeneous collection of clinical syndromes, not a disease or pathological or etiological entity.10 Little described cerebral palsy as “a persistent disorder of movement and posture appearing early in life and due to a developmental nonprogressive disorder of the brain.”3 Current definitions have reiterated that atypical execution of movement and interference with postural mechanisms are the key characteristics of this nonprogressive disorder affecting the developing brain.10,11
Cerebral palsy affects the total development of the child. The primary disorder is of motor execution, but common associated dysfunctions include sensory deficits (hearing or vision); epilepsy; learning disabilities; cognitive deficits; emotional, social, and behavioral problems; and speech and language disorders. The degree of severity varies greatly from mild to moderate to severe.10–12
Diagnostic categorization of the characteristics of cerebral palsy
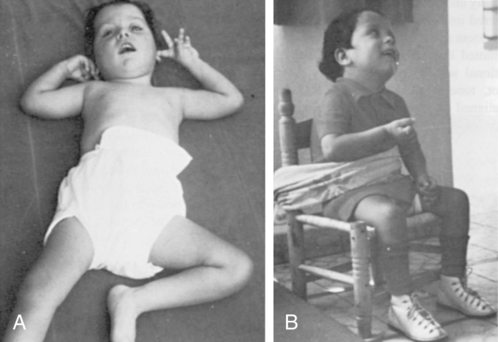
The clinician must be aware that the categorization of cerebral palsy is based on descriptions of observable characteristics; thus, it is a symptomatic description. The hypertonus of spasticity prevents a smooth exchange between mobility and stability of the body. Constriction of respiratory adaptability occurs with poor trunk control. Incrementation of postural tone occurs with an increase in the speed of even passive movement, and clonus may occur in response to sudden passive movement. Although diagnostic terms reflect the distribution of excessive postural tone, the entire body must be considered to be involved. Spasticity, by nature, involves reduced quantity of movement, which makes its distribution easier to identify. Recruitment of the corticomotor neuron pool is affected in the presence of spasticity, and therefore timing issues result in the poor grading of agonists and antagonists.13,14 There is also a risk of reduction in the range of limb movements over time when therapy does not include active adaptation in end ranges and organization of postural transitions.15 This category (spasticity) has the highest occurrence of cases of cerebral palsy.16 There are several spastic types of cerebral palsy that require clarification. Spastic diplegia implies that the lower extremities are more involved than the upper extremities but could manifest with varying degrees of hand function, and often the involvement is asymmetrical.14 Hemiplegia displays involvement of one side of the body and can manifest itself with the arm involved more than the leg or the leg involved as much as or more than the arm.10 Quadriplegia, as the term implies, involves the entire body.10
Dyskinetic syndromes, which include athetosis and dystonic types of cerebral palsy, are characterized by involuntary movements. The term dyskinetic is commonly used with children who lack posture and axial and trunk coactivation. The excessive peripheral movement of the limbs occurs without central coactivation. Dystonic types of cerebral palsy are dominated by tension, and athetosis usually has a hypotonic base or underlying tone. Dyskinetic syndromes may occur with greater involvement in particular extremities, although the condition most often interferes with postural stability as a whole. When pathological or primitive reflexes are used to accomplish movement, there is a difficulty with midline orientation. Dyskinetic distribution of postural tone is changeable in force and velocity, particularly during attempted movement by the individual. Midrange control is limited if present at all, and frequently end ranges of motion are used to accomplish a motor task.10 For these reasons, these children have a reduced risk for contractures over time.
Hypotonicity is another category of cerebral palsy, but it may also mask undiagnosed degenerative conditions (see Chapter 13). Recent reports suggest that “pure hypotonia” is not an attribute of cerebral palsy, and further testing to rule out other causation may be indicated.16
True ataxia is a cerebellar disorder that is seen more frequently as a sequela of tumor removal (see Chapters 21 and 25) than as a problem occurring from birth. Ataxic syndromes are more commonly found in term infants. This type of cerebral palsy is a diagnosis of exclusion. In a small number of patients there is congenital hypoplasia of the cerebellum. Most of these children are hypotonic at birth and display delays in motor acquisition and language skills.10 Recruitment and timing issues remain problems in this population. Trajectory of the limbs, speed, distance, power, and precision are frequently documented as problems in this category. Midline is often achieved, but control of midrange movements of the extremities and control of trunk postural reactions are affected.
These classifications, even when accurately applied, give the therapist only a general idea of the treatment problem and must be supplemented by a specific analysis of posture and movement control during task performance, an interview for home care information, and assessment of treatment responses (see Chapters 7 and 8). The therapist is then ready to establish treatment priorities for the individual child.
Many of the characteristics described in the preceding paragraphs also apply to children who have had closed head traumas or brain infections. Further information can be obtained in Chapters 24 and 26. Some of the treatment suggestions that follow may also be applied in such cases. As with cerebral palsy, early positioning and handling after trauma may deter later problems.
Evaluative analysis of the individual child
Initial observations and assessment
A problem-based approach to the assessment and management of the child with cerebral palsy includes the family as key members of the team.17 While observing the child, the experienced therapist will want to periodically elicit from the parents their view of the problem. By listening carefully, the therapist will also be able to discern the emotional impressions that have surrounded previous experiences with professionals. Sometimes what is not said is more important than what is verbally offered immediately. Listening carefully and clarifying facts are more important than overwhelming the parents with excessive information and suppositions during early contacts. Observation of the family response to information will keep the therapist on track in developing a positive relationship with parents that deepens over time. The therapist’s role is often as interpreter of medical information as parents attempt to make some sense of their child’s diagnosis.
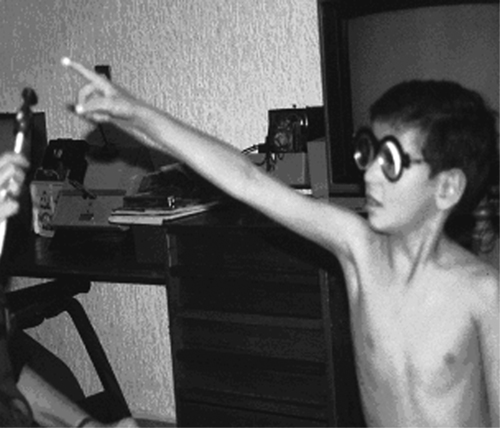
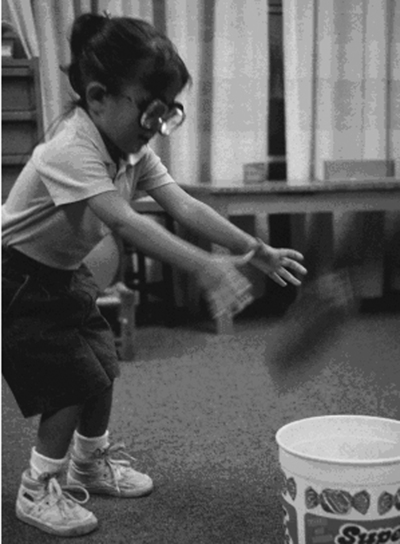
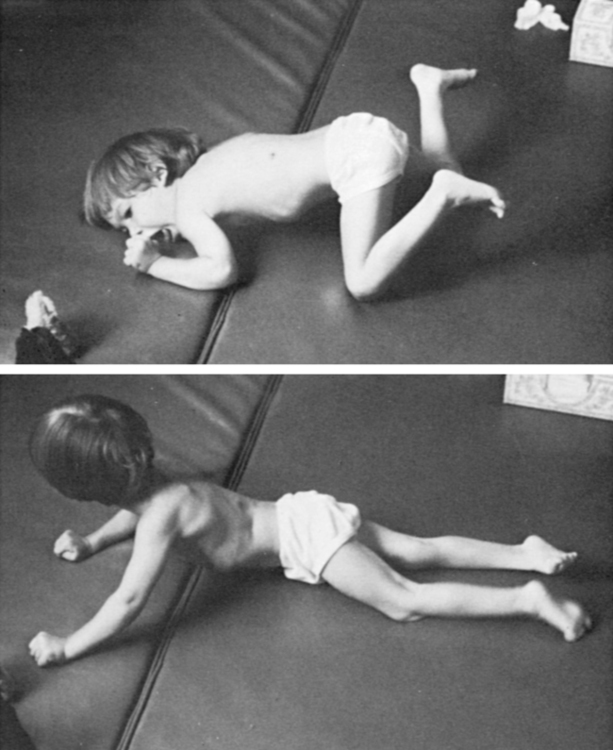
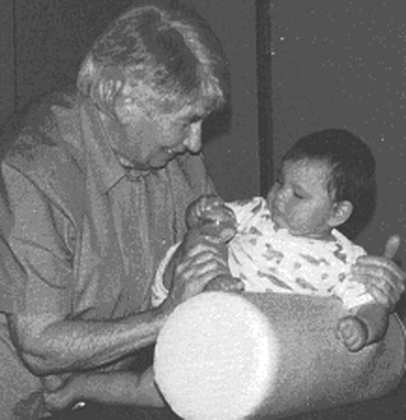
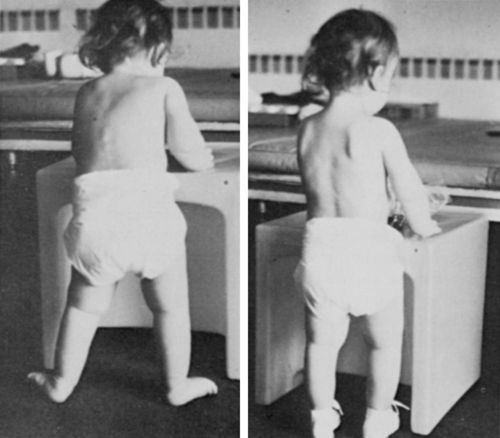
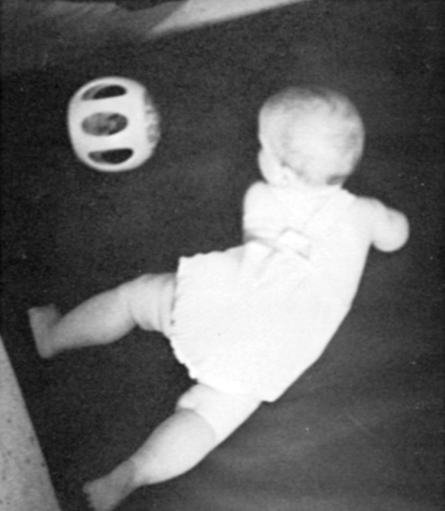
The next general step is to observe, in as much detail as possible, the spontaneous movement of the child when separated from the parent (Figure 12-1). Is the child very passive? Does he or she react to the supporting surface (Figure 12-2)? Are there atypical patterns of movement to reach a toy? Are clearly typical responses occurring with specific interference by reflexive synergies or total patterns of movement? Does the child rely heavily on visual communication? Do the eyes focus on a presented object, or does the postural abnormality increase with an effort to focus the eyes? Does the child lead or follow hand activity? Does an effort to move result only in an increase of postural tone with abnormal distribution? Does respiration adapt to new postural adaptations (Figure 12-3)? Is the child able to speak as well while standing as while sitting?
 Typical infants accumulate a multitude of experiences as they move smoothly in their environments.
Typical infants accumulate a multitude of experiences as they move smoothly in their environments.
 Emotional reactions are also translated into stronger spastic reactions influencing respiratory adaptation (see Chapter 5 on the limbic system).
Emotional reactions are also translated into stronger spastic reactions influencing respiratory adaptation (see Chapter 5 on the limbic system).This type of observation is valuable because movement patterns directly reflect the state of the central nervous system and can generally be seen while the parent is still handling the child.18 Once the child is on the mat or treatment table, outer clothing can be removed to observe interactions of limbs and trunk. Movement responses of the child can gradually be influenced directly by the therapist. Many disabled children associate immediate undressing in a new environment with a doctor’s office, and the chance to establish rapport is lost. In some instances it is preferable to have the parent gently remove some of the child’s clothing or even to leave the child dressed during the first therapy session. Gaining the trust of the child and parent is crucial during the first few sessions.
Standardized assessments are often used by facilities to document the developmental level of the functioning of a child with disability and to justify treatment. The Gross Motor Function Measure (GMFM) was developed to assess children with cerebral palsy and has good reliability and validity for children aged 5 months to 16 years.19,20 The Gross Motor Function Classification System (GMFCS), developed in 1997, is often used in conjunction with the GMFM.21,22 The GMFCS has five levels of classification for gross motor function, emphasizing movement initiation related to sitting, walking, and mode of mobility. Descriptors of motor function span an age range of 2 to 18 years, reflecting environmental and personal factors. The Pediatric Evaluation and Disability Inventory (PEDI) assesses children aged 6 months to 7.5 years in three domains: social, self-care, and mobility.23 The Functional Independence Measure for Children was developed as a test of disability in children aged 6 months to 12 years. This assessment covers self-care, sphincter control, mobility, locomotion, communication, and social cognition.24–26 This tool has been used to track outcomes over time. Although several instruments have been developed that meet psychometric criteria to document function in children with disabilities, the GMFM and the PEDI are thought to be the most responsive to change in this population of children because of their good reliability and validity.27,28 Often the decision to use an instrument to assess development will be left up to the clinician or facility. To date, there is no one tool that will cover all the categories necessary to document change in a child with cerebral palsy, so the clinician will need to rely on observational skills to describe quality of movement and response to changes in position in space and handling.
Each child will differ in the ability to separate from her or his parents. Spontaneity of movement, interest in toys, general activity level, and communication skills will also vary from child to child.29 Responding to the specific needs of the child enables the therapist to set priorities more effectively. If fatigue is likely to be a factor, it is important first to evaluate those reactions that present themselves spontaneously, followed by direct handling to determine the child’s response and potential for more typical movements. Movements or abilities for which there is a major interference from spasticity, reflexive responses, or poor balance may be better checked at the termination of the assessment so that the child remains in a cooperative mood as long as possible. Information regarding favorite sleeping positions, self-care independence, and chair supports used at home can be requested as the session comes to a close.
Clinical reasoning involves taking information from the assessment, including observations, results from standardized tools, family input, and the therapist’s handling of the child to formulate a treatment plan. Placing this information into a framework that makes sense to the therapist, the physician, other health professionals, and the family will assist in goal writing. The International Classification of Functioning, Disability and Health (ICF)30 is well known in the field of health care and allows one to see the overall interaction of the person with his or her environment and activities in the presence of the health condition.30
Reactions to placement in a position
If the child totally avoids certain postures during spontaneous activity, these are likely to be the more important positions for the therapist to evaluate. Observing how the child conforms to the support surface and how much contact there is with the surface will provide information about the ability to initiate movement from the surface. Support surface contact is essential for weight bearing and weight shifting to occur; both are critical for movement. Placement of the child in the previously avoided position will permit the therapist to feel the resistance that prevents successful control by the child.29 As mentioned previously, this may be held for the end of the assessment. The parent should play an active role in the assessment whenever possible. Continued dialog with the parents reveals factors such as the frequency of a poor sitting alignment at home or a habitual aversion to the prone position. Sitting close to the television set or tilting the head when looking at books should also be noted so that functional vision skills can be related to other therapy interventions.31 These contributions by the parents establish the importance of good observation and the need for parents and the therapist to work cooperatively. Therapists of different specialties need to initiate continuing communication to coordinate therapy objectives.
According to the guide for typical development, infants should be able to maintain the posture in which they are placed before they acquire the ability to move into that position alone.32,33 The problems presented by cerebral palsy occur to some extent as a reaction to the field of gravity in which the child moves.32 Visual perceptions of spatial relationships motivate and determine movement patterns while the child must react at a somatic level to the support surface. It is helpful, therefore, to attempt placement of the infant or child into developmentally or functionally appropriate postures that are not assumed spontaneously (Figure 12-4). Resistance to placement indicates an increase in tone, a structural problem, or an inability to adapt to the constellation of sensory inputs for that alignment. A movement that resists control by the therapist will be even less possible for the child. What appears to be a passive posture may hide rapid increases in hypertonicity when movement is initiated or instability of a proximal joint when weight bearing is initiated. A child may have learned to avoid excitation of the unwanted reactions and may fix the body position to avoid the alignment that cannot be controlled. Another child may enjoy the sensory experience of accelerated changes in postural tone and deliberately set them off as a means of receiving the resulting stimulation to his or her system.
Visual-motor assessment
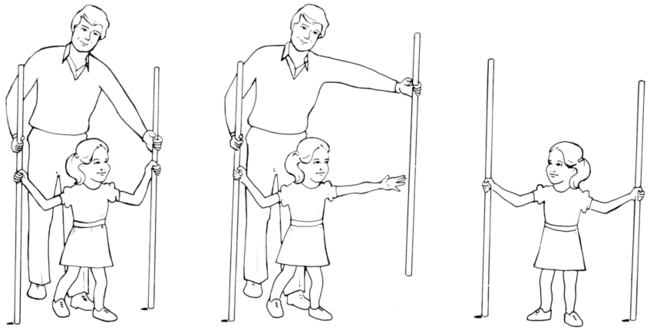
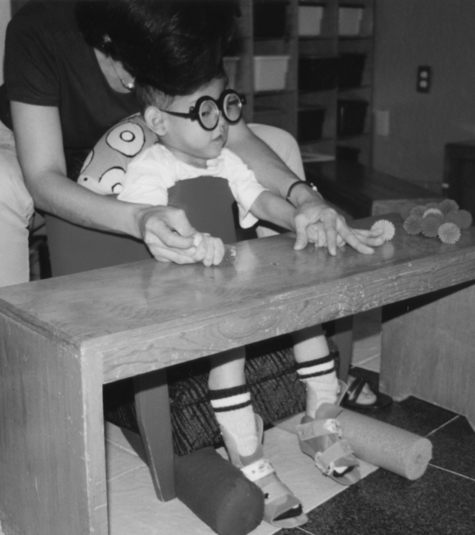
It is the visual-motor aspect of performance function that is of primary concern to the therapist because spatial judgments are needed to control movement of the body in an upright alignment. The infant who is able to stand and walk along a support and then seems unable to let go of the support is often found to have functional vision interferences. The child with cerebral palsy most often demonstrates significant neuromotor delay in the developmental process, which often results in the inadequate establishment of matching of inputs from the postural and visual systems (Figure 12-5). Visual-motor learning experiences are filled with compensatory responses from both systems. Vision plays an important role in early motor development for learning about, manipulating, and exploring the environment. Therefore vision requires attention during the assessment of motor abilities. (Refer to Chapter 28.)
The visual system in its development has many parallels with the postural system.34 Binocular control and freedom of movement are necessary for the system to function properly. Ambient visual processing must be integrated with central visual processing to take in information that relates to position in space and to focus on a particular target. A simple screening examination may check acuity at 20 feet on the E chart and declare vision to be normal. An ophthalmological examination is needed to determine the health of the eye structures, particularly in the case of infants born preterm. Equally important is a functional vision examination given by a behavioral or developmental optometrist to reveal the level of efficiency that the two eyes have achieved in working together and whether the ability to focus in far and near ranges is smoothly established. Strabismus dysfunctions commonly coexist with cerebral palsy and may cause the child to receive a double image of environmental objects. Judgments about space are related to a three-dimensional perception of the surrounding environment, which requires coordinated use of the two eyes. Conservative management of eye alignment problems is done with the use of lenses and prisms by the experienced optometrist, which permits the therapist to work for basic head control by the child before any irreversible changes are made to the eye muscles. Eye movement differentiates from head movement in much the same way that the hand differentiates from general arm movement, corresponding to general maturation of the central system.
Because the visual system is first a motor system, children with cerebral palsy most often have difficulty separating eye movement from head movement and controlled convergence for focal changes. When their posture is supported, eye movement can proceed to evolve in accuracy and complexity. With inadequate alignment of the head in relation to the base of support, the visual system accumulates distortions and inconsistent input, which leads to the formation of an inadequate perceptual base for later motor learning (see Chapters 4 and 28). Even after improvement in the control of posture and movement, the visual system continues to adapt to the previous faulty visual-motor learning, resulting in perceptual confusion and inefficient organization of body movement in space. The therapist who is working for improved motor control may notice that such a child reacts with adequate postural adaptations when facing the therapist or a support and that the movement quality seems to disintegrate when the child faces an open space. This immediately jeopardizes the ability of the child to use her or his new responses after leaving the therapy environment. Visual orientation to the environment will dictate alignment against gravity, and the reverse is also true; poor alignment against gravity will affect visual orientation to the environment. Movement, postural stability, and muscle activation are closely related to vision.35
Padula, a behavioral optometrist specializing in neuro-optometric rehabilitation, has described a posttrauma vision syndrome in adults with acquired central dysfunction and has applied this information to children with cerebral palsy.36 A perceptual distortion in the perceived midline of the body, known as visual midline shift syndrome, is corrected with the use of prescribed prism lenses, which then permits the child to step into the perceived space with more confidence (Figure 12-6). The observant therapist will begin to notice that the sudden increase in neuromuscular tension in a child taking steps in a walker is often accompanied by closing of the eyes. This seems to be a momentary inability of the central processing system to integrate the information arriving from different sources. With the use of prism correction, the child experiences the body as more coherent with visual-spatial perceptions. By incorporating an understanding of visual observations into intervention strategies, physical and occupational therapists are able to note compensatory adaptations by the complementary systems and use them to their advantage in effective treatment intervention.
Some children who walk on their forefeet or even on their toes and who have made little if any permanent gait change after the use of inhibitory casting or orthotics also fall into the population described previously. With prisms that correct the perception of forward space, the child places the entire foot in contact with the support. Such prism lenses are used during therapy handling as a perceptual learning experience for the child, with the optometrist and the therapist coordinating their efforts. Hand-coordination activities also require timing of reach and grasp that is based on feed-forward input from the visual system.35 In some cases the therapist observes the visual system to overfocus in the moment that the child loses control of his or her postural stability. This suggests that the visual system may be attempting to compensate for the inadequacy of the postural control, much in the same way that we all adjust our head position to see better. Understanding the nature of the continuing dynamic interaction between these two functional subsystems of the central nervous system and attending to the needs of visual-postural orientation will increase the successful evolution of clients with cerebral palsy.
Posture and movement compensations
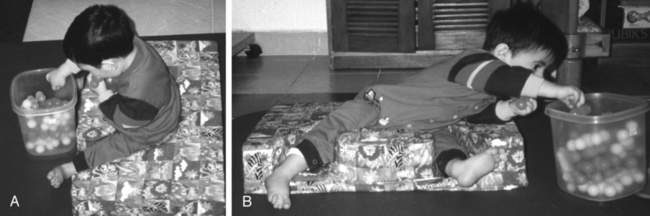
The quality of a body posture or position in space determines the quality of the movement that is expressed. Lack of head control, poor midline organization, and deficient trunk strength begin the process of compensation. From a distorted starting position the movement initiated is one that is restricted (Figure 12-7). The lack of central “core” stability in the body restricts the full mobility of a limb. This limitation over time is increased by fascial and muscular restrictions on smooth coordinated muscle action. The child continues to learn the atypical responses because the movement patterns tend to be reinforced by either accomplishment or reinforcement of some kind from the environment. Compensatory movement patterns evolve because of necessity rather than any feedback as to efficiency or functional smoothness.
Active therapy intervention allows the sensorimotor learning of the child to be modified so that some part of the compensatory response becomes unnecessary and the movement becomes more typical (Figure 12-8). This relative approximation of what is expected in a typical response may occur in the area of initiation, timing, strength, or ability to sustain an antigravity alignment. As movement expression and postural stability are better established, the compensatory patterns are used less often, and new motor learning occurs on a base of closer-to-normal experience.
Compensatory processes have their positive aspects.37 The independence finally achieved by the older child reflects her or his intelligence and motivation and the family’s attitude toward the child and the disability. The most debilitating handicap of cerebral palsy in an intelligent child may be social or psychological when the child is not accepted by the family and therefore cannot develop a positive self-image. Compensatory movement patterns may permit greater independence, if and when they do not limit or block the active learning of new motor strategies.
Other assessment considerations
Nutritional aspects of neuromotor function
Nutrition is viewed as providing an important biochemical base for enhanced human performance. Williams,38 author of the classic reference Biochemical Individuality, was one of the first to point out the existence of significant variability in the need for specific individualized nutrients because of differences in assimilation and other factors. Physicians Crook and Stevens,39 Smith,40 Pfeiffer,41 and Cott42 are a few of the leaders who have analyzed the link between nutrient intake and behavioral differences in children and adults. Many of these references address issues of attention and learning. To have efficient function of the transmitters at the myoneural junction and good health for the myelinated neurons of the nervous system, a variety of trace elements must be present.41 Lack of dendritic proliferation is associated with malnutrition regardless of the cause.43 The ambulatory child with cerebral palsy will need to be considered for a new level of energy expenditure to avoid short stature and poor nutritional status.44
Another body of work explains more about the direct link between food intake and muscle efficiency for high performance and normal function. The need for water is paramount for healthy fascia. In children with cerebral palsy and related disorders there is often from the beginning a difficulty in the smooth automatic sucking needed for nutritive intake. Uncoordinated patterns of mandibular and tongue motion persist when not addressed in early and precise intervention strategies. Even the digestive process is affected negatively by inadequate chewing, a higher-than-typical percentage of food allergies, and less-than-efficient physiological functions.45
It is likely that brain dysfunction in some of these children extends to the hypothalamus, thus influencing the entire digestive process. Duncan and colleagues46 have documented the risk of osteopenia in nonambulatory children with cerebral palsy. This retrospective study showed that fewer than 75% of the calories needed were administered to 95% of the children with gastrostomy tubes. Nutrients were also deficient. This may explain part of the poor physical response level of such children. Sonis and colleagues47 looked specifically at energy expenditure in children and adolescents with spastic quadriplegia in relation to food intake. They found dietary intake to be markedly overreported for this population and determined that nutrition-related growth failure was likely related to inadequate energy intake. Reflux is also common in infants with developmental problems. In some infants reflux subsides as the physical stress is reduced in the tissues bordering the upper thoracic and cervical spine, but it can be related to milk sensitivity or even susceptibility to environmental contaminants.
To supplement nutritional intake in the child with cerebral palsy, the individual child must be considered with regard to age, size, activity level, and growth factors.48 Ideally, blood, urine, or hair analyses would be done to determine nutrient imbalances, and supplementation with specific nutrients would be guided by a specialist. Environmental medicine has taken the lead in this type of work. The rehabilitative process places increased demands on the entire system and requires fuel to set the stage for improved muscle function. Protein, carbohydrates, and adequate hydration are sources that build muscle and provide a foundation for strengthening and the advancement of motor skills in populations without disability.49,50 A well-balanced diet will provide the requisite energy for exercise. However, little research has been done specifically on children with cerebral palsy and appropriate levels of protein during exercise. Therefore it is necessary to discuss these issues with the family using caution unless specifically trained to do so. A nutritional consultation is warranted when concerns arise in this area.
Consideration of supplemental oxygen
Shintani and colleagues51 performed a careful study of 233 children with cerebral palsy to determine the presence of obstructive sleep apnea. In 10 children with cerebral palsy who were received at the hospital for treatment of severe obstructive sleep apnea, these authors determined that adenoidal or tonsillar hypertrophy were noted in only four children and that the main cause of sleep apnea in the other six children was pharyngeal collapse at the lingual base. Fukumizu and Kohyama52 looked at central respiratory pauses, sighs, and gross body movement during sleep in 19 healthy children, ages 3 months to 7 years. Central pauses occurred more often during non–rapid-eye-movement sleep and increased with age. Developmental differences need further study.
Decreased oxygen levels have been associated with impaired cognitive and physical performance in the literature.53 In the presence of inadequate peripheral oxygen saturation, low levels of oxygen can be administered during the night. This practice has been used with selected low-tone and athetoid children for improved energy during the day during growth changes, but formal study is needed on a larger group of children with cerebral palsy. Better oxygenation of the tissues can also result in increased food intake and consequently improved energy levels.
Roles of the therapist
Role of the therapist in direct intervention
The primary role of the therapist is in direct treatment or physical handling of the child in situations that offer opportunities for new motor learning. This should precede and accompany the making of recommendations to parents, teachers, and others handling the child. Positioning for home and home handling recommendations should always be tried first by the therapist during a treatment session. As noted for the initial assessment, many interventions will cause a reaction unique to the particular youngster.29,54 It is the role of the therapist to analyze the nature of the response that is accompanied by adaptation inadequacies, to analyze the movement problems, and to choose the most effective intervention (Figure 12-9). It will then be possible for other persons to manage play activities and supervise independent functioning that reinforce treatment goals.55
Case management and direct intervention
Simple documentation of observed changes in a child over a series of regular clinic visits is still too common for many children with cerebral palsy. Regular appointments, with periodic assignment of a new piece of apparatus, do not constitute active treatment. Although physical intervention in the form of direct handling of the child is considered a conservative treatment by most physicians, relatively few children receive sufficient physical treatment at an early age.56,57 Therapists need to demonstrate their unique preparation and describe their interventions in ordinary language so that families as well as other health care professionals understand the importance of specific treatment versus general programs of early stimulation that are designed for neurologically intact infants.
The prognosis for change in cerebral palsy is too often based on records of case management rather than on the effect of direct and dynamic treatment by a well-prepared therapist. Bobath32,58 documented accurately the developmental sequence expected in the presence of spasticity or athetosis. Her book consolidates some observations of older clients that help professionals understand the uninterrupted effects of the cerebral palsy condition. In any institution one can observe the tightly adducted and internally rotated legs, the shoulder retraction with flexion of the arms, and the chronic shortening of the neck so common as the long-term effects of cerebral palsy. The long-term influence of athetosis results in compensatory stiffness or limited movement patterns to create a semblance of the missing postural stability while a limited number of movement patterns with limited degrees of freedom are used to function (Figure 12-10).
Within the clinical community there is increasing evidence that soft tissue restrictions further limit spontaneous movement in children with cerebral palsy. The fact that these fascial restrictions are often found in infants suggests that they originate early rather than as a gradual result of limited ranges in movement. Because of the tendency of fascial tissue to change in response to any physical trauma or strong biochemical change, some of these characteristics might be originating with traumatic birth experiences, and they would be exacerbated by daily use of limited patterns of movement. Tissue restrictions can also occur with immobilization or general infectious processes.59–61 Soft tissue begins to change its physiological structure with the application of gentle sustained pressure, so it serves as documentation that there are changes caused by the therapist’s simple hand contact. Some of the sensory information in the form of tapping or holding or application of pressure affects fascial meridians and muscle alignments.62 A therapist must be prepared to defend his or her approach with a solid foundation, theory, and objective outcomes. Objective documentation is important when dealing with any population but essential for demonstrating therapeutic change.
Applying specific soft tissue treatment techniques to any person with a neuromotor disorder creates the need for immediate follow-up with practice of new skills using this improved range of motion. Creating excessive tissue mobility in a given area of the body can destroy the delicate patterns of coordination that permit synergic function in the person with cerebral palsy, so functional activation of the body after each specific mobilization is strongly recommended to integrate the tissue change. Well documented in the literature on current motor control and motor learning is the need to practice, practice, practice.63 Practice time is related to skill performance; the amount and type of practice are determined by the stage of learning that an individual is in and the type of task to be learned63–65 (see Chapter 4 on motor control and learning). Interestingly, most of what we know about motor control and motor learning is based on individuals who are “typicals,” and it is yet to be determined whether the same principles that are considered important in healthy individuals apply to people with disability. However, it makes sense that practice would influence the use of any new or relearned skill.
An occupational therapist, Josephine Moore, stressed Bach-y-Rita’s66 works to emphasize some important points for therapists regarding the concept of increasing functional demands on the central system and the importance of the neck structures in developmental movement sequences. Children with spasticity often have a lack of developmental elongation of the neck, whereas children with athetoid or dystonic movement lack neck stability and consistent postural activation. Tone changes often originate with changes in the delicate postural interrelationship between head and body or with ambient visual processing.
By appreciating the abundance of polysynaptic neurons and parallel processing in the central nervous system, the therapist will become more optimistic regarding his or her role as facilitator and feedback organizer to guide new movement. Restak,67 in his book The New Brain, confirms the continual reorganization of the brain in response to new input. Several animal and human studies on neuroplasticity have confirmed that the brain reorganizes after an injury and that this reorganization is shaped by rehabilitation and motor skill learning.68–71 In the child with cerebral palsy, the therapist looks for subtle changes in the child’s response to determine newly integrated sensorimotor learning. For example, excessive emphasis on extensor responses in the prone posture for the older child can jeopardize the quality of neck elongation in sitting, so it is essential to work on the components necessary for control of the new posture desired.
Special needs of infants
The direct treatment of infants deserves special mention because there are significant differences in intervention strategies for the infant and the older child. Aside from the delicate situation of the new parents, the infant is less likely to have a diagnosis and presents a mixture of typical and atypical characteristics. It is essential that the clinician have a strong foundation in the nuances of typical developmental movement and early postural control.4,72 Soft tissue issues must be addressed in detail. Direct intervention can be offered as a means of enhancing development and overcoming the effects of a difficult or preterm birth. It will be important, however, to pursue a diagnosis for the infant who reaches 8 or 9 months of age and continues to need therapy because third-party payers often require a diagnosis beyond developmental delay or prematurity.
Infants with early restrictions in motor control should be followed until they are walking independently, even if they no longer need weekly therapy. Infant responses can change rapidly as the therapist organizes the components of movement control. Soft tissue restrictions should be treated initially to have more success with facilitated movement responses. Careful observation is essential because all but the severely involved infant will change considerably between visits. The therapist should invest some time in training the parents to become skilled observers while appreciating the small gains made by their infant. Physiotherapist Mary Quinton73 has written specific intervention strategies for babies (Figure 12-11). Infant massage is important to improve the bonding of mother and child and to improve physiological measures.74,75
Orientation to treatment strategies
Inhibiting or stopping the movement of one part of a movement range or even one limb must be done in a way that permits the child to activate the body in a functional way. The child who lies in the supine position with extreme pushing back against the surface is rarely seen when therapy intervention has started early. The therapist initially eliminates the supine position entirely but would incorporate into the treatment plan the activation of balanced flexion and extension in sitting with the ability to vary pelvic tilt for functional play and reaching (Figure 12-12). The child might later be reintroduced to a supine position with postural transitions that support balanced control of the body with more differentiated movement.
One of the primary considerations for the child with spasticity is adequate respiratory support for movement. Mobility of the thoracic cage and the midtrunk must be combined with trunk rotation during basic postural transitions (Figure 12-13). Consideration of age-appropriate movement velocity will guide the therapist in choosing activities that challenge better respiratory adaptability and prepare for speech breathing to support vocalization. The therapist will find it helpful to hum or sing or even make silly sounds that encourage sound production by the child during therapy. Movement of the child’s body changes respiratory demands and frequently results in spontaneous sound production during therapy. Assessing the ability to sustain a breath to speak is easily done during a therapy session by counting the letters in the alphabet that can be said with one breath. This should be done with the child supine and in an upright position because trunk control required while sustaining a breath changes with the posture attained against gravity. Describing the chest shape and movement of the thorax observed can serve to assist the therapist in problem solving and prioritizing the treatment plan.

 Rotational patterns combined with transitional movements can be used to mobilize the thoracic cage.
Rotational patterns combined with transitional movements can be used to mobilize the thoracic cage.The therapist working with the child with cerebral palsy constantly monitors the quality of the child’s motor response. These continuing observations guide the manipulation of the environment and the assistance given the child to move toward a functional goal. Is the body tolerating the position? Does the child adapt to the supporting surface and use the supporting surface contact for movement initiation (Figure 12-14)? Is the movement of a limb graded and without unwanted associated reactions in other parts of the body? By analyzing the answers to such questions, the therapist is guided to an appropriate sequence of the therapy session and is enabled to set functional treatment goals and realistically change prognoses.

 This child has little contact with the supporting surface, resulting in poor movement initiation.
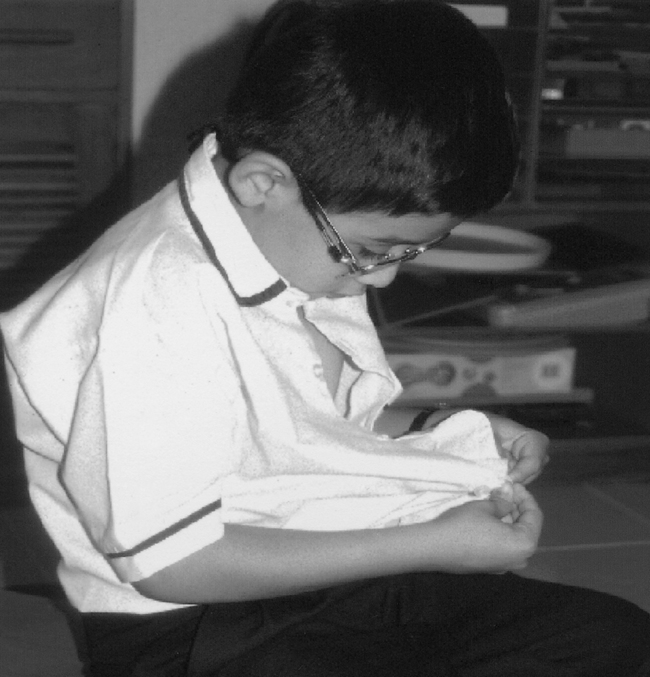
This child has little contact with the supporting surface, resulting in poor movement initiation.The developmental meaning attached to the sensation of typical movement is complex and starts with the ability to process contrasting stimuli. While several parts of the body are stable, another is moving. Stability of the proximal body permits a limb to extend forcefully or to be maintained in space. Each new level of developmental dissociation of movement increases the complexity of central nervous system processing. The process of self-feeding illustrates how internal and external stimuli impinge simultaneously on the central nervous system. The process of guiding a full spoon toward the mouth initially engages the child’s attention. The arm is lifted at the shoulder to bring the fragrant food odor to the level of the mouth before elbow flexion takes the spoon to the face (Figure 12-15). Between 2 and 6 years of age the self-feeding pattern is modified and the elbow moves down beside the body. Now the motor aspect of the task has become procedural and more efficient, permitting the child to participate in social exchanges with the family at the same time that she or he manages independent self-feeding. The complexity of the task increases with the secondary task of social exchange.
A solid understanding of typical developmental sequences is essential for the clinician providing direct treatment intervention.18,76 Early responses of the typical infant change from a self-orientation to an environmental orientation as new developmental competence emerges. More sophisticated balance in independent sitting occurs as the ability to pull to standing at a support begins to develop. Such knowledge of developmental details supports the therapist in introducing postural activities at a higher developmental level to integrate more basic abilities. The assisted self-dressing process is an effective way to introduce and integrate new movement and sensorimotor learning while using established movement skills. To sit well, the child needs practice moving over the base of support and coming in and out of sitting, and control of coming to stand from sitting. To walk well, the child may need to practice running to allow practice in changing rate, direction, range, and balance. Sitting is made more dynamic by using a gymnastic ball as a seat. Transitional adaptations of posture may be elaborated during therapy sessions to include more complex alignments. Specific techniques are reviewed in Chapter 9.
With the child dominated by athetoid movement, the therapist’s role relates primarily to organization and grading of seemingly erratic movement responses and establishing function around midline. These children have the ability to balance, but their balance reactions are often extreme in range and velocity. Their movements are rarely in the midline, asymmetrical, and frequently dominated by primitive reflexes, with poor midrange control of the trunk and extremities. Cognitively they are eager to participate and usually are responsive to working on specific goals that relate to functional success. By working to improve central control, the therapist gradually introduces taking of body weight over the limbs, with assistance to grade the postural control of the central body. By working closely with a behavioral optometrist the therapist can use visual input to improve the child’s balance reactions. In these children the therapist may note that disruption of eye alignment or focusing results in a momentary disorganization of postural control (see Chapter 28).
Movement control must become procedural so that it is not interrupted by every environmental distraction. This is more likely to happen when balanced activity of the visual, vestibular, and proprioceptive systems has been achieved. Independent ambulation becomes practical when the individual is able to think of something else at the same time. The therapist begins this process by carrying on a conversation with the child to engage the cognitive attention so that the motor act becomes more automatic. The concept of graded stress is discussed in Chapters 5 and 6.
Direct intervention for the hemiplegic child takes into account the obvious difference in postural tone between one side of the body and the other. Treatment for children that addresses itself only to the more affected side of the body will not prove to be effective. The critical therapeutic experience seems to be that of integration of the two sides of the body and the establishment of midline (Figure 12-16). The child with hemiplegia differs from the adult stroke patient in that the adult had a clearly established midline and integration of both sides of the body by learning to cross midline before the stroke episode. The child with hemiplegia has not had that experience and will need emphasis on this during intervention. The integration of both sides of the body begins early for the typical infant, with lateral weight shifts in a variety of developmental patterns, and leads to postural organization that permits later reaching for a toy while the body weight is supported with the opposite side of the body. The child with a contrast in the sensorimotor function of the two sides of the body needs to experience developmental patterns that include rotation within the longitudinal body axis and lateral flexion of the trunk, the more affected side forward. The more affected side needs the experience of supporting the body and the experience of initiating movement.
Development of hand use first focuses on bilateral arm activity while keeping the affected hand well within the functional visual field (Figure 12-17). The infant or young child works primarily in sitting until dynamic trunk flexion is activated. Pelvic mobility is essential to activate the necessary trunk responses. The therapist may find that true lateral flexion of the more affected side of the body is fully as difficult for some children as the initial active elongation of that side. There tends to be a high incidence of soft tissue restrictions in the shoulder and neck of the affected side. Children with hemiplegia have difficulty in sustaining a balanced posture against the influence of gravity, and some begin to struggle to do everything with the less affected side. This characteristic contrast in function may contribute to the development of seemingly hyperactive behavior that is related to the inability of the central nervous system to resolve contrasting incoming information. Hyperkinetic responses in one side of the body may compensate for relative inactivity in the opposite side. Leg length discrepancy, scoliosis, pelvic obliquity, and shortening between the ribs and pelvis may develop. One goal of treatment is to bring these divergent response levels closer together so that the child can experience more comfortable postural change and adapt to later school demands.
 Bilateral arm activity with visual regard that corresponds to hand motion incorporated into therapy.
Bilateral arm activity with visual regard that corresponds to hand motion incorporated into therapy.The greater the discrepancy between the sensorimotor experience of the one side of the body and the other, the more tendency the system seems to have to reject one of the messages. This can lead to distortions in verticality and is a major interference in bilateral integration. Functional vision evaluation is important to avoid the midline shift problem that will distort postural control. As body weight is shifted to the more intact side, flexor withdrawal patterns of the limbs increase in frequency and strength in some children. These postural reactions are often associated with lack of full weight bearing on the more affected side. The presence of a lateral visual midline shift or some visual field loss may increase the avoidance of bearing weight on the more affected side.72 One important therapy goal is the achievement of graded weight shift through the pelvis during ambulation (Figure 12-18).
The child with low muscle tone is perhaps the greatest challenge for both therapist and parent. Adequate developmental stimulation is difficult unless positioning can be varied. Placing the child in a more upright alignment, although it is achieved with complete support initially, seems to aid the incrementation of postural control. To prepare the low-tone body for function, it is helpful to review the articulations for possible soft tissue restrictions. However, equally important is not to take away muscle tightness that is providing a form of stability for the child without the ability to give him or her another form of stability for functional use. The neck and shoulder girdle are particularly vulnerable. Strong proprioceptive input while accurate postural alignment is ensured is an important part of the treatment session. A direct push-pull motion of the limbs, which is gentle traction alternated with approximation as described by Bobath,77 also assists in maintaining antigravity positions and creates postural variance in the practice of antigravity postural reactions. Positioning at home may include a high table that supports the arms, allows for increased trunk extension in good alignment, and permits voluntary horizontal arm motion. The therapist must be cautious of the tendency to fixate in response to trunk instability and initial hypotonicity. This seemingly hypertonic response, which can be distributed in the deeper musculature, contributes to limited adaptability rather than differentiated postural control. It is difficult to ramp up the corticomotor neuron pool even though the child’s motor output may remain limited; changes in positioning and opportunities for the child to have other sensory and visual experiences will often serve to motivate the child and contribute to motor learning. Home handling needs to include a variety of positions during each day for seating and play. Consistency in these practices is essential for the child with low tone to progress.
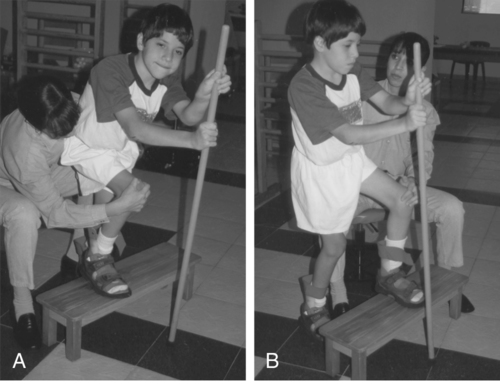
The process of undressing and dressing can be a dynamic part of the treatment program for any child (Figure 12-19). Diagonal patterns of movement that are incorporated into the removal of socks and shoes assist in the organization of midline orientation. Weight shifts and changes in stability-mobility distribution occur throughout the dressing process. Concepts of direction and spatial orientation are applied to the relationship of body parts and clothing. Directional vocabulary terms and names of clothing and body parts are learned with this experience. A bench is useful because it permits the adult to sit behind the child who is just beginning to participate actively. The older child with difficult balance reactions can use the bench in a straddle-sit alignment (Figure 12-20). Aside from the physical and perceptual benefits, this achievement of dressing independently is one that offers the child a feeling of pride and independence. It is also a very practical preparation for the future when it is introduced in keeping with individual developmental and emotional needs (Figure 12-21).
Research
Constraint-induced movement therapy (CIMT) was developed from basic science experiments on deafferenated monkeys to overcome learned nonuse of the upper extremity.78,79 This forced use approach was adapted for adult patients after a stroke; the affected upper extremity is forced to participate in activities and the less involved upper extremity is constrained. Practice is intense, with 6 hours of mass practice for a 2-week period.80–82 This protocol has been quite successful, with significant improvement in upper extremity movement and use of the affected limb. CIMT is very popular and is now beginning to appear in the clinical setting. The pediatric client has also demonstrated a favorable response to this treatment protocol in several single-case studies.83–87 In a clinical randomized trial by Taub and colleagues,88 children with hemiplegia or brain injury receiving CIMT for 21 consecutive days, 6 hours a day, demonstrated significant improvement in the amount of use, quality of movement, and spontaneous use of the affected upper extremity. These results were sustained at 6-month follow-up. Several studies from around the world are beginning to show up in the literature with varied methods. Most of these studies are promising; however, further investigation is necessary to establish the critical threshold, adequate dosage, and selection process for subjects who will benefit the most.89–93 Clinicians are beginning to adapt these studies to their therapeutic settings and modify the protocols for clinical use and reimbursement potential.
Treadmill training has also been used in children with cerebral palsy.94–101 The treadmill has been instrumental in rehabilitation for many years with a variety of purposes. This treatment began with animal studies on spinalized cats and rats and their responses to training on a treadmill in the recovery of a walking pattern.102–105 Today this treatment is used in many populations, including those with spinal cord injury, traumatic brain injury, Parkinson disease, stroke, and cerebral palsy.106 The use of the treadmill in children with cerebral palsy has shown promising results: improvement in gait pattern, increased walking speed, decreased coactivation in lower extremity musculature, overall gross motor skill improvement, and improved and stabilized energy expenditure.94–101 Treadmill training interventions have taken on many different faces, including use of a regular treadmill, commercial equipment, and high-tech body-weight support systems (Figures 12-22 and 12-23). Commercial equipment is now available to assist with supporting the body weight of individuals who otherwise would not be candidates for such a treatment. Clinical adaptations have also been incorporated to accommodate smaller bodies on a treadmill, which allows the therapist to assist from behind or from the side. Setting goals for this treatment must be precise, with an understanding of the purpose intended for its use: improving endurance, changing the parameters of the gait pattern, strengthening, and gait training. Each goal must be based on a sound theoretical foundation, which is now available from the literature.
Strength training was never thought possible in the presence of spasticity in children with cerebral palsy. Several studies have now shown that strength can improve in children with spastic cerebral palsy.107–110 Circuit training was used in an afterschool training program for 4 weeks, two times a week for 1 hour of intense group training, resulting in improved strength and functional performance.107 Strength was maintained in this group of individuals at an 8-week follow-up posttest. Dodd and colleagues108 set up a home-based lower extremity strengthening program in a randomized clinical trial with 21 individuals with cerebral palsy. All subjects in the treatment group had improved lower extremity strength that was maintained at follow-up periods of 6 and 12 weeks. In a study focused on biofeedback and strength training to improve dorsiflexion and range of motion, Toner and co-workers110 demonstrated significant changes in active range of motion and dorsiflexion strength.110 Strength training in the presence of spasticity is also documented in adults as beneficial not only for conditioning, improved range of motion, and psychological well-being, but in some cases reduction of spasticity.111–114 Strength training in children and adolescents with cerebral palsy has continued with investigations into the intensity, type of contractions to practice, and dosage.115,116 Interestingly, a systematic review of common physical therapy interventions in school-aged children found that strength training demonstrated significant improvements in selected muscle groups but no meaningful change in function. Martin and colleagues117 and Moreau and colleagues118 studied muscle architecture as a predictor of maximum strength and its relationship to activity levels in cerebral palsy.118 They found that ultrasound measures of the vastus lateralis muscle thickness adjusted for age and the GMFCS level were correlated and predictive of maximum torque in children with and without cerebral palsy. A variety of methods for strength training can be incorporated into a clinical treatment setting or home exercise program with anticipated improvement in muscle strength, which may also result in improved functional status for children with cerebral palsy. Strength training encompasses free weights, aerobic workouts, stretch bands or tubing, and machines that address resistive exercise (Figure 12-24).
Many adjuvant therapies that are popular in combination with other treatments are available to individuals with cerebral palsy. Electrical stimulation (ES) has been used in a variety of ways with children with cerebral palsy. In several case reports by Carmick,119–121 neuromuscular ES used in conjunction with task-oriented practice was found to improve sensory awareness, strength, gait parameters, and passive and active range of motion. Neuromuscular ES was used as an adjunct therapy with upper and lower extremity practice protocols.119–122 ES has been used in conjunction with 6 weeks of intensive therapy to improve sitting posture and trunk control for children with spastic cerebral palsy. Radiographic studies confirmed the statistical significance in decreasing the kyphotic angle of the spine and sitting score on the GMFM.123 Two recent studies documented an improved gait pattern and reduced spasticity in 27 children with spastic diplegic cerebral palsy after use of transcutaneous electrical nerve stimulation on selected lower extremity musculature for 15 minutes, three times a day, for 1 week.124,125 Neuromuscular ES was used successfully in combination with dynamic splinting to improve upper extremity range of motion at the elbow and wrist in 6 children with cerebral palsy.126 ES has been in the therapy arena for many years, and its selective use with children who have cerebral palsy may supplement regular therapy sessions with enhanced results. (Therapeutic subthreshold ES at meridian points is discussed in the section on electroacupuncture treatments and in Chapter 39.)
Botulinum toxin A (BtxA) has been used to assist in decreasing spasticity because it provides a permissive condition that improves and increases range of motion and practice of new motor patterns without interference from increased muscle tone. Gait velocity, stride length, range of motion, and decreased spasticity were noted to be significant in 33 subjects with cerebral palsy after local injections of BtxA.127 Several studies have shown a decrease in spasticity, successful treatment of foot deformities, and improved gait parameters with BtxA.128–131 In a study by Galli and colleagues,132 dynamic dorsiflexion improved during stance and swing phases of gait, with significant improvement in foot placement at initial contact. BtxA has been used with varying results as an adjunct treatment for the management of upper extremity spasticity.133 Lukban and colleagues134 reviewed six randomized clinical trials with a total of 115 children receiving BtxA in the upper extremities. Five of the six trials demonstrated a reduction in spasticity that was time limited, and four of the six trials documented improved hand function. Four systematic reviews concluded that there simply was not enough evidence to support or refute the effectiveness of BtxA for upper extremity use. It allows for the reduction of muscle tone and opens a window of practice opportunity, in combination with other treatments, to learn new movement possibilities. BtxA has a temporary effect, so the critical element is its combination with other treatment modalities. Park demonstrated improved range of motion and decreased spasticity in ambulatory children with cerebral palsy when BtxA was used in combination with serial casting.135 It has also been used as an alternative to control the progression of hip dislocation and hip pain in children with cerebral palsy.136
Soft tissue mobilization is a method of stretching tight structures that have become restricted from overuse, spasticity, deformities, muscle shortening, surgeries, trauma, and poor nutrition. This type of stretching has strong roots in osteopathic medicine but is not limited to that area of expertise. Over the years, research investigating the cellular and tissue changes that occur with immobilization has revealed some interesting and shocking alterations in the muscle and collagen fibers. With immobilization, slow muscle fibers show greater atrophy than fast fibers do.59 There is atrophy, a decrease in peak torque, an increase in fatigue resistance, loss of strength, and reduced central activation when the plantar flexors of the ankle are immobilized.137,138 In a recent study of children with severe spasticity, muscle biopsies were performed on the vastus lateralis to determine collagen accumulation in the spastic muscle. An increased accumulation of collagen I fibers in the endomysium of the muscle was noted, with thickening and decreased muscle fiber content in the more severe cases.139 This study, in combination with what we understand about healthy muscle, reinforces the need to keep the muscles flexible and active to help prevent this accumulation of collagen. Soft tissue mobilization and deep tissue stretching are methods that can improve the ability of the tissue to lengthen and fold, allowing for a more efficient activation of the muscle fibers, thus optimizing the formation of typical synergies during practice of motor skills.
As mentioned earlier, children with cerebral palsy often have visual difficulties that are not acuity problems and that are not correctable with a standard lens. Vision therapy has demonstrated good results when emphasis is placed on ocular motility and accommodation.140 When children were given intense visuo-oculomotor training, improvement was noted in visuo-oculomotor control.141 Improvement in the child’s ability to execute smooth pursuit precision and maximum velocity, improvement of saccadic movement precision and stability, and shortening of the saccadic reaction time were significant after training.141 Although many clinicians are not experts in the area of vision, vision is an important part of every therapy session. Incorporating vision as an integral part of a therapy session will not only improve the child’s orientation in space but will address his or her ability to scan the environment while learning to move through space.
Medical influences on treatment
Because the problems of cerebral palsy are so varied, the condition lends itself to diverse interventions, some of which have a longer life than others. Management of spasticity has always been an area of great concern and interest, and over the years several treatments have been offered to control this positive sign. Various medications have been used to control spasticity; baclofen, diazepam, and dantrolene remain the three most commonly used pharmacological agents in the treatment of spastic hypertonia.142 (See Chapter 36 for additional information.) The baclofen pump has been used in children with excessive spasticity. This pump is implanted in the lower abdomen with a catheter leading to the intrathecal space for the administration of the drug. This treatment for spasticity has been effective for some types of cerebral palsy but led to complications in some patients with mixed cerebral palsy, low body weight, younger age, gastrostomy tubes, and nonambulatory status.143–145
The cerebellar implant so popular in the late 1970s offered the possibility of regulating tone by supplementing cerebellar inhibition.146–149 As time passed, the procedure was used less often, and patients had difficulty getting repairs or replacement parts for the implant. The procedure that largely replaced the cerebellar implant was the placement of four electrodes in the cervical area to offer more control over postural tone.150 These had the advantage of being adjustable so that the individual or a family member could make daily choices as to the optimal tone distribution. In some cases early success gave way to disappointment as the system adapted to the inputs. In some cases the child or adolescent had to make a decision whether movement or speech was more important on a given day. Therapy was always recommended after the procedure, although the nature of the specific program was left to the family to decide. The success of the cerebellar stimulator is considered moderate when used on a select group of individuals with cerebral palsy.146–149 Other, more recent spasticity management programs are less invasive and are often considered before use of this invasive procedure.
In 1968 a posterior rhizotomy surgical intervention was developed, with some success reported in reducing spasticity.151,152 It remained for Peacock and Arens153 to apply the procedure more selectively and functionally and to bring it to the United States from South Africa. On the basis of their experience, Peacock and colleagues insisted on daily neurodevelopmental (Bobath) treatment for at least 1 year after the surgical intervention. Electromyographic testing before and during the surgery is used to determine which posterior nerve rootlets are creating the spasticity in the lower extremities.154 The foundations for success are accurate selection of the child, an experienced surgeon, and careful analysis of therapy goals.
A more recent improvement in the selective dorsal rhizotomy (SDR) procedure was developed by Lazareff and colleagues,155 who enter a limited number of levels rather than five levels of the spinal column and prefer to work close to the cauda equina, according to the technique of Fasano.156 Several studies have documented improvement in function and strength and reduction of spasticity outcomes as far out as 3 to 5 years.151,157 In a more recent longitudinal study by Nordmark and co-workers,158 it was found that SDR was safe and effective in reducing spasticity without major complications. When combined with physical therapy and careful selection of candidates for the procedure, the functional outcomes over a period of 5 years were lasting. Trost and colleagues159 reported on differences between preoperative and postoperative measures: the Ashworth scale for spasticity, the Gillette Gait Index, oxygen cost for gait efficiency, and the Gillette Functional Assessment Questionnaire for functional mobility. All outcome measures demonstrated improvement for the 136 subjects as a whole. Careful selection of the appropriate candidate for this surgery followed by intense therapy intervention is essential for the success of the procedure and for optimizing motor outcomes.
A new approach to controlling spasticity is percutaneous radiofrequency lesions of dorsal root ganglion (RF-DRG), a noninvasive procedure that has been reported in the literature recently. Vles and colleagues160 performed a pilot study of 17 patients with a diagnosis of cerebral palsy. They reported that this new treatment is promising for reducing spasticity and improving function in children with cerebral palsy. Further investigation into this treatment is necessary to assess its effectiveness.
Alcohol (phenol) blocks and the use of botoxin (botulinum toxin) (BtxA) have been used locally to affect a change in the individual muscle or motor point injected.142,161–167 Both orthopedists and neurologists have taken an interest in the use of botoxin to block selected muscle responses for a temporary period. BtxA has been reported to have fewer side effects than the phenol blocks and is now considered the drug of choice for this type of procedure.130 These conservative interventions serve to delay surgery until the child is more capable of responding to postsurgical therapy programs. Botulinum toxin injection combined with serial casting has been shown to improve range of motion, muscle tone, and dynamic spasticity in ambulatory children with cerebral palsy.135 Therapists should be involved in the decision-making process of determining interventions for reduction of spasticity because they often are the most familiar with the child’s movement strategies and the postural changes that occur in muscle tone as the child moves against gravity.
Orthopedic surgical intervention continues to be effective in cerebral palsy when there are tendon contractures or specific structural limitations that are not accompanied by excessive levels of spasticity.168,169 In any surgery the outcome is much improved by close coordination between therapist and surgeon, with a functional orientation toward goal setting for the child. Early standing after surgery and use of dynamic footplates inside the casts and orthotics after cast removal will generally improve functional outcomes. Bony surgeries that offer better joint stability are usually planned for the termination of growth. The orthopedist is also able to guide conservative positioning measures to prevent hip problems resulting from spasticity while direct treatment intervention continues. Bracing of the trunk, which is sometimes warranted for scoliosis or kyphosis, is prescribed by the orthopedist. Surgical intervention for spinal deformities is determined by the physician, with consideration of the child’s age, condition, and health and the degree of curvature.
Children with cerebral palsy differ in their ability to relax completely during sleep, and a small number of these children can benefit from inhibitive casting or night bracing. More often this type of positioning is used during therapy sessions and independent ambulation to combine control with weight bearing.170 The orthopedist should participate in any plan for prolonged immobilization or temporary casting that will be used on a 24-hour schedule, such as serial casting to improve range of motion.171,172 A variety of lower-extremity bracing is available, and its selection is dependent on the segment to control and the outcomes sought in positioning or dynamic action, as in ambulation (Figure 12-25).
Equipment
Equipment recommendations must take into account the physical space in the home and the amount of direct treatment available to the child (Figure 12-26). Young children in particular can often use normal seating with slight adaptations. This not only is more socially and financially acceptable but also permits changes as required by the child’s developmental progress. The portability of supportive seats or standers encourages the family to take the apparatus along for weekend outings or visits to relatives. Chair designs should place children at an age-appropriate level in their environments. This permits a better quality of visual exploration and facilitates social exchange with siblings and visiting peers. When planning the amount of physical support needed by the child, the therapist considers varying the structural control in relation to activity (Figure 12-27). The child who is merely watching the play of others or a television presentation may successfully control trunk and head balance independently with minimal support. However, concentration on hand skills or self-feeding may necessitate trunk control assistance via a chair insert to avoid the child’s use of compensatory reactions. As postural reactions become more integrated and hence more automatic, support should be diminished. There are now several options available to the consumer on the internet. Families and therapists alike can search online for commercially available products and alternatives to commercially available products.
Adaptive equipment is not the only type of equipment that the therapist must consider for clients. Conditioning and strengthening, now recognized as beneficial to children and adults with cerebral palsy, open the door for equipment that lends itself to these parameters.107–114 Exercise bikes, treadmills (see Figure 12-22), light weights (see Figure 12-24), and balance equipment (Figure 12-28) are all valuable adjuncts to a home exercise program and should be considered, when appropriate, for a particular individual. Many of the commercially available items found at a sporting goods store can be well adapted to fit the needs of the higher functioning person with cerebral palsy. With more emphasis on working out, sports equipment can even be found in discount stores. Offering to adapt equipment for your clients can encourage and increase compliance with exercises given for home exercise programs.
Alternative therapies
Hyperbaric oxygen treatment is gaining popularity as a treatment for cerebral palsy in children. Clinics are beginning to spring up worldwide for this type of therapy. Research on this treatment has been inconclusive, and scientific evidence for its efficacy is lacking.173,174 Clinicians should keep abreast of the latest developments in the treatment of cerebral palsy and inform families about the pros and cons of designer treatments. Currently the Undersea and Hyperbaric Medicine Society (UHM) states that there is not enough evidence to recommend the use of hyperbaric oxygen therapy for cerebral palsy.175,176 A systematic review by McDonagh and colleagues177 found that there was no significant difference between pressurized air versus room air pressure and that the subjects in both groups made gains. This topic remains controversial even within the UHM. Several articles and editorials have been written with the overwhelming conclusion that randomized clinical trials should be carried out to determine the effectiveness of this treatment.
The Adeli suit is a compression garment with bungee cord–like elastic cords attached to the suit, along the trunk and extremities. This suit, once referred to as the therapeutic space suit or treatment-loading suit, was developed for Russian cosmonauts to counteract the adverse effect of long-term zero gravity on the skeletal muscles.178 There are a few studies that suggest that there are benefits for children with cerebral palsy when they receive therapy in the suit.175,178–181 The suit allows for controlled practice of activities with resistance, and assistance when necessary; the cords are attached in a variety of ways to give different types of practice repetitions. As is prescribed by the proponents of this approach, intense practice is warranted to reap the benefits. This therapy is expensive, and the suit, if bought to use at home, is also very expensive. Rosenbaum175 has suggested that the benefits of this therapy vary with the type and severity of the involvement, the child’s ability to participate in controlled movement, and the tolerance to wearing the suit for extended periods of time. In Australia the Upsuit, described by Blair et al as being made of a stretchy material, has been investigated for use with children with cerebral palsy.182 Similar results have been noted by Chauvel et al that the type of cerebral palsy and the person’s ability to participate in movement forecast the potential outcomes.183 The Upsuit was also noted to compromise lung capacity, which interfered with the child’s ability to participate.182 As clinicians, it is important for us to stay abreast of the latest developments and to provide families with reasonable alternatives. Although intense practice is well known in the literature as being beneficial for motor learning, the addition of the suit brings in a component that “appears” to provide stability and graded control during practice. Caution when describing this approach to families is warranted because some evidence suggests that it may not be appropriate for every child with cerebral palsy. The long-term effects and measurable outcomes after the use of the Adeli suit and the Upsuit are not documented in the literature.175,184,185 The following questions must be asked: What happens to the motor abilities of the child when the suit is removed? Has the suit actually prevented the development of postural antigravity coactivation of the trunk and proximal axial joints?
In the mid-1980s Pape186 published a case series involving five children with cerebral palsy receiving therapeutic (subthreshold) ES. Reported from this case series was that overnight use of low-intensity ES in combination with standard therapy demonstrated significant improvement in gross motor, balance, and locomotor skills as measured by the Peabody Developmental Motor Scales in children with mild cerebral palsy.186 Results reported were based on observations by individuals who were not blinded to the purpose of the study, and therefore the research design was biased. In a follow-up study Steinbok and colleagues187 followed children who had undergone selected dorsal rhizotomy and received therapeutic ES for 1 year. Although this study reported improvement in gross motor function, no other measures were changed: range of motion, spasticity, or strength. Two well-controlled clinical trials investigating this method of threshold electrical stimulation (TES) delivery concluded that no objective effects on motor or ambulatory function or clinical benefit for children and youths with cerebral palsy were detected.188,189 In two separate randomized placebo-controlled clinical trials using TES, the results indicated no significant clinical benefit observed when compared with neuromuscular ES.188,190 (Refer to Chapter 9 for additional discussion.) Parents often report changes with this therapy, but the objective measures do not demonstrate significant results. Clinicians in the field have reported that overnight use of subthreshold ES builds muscle bulk, but unless combined with active participation of the musculature, overall improvement in movement may not be seen. This therapy, for children with cerebral palsy, requires a special stimulation unit that is subthreshold and capable of being used at night and has a shutoff setting that is activated if the electrodes become disconnected from the child. The unit is costly and further requires a clinician who is specially trained in its use to evaluate and periodically update the treatment protocol. Significant benefits for this type of ES have not been documented.
The Peto method or “conductive education” (CE), developed by Andres Peto in Budapest after World War II, has been used in children with disabilities.191 This approach is an educational versus medical model, as the name implies, and the focus is on the many aspects of child development.192 It is based on practice and repetition combined with verbal guidance of a trainer (conductor) and self-verbalization by the child as he or she performs the task or activity.175 Most of the claims that promote its value have come from the Peto Institute in Budapest, Hungary. The institute has been very selective in choosing candidates for this approach on the basis of the child’s potential for independent mobility and function with a good overall prognosis.175,191,193 Research into this method of delivery of services to children with cerebral palsy has been sparse outside the Peto Institute’s studies. In two studies in Australia, CE was found to have encouraging results in developmental changes.194,195 In a randomized controlled study with children assigned to a CE group or a neurodevelopmental intervention group, no significant differences were noted in the two groups.198 This approach advocates intense practice of all skills, motor and educational, with emphasis on self-doing regardless of whether a compensatory pattern is used. Various pieces of equipment are used to facilitate independent skills: wooden slatted beds to allow the child to pull and maneuver, and wooden ladders mounted on the wall to assist with dressing and transitions. The literature on CE does stress the concept of intense practice for motor learning. Similarly, promoting practice in the CE environment must transfer to home and community for carryover to everyday life situations.63 To fully optimize the outcomes of CE, a commitment from the family is essential, as is the case in most therapeutic approaches. Further investigation into this approach is warranted before this philosophy is fully supported. For a selected group of individuals, CE research results seem hopeful, although transfer to unpracticed tasks and different environments may be minimal.197–199
The Feldenkrais method was developed by an Israeli engineer, Moshe Feldenkrais, while looking for a solution to his own knee problem. (Refer to Chapter 39 for additional discussion.) He started analyzing body alignment for more efficient movement.200,201 This form of body work has been used to help dancers, gymnasts, and other skilled persons improve their performance. Some therapists have undertaken the long training necessary to understand typical movement in more detail and to improve the movement coordination of their clients with neuromotor challenges. There is no published research on this method, but several books and training courses exist that promote its use. In a review article by Liptak184 on alternative interventions, the Feldenkrais method is described; however, no articles have been published examining its use with children who have cerebral palsy.
Ida Rolf, trained in physics, had a son with some postural disorganization.202 She developed a structural approach, called the Rolfing technique, to improve body alignment; the technique uses specific release of deep soft tissue to restore effortless postural control against gravity.203 She was able to make positive changes in the movement patterns of many children with cerebral palsy, but she never claimed to treat the disorder itself. This approach requires special training in the Rolfing technique, which is a type of deep tissue massage.
Dr. William Sutherland,204 an osteopathic physician, developed direct treatment of the cranium, which is referred to commercially as cranial therapy or cranial sacral treatment. (Refer to Chapter 39 for additional information.) This type of therapy is believed to have wide application to many disabilities and conditions.205 Today, there are persons trained at many different levels, so the family of a child with cerebral palsy seeking this treatment will need to be certain that the practitioner is a professional and that she or he has experience with small children.206 Cranial treatment is purported to restore the physiological motion of the craniosacral system, improving circulation of fluids to the brain as well as respiratory function, to which it is believed to be closely linked. Research has been encouraged in this area to substantiate the claims of this approach.
Developing a personal philosophy of treatment
The practicing therapist continues to learn much about the nuances of typical human development (see Chapter 3).207 The dynamic interaction of developmental movement components becomes more significant as the therapist acquires greater clinical experience and recognizes developmental change as a reflection of central nervous system maturation. Increasing knowledge of the functional nature of sensory systems and central nervous system processing will influence the choice of treatment techniques. Direct intervention will have more depth and specificity to improve the child’s control of posture and movement while the therapist appreciates the complex interaction of developmental factors in cerebral palsy. On the basis of individual experience, each therapist develops a personal philosophy of treatment that incorporates new research findings and evolving perceptions of the problem of central nervous system dysfunction. Without a philosophical or theoretical orientation for decision making, the therapist may succumb to following each promising treatment idea that is learned without having a clear image of the potential benefits for the specific client. “Commercial” programs may benefit the child whose needs match the program objectives. An “individualized” program adapts to the needs of the particular child and is shaped by the response of that child during therapy. Without an internalized treatment goal toward which independent techniques are applied, the result may remain ineffective and unconvincing. The therapist in a direct treatment situation must develop a concise visualization of what is to be achieved in each session with the individual child based on a sound foundation. The repetition and practice that are so critical for learning must often be carried out at home, and the therapist becomes responsible for family instruction. Home exercise programs must be tailored for both the child and the family situation and must be in alignment with the goals and expectations of the family. These programs need to be practical, fun ideas for practice that can be incorporated into the child’s home life with reasonable assurance that the activities can and will be carried out regularly. Creative therapeutic ideas for playtime, dressing, grooming, mealtime, and relaxation time are best addressed in the home exercise program because these are everyday tasks that every family encounters and the family is likely to be compliant.208 The time spent in therapy throughout the week cannot substitute for all the hours spent at home and school.
Involving the family
To be successful, therapy for the child with cerebral palsy includes active family participation. Variability of practice in different environments tends to promote more effective motor learning, and parents who learn to help their child early begin to understand the importance of their participation as well as the nature of their child’s disability. Parents are in the process of healing their own self-image, which was so injured when they learned of their child’s disability. They should not be expected to become therapists per se but should learn to observe small gains in treatment sessions that offer insight into the child’s current strengths and weaknesses.17
Parents need to adapt their expectations in keeping with the child’s continuing change and emotional maturity. Parenting a child with cerebral palsy is no easy task, and the therapist will do well to develop respect for this demanding role. No one provides more for the child with cerebral palsy than the nurturing parent who guides the child to self-acceptance of limitations without destroying personal initiative. This is the child who most often becomes an independent working adult (Figure 12-29).
Role of the therapist in indirect intervention
Communication for the nonverbal client with cerebral palsy must be an integral part of the therapy or school program.209 A simple start may be made with pictures to permit choices in food, clothing, and therapy activities. The parents need encouragement to begin the process of letting the child make some simple choices in food, clothing, or preferred activities. Although computers have their place, the child should have the communication device with him or her at all times. Language development in the young child is enhanced by having this type of alternative communication device available while articulation is still difficult. Use of head movement is a powerful influence on muscle tone changes that may cause negative regression in postural or visual control. Care and consideration should be taken when evaluating the body part to access the device. Postural and visual control is essential toward the goal of better function and communication. A solution that was successful with one 9-year-old athetoid girl was moving the elbow back to a switch mounted on the vertical bar of the wheelchair backrest to access her communication device. Any activity that is repeated on a daily basis should be examined in light of possible interference by atypical patterns.
Affordable electronic systems with voice recording, portability, and growth features are available. Communication, which can be achieved by coordinating efforts with the speech pathologist, can make the difference between passivity and active participation in the environment.209 Play can be encouraged with the use of switch toys and touch-screen computers. Many new programs are being developed for computers and electronic interactive books.
Therapy in the community
Therapists are often concerned with body functions and structure and neglect to address participation in real-life activities such as school attendance, sports, employment, and involvement in the community.210 Children with mild dysfunction as a result of cerebral palsy may be successfully incorporated into physical education (PE) classes if the teacher is prepared to make some small adaptations. Teachers generally appreciate the opportunity to discuss with the therapist specific limitations of the child and those movements that should be encouraged. Taking the opportunity to meet with the PE coach to establish adaptations and modifications or appropriate participation in activities is time well spent for the child’s integration into the class. PE class is often rewarding for the child and important in establishing peer relationships. For better success the child with functional limitations can be incorporated into a class that follows the British form of movement education, which places much less emphasis on intragroup competition and encourages each child to progress at her or his own rate.
It is important to keep direct, active treatment available for older children, adolescents, and adults who are motivated to change. Now that more effective procedures are available for changing some of the basic neurophysiological movement characteristics observed in children with cerebral palsy, it is possible to achieve change with direct treatment of the older client. The adolescent often responds best to short-term, goal-oriented therapy programs that are patient centered. Motor learning concepts are better understood by both the therapist and the client and can be incorporated in activities after mobilizing tissues that have been unused for so many years (see Chapters 4 and 9). With current program directions, many older clients may not have had the opportunity for direct treatment over time by a qualified therapist. For the minimally involved teenager, young adult, and adult with cerebral palsy the local gym offers an alternative to direct therapy. General conditioning is very popular in community programs including weight training, endurance training, water exercises, yoga, and walking programs. A therapist can be consulted to establish an appropriate program for the individual who wants to work out at the gym on equipment, attend special classes that are offered, or work out in the pool. When asked, it is the therapist’s area of expertise to help identify and make recommendations regarding functional movement and activity participation for adults with developmental disabilities such as cerebral palsy. (See the section in Chapter 35 on adults with developmental disabilities.) The movement toward a health orientation as opposed to crisis intervention for illness will also affect services for children and adults with cerebral palsy. This population does not have an illness or an active disease process, and they strive to lead as normal a life as possible. Many adults with neuromotor disabilities express their preference to participate in the decisions that are made for them regarding their ultimate lifestyle and participation in the community. The therapist who works with this population should familiarize himself or herself with the patient’s living situation—family home, group home, or independent living—as well as the support system and work environment if applicable. These factors should be considered when establishing a viable program. Many opportunities for employment and volunteerism exist in communities for individuals with disabilities. This may require that the therapist venture into the workplace to assess accessibility and modifications that can be done in that environment to make for successful integration of the individual into the community. Optimal health for the adult with cerebral palsy has yet to be described, and much more data must be collected. However, it is an exciting time as our society moves forward in its views and acknowledgment of disability (see Chapter 35).
Psychosocial factors in cerebral palsy
Parental guidance of the child with functional limitations is also influenced by the adults’ adaptation to their offspring’s problem. Parents need to resolve in their own way the emotional impact of the child’s disability. Parents need time to grieve the loss of dreams they had for their child, and each person will approach this in his or her own way and time. Each major milestone anticipated in a typical child’s life may bring on the grieving process again. Most parents feel inadequate, ignorant, and relatively helpless at being unable to remedy the situation for their child. They need help in feeling good about themselves before they can effectively guide the child toward self-acceptance as an adequate human being. Parents need guidance to provide themselves with opportunities to rest and renew their energies. Therapists can be instrumental during this process by remaining nonjudgmental. (Refer to Chapter 6 for additional information.)
Documentation
Developing a plan of care (POC) with objective measurable goals is required for documentation of progress in intervention and reimbursement from third-party payers. (Refer to Chapter 10 for additional recommendations.) Carefully extracting a child’s strengths and weaknesses from the assessment should drive the POC. Using timed measures, distance, number of repetitions, standardized tools, and other measurable outcomes provides a source of encouragement for families and justification for continued intervention.
Methods of intervention or treatment are measurable for research and applicable to the functional problems presented by a diagnosis of cerebral palsy. Once a specific research question has been formulated, systematic recordings of appropriate data can be gathered over time to accumulate data for a viable study. There is value in longitudinal reporting of a single case or a small group of individuals who have some characteristics in common because this aids our understanding of what we need to prevent in the young child to permit optimal function later. (See Chapters 8 and 10 for suggestions of impairment and disability measurements to be used as objective measures for functional outcome studies and record keeping.) Clinicians have a difficult time putting into words exactly what takes place during intervention, which further complicates research investigation into the efficacy of treatment. Descriptive analysis of treatment is essential to document and begin to understand what a therapist does during a therapy session. Understanding what takes place in therapy will help identify questions that could be investigated more closely.
The way in which therapists learn to view a problem determines, to a large extent, the potential range of solutions available to them. Cerebral palsy is a complex of motor and movement inabilities that cluster about the inadequacy of central nervous system control, visual and soft tissue restrictions, and the amazing ability of the human body to compensate. Therapists need to look critically at developmental processes, qualities of movement, postural adjustments, timing and limitations of movements, and the range of dynamic functional movement. New areas of motor learning and systems and chaos theories offer the researcher novel approaches to the challenge of cerebral palsy and the resultant disorder of posture control and movement learning. Environmental factors may have as much influence as specific central nervous system limitations. Early intervention should be analytical, specific, and based on a theoretical foundation. Posture and movement control begins to change with direct treatment. Analysis of the postural components and movement characteristics of children with cerebral palsy will lead to meaningful research more quickly than will professional reliance on the traditional definitions of the medical condition. Thorough documentation of therapy progress using objective measures is critical for development of more effective intervention strategies in the future (see Chapter 10).
*This chapter is dedicated to Christine Nelson—master clinician, true friend, and mentor. Her gifts as a clinician and artistic eclectic approach to the treatment of children were unmatched and often seemed beyond what one could comprehend. She ever changed those she touched and enlightened all those she taught. Christine will be forever missed and yet her gift of touch will be everlasting and live on in her patients, students, and friends.