Chapter 53 Maintenance and Replacement Therapy
Maintenance intravenous fluids are used in a child who cannot be fed enterally. Along with maintenance fluids, children may require concurrent replacement fluids if they have continued excessive losses, such as may occur with drainage from a nasogastric (NG) tube or with high urine output due to nephrogenic diabetes insipidus. If dehydration is present, the patient also needs to receive deficit replacement (Chapter 54). A child awaiting surgery may need only maintenance fluids, whereas a child with diarrheal dehydration needs maintenance and deficit therapy and also may require replacement fluids if significant diarrhea continues.
Maintenance Therapy
Children normally have large variations in their daily intake of water and electrolytes. The only exceptions are patients who receive fixed dietary regimens orally, via a gastric tube, or as intravenous total parenteral nutrition. Healthy children can tolerate significant variations in intake because of the many homeostatic mechanisms that can adjust absorption and excretion of water and electrolytes (Chapter 52). The calculated water and electrolyte needs that form the basis of maintenance therapy are not absolute requirements. Rather, these calculations provide reasonable guidelines for a starting point to estimate intravenous therapy. Children do not need to be started on intravenous fluids simply because their intake is being monitored in a hospital and they are not taking “maintenance fluids” orally, unless there is a pathologic process present that necessitates high fluid intake.
Maintenance fluids are composed of a solution of water, glucose, sodium, and potassium. This solution has the advantages of simplicity, long shelf life, low cost, and compatibility with peripheral intravenous administration. Such a solution accomplishes the major objectives of maintenance fluids (Table 53-1). Patients lose water, sodium, and potassium in their urine and stool; water is also lost from the skin and lungs. Maintenance fluids replace these losses and therefore avoid the development of dehydration and deficiency of sodium or potassium.
Maintenance Water
The goal of maintenance water is to provide enough water to replace these losses. Although urinary losses are approximately 60% of the total, the normal kidney has the ability to markedly modify water losses, with daily urine volume potentially varying by more than a factor of 20. Maintenance water is designed to provide enough water so that the kidney does not need to significantly dilute or concentrate the urine. It also provides a margin of safety, so that normal homeostatic mechanisms can adjust urinary water losses to prevent overhydration and dehydration. This adaptability obviates the need for absolute precision in determining water requirements. This fact is important, given the absence of absolute accuracy in the formulas for calculation of water needs. Table 53-2 provides a system for calculating maintenance water on the basis of the patient’s weight and emphasizes the high water needs of smaller, less mature patients. This approach is reliable, although calculations based on weight do overestimate the water needs of an overweight child, in whom it is better to base the calculations on the lean body weight, which can be estimated by using the 50th percentile of body weight for the child’s height. It is also important to remember that there is an upper limit of 2.4 L/24 hr in adult-sized patients. Intravenous fluids are written as an hourly rate. The formulas in Table 53-3 enable rapid calculation of the rate of maintenance fluids.
Table 53-2 BODY WEIGHT METHOD FOR CALCULATING DAILY MAINTENANCE FLUID VOLUME
| BODY WEIGHT | FLUID PER DAY |
|---|---|
| 0-10 kg | 100 mL/kg |
| 11-20 kg | 1,000 mL + 50 mL/kg for each kg >10 kg |
| >20 kg | 1,500 mL + 20 mL/kg for each kg >20 kg* |
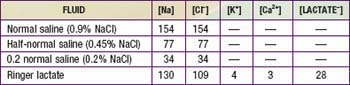
Intravenous Solutions
The components of the commonly available solutions are shown in Table 53-4. Normal saline (NS) and Ringer lactate (LR) are isotonic solutions; they have approximately the same tonicity as plasma. Isotonic fluids are generally used for the acute correction of intravascular volume depletion (Chapter 54). The usual choices for maintenance fluid therapy in children are half-normal saline ( ) and 0.2NS. These solutions are available with 5% dextrose (D5). In addition, they are available with 20 mEq/L of potassium chloride, 10 mEq/L of potassium chloride, or no potassium. A hospital pharmacy can also prepare custom-made solutions with different concentrations of glucose, sodium, or potassium. In addition, other electrolytes, such as calcium, magnesium, phosphate, acetate, and bicarbonate, can be added to intravenous solutions. Custom-made solutions take time to prepare and are much more expensive than commercial solutions. The use of custom-made solutions is necessary only for patients who have underlying disorders that cause significant electrolyte imbalances. The use of commercial solutions saves both time and expense.
) and 0.2NS. These solutions are available with 5% dextrose (D5). In addition, they are available with 20 mEq/L of potassium chloride, 10 mEq/L of potassium chloride, or no potassium. A hospital pharmacy can also prepare custom-made solutions with different concentrations of glucose, sodium, or potassium. In addition, other electrolytes, such as calcium, magnesium, phosphate, acetate, and bicarbonate, can be added to intravenous solutions. Custom-made solutions take time to prepare and are much more expensive than commercial solutions. The use of custom-made solutions is necessary only for patients who have underlying disorders that cause significant electrolyte imbalances. The use of commercial solutions saves both time and expense.
Maintenance Fluids and Hyponatremia
Patients with other potential causes of ADH production must have careful monitoring of their electrolytes and fluid input and output. Patients with possible subtle volume depletion (Chapter 54) should receive 20 mL/kg (maximum of 1 L) of isotonic fluid (NS, LR) over 1-2 hr to restore their intravascular volume before maintenance fluids are initiated. The patient can then be switched to D5  + 20 mEq/L KCl at a standard maintenance rate. Patients of any weight with possible volume depletion should not routinely receive fluids with 0.2NS, unless there is a specific indication. Patients who are at risk for producing ADH owing to etiologies other than volume depletion may need to receive less than maintenance fluids to avoid hyponatremia.
+ 20 mEq/L KCl at a standard maintenance rate. Patients of any weight with possible volume depletion should not routinely receive fluids with 0.2NS, unless there is a specific indication. Patients who are at risk for producing ADH owing to etiologies other than volume depletion may need to receive less than maintenance fluids to avoid hyponatremia.
Variations in Maintenance Water and Electrolytes
The calculation of maintenance water is based on standard assumptions regarding water losses. There are patients, however, in whom these assumptions are incorrect. To identify such situations, it is helpful to understand the source and magnitude of normal water losses. Table 53-5 lists the 3 sources of normal water loss.
Table 53-6 lists a variety of clinical situations that modify normal water and electrolyte losses. The skin can be a source of very significant water loss, particularly in neonates, especially premature infants, who are under radiant warmers or are receiving phototherapy. Very low birthweight infants can have insensible losses of 100-200 mL/kg/24 hr. Burns can result in massive losses of water and electrolytes, and there are specific guidelines for fluid management in children with burns (Chapter 68). Sweat losses of water and electrolytes, especially in a warm climate, can also be significant. Children with cystic fibrosis have increased sodium losses from the skin. Some children with pseudohypoaldosteronism also have increased cutaneous salt losses.
| SOURCE | CAUSES OF INCREASED WATER NEEDS | CAUSES OF DECREASED WATER NEEDS |
|---|---|---|
| Skin | Radiant warmer | Incubator (premature infant) |
| Phototherapy | ||
| Fever | ||
| Sweat | ||
| Burns | ||
| Lungs | Tachypnea | Humidified ventilator |
| Tracheostomy | ||
| Gastrointestinal tract | Diarrhea | — |
| Emesis | ||
| Nasogastric suction | ||
| Renal | Polyuria | Oliguria/anuria |
| Miscellaneous | Surgical drain | Hypothyroidism |
| Third spacing |
Replacement Fluids
The gastrointestinal (GI) tract is potentially a source of considerable water loss. GI water losses are accompanied by electrolytes and thus may cause disturbances in intravascular volume and electrolyte concentrations. GI losses are often associated with loss of potassium, leading to hypokalemia. Because of the high bicarbonate concentration in stool, children with diarrhea usually have a metabolic acidosis, which may be accentuated if volume depletion causes hypoperfusion and a concurrent lactic acidosis. Emesis or losses from an NG tube can cause a metabolic alkalosis (Chapter 52).
Diarrhea is a common cause of fluid loss in children. It can cause dehydration and electrolyte disorders. In the unusual patient with significant diarrhea and a limited ability to take oral fluid, it is important to have a plan for replacing excessive stool losses. The volume of stool should be measured, and an equal volume of replacement solution should be given. Data are available on the average electrolyte composition of diarrhea in children (Table 53-7). With use of this information, it is possible to design an appropriate replacement solution. The solution shown in Table 53-7 replaces stool losses of sodium, potassium, chloride, and bicarbonate. Each 1 mL of stool should be replaced by 1 mL of this solution. The average electrolyte composition of diarrhea is just an average, and there may be considerable variation. It is therefore advisable to consider measuring the electrolyte composition of a patient’s diarrhea if the amount is especially excessive or if the patient’s serum electrolyte levels are problematic.
Table 53-7 REPLACEMENT FLUID FOR DIARRHEA
AVERAGE COMPOSITION OF DIARRHEA
APPROACH TO REPLACEMENT OF ONGOING LOSSES
Loss of gastric fluid, via either emesis or NG suction, is also likely to cause dehydration, in that most patients with either condition have impaired oral intake of fluids. Electrolyte disturbances, particularly hypokalemia and metabolic alkalosis, are also common. These complications can be avoided by judicious use of a replacement solution. The composition of gastric fluid shown in Table 53-8 is the basis for designing a replacement solution.
Table 53-8 REPLACEMENT FLUID FOR EMESIS OR NASOGASTRIC LOSSES
AVERAGE COMPOSITION OF GASTRIC FLUID
APPROACH TO REPLACEMENT OF ONGOING LOSSES
Patients with gastric losses frequently have hypokalemia, although the potassium concentration of gastric fluid is relatively low. The associated urinary loss of potassium is an important cause of hypokalemia in this situation (Chapter 52). These patients may need additional potassium either in their maintenance fluids or in their replacement fluids to compensate for prior or ongoing urinary losses. Restoration of the patient’s intravascular volume, by decreasing aldosterone synthesis, lessens the urinary potassium losses.
The approach to decreased or increased urine output is similar (Table 53-9). The patient receives fluids at a rate to replace insensible losses. This is accomplished by a rate of fluid administration that is 25-40% of the normal maintenance rate, depending on the patient’s age. Replacing insensible losses in the anuric child will theoretically maintain an even fluid balance, with the caveat that 25-40% of the normal maintenance rate is only an estimate of insensible losses. In the individual patient, this rate is adjusted on the basis of monitoring of the patient’s weight and volume status. Most children with renal insufficiency receive little or no potassium because the kidney is the principal site of potassium excretion.
Most children with polyuria (except in diabetes mellitus; Chapter 583) should be started on replacement of insensible fluid plus urine losses. This approach avoids the need to attempt to calculate the volume of urine output that is “normal” so that the patient can be given replacement fluid for the excess. In these patients, urine output is, by definition, excessive, and it is important to measure the sodium and potassium concentrations of the urine to help in formulating the urine replacement solution.
Armon K, Riordan A, Playfor S, et al. Hyponatraemia and hypokalaemia during intravenous fluid administration. Arch Dis Child. 2008;93:285-287.
Au AK, Ray PE, McBryde KD, et al. Incidence of postoperative hyponatremia and complications in critically-ill children treated with hypotonic and normotonic solutions. J Pediatr. 2008;152:33-38.
Choong K, Kho ME, Menon K, et al. Hypotonic versus isotonic saline in hospitalised children: a systematic review. Arch Dis Child. 2006;91:828-835.
Coulthard MG. Will changing maintenance intravenous fluid from 0.18% to 0.45% saline do more harm than good? Arch Dis Child. 2008;93:335-340.
Hilton AK, Pellegrino VA, Scheinkestel CD. Avoiding common problems associated with intravenous fluid therapy. Med J Aust. 2008;189:509-513.
Jacob M, Chappell D, Rehm M. Clinical update: perioperative fluid management. Lancet. 2007;369:1984-1986.
Neville KA, Verge CF, Rosenberg AR, et al. Isotonic is better than hypotonic saline for intravenous rehydration of children with gastroenteritis: a prospective randomised study. Arch Dis Child. 2006;91:226-232.
Yung M, Keeley S. Randomised controlled trial of intravenous maintenance fluids. J Paediatr Child Health. 2009;45:9-14.

 + 20 mEq/L KCl (osmolality = 472) can be administered.
+ 20 mEq/L KCl (osmolality = 472) can be administered. . The other recommends that normal saline be used as the maintenance fluid; most centers have not adopted the routine use of NS as the initiating maintenance solution.
. The other recommends that normal saline be used as the maintenance fluid; most centers have not adopted the routine use of NS as the initiating maintenance solution. + 20 mEq/L KCl or D5 0.2NS + 20 mEq/L KCl. Children weighing less than approximately 10 kg do best with the solution containing 0.2NS because of their high water needs per kilogram. Larger children and adults may receive the solution with
+ 20 mEq/L KCl or D5 0.2NS + 20 mEq/L KCl. Children weighing less than approximately 10 kg do best with the solution containing 0.2NS because of their high water needs per kilogram. Larger children and adults may receive the solution with  . These guidelines assume that there is no disease process present that would require an adjustment in either the volume or the electrolyte composition of maintenance fluids (children with renal insufficiency may be hyperkalemic or unable to excrete potassium and may not tolerate 20 mEq/L of potassium). These solutions work well in children who have normal homeostatic mechanisms for adjusting urinary excretion of water, sodium, and potassium. In children with complicated pathophysiologic derangements, it may be necessary to empirically adjust the electrolyte composition and rate of maintenance fluids on the basis of electrolyte measurements and assessment of fluid balance. In all children, it is critical to carefully monitor weight, urine output, and electrolytes to identify overhydration or underhydration, hyponatremia, and other electrolyte disturbances, and to then adjust the rate or composition of the intravenous solution accordingly.
. These guidelines assume that there is no disease process present that would require an adjustment in either the volume or the electrolyte composition of maintenance fluids (children with renal insufficiency may be hyperkalemic or unable to excrete potassium and may not tolerate 20 mEq/L of potassium). These solutions work well in children who have normal homeostatic mechanisms for adjusting urinary excretion of water, sodium, and potassium. In children with complicated pathophysiologic derangements, it may be necessary to empirically adjust the electrolyte composition and rate of maintenance fluids on the basis of electrolyte measurements and assessment of fluid balance. In all children, it is critical to carefully monitor weight, urine output, and electrolytes to identify overhydration or underhydration, hyponatremia, and other electrolyte disturbances, and to then adjust the rate or composition of the intravenous solution accordingly. of the calculated maintenance rate. Subsequent maintenance fluids should contain
of the calculated maintenance rate. Subsequent maintenance fluids should contain  , even in smaller patients, unless there is a specific indication to use 0.2NS. Electrolytes should be measured at least daily.
, even in smaller patients, unless there is a specific indication to use 0.2NS. Electrolytes should be measured at least daily. of total maintenance water (40% in infants and closer to 25% in adolescents and adults). Insensible losses are composed of evaporative losses from the skin and lungs that cannot be quantitated. The evaporative losses from the skin do not include sweat, which would be considered an additional (sensible) source of water loss. Stool normally represents a minor source of water loss.
of total maintenance water (40% in infants and closer to 25% in adolescents and adults). Insensible losses are composed of evaporative losses from the skin and lungs that cannot be quantitated. The evaporative losses from the skin do not include sweat, which would be considered an additional (sensible) source of water loss. Stool normally represents a minor source of water loss. is usually appropriate initially, although its composition may have to be adjusted if urine output increases significantly.
is usually appropriate initially, although its composition may have to be adjusted if urine output increases significantly.


