CHAPTER 12 MACS facelift
Introduction/key points
• Modern facelifting techniques involve facial sculpturing combined with tension-free skin redraping. Sculpturing is achieved by suturing, judicious liposculpture, volume addition with microfat grafts, or a combination of these techniques.
• Our favored technique for minimally invasive facial rejuvenation is the MACS-lift (minimal access cranial suspension lift).
• A short-scar facelift is not the same as a traditional facelift with a short scar.
• A vertical vector in the face and neck is the rejuvenating one.
• Vertical facelifting techniques involve a temporal hairline incision to prevent sideburn elevation.
• Poor skin quality may require lengthening of the incision in the postauricular region to facilitate correct skin redraping.
Indications
Two variations of the procedure are described:
1. The simple MACS-lift (S-MACS), where two purse string sutures are placed to correct the lower third of the face and neck (the jowls, marionette grooves and the cervicomental angle).
2. The extended MACS-lift (X-MACS), where a supplementary third purse string suture is used to suspend the malar fat pad. This suture has an additional effect on the lower eyelid, the midface and the nasolabial groove.
Simple MACS-lift
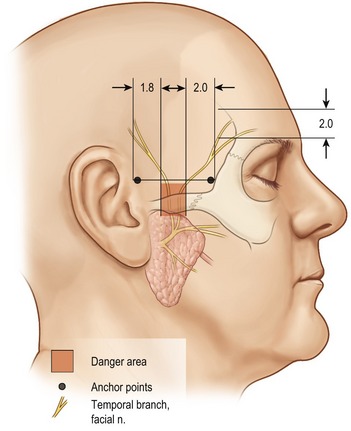
Two purse string sutures are used to correct the jowls, the marionette grooves and the neck. They are anchored to the deep temporal fascia above the zygomatic arch, 1 cm in front of the auricular helix. The first suture runs as a narrow vertical U-shaped purse string towards the mandibular angle, incorporating the posterior border of the platysma muscle. Following liposuction of the neck, tying this suture under maximum tension produces a strong vertical lift on the lateral part of the platysma, correcting the cervicomental angle. The second purse string suture starts from the same anchoring point above the zygomatic arch and runs obliquely in the direction of the jowls as a wider O-shaped loop. Tying this suture corrects the jowls, the marionette grooves and downward slanting corners of the mouth (Fig. 12.1).
Extended MACS-lift
An additional point 2 cm below the lateral canthus is marked preoperatively with the patient sitting. This is the inferior limit of the third purse string suture and is included in the skin undermining. This suture also originates from the deep temporal fascia, but at its anterior aspect, lateral to the orbital rim. It provides strong correction of the nasolabial fold, enhancement of the malar region, lifting of the midface and shortening of the vertical height of the lower eyelid (Fig. 12.1).
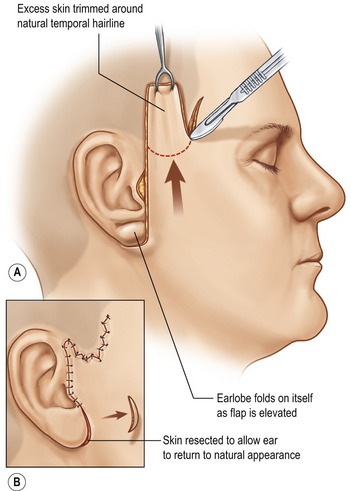
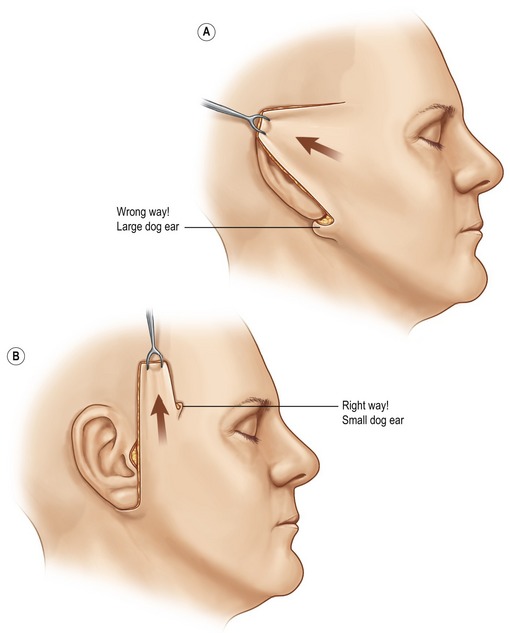
In both the S-MACS and X-MACS the skin is redraped in a completely vertical direction and skin excess above the temporal hairline incision is resected. As there is no lateral traction on the skin, there is no dog ear at the level of the earlobe, eliminating the need for a post-auricular extension of the incision (Fig. 12.2).
In classical teaching, smoking is considered an absolute contraindication to facelift surgery. As a result of the limited subcutaneous undermining and the absence of multiplanar dissection, we only consider smoking a relative contraindication to performing a MACS-lift.
Technical steps
Infiltration
Infiltration follows the sequence of procedures: first the upper eyelids, followed by the submental area, and finally the cheeks. (For the anesthetic solution see Table 12.1.)
| 100 mL NaCl 0.9% |
| 20 mL lidocaine 2% |
| 10 mL ropivacaine 10 mg/mL |
| 2 mL sodium bicarbonate 8.4% |
| 0.2 mL levorenin 1 mg/mL |
| 10 mg triamcinolone |
Preoperative marking: incision
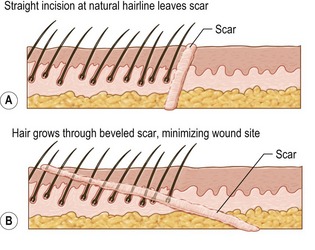
It continues forwards in a zigzag pattern, 2 mm within the lower and anterior aspect of the sideburn. In this part of the incision the knife is beveled at an angle almost tangential with the skin, cutting hair shafts perpendicularly (Fig. 12.3). This maneuver allows hairs to grow through the scar. After hair regrowth the scar will be hidden within the hairline and becomes virtually invisible. The purpose of the zigzag is to increase the length of the temporal incision making it a similar length to the cheek flap, reducing potential dog ear formation.
Suction lipectomy
In cases where microfat grafting is planned, the submental fat can be harvested with a special grating cannula (Fig. 12.4: “ToVer cannula,” Wells-Johnson, Tucson, AZ) which delivers fine-particle fat (1 mm diameter). If insufficient donor fat is present in the submental area, further fat can be harvested from the abdomen or love handles, using other cannulas (Fig. 12.5: “Becker Grater Round” cannula with 1 mm holes, Wells-Johnson, Tucson AZ).
Microfat grafting
Fat is prepared and injected as soon as possible after harvesting. We sieve it through a fine-meshed sterile cloth, rinsing away blood and oil with normal saline. The fat is injected with 18 G fat grafting cannulas (Fig. 12.6: Wells-Johnson, Tulip).
The skin puncture is made with a 16 G pink needle, and does not require closure after the procedure.
Anchor point
The sagging facial soft tissues are suspended by purse string sutures that are woven into the SMAS, which is not undermined. The anchor point for these sutures is the deep temporal fascia above the zygomatic arch, at a safe distance from the frontal branch of the facial nerve (Fig. 12.7).
The first purse-string suture: the vertical loop
See Fig. 12.1, dotted black line.
Suturing goes down to the lower limit of the skin undermining. At this point, two or three solid bites in the superior edge of the platysma muscle are taken (Fig. 12.8A). Then, suturing changes direction, turning upwards, back towards the starting point. This creates a narrow U-shaped purse string loop with a width of approximately 1 cm. The knot is then tied under maximum tension.
Skin redraping and resection
Classically in facelift surgery there is always a horizontal component to the skin redraping. This causes skin redundancy around the earlobe, requiring a post auricular extension of the incision (Fig. 12.9, Fig. 12.10B).
Skin resection on the cheek flap is carried out in a curvilinear fashion. The zigzag border of the temporal hairline incision expands to incorporate this linear cheek flap, compensating for any incongruity and reducing possible dog ear formation. The earlobe is then set back into the cheek flap (Fig. 12.2).
Closure is with buried interrupted 4-0 Vicryl® sutures.
The remainder of the wound is closed with interrupted 6-0 nylon sutures.
The short-scar temporal lift
Technique
The subcutaneous undermining is performed through the MACS-lift incision. Then a 4 cm horizontal cut is made in the hair-bearing skin above the lateral third of the eyebrow. Subgaleal undermining proceeds until the “transition line” is reached. Here the tips of the dissecting scissors are turned upwards, and the galea is transected with guidance from the nondominant middle finger. Any bleeding points are identified and cauterized. The cranial edge of the transected galea is suspended to the galea at the scalp incision with 2–3 U-shaped 2-0 Vicryl sutures. A few millimeters of skin are resected to minimize wrinkling distal to the incision, but it is not necessary to completely flatten this area, as any residual folds will disappear spontaneously with resorption of the Vicryl suture. Skin closure is performed with a running 3-0 nylon suture, which is removed together with the facelift sutures six days postoperatively.
The pinch lower lid blepharoplasty
After performing an extended MACS-lift, the malar mound is moved vertically creating skin excess in the lower eyelid. This excess is estimated by pinching with forceps and is marked with methylene blue. A pinch blepharoplasty is performed via a classical lower eyelid blepharoplasty incision. The skin is released from the orbicularis, redraped and the excess resected. Closure is with a running 5-0 nylon intradermal suture.
Results
Case 1 (side and frontal view)
• Botulinum toxin to the corrugator and depressor supercilii muscles.
• Submental liposuction with removal of fat between the skin and platysma muscle and some fat removal from the jowls.
• Transconjunctival lower eyelid fat removal.
• An upper eyelid blepharoplasty with resection of skin, orbicularis oculi muscle and conservative removal of fat from the medial compartment.
Case 2 (frontal and  view)
view)
This 56-year-old woman requested rejuvenation of the lower and middle third of the face. She presents with platysmal bands, a lax submental and upper neck region, jowls, marionette grooves, downward slanting corners of the mouth, upper lip rhytids, marked nasolabial folds and emptiness of the midface with hollow lower eyelids. She also has empty upper eyelids but her eyebrow position is satisfactory. Note the inframalar depression in the  view.
view.
Case 3 (side and frontal view)
An additional postauricular incision was necessary to remove skin folds.
Case 4 (frontal and  view)
view)
Case 5 (frontal and  view)
view)
This 53-year-old woman is seeking minimally invasive facial rejuvenation. She wears her hair short and does not want any scars behind her ears. Clinical examination reveals laxity in the neck with platysmal bands, jowls, marionette grooves, fine perioral rhytids on thin lips, a marked nasolabial fold and an empty deflated midface with obvious demarcation between the lid–cheek junction. She also requested correction of her nasal hump and hanging columella.
• Lower eyelid pinch blepharoplasty.
• Microfat grafting of the nasojugal groove (1 mL/side), the zygomatic area (9 mL/side), upper lip (5 mL in the vermilion and whole upper lip), lower lip (3 mL), nasolabial groove and corner of the mouth (1.5 mL/side).
• Erbium laser resurfacing of the upper lip.
• Open rhinoplasty with hump reduction, tip refinement and correction of the columellar-alar relationship.
Summary/conclusions
Pearls & pitfalls
• The greatest limitation in using a short scar facelift is the fear of insufficient skin contouring in the neck. In over 95% of patients this is not the case, provided that the facelift vector is vertical as described.
• The minority of patients who present with poor neck skin will show marked vertical pleats below the lobule after skin redraping. This can easily be corrected using a posterior cervicoplasty.
• This consists of a zigzag occipital hairline skin incision through which subcutaneous undermining is performed beyond the vertical skin pleats.
• The skin is then redraped; any excess is determined with the d’Asumpcao forceps and excised.
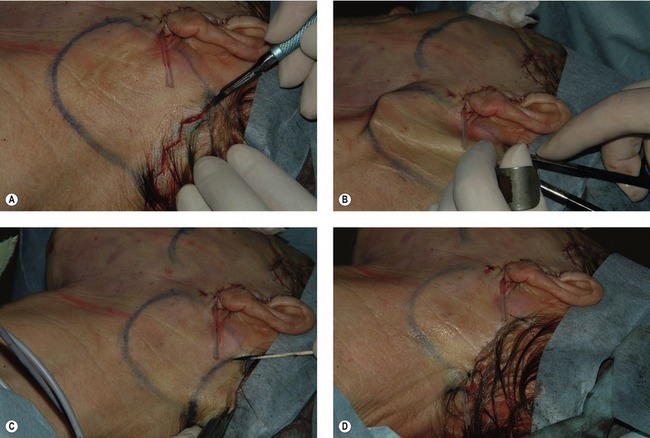
• Closure is performed with 4-O Vicryl and 5-0 nylon sutures (Fig. 12.11A–D).
• Rarely, a patient with a thick heavy neck is encountered (Fig. 12.12, pre- and postoperatively). One should not hesitate to add a short submental incision, with an open lipectomy in the preplatysmal and occasionally subplatysmal planes. The neck skin is then widely undermined from ear lobule to ear lobule.
• After completion of an MACS-lift the skin is vertically redraped. No postauricular skin resection is necessary.
Summary of steps
3. Microfat grafting, if indicated.
5. Placement of the 2 or 3 0-PDS purse string sutures anchored to the deep temporal fascia above the zygomatic arch.
6. Short scar temporal lifting if indicated.
7. Skin redrapement and resection.
9. Pinch lower lid blepharoplasty.
10. Ancillary procedures (upper lid blepharoplasty, skin resurfacing, lip lift, etc).
Aston SJ, Bernard RW, Casson PR, Klatsky SA. Secondary face lift. Panel Discussion. Aesthet Surg J. 2002;22:277–283.
Baker D, Massiha H, Nahai F, Tonnard PL. Short scar face lift. Panel Discussion. Aesthet Surg J. 2005;25:607–617.
Baker DC, Hamra ST, Owsley JQ, Ramirez OM. Ten year follow-up on the twin study. Panel presented at Annual Meeting of the American Society for Aesthetic Plastic Surgery; April 2005, New Orleans, Louisiana.
Besins T. The “RARE” technique (reverse and repositioning effect): The renaissance of the aging face and neck. Aesthet Plast Surg. 2004;28(3):127–142.
Camirand A, Doucet J. A comparison between parallel hairline incisions and perpendicular incisions when performing a face lift. Plast Reconstr Surg. 1997;99:10–15.
Coleman SR. Structural fat grafting: more than permanent filler. Plast Reconstr Surg. 2006;118:108S–120S.
Coleman SR. Structural fat grafting. St Louis: Quality Medical Publishing; 2004. 29–57
Connell BF, Semlacher RA. Contemporary deep layer facial rejuvenation. Plast Reconstr Surg. 1997;100:1513–1523.
Feldman JJ. Neck lift. St Louis: Quality Medical Publishing; 2006.
Fogli A. Temporal lift by galeopexy. A review of 270 cases. Aesthet Plast Surg. 2003;27(3):159–165.
Gonzàlez-Ulloa M, Flores ES. Senility of the face: Basic study to understand its causes and effects. Plast Reconstr Surg. 1965;36:239–246.
Isse NG. Endoscopic forehead lift: Evolution and update. Clin Plast Surg. 1995;22:661.
Labbé D, Franco RG, Nicolas J. Platysma suspension and platysmaplasty during neck lift: Anatomical study and analysis of thirty cases. Plast Reconstr Surg. 2006;117:2001–2009.
Matarasso A, Hutchinson O. Evaluating rejuvenation of the forehead and brow: An algorithm for selecting the appropriate technique (follow up). Plast Reconstr Surg. 2003;112:1467.
Paul MD, Calvert JW, Evans G. The evolution of the midface lift in aesthetic plastic surgery. Plast Reconstr Surg. 2006;117:1809–1827.
Pessa JE. An algorithm of facial aging: Verification of Lambros’ theory by three-dimensional stereolithography, with reference to the pathogenesis of midfacial aging, scleral show, and the lateral suborbital trough deformity. Plast Reconstr Surg. 2000;106(2):479–488.
Singer D, Sullivan P. Submandibular gland I: An anatomic evaluation and surgical approach to submandibular gland resection for facial rejuvenation. Plast Reconstr Surg. 2003;112:1150–1154.
Tonnard PL, Verpaele A, et al. 300 MACS-lift short scar rhytidectomies: Analysis of results and complications. Eur J Plast Surg. 2005;28:198–205.
Tonnard PL, Verpaele A. Optimizing results from minimal access cranial suspension lifting (MACS-lift). Aesthet Plast Surg. 2005;29:213–220.
Tonnard PL, Verpaele A. The MACS-lift short scar rhytidectomy. St Louis: Quality Medical Publishing; 2004.
Verpaele A, Tonnard PL, Pirayesh A, Guerao FP, Gaia S. The third suture in MACS-lifting: Making midface lifting simple and safe. JPRAS. 2007;60:1287–1295.

 hours, under local anesthesia as an outpatient. In comparison to a traditional facelift, the MACS-lift involves a shorter scar, lower morbidity and a quicker recovery time.
hours, under local anesthesia as an outpatient. In comparison to a traditional facelift, the MACS-lift involves a shorter scar, lower morbidity and a quicker recovery time.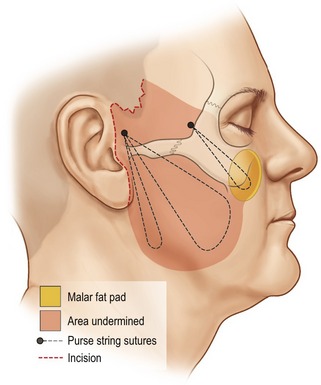



 and platysma in the lower
and platysma in the lower  , are taken. It is important to confirm that every bite of the needle takes a substantial piece of SMAS, to prevent the suture from pulling through.
, are taken. It is important to confirm that every bite of the needle takes a substantial piece of SMAS, to prevent the suture from pulling through.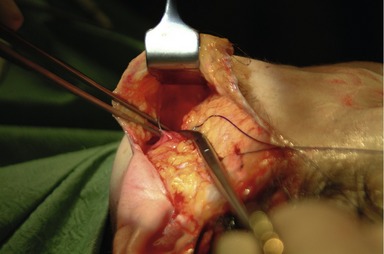

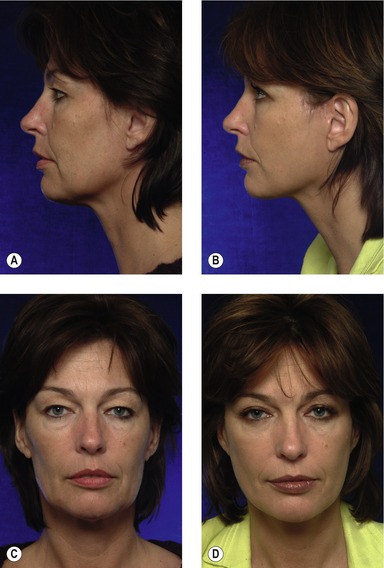

 view. There is also blending of the lid–cheek junction and a reduction of the vertical height of the lower eyelid.
view. There is also blending of the lid–cheek junction and a reduction of the vertical height of the lower eyelid.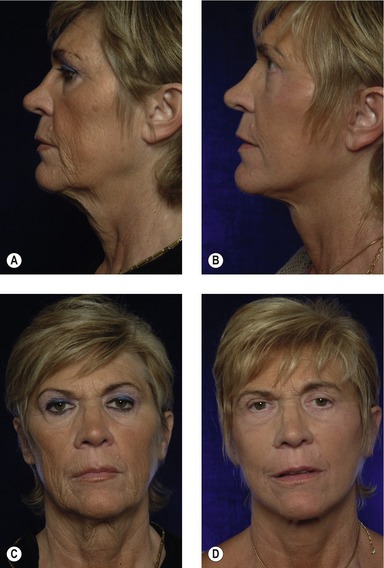

 view. In this, the effect of the temporal lift can also be seen. The tail of the eyebrow has been raised about 1 cm but the beard and sideburn remain in an anatomical position. Note the quality of the 4 cm horizontal scar from the temporal lift.
view. In this, the effect of the temporal lift can also be seen. The tail of the eyebrow has been raised about 1 cm but the beard and sideburn remain in an anatomical position. Note the quality of the 4 cm horizontal scar from the temporal lift.
 years after surgery. There is correction of the cervicomental angle, the jowls, marionette grooves and nasolabial folds, with an obvious improvement in the midface. This is most obvious in the
years after surgery. There is correction of the cervicomental angle, the jowls, marionette grooves and nasolabial folds, with an obvious improvement in the midface. This is most obvious in the  view where the flat zygomatic area has been transformed into a youthful malar prominence. There is blending of the lid–cheek junction. The upper and lower lips have been naturally augmented and the fine rhytids have been eradicated by the laser treatment. The rhinoplasty has had a complementary effect on the rejuvenating surgery. Microfat grafting has produced the additional augmentation necessary in this thin deflated patient. This cannot be achieved by classical facelift procedures alone.
view where the flat zygomatic area has been transformed into a youthful malar prominence. There is blending of the lid–cheek junction. The upper and lower lips have been naturally augmented and the fine rhytids have been eradicated by the laser treatment. The rhinoplasty has had a complementary effect on the rejuvenating surgery. Microfat grafting has produced the additional augmentation necessary in this thin deflated patient. This cannot be achieved by classical facelift procedures alone.