46 Lumbar Sympathetic Block
Placement
Anatomy
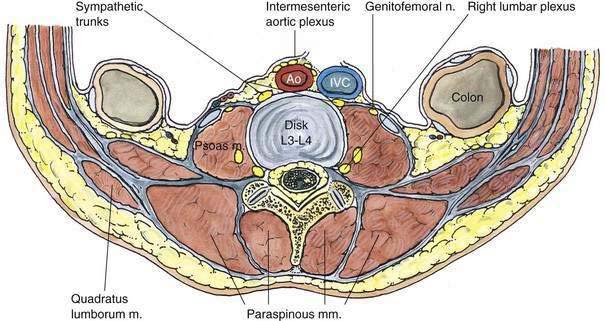
The lumbar sympathetic chain, with its accompanying ganglia, is located in the fascial plane immediately anterolateral to the lumbar vertebral bodies (Fig. 46-1). The sympathetic chain is separated from the somatic nerves by the psoas muscle and fascia. The lumbar regions L1, L2, and sometimes L3 provide white rami communicantes to the sympathetic chain, and all five lumbar vertebrae are associated with gray rami communicantes. These rami are longer in the lumbar region than in the thoracic region. This is anatomically important because it allows needle placement nearer the anterolateral border of the vertebral body in the lumbar region. Conceptually, the anatomy important to anesthesiologists performing lumbar sympathetic nerve block is also the anatomy important for celiac plexus nerve block.
Position
My experience suggests that lumbar sympathetic nerve block is most effectively carried out in a manner similar to that used for celiac plexus block (see Chapter 47, Celiac Plexus Block). The patient should be prone with a pillow under the mid-abdomen to help reduce lumbar lordosis. (Despite this recommendation, many clinicians continue to use the lateral position successfully.)
Needle Puncture
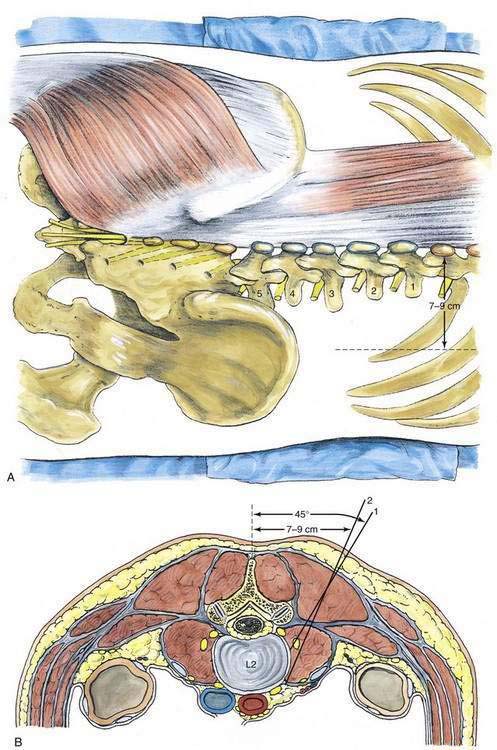
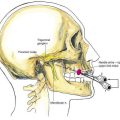
Most experienced anesthesiologists now carry out this block through a single needle. This is possible because placing the needle tip at the anterolateral border of the second or third lumbar vertebral body allows the local anesthetic solution to spread along the fascial plane enveloping the sympathetic chain. As an example, the second lumbar vertebral spine is identified, and a mark is made lateral to it in the horizontal plane, 7 to 9 cm from the midline, as illustrated in Figure 46-2. A skin wheal is raised, and a 15-cm, 20- or 22-gauge needle is directed in the horizontal plane at an angle of 30 to 45 degrees from a vertical plane through the patient’s midline. It is inserted until it contacts the lateral aspect of the L2 vertebral body. If it comes into contact with the vertebral transverse process at a more superficial level (at only 3 to 5 cm), the needle can simply be redirected cephalad or caudad to avoid the transverse process. The vertebral body is usually located at a depth of 7 to 12 cm.
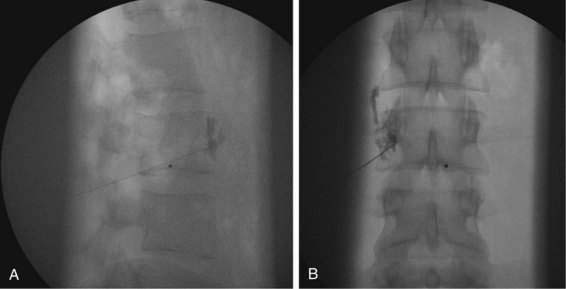
Once the needle’s position on the lateral aspect of the vertebral body is certain, the needle is withdrawn and redirected at a steeper angle until it slides off the anterolateral surface of L2. This needle insertion and redirection process is almost identical to that described for the celiac plexus block. For the lumbar sympathetic block, once the needle is in position, approximately 15 to 20 mL of local anesthetic solution is injected. With proper needle tip position, this volume will allow spread along the axis of the sympathetic chain (Fig. 46-3).
Potential Problems
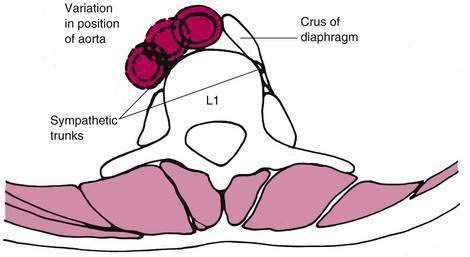
As illustrated in Figure 46-4, a potential problem with the lumbar sympathetic block is puncture of the aorta. Most often this results in no sequelae. Nevertheless, anesthesiologists should be aware that the position of the aorta relative to the vertebral body ranges from an anterolateral position to a midline position. Because the needle is directed toward the neuraxial structures, both epidural and spinal block can result from an errantly placed needle. Thus, development of a postural headache after a lumbar sympathetic block should lead the anesthesiologist to think of unrecognized dural puncture. Also, when using neurolytic agents, one should be aware that spillover onto lumbar roots is a possibility, although it happens rarely.