Lumbar instability
Definitions
At the most simple level, instability is a lack of stability, a condition in which application of a small load causes an inordinately large, perhaps catastrophic displacement.1 This is also the description given by the American Academy of Orthopaedic Surgeons, who state: ‘Segmental instability is an abnormal response to applied loads, characterized by motion in motion segments beyond normal constraints.’2
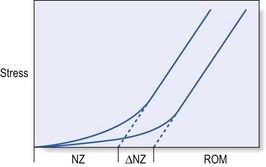
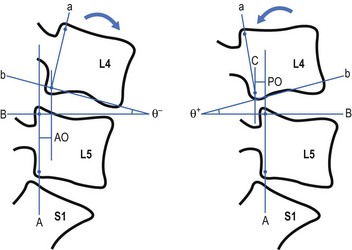
A biomechanically more accurate definition of segmental instability, using a ‘neutral zone’ concept, has been proposed by Panjabi. The neutral zone concept is based on the observation that the total range of motion (ROM) of a spinal motion segment may be divided into two zones: a neutral zone and an elastic zone (Fig. 37.1).3 The neutral zone is the initial portion of the ROM during which spinal motion is produced against minimal internal resistance. The elastic portion of the ROM is the portion nearer to the end-range of movement that is produced against substantial internal resistance. Segmental instability is thus defined as a decrease in the capacity of the stabilizing system of the spine to maintain the spinal neutral zones within physiological limits in order to prevent neurological deficit, major deformity and/or incapacitating pain.4 This definition describes joints that, early in range and under minor loads, may exhibit excessive displacement.
The clinical definition of instability is: ‘a condition in which the clinical status of a patient with low back problems evolves, with the least provocation, from the mildly symptomatic to the severe episode’.5 Others consider instability to exist only when sudden aberrant motions such as a visible slip or catch are observed during active movements of the lumbar spine or when a change in the relative position of adjacent vertebrae is detected by palpation performed with the patient in a standing position versus palpation performed with the patient in a prone position.6
Anatomy
Inert structures
The passive subsystem consists primarily of the vertebral bodies, discs, zygapophyseal joints and joint capsules, and spinal ligaments. The passive subsystem plays its most important stabilizing role in the elastic zone of spinal ROM (i.e. near end-range),7 and numerous studies have been conducted that demonstrate the relative contributions of passive structures to segmental stability.
The posterior ligaments of the spine (interspinous and supraspinous ligaments), along with the zygapophyseal joints and joint capsules and the intervertebral discs, are the most important stabilizing structures when the spine moves into flexion.8–11 End-range extension is stabilized primarily by the anterior longitudinal ligament, the anterior aspect of the annulus fibrosus and the zygapophyseal joints.12,13 Rotational movements of the lumbar spine are stabilized mostly by the intervertebral discs, the zygapophyseal joints and, for the L4–L5 and L5–S1 segments, the iliolumbar ligaments too.14
Injury to the inert stabilizing system may have important implications for spinal stability. Intervertebral disc degeneration, weakening of the posterior longitudinal ligaments and early degeneration of the facet joints may increase the size of the neutral zone, increasing demands on the contractile subsystem to avoid the development of segmental instability.3
Contractile structures
During recent decades, a variety of studies have documented the stabilizing effect of muscles on the lumbar spine.15–18 The lumbar erector spinae muscle group provides most of the extensor force required for many lifting tasks.19 Rotation is produced primarily by the oblique abdominal muscles. The multifidus muscle seems to be able to exert some segmental control and is therefore proposed to function as a stabilizer during lifting and rotational movements of the lumbar spine.20 The role of the oblique abdominal and transversus abdominis muscles in spinal stability has been the subject of much debate. The abdominals have been thought to play a stabilizing role, either by increasing intra-abdominal pressure or by creating tension in the lumbodorsal fascia.21
Neuromuscular control
The neural control system may also play an important part in stabilization of the spine. Panjabi describes the stability system as being composed of an inert spinal column, the spinal muscles and a control unit.22 In this model, changes in spinal balance resulting from position and load are monitored by transducers embedded in the ligaments that relay information to the control unit. When conditions that challenge spine stability are detected, the control unit activates the appropriate muscles to protect or restore stability, or to avoid instability. Evidence for this hypothesis is found in studies showing that patients with low back pain (LBP) often have persistent deficits in neuromuscular control.23,24 This hypothesis was further supported by a recent electromyographic study demonstrating that a primary reflex arc exists from mechanoreceptors in the supraspinous ligament to the multifidus muscles. Such a reflex arc could be triggered by application of loads to the isolated supraspinous ligament, which in turn initiates activity of the multifidus muscles at the level of ligament deformation, as well as one level above or below.25
Classification of lumbar instability
The major categories of segmental instability are shown in Box 37.1.26 Tumours, infections and trauma are beyond controversy. They produce mechanical weakening of the anterior columns and can be diagnosed by medical imaging and by biopsy. Spondylolisthesis is a more controversial category. The condition is rarely progressive in teenagers or adults and can therefore be considered as stable in these age groups.27 However, it has been suggested that concurrent severe disc degeneration at the level of listhesis may lead to progression of slip and convert an asymptomatic and stable lesion into a symptomatic one.28
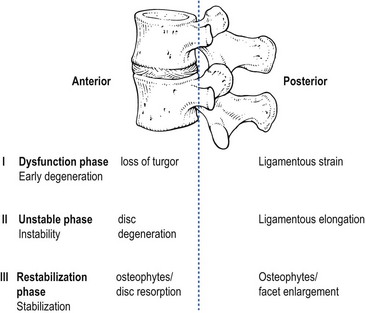
More difficulties arise with respect to so-called ‘degenerative instability’. The ageing of the lumbar spine has been discussed thoroughly (see Ch. 32). Grossly, it occurs in three sequential phases: dysfunction, instability and restabilization.29
During the early phase of degeneration (dysfunction), small annular tears and early nuclear degeneration appear in the disc, and ligamentous strains develop in the posterior ligaments and in the capsules of the zygapophyseal joints. The unstable phase includes reduction of disc height, gross morphological changes in the disc, and laxity of the spinal ligaments and facet joints. These changes lead to an increased and abnormal range of movement and to increased liability to disc displacements. During the restabilization phase, further physiological changes in the disc, such as increased collagen and decreased water content, together with the development of spinal osteophytes and gross osteoarthrosis of the zygapophyseal joints, result in increased stiffness of the spine and consequent stabilization (Fig. 37.2).
Biomechanical studies, both in vivo and in vitro, have confirmed this hypothesis: loss of stiffness, accompanied by annular tears or even nuclear disruption, has been reproduced in the laboratory by repetitive loading cycles which simulate normal human exposures.30 In other experiments, load applications to degenerative segments have revealed loss of stiffness, sometimes with quite dramatic results.31 However, difficulty remains in translating these anatomical and functional changes into clinical descriptions that could serve as a basis for diagnosis and treatment.
A further classification system for degenerative lumbar instability (Box 37.2), based on a combination of history and radiographic findings, has been proposed.32
• A primary instability is one where there has been no prior intervention or treatment which might account for the development of the process.
• A secondary instability involves surgical destruction of one or more of the restraining elements of the spine. Secondary instabilities may develop after discectomies,33 decompressive laminectomies, spinal fusions and chemonucleolysis.34
Rotational instability is still a hypothetical entity and so far normal radiological limits have not been identified.35
Translational instability is the most classic and best known of the primary degenerative instabilities. It is characterized by excessive anterior translation of a vertebra during flexion of the lumbar spine. At an early stage, it presents with disc space narrowing and traction spurs; later on, it represents degenerative spondylolisthesis. However, anterior translation is a normal component of flexion, and once again the difficulty that arises is setting a limit of normal translation. Many asymptomatic individuals exhibit anterior slips of more than 3 mm36; 4 mm of translation occurs in 20% of asymptomatic patients.37
Retrolisthesis develops when degeneration of the disc and the consequent decrease in disc height force the zygapophyseal joints into extension (see p. 442). Again, it has been shown that similar appearances occur in asymptomatic individuals.38 Therefore, the simple detection of retrolisthesis on a radiograph is not an operational criterion for instability.
Instability and the clinical concept of mechanical lesions of the lumbar spine
Spinal instability is not a painful condition but may predispose to secondary lesions:
Segmental instability and discodural interactions
The typical history is usually that of recurrent back pain, which begins either suddenly or gradually, depending on the consistency of the shifted fragment (‘nuclear’ or ‘annular’) (see Ch. 33, Dural concept). There are bouts of backache a few times a year, and between the attacks the patient is fit and the back is painless. However, the slightest sudden movement or unaccustomed posture leads to a new discal shift, resulting in a renewed discodural interaction and pain.
Segmental instability and ligamentous lesions
Postural ligamentous pain appears when normal ligaments are subjected to abnormal mechanical stresses (see Ch. 34, Ligamentous concept). This may occur during the dysfunction stage: some loss of turgor in the disc and the decrease in intervertebral joint space cause some laxity of the segment and an increase of the neutral zone. The facet joints override, with the upper articular processes sliding downwards over the lower. The joints adopt the extension position and the posterior capsules become overstretched. As instability proceeds, more tension is imposed on the ligaments and the facet joint capsules, leading to more postural ligamentous pain.
Segmental instability and the stenotic concept
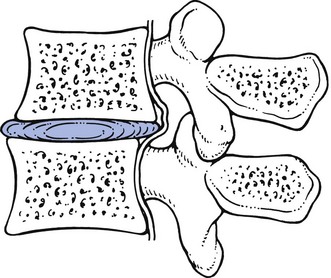
Instability and the subsequent retrolisthesis may narrow the radicular canal and subsequently compress the nerve root (see Ch. 35, Stenotic concept). Usually, the process results from combined anterior pressure exerted by a buckled posterior longitudinal ligament and posterior compression of the superior articular process. The mechanism is as follows: considerable narrowing of the intervertebral disc space causes the posterior longitudinal ligament, which contains some fragments of remaining disc tissue, to bulge dorsally. This is especially the case in the standing or lordotic position. Because of the inclination of the facet joints, narrowing of the disc and increased laxity of the segment also result in retrolisthesis of the upper vertebra, which brings the nerve root in close contact with the tip of the anterior articular process of the vertebra below (Fig. 37.3).
Diagnosis of lumbar instability
Diagnosis is usually based on history, clinical examination, functional tests and imaging. Some elements can be found in the patient’s history. It is believed that frequent recurrences of LBP precipitated by minimal perturbations, lateral shifts in prior episodes of LBP, short-term relief from manipulation and an improvement of symptoms with the use of a brace in previous episodes of LBP are confirmatory data for instability.39
Clinical observations
Some authors state that the palpation of increased mobility with passive intervertebral motion testing is indicative of instability.40 The validity of these techniques, however, has never been demonstrated.41 Others have proposed that aberrant motions such as the instability catch occurring during active ROM testing indicate instability.6,42,43 The instability catch has been described as a sudden acceleration or deceleration of movement, or a movement occurring outside of the primary plane of motion (e.g. side bending or rotation occurring during flexion) and is proposed as an indication of segmental instability. However, this definition of an ‘instability catch’ is far too broad, because in the present description it also includes the common painful arc sign which indicates a momentary discodural interaction during movement (see p. 455).
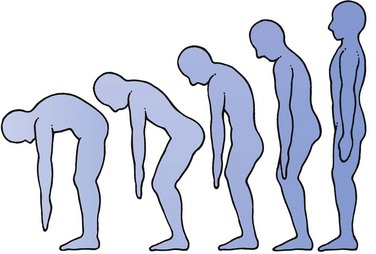
In our opinion, MacNab’s reversal of the normal spinal rhythm is much more characteristic of segmental instability.44 In a normal lumbar–pelvic rhythm, there is a smoothly graded ratio between the degree of pelvic rotation and that of lumbar flattening. This rhythm may be disturbed in regaining the erect posture after forward flexion. In order to avoid putting an extension strain on the lumbar spine, the patient first slightly flexes the hips and knees in order to tuck the pelvis under the spine and then regains the erect position by straightening the legs (Fig. 37.4).
Radiological observations
A second observation is the presence of traction spurs (Fig. 37.5), as described by MacNab.45 The spur is considered to result from tensile stresses being applied to the outer annular fibres which attach to the vertebral body (see p. 444).46
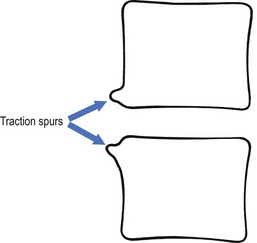
Fig 37.5 Traction spurs.
The third observation is the presence of spinal malalignment. This radiological assessment is based on the early observations of Knutsson, who defined instability as 3 mm or more of anterior translation measured between flexion and extension. However, as discussed earlier, there exists much debate about the upper limit of normal translations. Boden and Wiesel emphasized that any slip should be greater than 4 mm before instability could be considered.36 Others concluded that a minimum of 4 mm of forward displacement was necessary at the L3–L4 and L4–L5 levels to define instability,47 while at the L5–S1 level displacements of greater than 5 mm were necessary for accurate measurements (Fig. 37.6).48,49 Furthermore, it has also been suggested that many instabilities do not occur at the extremes of flexion and extension, which is the usual technique utilized in routine radiographic studies.
Treatment of lumbar instability
Patient education may be an important component in the treatment of patients with segmental instability. Education should, first of all, focus on avoiding loaded flexion movements, as they may create a posterior shift of the disc.51 Patients should also be made aware of the importance of avoiding end-range positions of the lumbar spine because these overload the posterior passive stabilizing structures (see p. 583).
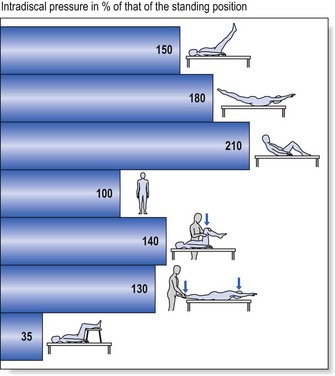
As the lumbar erector spinae muscles are the primary source of extension torque for lifting tasks, strengthening of this muscle group has been advocated.52 Intensive dynamic exercises for the extensors proved to be significantly superior to a regime of standard treatment of thermotherapy, massage and mild exercises in patients with recurrent LBP.53–55 The abdominal muscles, particularly the transversus abdominis and oblique abdominals, have also been proposed as having an important role in stabilizing the spine by co-contracting in anticipation of an applied load. However, exercises proposed to address the abdominal muscles in an isolated manner usually involve some type of sit-up manœuvre that imposes dangerously high compressive and shear forces on the lumbar spine56 and may provoke a posterior shift of the (unstable) disc (Fig. 37.7). Alternative techniques should therefore be applied when training these muscles.
Some authors strongly suggest that the transversus abdominis57 and the multifidus muscles make a specific contribution to the stability of the lower spine,58,59 and an exercise programme that proposes the retraining of the co-contraction pattern of the transversus abdominis and multifidus muscles has been described.60 The exercise programme is based on training the patient to draw in the abdominal wall while isometrically contracting the multifidus muscle, and consists of three different levels:
• First, specific localized stabilization training is given. Lying prone, sitting and standing upright, the patient performs the isometric abdominal drawing-in manœuvre with co-contraction of the lumbar multifidus muscles.
• During the phase of general trunk stabilization, the co-contraction of the same muscles is carried out on all fours, and then elevating one arm forwards and/or the contralateral leg backwards, or on standing upright and elevating one arm forwards and/or bringing the contralateral leg backwards.
• Third, there is the stabilization training. Once accurate activation of the co-contraction pattern is achieved, training is given in functional movements, such as standing up from a sitting or lying position, bending forwards and backwards and turning. All daily activities are then integrated.
A significant result from a randomized trial has recently been reported comparing this exercise programme with one of general exercise (swimming, walking, gymnastic exercises) in a group of patients with chronic LBP.61
Despite the positive results with muscular training programmes, it remains difficult to understand how training of the lumbar and abdominal muscles can improve segmental stability. Not only do the muscles (except for multifidus) have multisegmental attachments to the lumbar vertebrae, but also they are not very well oriented to resist displacements. Because they mainly run longitudinally, they can only resist sagittal rotation and are not able to resist anterior or posterior shears. However, whenever the muscles contract, and especially when they do this simultaneously, they exert a compressive load on the whole lumbar spine, as well as on the unstable segment. By compressing the joints, the muscles make it harder for the joints and for the intradiscal content to move.62 The most important contribution of trained muscles to spinal stability may therefore be the creation of a rigid cylinder around the spine and increased stiffness.
Sclerosant treatment
The infiltration produces a local inflammatory reaction, which is followed by increased proliferation of fibroblasts and the production of new collagen fibres. The final outcome is tightening, reinforcement and loss of normal elasticity of the connective tissue which decreases the mobility and increases the stability of the injected segments.63–65
The beneficial effect of this treatment method was recently shown in a double-blind controlled study that demonstrated a statistically significant difference between the active therapy group and those who received injections with a saline solution only.66
Technique
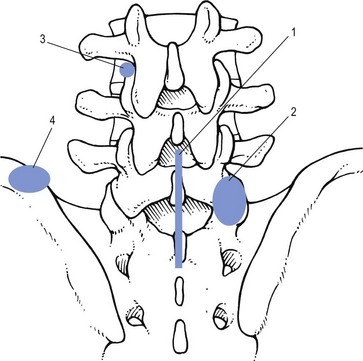
• The first injection is at the interspinous and supraspinous ligaments.
• The second injection is given at the posterior capsules of the zygapophyseal joints.
• The third injection is given at the lateral aspects of the laminae, where the ligamentum flavum and the medial aspects of the deeper layer of the fascia lumborum merge.
• The fourth injection aims at the insertion of the iliolumbar ligaments and the insertion of the thoracolumbar fascia on the posterior superior iliac spine (Fig. 37.8).
Surgery
The indications for spinal fusion in the treatment of degenerative instability are controversial. The basic problem lies, as discussed earlier, in the definition and the diagnosis of the disorder. However, despite the fact that indications for the procedure are uncertain, that costs and complication rates are higher than for other surgical procedures performed on the spine, and that long-term outcomes are uncertain, the rate of lumbar spinal fusion is increasing rapidly in the United States.67,68 The rate of back surgery and especially of spinal fusion operations is at least 40% higher in the US than in any other country and is five times higher than in the UK.69 Although there have been no randomized trials evaluating the effectiveness of lumbar fusion for spinal instability, the feeling remains that the operation should be reserved for patients with severe symptoms and radiographic evidence of excessive motion (greater than 5 mm translation or 10° of rotation) who fail to respond to a trial of non-surgical treatment.70 The latter should consist of a combination of patient education, physical training and sclerosing injections.
References
1. Pope, MH, Panjabi, M, Biomechanical definitions of spinal instability. Spine 1985; 10:255–256. ![]()
2. American Academy of Orthopaedic Surgeons. A glossary on spinal terminology. Chicago: American Academy of Orthopaedic Surgeons; 1985.
3. Panjabi, MM, The stabilizing system of the spine, part II: neutral zone and instability hypothesis. J Spinal Disord 1992; 5:390–396. ![]()
4. Panjabi, MM, Oxland, TR, Yamamoto, I, Crisco, JJ, Mechanical behavior of the human lumbar and lumbosacral spine as shown by three-dimensional load-displacement curves. J Bone Joint Surg 1994; 76A:413–424. ![]()
5. Kirkaldy-Willis, W, Farfan, H, Instability of the lumbar spine. Clin Orthop 1982; 165:110–123. ![]()
6. Paris, SV, Physical signs of instability. Spine 1985; 10:277–279. ![]()
7. Panjabi, MM, Goel, VK, Takata, K, Physiologic strains in the lumbar spinal ligaments: an in vitro biomechanical study. Spine 1982; 7:192–203. ![]()
8. Adams, MA, Hutton, MC, Stott, JRR, The resistance to flexion of the lumbar intervertebral joint. Spine 1980; 5:245–253. ![]()
9. McGill, SM, Estimation of force and extensor moment contributions of the disc and ligaments at L4–L5. Spine 1988; 13:1395–1402. ![]()
10. Solomonow, M, Zhou, B, Harris, M, et al, The ligamento-muscular stabilizing system of the spine. Spine 1998; 23:2552–2562. ![]()
11. Kong, WZ, Goel, VK, Gilbertson, LG, Weinstein, JN, Effects of muscle dysfunction on lumbar spine mechanics. A finite element study based on a two motion segments model. Spine 1996; 21:2197–2206. ![]()
12. Haher, TR, O’Brien, M, Dryer, JW, et al, The role of the lumbar facet joints in spinal stability: identification of alternative paths of loading. Spine 1994; 19:2667–2670. ![]()
13. Sharma, M, Langrana, NA, Rodriguez, J, Role of ligaments and facets in lumbar spinal stability. Spine 1995; 20:887–900. ![]()
14. Basadonna, P-T, Gasparini, D, Rucco, V, Iliolumbar ligament insertions; in vivo anatomic study. Spine 1996; 21:2313–2323. ![]()
15. Bogduk, N, Macintosh, JE, Pearcy, MJ, A universal model of the lumbar back muscles in the upright position. Spine 1992; 17:897–913. ![]()
16. Hodges, PW, Richardson, A, Inefficient muscular stabilization of the lumbar spine associated with low back pain. Spine 1996; 21:2640–2650. ![]()
17. Gudavalli, MR, Tirano, JJ, An analytical model of lumbar motion segment in flexion. J Manip Physiol Ther 1999; 22:201–208. ![]()
18. Gardner-Morse, M, Stokes, IA, Laible, JP, Role of muscles in lumbar spine stability in maximum extension efforts. J Orthop Res 1995; 13:802–808. ![]()
19. Macintosh, JE, Pearcy, MJ, Bogduk, N, The axial torque of the lumbar back muscles: torsion strength of the back muscles. Aust N Z J Surg 1993; 63:205–212. ![]()
20. Macintosh, JE, Bogduk, N. The biomechanics of the lumbar multifidus. Clin Biomech. 1986; 1:205–213.
21. Vleeming, A, Pool-Goudzwaard, AL, Stoeckaert, R, et al, The posterior layer of the thoracolumbar fascia: its function in load transfer from spine to legs. Spine 1995; 20:753–758. ![]()
22. Panjabi, M, The stabilizing system of the spine I. Function, dysfunction, adaptation and enhancement. J Spinal Disord 1992; 5:383–389. ![]()
23. Hodges, PW, Richardson, A, Evaluation of the relationship between the findings of a laboratory and a clinical test of transversus abdominis function. Physiother Res Internat 1996; 1:30–40. ![]()
24. Luoto, S, Taimela, S, Hurri, H, et al, Psychomotor speed and postural control in chronic low back pain patients: a controlled follow-up study. Spine 1996; 21:2621–2627. ![]()
25. Solomonow, M, Zhou, B, Harris, M, et al, The ligamento-muscular stabilizing system of the spine. Spine 1998; 23:2552–2662. ![]()
26. Frymoyer, JW. Segmental instability. In: Frymoyer JW, ed. The Adult Spine. New York: Raven Press; 1991:1873–1891.
27. Axelsson, P, Johansson, R, Stromqvist, B, Is there increased intervertebral mobility in isthmic adult spondylolisthesis? A matched comparative study using stereophotogrammetry. Spine 2000; 25:1701–1703. ![]()
28. Floman, Y, Progression of lumbosacral isthmic spondylolisthesis in adults. Spine 2000; 25:342–347. ![]()
29. Kirkaldy-Willis, W. Managing Low Back Pain. New York: Churchill Livingstone; 1988.
30. Adams, MA, Hutton, WC, Prolapsed intervertebral disc: a hyperflexion injury. Spine 1982; 7:184–191. ![]()
31. Wilder, DG, Pope, MH, Frymoyer, JW, The biomechanics of lumbar disc herniation and the effect of overload and instability. J Spinal Disord 1988; 1:16–33. ![]()
32. Frymoyer, JW, Pope, MH. Segmental instability. Semin Spine Surg. 1991; 3:109–118.
33. Wietfeld, K. Diagnostik und konservative Therapie lumbaler Instabilitäten nach Nucleotomien. Orthop Praxis. 1995; 12:977–980.
34. Sepulveda, R, Kant, AP, Chemonucleolysis failures treated by PLIF. Clin Orthop 1985; 193:68–74. ![]()
35. Farfan, HF, Gracovetsky, S, The nature of instability. Spine 1984; 9:714–719. ![]()
36. Boden, SD, Wiesel, SW, Lumbosacral segmental motion in normal individuals. Have we been measuring instability properly? Spine 1990; 15:571–576. ![]()
37. Hayes, MA, Howard, TC, Gruel, CR, Kopta, JA, Röntgenologic evaluation of lumbar spine flexion–extension in asymptomatic individuals. Spine 1989; 14:327–331. ![]()
38. Lehman, T, Brand, R. Instability of the lower lumbar spine. Orthop Trans. 1983; 7:97.
39. Delitto, A, Erhard, RE, Bowling, RW, A treatment-based classification approach to low back syndrome: identifying and staging patients for conservative treatment. Phys Ther 1995; 75:470–485. ![]()
40. Maitland, GD. Vertebral Manipulation, 5th ed. Oxford: Butterworth Heinemann; 1986.
41. Maher, CG, Adams, R, Reliability of pain and stiffness assessments in clinical manual lumbar spine examination. Phys Ther 1994; 74:801–809. ![]()
42. Nachemson, A, Lumbar spine instability: a critical update and symposium summary. Spine 1985; 10:290–291. ![]()
43. Ogon, M, Bender, BR, Hooper, DM, et al, A dynamic approach to spinal instability, part II: hesitation and giving-way during interspinal motion. Spine 1997; 22:2859–2866. ![]()
44. MacNab, I. Backache. Baltimore: Williams & Wilkins; 1983.
45. MacNab, I, The traction spur: an indicator of segmental instability. J Bone Joint Surg 1971; 53A:663–670. ![]()
46. Nathan, H. Osteophytes of the vertebral column. An anatomical study of their development according to age, race, and sex with considerations as to their etiology and significance. J Bone Joint Surg. 1962; 44A:243–268.
47. Hayes, MA, Howard, TC, Gruel, CR, Kopra, JA, Roentgenographic evaluation of lumbar spine flexion–extension in asymptomatic individuals. Spine 1989; 14:327–331. ![]()
48. Woody J, Lehmann T, Weinstein J, et al. Excessive translation on flexion–extension radiographs in asymptomatic populations. Presented at the meeting of the International Society for the Study of the Lumbar Spine, Miami, Florida 1988.
49. Shaffer, WO, Spratt, KF, Weinstein, J, et al, Volvo award in clinical sciences. The consistency and accuracy of roentgenograms for measuring sagittal translation in the lumbar vertebral motion segment. An experimental model. Spine 1990; 15:741–750. ![]()
50. Dupuis, PR, Young-Hing, K, Cassidy, JD, Kirkaldy-Willis, WH, Radiologic diagnosis of degenerative lumbar spinal instability. Spine 1985; 10:262–276. ![]()
51. McGill, SM, Estimation of force and extensor moment contributions of the disc and ligaments at L4–L5. Spine 1988; 13:1395–1402. ![]()
52. Callaghan, JP, Gunning, JL, McGill, SM, The relationship between lumbar spine load and muscle activity during extensor exercises. Phys Ther 1998; 78:8–18. ![]()
53. Manniche, C, Hesselsoe, G, Bentzen, L, et al, Clinical trial of intensive muscle training for chronic low back pain. Lancet 1988; 24–31. ![]()
54. Manniche, C, Lundberg, E, Christensen, I, et al, Intensive dynamic back exercises for chronic low back pain: a clinical trial. Pain 1991; 57:53–63. ![]()
55. Hansen, FR, Bendix, T, Skov, P, et al, Intensive dynamic back-muscle exercises, conventional physiotherapy, or placebo-control treatment of low back pain. Spine 1993; 18:98–107. ![]()
56. McGill, SM, Distribution of tissue loads in the low back during a variety of daily and rehabilitation tasks. J Rehabil Res Dev 1997; 34:448–458. ![]()
57. Hodges, PW, Is there a role for transversus abdominis in lumbo-pelvic stability? Manual Therapy. 1999;4(20):74–86. ![]()
58. Hides, J, Stokes, MJ, Saide, ML, et al, Evidence of lumbar multifidus muscle wasting ipsilateral to symptoms in patients with acute/subacute low back pain. Spine 1994; 19:165–172. ![]()
59. Wilke, H, Wof, S, Claes, LE, et al, Stability increase of the lumbar spine with different muscle groups. Spine 1995; 20:192–198. ![]()
60. Richardson, CA, Jull, GA, Muscle control–pain control: what exercises would you prescribe? Manual Therapy 1995; 1:2–10. ![]()
61. O’Sullivan, PB, Twomey, LT, Allison, GT, Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine 1997; 22:2959–2967. ![]()
62. Wilke, HJ, Wolf, S, Claes, LE, et al, Stability increase of the lumbar spine with different muscle groups: a biomechanical in vitro study. Spine 1995; 20:192–198. ![]()
63. Liu, Y, Tipton, C, Matthes, R, et al, An in situ study of the influence of a sclerosing solution in rabbit medial collateral ligaments and its junction strength. Connect Tissue Res 1983; 11:95–102. ![]()
64. Maynard, J, Pedrini, V, Pedrini-Mille, A, et al, Morphological and biochemical effects of sodium morrhuate on tendons. J Orthop Res 1985; 3:236–248. ![]()
65. Klein, R, Dorman, T, Johnson, C. Proliferant injections for low back pain: histologic changes of injected ligaments and objective measurements of lumbar spinal mobility before and after treatment. J Neurol Orthop Med Surg. 1989; 10:123–126.
66. Klein, R, Eek, B, DeLong, B, Mooney, V, A randomized double-blind trial of dextrose–glycerine–phenol injections for chronic, low back pain. J Spinal Disord 1993; 6:23–33. ![]()
67. Deyo, RA, Ciol, MA, Cherkin, DC, et al, Lumbar spinal fusion: a cohort study of complications, reoperations, and resource used in the Medicare population. Spine 1993; 18:1463–1470. ![]()
68. Davis, H, Increasing rates of cervical and lumbar spine surgery in the United States, 1979–1990. Spine 1994; 19:1117–1124. ![]()
69. Cherkin, DC, Deyo, RA, Loeser, JD, et al, An international comparison of back surgery rates. Spine 1994; 19:1201–1206. ![]()
70. Sonntag, VKH, Marciano, FF, Is fusion indicated for lumbar spinal disorders? Spine. 1995;20(suppl):138S–142S. ![]()