Chapter 36 Lumbar and Sacral Spine
Anatomy
Osseous Anatomy
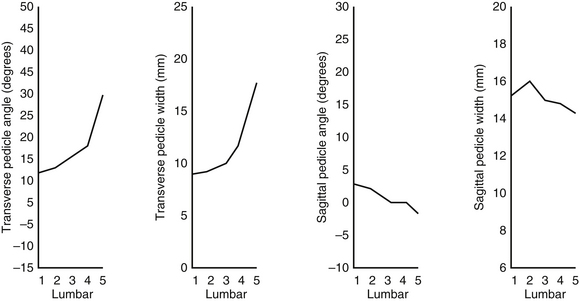
In the lumbar spine, the large osseous ring that surrounds the spinal canal is bordered ventrally by a cancellous cylindric mass (the vertebral body), dorsally by the vertebral arch, and dorsolaterally by the pedicles. Three other key vertebral elements are located near the pedicle and laminae: transverse process and superior and inferior articular processes. With its neural and bony relationships, the pedicle is key to conceptualizing the lumbar spine. The pedicles are wide and thick and are widely spaced on the rostral dorsolateral aspect of the body. In the rostral/caudal dimension, their height is one-half that of the vertebral body. The angles in the transverse and sagittal planes increase and decrease, respectively, as the lumbar spine is descended1 (Fig. 36-1).
The articular processes bear complementary relationships rostrally and caudally. The rostral facet is concave and faces dorsomedially to meet the caudal facet from above. The caudal facet, an extension of the lumina, faces ventrolaterally and complements the superior articulating facet of the vertebral body below. The junction of the two facets forms the roof of the neural foramina (Fig. 36-2).
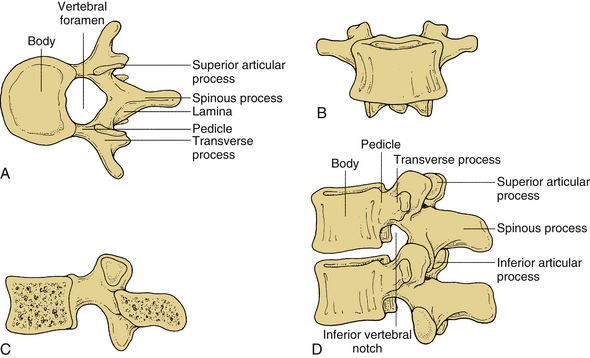
FIGURE 36-2 A, Lumbar vertebra viewed from above; B, ventral; C, median sagittal; D, in articulation.
The sacrum consists of five fused vertebrae. It has a triangular shape and forms the dorsal aspect of the pelvis. It joins with the fifth lumbar vertebra via the L5-S1 disc and facets. The five fused vertebrae have homologous structures referable to the lumbar spine. The transverse processes are the laterally projecting alae that articulate with the pelvis. A prominent midline dorsal ridge represents the fused spinous processes. More laterally, another ridge forms the sacral articular crest with a functional superior articular process at S1. This facet faces caudally and dorsally. Because of the sacrovertebral angle created by the tilt of the sacrum as it joins the fifth lumbar vertebra, this joint functions to prevent ventral displacement of the lumbar spine on the sacrum. Ventrally, transverse ridges represent fused vertebrae and enclose remnants of intervertebral discs. Foramina dorsally and ventrally provide sites of exit for the ventral and dorsal divisions of the sacral nerves. The sacrum is the most variable portion of the spine. Lengthening or shortening of the lumbar spine by deletion or addition of segments to and from the sacrum is not uncommon2 (Fig. 36-3).
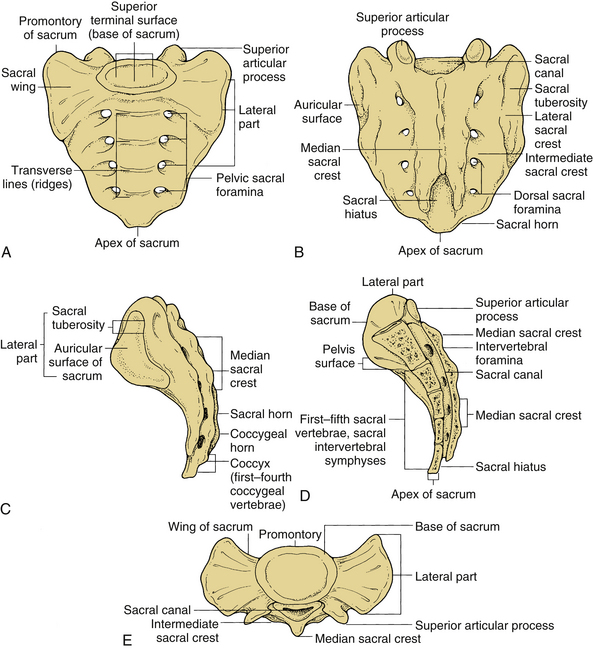
FIGURE 36-3 The sacrum: A, ventral, B, dorsal, C, sagittal, D, medial sagittal, and E, rostral views.
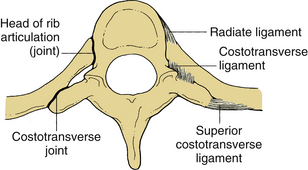
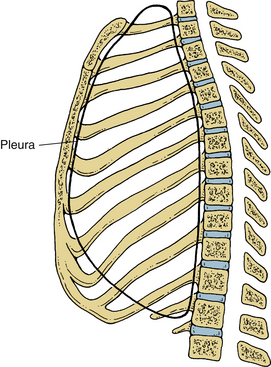
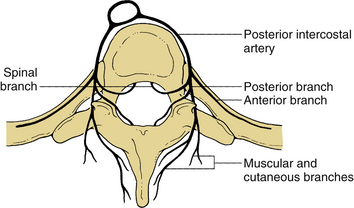
Thoracic vertebrae T2-9 have points of articulations for each rib: one on the vertebral body and the other on the corresponding transverse process. T11 and T12 have a single costal facet on their pedicles (Fig. 36-4). The typical rib has a head, a neck, a tubercle, and a shaft or body. The crest of the head is joined to the intervertebral disc by an intra-articular ligament with two surface articulations: one on the numerically corresponding vertebra and one on the vertebra above it. The neck is the nonarticulating portion of rib between the head and tubercle. The tubercle is on the dorsal portion of the rib at the junction of the neck and shaft. The tubercle of most ribs has a smooth convex facet that articulates with the transverse process of the corresponding vertebra and a rough nonarticular surface to which the lateral costotransverse ligament attaches. The body of the rib is thin and flat, with its greatest diameter in the rostral to caudal orientation. The point of greatest curvature is called the angle of the rib. The costal groove and the flange formed by the caudal border of the rib accommodate and protect the intercostal vessels and nerve that accompany the rib. The 11th and 12th ribs are short and capped with cartilage. They have a single facet on their heads and no neck or tubercle. The 11th rib has a slight angle and a shallow costal groove. The 12th rib has neither of these features. Minet3 classifies the 12th rib as long, medium, or short. The long type is parallel to the 11th rib, and the short type is horizontal and less oblique than the long type. For thoracolumbar surgery, it is important to understand the relationship of the pleural sac to the 12th rib. The pleural sac passes caudally over the inferior border to the 12th rib and continues in this direction for 1 to 2 cm. From there it passes horizontally, crossing caudally, and 3 to 4 cm lateral to the 12th rib head, it continues to pass along the 12th rib for another 7 to 8 cm3 (Fig. 36-5).
Lumbar Spine
Muscles and Ligaments
The intrinsic and extrinsic musculature adjacent to the spine is commonly dissected in approaches to the spine and provides important landmarks in specific approaches. Intrinsic muscles consist of the erector spinae, multifidus, quadratus lumborum, and deep muscles. The large erector spinae muscle is divided into three columns: iliocostalis, longissimus, and spinalis muscles. The iliocostalis muscle, as its name indicates, is the most lateral of the group and arises from the iliac crest and inserts into the ribs. The longissimus muscle, intermediate in the column, runs between the transverse processes of the vertebrae. The spinalis muscle, the most medial, inserts and attaches to spinous processes in the lumbar and thoracic region. All three columns of the erector spinae muscle extend the vertebral column and bend the vertebral column laterally.
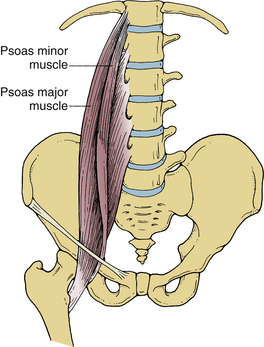
Central to the erector spinae muscles are several short muscles that interconnect adjacent and nearby vertebral bodies. This group of small muscles, called the multifidus muscles, originates on the mamillary processes of the rostral facets and runs rostrally and medially to insert on the spinous processes of vertebrae two to four segments above. The quadratus lumborum muscle is located ventral and lateral to the erector spinae muscles. This muscle originates on the iliac crest and iliolumbar ligament and runs obliquely to insert ventrally on the lowest rib and transverse processes of the upper four lumbar vertebrae. Ventral and medial to this muscle are the small intertransversarius muscles that span the transverse processes. Ventrolateral and adjacent to the lumbar vertebral bodies are the psoas muscles, which originate from the lateral aspects of the vertebral bodies and transverse processes of L1-5 and pass through the pelvis and into the thigh dorsal to the posterior inguinal ligament (Figs. 36-6 and 36-7).
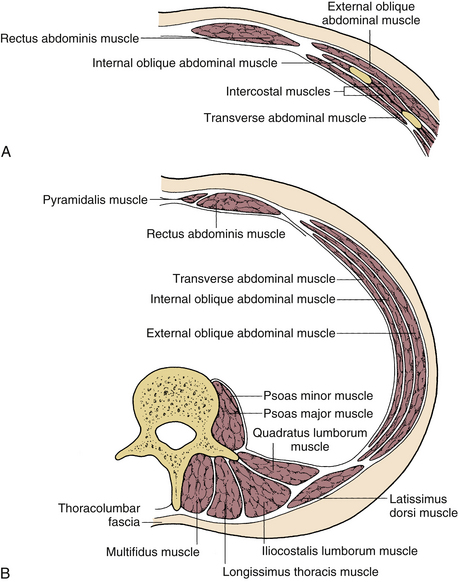
FIGURE 36-7 Coronal sections through the thoracoabdominal musculature above (A) and below (B) the umbilicus.
The extrinsic musculature consists of the rectus abdominis, external oblique, internal oblique, transversalis, latissimus dorsi, and serratus dorsalis caudalis muscles (see Fig. 36-7). The rectus muscles run bilaterally on the ventral abdominal wall from the pubis to the middle ribs. The internal and external oblique muscles and the transversalis muscles are layered superficial to deep as described. They arise from the ribs and thoracodorsal fascia dorsally and insert on the iliac crest caudally and the linea alba medially. The latissimus muscle is a large and diffuse muscle that originates on the sacrum, dorsal iliac crest, and 10th, 11th, and 12th ribs. The fibers in the costoiliac interval run rostrally and laterally. The serratus dorsalis caudalis muscle originates from the lower four ribs, runs caudally and medially, and inserts on the thoracolumbar fascia ventral to the latissimus dorsi muscle.
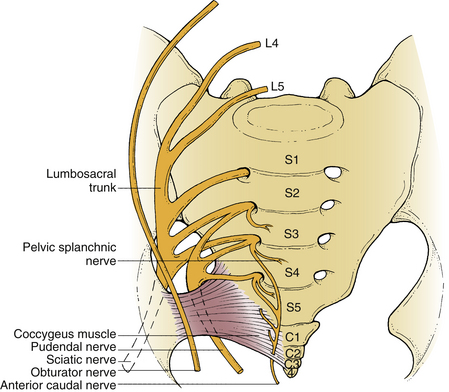
Exiting Nerve Roots
The lumbar plexus is formed within the psoas major muscle. The largest and most important branches of the lumbar plexus are the obturator and femoral nerves (L2, L3, and L4). The ilioinguinal and iliohypogastric nerves are derived from L1, enter the abdomen dorsal to the medial arcuate ligament, and pass inferolaterally, ventral to the quadratus lumborum muscle, piercing it near the anterior superior iliac spine. The genitofemoral nerve (L1 and L2) pierces the fascia iliaca and the ventral surface of the psoas major muscle and divides lateral to the common and external iliac arteries into two femoral and genital branches. The lumbosacral trunk (L4 and L5) is a large, flat nerve, from which the L4 component descends through the psoas major muscle on the medial part of the transverse process of the L5 vertebra and passes closely over the ala of the sacrum to join the first sacral nerve (Fig. 36-8).
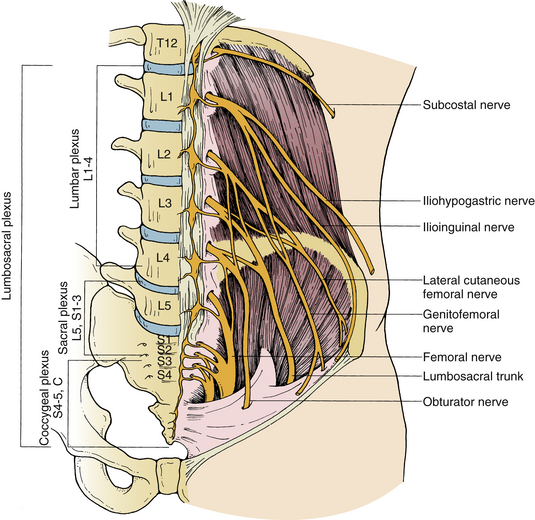
FIGURE 36-8 Anatomic representation of the lumbosacral plexus with the psoas muscle removed on one side.
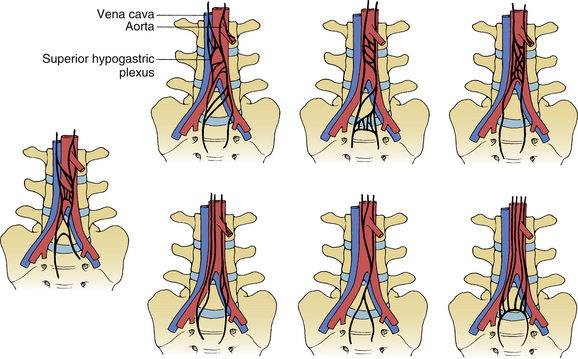
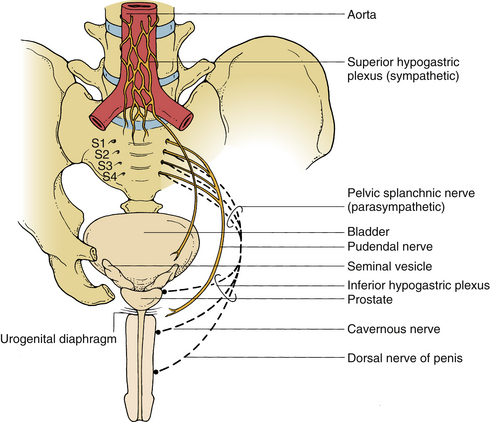
The sympathetic and parasympathetic nerves are distributed to the abdominal viscera via a tangle of plexuses and ganglia located on the ventral surface of the aorta. The principal components of this system are the celiac plexus ganglia, which are located on each side of the celiac trunk at the level of the rostral aspect of the first lumbar vertebra. The greater, lesser, and lowest splanchnic nerves are branches of thoracic sympathetic ganglia 5 to 12. The hypogastric plexus runs on the ventral surface of the aorta. It receives contributions from the lateral rami of the right and left lumbar sympathetic trunks and from median rami of the celiac plexus and the superior and inferior mesenteric plexuses. It spans the distance from the fourth lumbar to the first sacral vertebra. Its shape and bifurcations can be variable.4 In males the plexus innervates the bladder, vas deferens, and seminal vesicles and is important in the neurophysiology of ejaculation (Fig. 36-9).
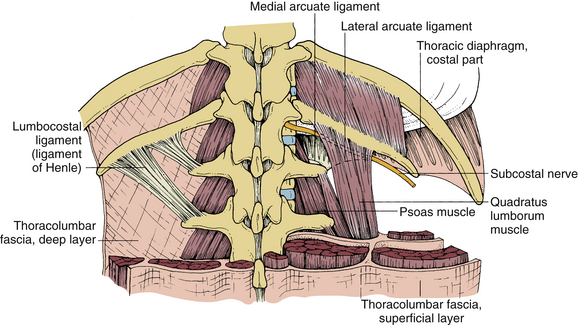
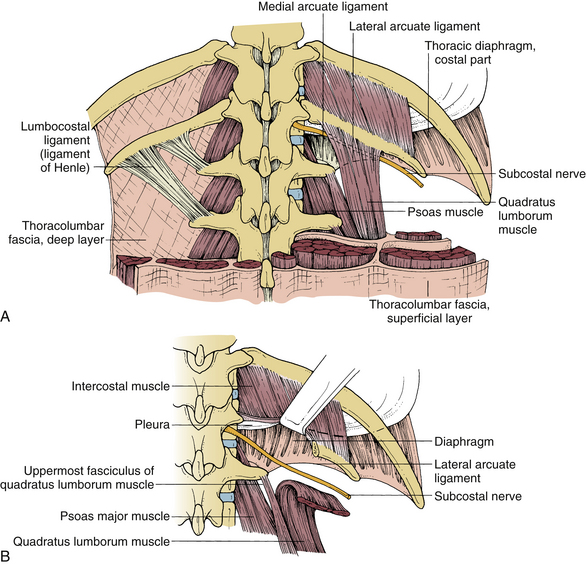
Soft Tissue Structures
The thoracolumbar junction is one of the more complicated areas of the vertebral column and has important soft tissue anatomic structures that require special attention. The thoracolumbar fascia is made up of dorsal, intermediate, and ventral layers. The dorsal layer surrounds the erector spinae muscles dorsally. It arises with the tendon of the latissimus dorsi on the sacrum and iliac crest and attaches on the spinous processes of the lumbar vertebrae. The intermediate layer of the thoracolumbar fascia attaches to all of the transverse processes of the lumber vertebrae and to the caudal border of the 12 rib. The lumbocostal ligament of Henle arises from the transverse process of L1 and runs rostrolaterally, inserting to the caudal border of the 12th rib close to its medial end. The ventral layer of the thoracolumbar fascia is attached to the lateral arcuate ligament rostrally, to the iliac crest caudally, to the transversalis fascias laterally, and to the psoas fascia medially. This layer covers the quadratus lumborum muscle and is in contact with the retroperitoneal contents5 (Fig. 36-10; see also Figs. 36-6 to 36-9).
The diaphragm consists of a muscular portion and a central aponeurosis termed the central tendon, on which the muscular portion converges (Fig. 36-11). The muscular portion is divided into three parts on the basis of its fibers’ origins: sternal, costal, and lumbar. The sternal part of the diaphragm arises from the xiphoid process. The costal part of the diaphragm arises from the internal surface of the caudal six ribs at the costal margin. The lumbar part of the diaphragm arises from the lumbar vertebrae by two crura and three arcuate ligaments. The musculotendinous crura envelop the aorta and attach ventrolaterally to the rostral two lumbar vertebral bodies on the left and the upper three on the right. The crura blend with the anterior longitudinal ligament of the lumbar spine. Three arcuate ligaments give rise to fibers of the diaphragm. The median arcuate ligament unites the medial sides of the two crura. The medial arcuate ligament on each side is a thickening of the ventral thoracolumbar fascia over the rostral part of the psoas muscle. From the medial insertion on the vertebral body, it runs over the psoas and has an attachment to the transverse process of the first lumbar vertebra. The lateral arcuate ligament is a thickening of the anterior thoracolumbar fascia running over the rostral aspect of the quadratus lumborum muscle forming attachments to the 12th rib and transverse process of the first lumbar vertebra.6
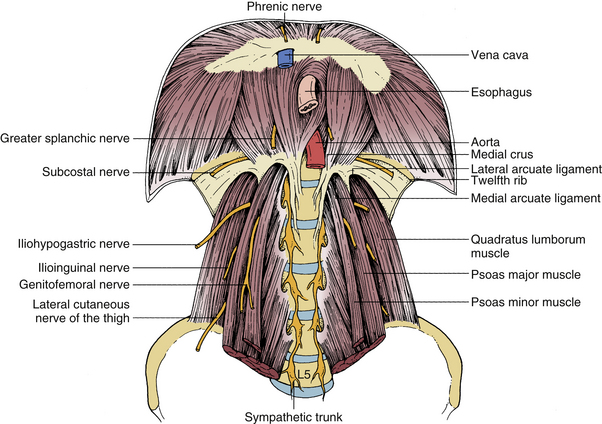
FIGURE 36-11 Anatomic representation of the diaphragm in relationship to lumbar spine and intimate structures.
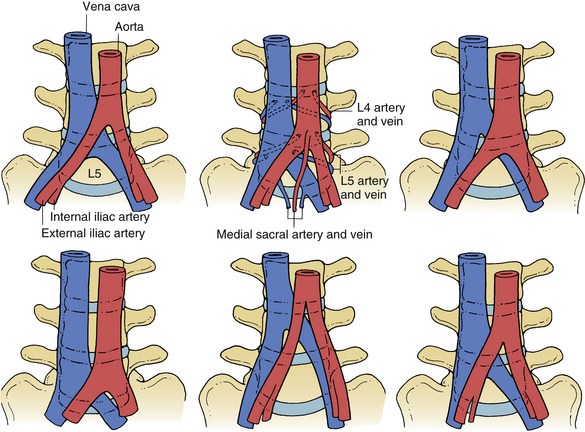
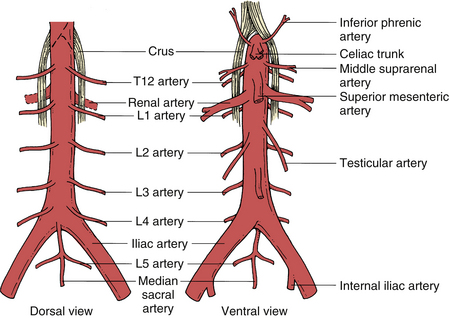
The abdominal aorta begins at the aortic hiatus in the diaphragm at the level of the T12-L1 intervertebral disc and ends at about the level of L4 by dividing into the two common iliac arteries. The inferior vena cava begins ventral to the fifth lumbar vertebra by the union of the common iliac veins and ascends to the right of the median plane. It pierces the central tendon of the diaphragm at the level of the eighth thoracic vertebra. Five anatomic variants of the aortocaval axis are outlined according to the level of bifurcation and origin of the aorta and vena cava, respectively7 (Fig. 36-12). The aorta is ventral to the vena cava and lumbar vertebral bodies and sits slightly to the left, and the vena cava is located slightly to the right.
The branches of the abdominal aorta may be grouped into four types: (1) those arising rostrally to the celiac (T12), superior mesenteric (L1), and inferior mesenteric (L3) arteries; (2) those arising laterally—the renal (L1), the middle suprarenal (L1), and the testicular or ovarian (L2) arteries; (3) those arising dorsolaterally—the parietal branches of the inferior phrenic arteries, which give rise to the superior suprarenal arteries and the four pairs of lumbar arteries; and (4) an unpaired parietal artery, the sacral artery, which arises from the dorsal surface of the aorta just proximal to its bifurcation (Fig. 36-13). The lumbar arteries pass dorsomedially. On the right they run dorsal to the inferior vena cava, dividing between the transverse processes into the ventral and dorsal branches. The ventral branch passes deep to the quadratus lumborum muscle to anastomose with the inferior epigastric arteries. Each dorsal branch passes dorsally lateral to the articular processes and supplies the spinal cord, cauda equina, meninges, erector spinae muscles, and overlying skin.8 The radicular arteries, which supply blood to the posterior and anterior spinal arteries, arise from these dorsal branches. The largest of these, the arteria radicularis magna (spinal artery of Adamkiewicz), supplies most of the blood to the caudal spinal cord including the lumbosacral enlargement (Figs. 36-14 and 36-15).
Tributaries of the inferior vena cava are the common iliac veins (L5), the lumbar veins, the right testicular or ovarian vein (the left drains into the left renal vein), the renal veins, the azygos vein, the right suprarenal vein (the left also drains into the renal vein), the inferior phrenic veins, and the hepatic veins. The lumbar veins consist of four or five segmental pairs. They may drain separately into the inferior vena cava or the common iliac vein, but they are usually united on each side by a vertical connecting vein, the ascending lumbar vein that lies dorsal to the psoas major muscle. Each ascending lumbar vein passes dorsal to the medial arcuate ligament of the diaphragm to enter the thorax. The right ascending lumbar vein joins the right subcostal vein to form the azygos vein, and the left subcostal vein forms the hemiazygos vein.6
Each kidney lies dorsal to the peritoneum on the dorsal abdominal wall. The kidneys lie along the vertebral column against the psoas muscle. The ureter is retroperitoneal throughout its length. It adheres to the peritoneum and is usually retracted with it during retroperitoneal approaches to the spine. The ureter descends nearly vertically along the psoas major muscle. On the right, it is next to the vena cava, and on both sides, it crosses the brim of the pelvis and the external iliac artery, just beyond the bifurcation of the common iliac artery.
Sacral Spine
Nerve Roots
The sacral canal contains sacral and coccygeal nerve roots. The filum terminale consists of two parts: interna and externa. The interna extends from the tip of the conus to the level of the second sacral neuroforamen. The externa begins at the level of the second sacral neuroforamen and attaches to the first coccygeal vertebra. The dorsal root ganglia is in the sacral canal, central and rostral to the foramina, from which their respective rami emerge. The sacral plexus is complex9 (Fig. 36-16). The predominant nerves of the plexus are the superior and inferior gluteal, sciatic, posterior, femoral, and pudendal nerves. The sympathetic trunk passes deep to the common iliac artery to run on the ventral surface of the sacrum. Each trunk continues caudally to the coccyx to form a single ganglion, the ganglion impar. The pelvic plexus lies embedded in the subperitoneal serosa lateral to the sacrum on the rostral surface of the obturator internus (Fig. 36-17).
Soft Tissue Structures
Important muscles in the sacral region include the gluteal, piriformis, and levator ani muscles. The floor of the pelvic cavity is made up mainly of the levator ani muscle. This muscle originates on the body of the pubis and the ischial spine and inserts on the central perineal tendon, the wall of the anal canal, the anococcygeal ligament, and the coccyx. It forms a sheet extending from the pubis ventrally, ischium laterally, and coccyx dorsally and encircles the urethra and anus in the middle. It is divided into three parts: pubococcygeus, puborectalis, and iliococcygeus muscles. The anococcygeal raphe of the ligament is the median fibrous intersection of the pubococcygeus muscle from each side and extends between the anal canal and the coccyx. Muscles in the gluteal region that become important are the gluteus maximus and the piriformis. The gluteus maximus originates on the external surface of the ileum (including the iliac crest), dorsal surface of the sacrum and coccyx, and sacrotuberous ligament. The piriformis muscle originates on the ventral surface of the sacrum and the sacrotuberous ligament.
The common iliac arteries pass caudally and laterally to bifurcate into the external and internal iliac arteries at the level of the lumbosacral disc. The right common iliac artery crosses over the right common iliac vein to lie lateral and ventral to it at the point of bifurcation of the artery. The left iliac artery runs parallel and lateral to the left iliac vein. Branches of the common and internal iliac arteries are the iliolumbar, lateral sacral, and superior and inferior gluteal arteries (Fig. 36-18). The venous anatomy is also variable, but on the whole it mirrors the arterial anatomy.
Surgical Approaches
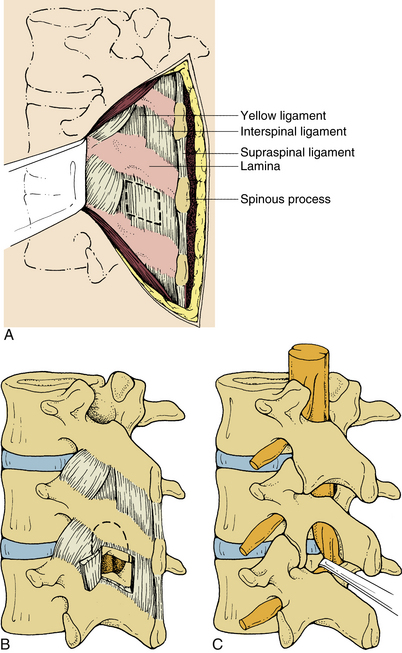
Dorsal Approach
The disc space at L5-S1 is located at the level of the interlaminar space. As one proceeds rostrally, each disc space becomes more rostral in relation to the interlaminar space. As a rule, one half of the laminae must be removed to approach the L3-4 or L4-5 discs (Fig. 36-19).
Ventral Approach
Although most approaches are dorsal, in selected cases a ventral approach is indicated. This approach has been used for lumbar sympathectomy, osteomyelitis, and ventral interbody fusion for many years.8,10–14
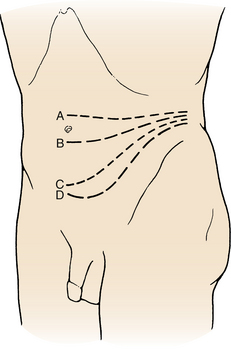
Approach to T12-L1
The length of the incision is dictated by the number of vertebrae to be exposed, and the thoracic ribs guide the rostral aspect of the incision. If the T11 body is to be adequately visualized, the T10 rib should be removed. If the body of T12 is to be exposed, the T11 rib should be removed, and for L1, the T12 rib should be removed. The incision is begun dorsally, near the midline, and it follows the appropriate rib ventrally and obliquely downward on the upper middle abdomen. Its end point is determined by the number of lumbar vertebrae to be exposed (Fig. 36-20).
With retraction of the sacrospinalis muscle, the intermediate layer of the thoracolumbar fascia is identified and followed to the ligament of Henle. This ligament is detached from the L1 transverse process at its lower border that is contiguous with the rostral insertion of the quadratus lumborum muscle. The parietal pleura is gently separated from the ventral surface of the quadratus lumborum muscle and retracted above the 12th rib. The medial half of the rib is resected after detaching the quadratus lumborum muscle from the 12th rib. The pleura is retracted upward with the periosteum of the 12th rib, and the quadratus lumborum muscle is retracted downward with the lower half of the periosteum of the 12th rib. The insertion of the lateral arcuate ligament is also detached from the transverse process of L1, leaving enough for reattachment. After verification that the pleura and peritoneum have been freed, the diaphragm is transected above the arcus lumbocostalis (medial arcuate ligament). The right medial crus of the diaphragm is also divided, following application of stay sutures. Phrenic and subcostal vessels may require ligation and incision. The subcostal nerve should be preserved (Fig. 36-21).
To expose the vertebrae, the retroperitoneal tissue and the parietal pleura are split at the thoracolumbar junction. The psoas muscle is retracted medially. A plane is established between the vertebral body and the psoas attachment to the bodies. If a body is collapsed or filled with tumor, it is important to locate normal landmarks above and below this body because tissue planes may be disrupted at the site of pathology. The psoas muscle is dissected medially until the base of the pedicle is palpated, and the ventral neural foramen is exposed. Transecting the parietal pleura in line with the vertebral bodies exposes the segmental vessels that run transversely over the vertebral bodies. They are mobilized, ligated, and transected as needed. The anterior longitudinal ligament can then be loosened with a periosteal elevator to establish the ventral plane in front of the pathologic site. When exposing the vertebral bodies, dissection should begin over the intervertebral discs, using the hinged anterior longitudinal ligament and the medially placed psoas muscle to protect the sympathetic chain and great vessels. If a more rostral exposure is required, the parietal pleura can be further retracted and the medial half of the 11th rib can be resected. During this dissection, it is important to recall the location of the ascending lumbar vein, azygos vein, thoracic duct, splanchnic nerves, and sympathetic plexus.
Retroperitoneal Approach to L2-5
The patient is placed in the lateral decubitus position, with the side of surgery dictated by the pathology. If one has a choice of sides, the left side is preferred to avoid liver retraction and manipulation of the vena cava. The spleen is smaller and can be easily retracted, although injury has been reported.15 The table is angled so that the middle of the patient’s body is concave and arched downward. This opens the space between the ribs and the iliac crest and allows the viscera to fall away. The upper hip should be flexed to relax the psoas muscle. The incision is dictated by the level to be exposed (Fig. 36-22). The umbilicus can be used as a guide. To expose L5-S1, an incision is made between the symphysis pubis and umbilicus, with a slightly higher incision used for L4-5. The incision for L3-4 is made at the umbilicus; for L2-3, the incision is above the umbilicus. If L2 exposure is desired, the skin incision begins near the midline at the level of the spinous process of T11 and continues along the 12th rib before running obliquely and vertically toward the rectus sheath. The caudal distance of the incision is dictated by the number of vertebral bodies to be exposed.
The latissimus dorsi, external oblique, internal oblique, and transversus muscles should be cut in line with the skin incision. The transversalis fascia is opened, and the retroperitoneal space is entered. The peritoneum is thin and blue and needs to be dissected thoroughly from the abdominal wall in all directions. The peritoneum is thickest laterally and is easier to separate from the transversalis in this location; toward the midline, it is thinner and more attached. A sponge or sharp dissection for adhesions can be used as needed. The correct plane of dissection may not be clearly obvious. The dissection follows dorsal to the kidney in the potential space between the renal fascia and quadratus lumborum and psoas muscles. The retroperitoneal fat and contents, along with the ureter (identified by its cylindric shape and peristaltic movements), are gently retracted medially. The quadratus lumborum muscle is identified. When palpating through this muscle, the transverse processes can be mistaken for the vertebral bodies. If in the correct plane, the psoas muscle will come into view. A common mistake is to enter the retropsoas space, which is a blind pouch between the psoas and the quadratus lumborum muscles (Fig. 36-23). On the surface of the psoas muscle, the genitofemoral nerve is noted as a small white structure lying on the belly of the psoas muscle. This nerve should be protected. The lumbar spine is immediately medial to the psoas muscle and can be obscured by this muscle. If access to L2 is required, it is helpful to resect the 12th rib. The periosteum is incised over the 12th rib, and the peripheral portion of the rib is resected, with care taken to not open the pleural cavity.
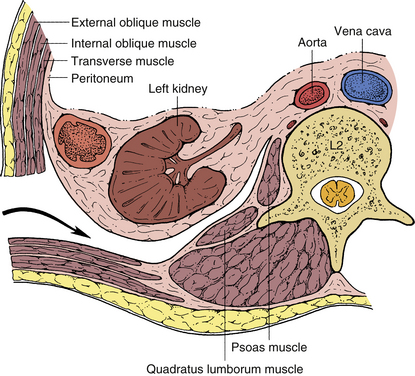
FIGURE 36-23 Retroperitoneal approach in the coronal plane and anatomic relationships to muscle and retroperitoneal contents.
A Finochietto rib retractor or Bookwalter retractor is used to open the wound longitudinally, and a padded Deaver retractor is used to retract the kidney and peritoneal contents medially. To expose the ventrolateral borders of L2-5, the psoas muscle can be mobilized dorsally with a Cobb elevator or Bovie. The sympathetic trunk, which lies just medial to the psoas muscle, should be preserved as much as possible. It should be remembered that the ascending iliolumbar vein crosses the L4-5 disc space and needs to be ligated and separated to expose the disc space and the L5 vertebral body. The segmental vessels located at the midportion of each vertebral body should be isolated, ligated, and cut outside the neuroforamina without retraction of the vessels. Once the segmental vessels have been incised, the aorta can be mobilized medially to expose the ventral aspect of the vertebral bodies. Next, the Cobb elevator can be used to separate the anterior longitudinal ligament from the ventral vertebral bodies. This provides a barrier of protection as the surgeon works on the selected vertebral body. If the pathology is not obvious or the sacral promontory is not evident, a radiograph should be obtained to determine the appropriate level.
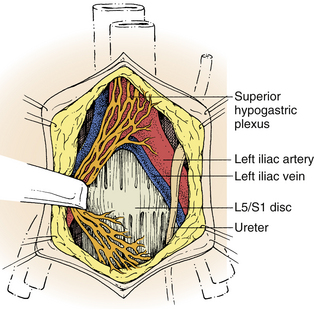
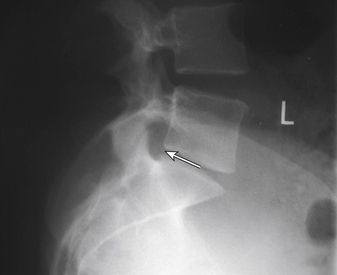
Transperitoneal or Retroperitoneal Paramedian Rectus Approach
One can decide at this point whether to use a transperitoneal or a retroperitoneal approach. A retroperitoneal approach on the left side is safe, with the viscera and hypogastric plexus being protected, but it has the disadvantage of a less direct route and less than maximal exposure of the spine.16 The parietal peritoneum can be retracted from the lateral abdominal wall with a swab stick or blunt hand dissection. Once the retroperitoneal contents are packed and retracted upward and lateral, the psoas muscle and genitofemoral nerves are visualized. The common iliac artery ventral to the vein can be seen through a layer of retroperitoneal fatty tissue. At the caudal margin of L4, the ureter and testicular vessels cross the common iliac artery laterally to medially. Midway above the aortic bifurcation runs the superior hypogastric plexus, which fans out ventrally to the promontory. For exposures above L5, the plexus is retracted medially; for exposures below L5, it is retracted laterally (Fig. 36-24). The psoas muscle is detached laterally, and the iliolumbar and segmental vessels are ligated and separated as needed. For lower lumbar access, the iliac vessels are freed from the anterior longitudinal ligament and mobilized contralaterally.
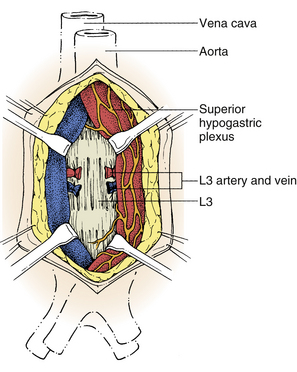
Transperitoneally, the peritoneum is a thin, blue membrane that is freed from the abdominal wall and opened in a linear fashion. The greater omentum, small bowel, and the mesenteric root are retracted rostrally. The mesocolon is retracted laterally, and the sigmoid colon retracted caudally. After the bowel is mobilized, the aortic bifurcation and sacral promontory are identified through the dorsal peritoneum. The dorsal peritoneum is opened in a linear fashion along the right common iliac artery from the aortic bifurcation to the bifurcation of the internal and external iliac arteries. Care should be taken to identify the ureter, which should cross the right external iliac artery and the hypogastric plexus, which is directly ventral to the fifth lumbar vertebra and the L5-S1 disc space. To aid in dissection, saline solution is infiltrated into the dorsal peritoneal tissue before incision. This elevates the peritoneal tissue while leaving the superior hypogastric plexus adherent to the aorta.5 The plexus is best preserved by finding the plane between the anterior longitudinal ligament and the prevertebral tissue and mobilizing the structures en bloc. The sacral vein and artery may be adherent to the sacrum. Ligation and incision may be necessary to mobilize the large vessels laterally. L3 and L4 may also be exposed in this dissection by ligating and transecting appropriate segmental vessels to allow lateral retraction of the aorta and common iliac arteries (Fig. 36-25). If the aortic bifurcation is located more rostral than usual, an interiliac approach may be used.
The parietal peritoneum is closed with running absorbable suture. Before the omentum is pulled down, one must ensure that no torsion is present on the mesenteric root. The ventral peritoneum is also closed, as was the dorsal peritoneum. The rectus and skin are closed in multiple layers.
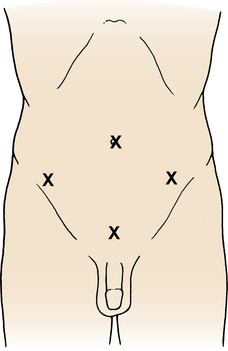
Laparoscopic Transperitoneal Approach
Especially for the case of disc pathology at L5-S1, a laparoscopic approach allows for a direct ventral exposure without the need for open laparotomy. As with the standard open procedure, a routine bowel prep, a Foley catheter, and an orogastric tube are used. The patient is positioned supine in steep Trendelenburg to aid in retracting the peritoneal contents toward the upper abdomen. Portals are placed in a diamond shape, with the superior/periumbilical portal being used for the camera, the middle or lateral portals for dissection and retraction, and the suprapubic portal for the spinal instrumentation (Fig. 36-26). The spinal working portal is not placed until the disc space is defined and the dorsal peritoneum and vasculature have been dissected free from it.
Dissection of the peritoneum is performed through a right-sided vertical incision as described earlier, with care taken to avoid coagulating on or near the hypogastric plexus. For exposure to the L5-S1 disc space, the middle sacral artery and several small veins may need to be clipped and then ligated. Once the disc space has been exposed, a long needle may be used to determine the angle of the L5-S1 disc space. This technique allows for optimal positioning for the spinal working portal, and it greatly assists the procedure (Fig. 36-27). Once completed, each portal is removed and each incision is closed in layers.
Approaches to the Sacrum
Surgical approaches to the sacrum vary according to the location of the pathologic lesion and according to whether debulking or en bloc resection is the surgical goal. This area is surgically challenging because of (1) its relationship to the pelvis, (2) dorsal tilt, (3) concavity, (4) long intraosseous course of the vertically positioned sacral nerve roots, and (5) approximation to the iliac wings and overhang of the superior iliac crests.17 Often, combined approaches are necessary because of these anatomic constraints. Ventral and dorsal approaches that have been described for the low lumbar spine are often applicable to the sacrum. Other approaches that are useful are the lateral sacroiliac approach and the perineal approach (if the pathology is caudal or extending laterally outside of the sacrum into the iliac wings). A combined ventral/dorsal abdominosacral approach or a radical sacrectomy is useful if en bloc resection is desired.17,18
The ventral approach is preferred for complete visualization of the presacral space and can be achieved with either transabdominal or retroperitoneal exposure.19 The former is preferred if bilateral visualization of the sacrum is desired, as in the case of large tumors. Ventral access allows exposure of the iliac and sacral vessels and other viscera for early control of the vascular supply of the tumor and for dissection of the tumor-viscera junction. These approaches provide good exposure of the mid sacrum and upper sacrum. Intradural or intraspinal tumors cannot be adequately exposed from a ventral approach.20 The main advantage of the retroperitoneal approach is the option for a combined retroperitoneal/dorsal exposure for intraspinal en bloc tumor resection.
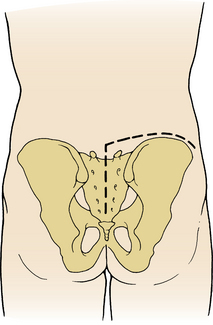
For lesions below the mid sacrum or upper sacrum (Fig. 36-28), the perineal approach is indicated.7 The patient is positioned in the flexed prone (i.e., Kraske) position. A single longitudinal incision is made, extending below the coccyx. Separating the anococcygeal raphe and releasing the gluteal and levator ani muscles exposes the presacral space. The anal canal and rectum are bluntly dissected from the tumor surface. After the tumor margins are identified, the lateral sacral attachments of the piriformis muscle and the sacrospinous and sacrotuberous ligaments are incised bilaterally. A laminectomy is performed dorsally at the foramina, one space above the lesion. The filum externa and nerve roots caudal to the determined level are divided and sectioned. An osteotome is used to section the sacrum ventrally through the perineal opening at the appropriate level, usually below S3. The tumor can then be removed en bloc or with wide margins. The wound is closed in layers over a suction drain.
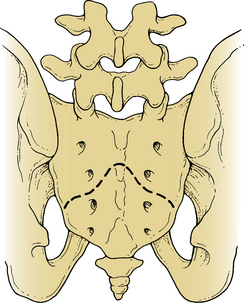
FIGURE 36-28 Dorsal representation of the lower third of sacrum that can be removed through a perineal approach.
The lateral approach to the sacroiliac joint allows simultaneous exposure of the dorsal and ventral surface of the sacroiliac joint for resection of tumors that involve the sacroiliac joint, lateral ala, and medial iliac wing. The incision is shaped like a hockey stick, starting over the sacrum and curving laterally over the iliac crest (Fig. 36-29). The muscular attachments of the abdominal, erector spinae, and gluteus muscles and the lumbodorsal fascia are detached and reflected. The gluteus muscles are elevated using a subperiosteal technique down to the sciatic notch. The gluteal vessels and nerves should be preserved. Ventrally subperiosteal elevation of the iliac and psoas muscles exposes the sacroiliac joint. Care must be taken to not injure the lumbosacral nerve trunk as it passes ventral to the surface of the sacroiliac joint. The osteotomy is performed in a dorsoventral direction. The sacral osteotomy is begun lateral to the upper three dorsal neuroforamina and directed ventrally. Laterally, the iliac osteotomy is carried down to the sciatic notch. The entire specimen is removed en bloc. The bony margins are covered with bone wax and Gelfoam, as desired, and closed in layers over drains.17
The abdominosacral approach is a combination of a low ventral sacral approach and a dorsal sacral approach.8 It is also used for the sacrectomy, if en bloc resection is indicated.18 The incision for the ventral approach varies, depending on whether rectum resection is required. If it can be preserved, the peritoneum need not be opened. A generous, semicircular incision provides adequate exposure of the sacrum after retracting the peritoneal contents rostrally. The patient is positioned supine with legs bent and flexed. The semicircular incision is made just above the pubis bone, cutting through the tendon of the rectus muscle, 1 cm above its attachments bilaterally (see Fig. 36-28). The peritoneum is swept upward to expose the common and external and internal iliac vessels. Vessel loops are applied for vascular control. This dissection is performed medially under the dorsal parietal peritoneum, preserving the superior hypogastric plexus and ureter, and meets in the midline behind the rectum.
The internal iliac arteries and veins are separated and controlled with vessel loops. The lateral and medial sacral veins and arteries are incised and ligated. If a sacrectomy above S1 is to be performed, iliolumbar vessels must also be taken. The periosteum is stripped, and the sympathetic nerve trunk is incised ventral to S1. Lateral to the sympathetic trunk, the lumbosacral nerves L4 and L5 pass ventral to the sacral wing and the sacroiliac joint. These must be released and protected. Finally, the sacrum is removed via osteotomy. It is advised that the osteotomy line be carried past the sacroiliac joint so that it can be palpated during the dorsal approach (Fig. 36-30). Also, if an en bloc resection is desired, the osteotomy should be performed one level above the tumor. The wound is closed in multiple layers or is closed temporarily, if the rectum is to be resected.
For a combined procedure, the patient is turned and a dorsal midline incision is made from L5 to the coccyx. The iliac attachments of the gluteus muscles are transected, leaving a cuff for reattachment. The sacral attachments of the gluteus maximus and underlying piriformis muscles and the anococcygeal, sacrospinous, and sacrotuberous ligaments are transected, also leaving a cuff. The gluteal nerves and vessels are preserved, if possible. The sciatic nerves are dissected through the sciatic notch and preserved. A partial lower L5 and upper sacral laminectomy is performed to expose the dural sac, which is ligated just below the last nerve root to be preserved. The ventral osteotomy line is then palpated, and the dorsal osteotomy is performed. This should extend from the midline through the sacroiliac joint. Stabilization of the lumbar spine to the ileum may be required, if the L5-S1 joints are taken. However, if the S1 vertebral body is left intact, stabilization is usually not necessary. Once the osteotomy is complete, the distal ends of the sacrificed sacral nerve roots are divided just proximal to their entry into the sciatic nerve. Bleeding is usually profuse. Hemostasis should be quickly achieved with bone wax and electrocautery. If the rectum can be preserved, the anal region is released from the dissecting bands that attach it to the coccyx. However, if it is to be included, the levator ani is transected on each side. In an en bloc procedure, the sacrospinal muscles are taken with the specimen to avoid violating the tumor wall. The wound is closed in multiple layers over a drain. If the rectum has been included in the specimen, the patient is placed in the supine position and the abdomen is opened again. The sigmoid colon is removed from its mesentery, a colostomy is performed, and the pelvic peritoneum is closed. The wound is again closed in a standard fashion.
Complications
Vascular Complications
Lumbar veins can be variable in location, especially the fifth, or iliolumbar, vein. This vein drains into either the vena cava or left iliac vein and can become a tether, if it becomes necessary to move the vena cava from left to right. The risk of avulsion of the vein directly off the vena cava exists and can cause rapid blood loss. As the left iliac vein courses over the disc space at L5-S1, it can be stretched and flat. It must be identified and controlled to avoid injury when opening the L5-S1 disc space.21 This vein can also be large, bulbous, and difficult to retract. If it is lacerated, proximal and distal control must be obtained before repair.
Pulmonary Complications
Pleural tears should be treated with a tube thoracostomy. Chylothorax has been reported because of damage to the thoracic duct during ventral surgery while mobilizing the right crus of the diaphragm.22
Neural Complications
Neural injury can occur to the superior hypogastric plexus, sympathetic chain, cauda equina, or lumbosacral plexus. The superior hypogastric plexus is responsible for closure of the bladder neck during ejaculation. If the plexus is damaged, the result may be retrograde ejaculation.20 This damage may be avoided by careful dissection of structures within the bifurcation of the aorta. By entering this area to the right of the left iliac artery and vein and sweeping the tissue from left to right, one can retract this tissue en bloc to preserve the plexus (see Fig. 36-24). Blunt dissection with gentle retraction of the prevertebral tissue must be used and excessive electrocautery avoided.
The paraspinous sympathetic lumbar chain must usually be stretched or cut in the normal course of the ventral approach. Usually, the patient complains of a cold foot on the opposite side of the dissection. In fact, the ipsilateral foot is abnormally warm because of the lack of vasoconstrictive ability on the side of the surgery.
Benzel E.C. Biomechanically relevant anatomy and material properties of the spine and associated elements. In Benzel E.C., editor: Biomechanics of spine stabilization: principles and clinical practice, ed 1, New York: McGraw-Hill, p 3, 1995.
Found E.M., Weinstein J.N. Surgical approaches to the lumbar spine. In: Frymoyer J.W., editor. The adult spine: principles and practice. ed 1. Philadelphia: Lippincott-Raven; 1991:1522.
McCormick P.C., Post K.D. Surgical approaches to the sacrum. In: Doty J.R., Rengachry S.S., editors. Surgical disorders of the sacrum. ed 1. New York: Thieme; 1994:257.
Sacks S. Anterior interbody fusion of the lumbar spine. J Bone Joint Surg [Br]. 1965;47:211.
Watkins R. Anterior lumbar interbody fusion surgical complications. Clin Orthop. 1992;284:47.
1. Benzel E.C. Biomechanically relevant anatomy and material properties of the spine and associated elements. In Benzel E.C., editor: Biomechanics of spine stabilization: principles and clinical practice, ed 1, New York: McGraw-Hill, p 3, 1995.
2. Stephen E.I., Botsford D.J. Surgical anatomy and operative approaches to the sacrum. In: Frymoyer J.W., editor. The adult spine: principles and practice. ed 1. Philadelphia: Lippincott-Raven; 1991:2099.
3. Minet J. Etude de la 12 cote et de 3 ses variations: application a la incision lombaire. Arch D Mald. 1935;9:47.
4. Labate J.S. The surgical anatomy of the superior hypogastric plexus—“presacral nerve.”. Surg Gynecol Obstet. 1938;67:199.
5. Mirbaha M.M. Anterior approach to the thoracolumbar junction by a retroperitoneal-extrapleural technic. Clin Orthop. 1973;91:41.
6. Moore K.L. The abdomen. In Moore K.L., Dalley A.F., editors: Clinically oriented anatomy, ed 2, Baltimore: Williams & Wilkins, 1985. p 268
7. Louis R. Chirurgie de rachis. Anatomie Chirurgicale et Voles D’Abord. Berlin: Springer-Verlag; 1982.
8. Crock H.V. Anterior lumbar interbody fusion. Clin Orthop. 1980;82:157.
9. Rengachry S.S. Surgical anatomy of the sacrum. In: Doty J.R., Rengachry S.S., editors. Surgical disorders of the sacrum. ed 1. New York: Thieme; 1994:31.
10. Blumenthal S.L., Baker J., Dossett A., Selby K.D. The role of anterior lumbar fusion for internal disc disruption. Spine (Phila Pa 1976). 1988;13:566.
11. Freebody D., Bendall R., Taylor R.D. Anterior transperitoneal lumbar fusion. J Bone Joint Surg [Br]. 1971;53:617.
12. Kirkaldy-Willis W.H., Thomas G.T. Anterior approaches in the diagnosis and treatment of infections of the vertebral bodies. J Bone Joint Surg [Am]. 1965;47:87.
13. Newman M.H., Grinstead G.L. Anterior lumbar interbody fusion for internal disc disruption. Spine (Phila Pa 1976). 1992;17:831.
14. Sterner B., Gunterberg B. High amputation of the sacrum for extirpation of tumors. Spine (Phila Pa 1976). 1978;3:351.
15. Hodge D.W., DeWald R.L. Splenic injury complicating the anterior thoracoabdominal surgical approach for scoliosis. J Bone Joint Surg [Am]. 1983;65:396.
16. Found E.M., Weinstein J.N. Surgical approaches to the lumbar spine. In: Frymoyer J.W., editor. The adult spine: principles and practice. ed 1. Philadelphia: Lippincott-Raven; 1991:1522.
17. McCormick P.C., Post K.D. Surgical approaches to the sacrum. In: Doty J.R., Rengachry S.S., editors. Surgical disorders of the sacrum. ed 1. New York: Thieme; 1994:257.
18. Sacks S. Anterior interbody fusion of the lumbar spine. J Bone Joint Surg [Br]. 1965;47:211.
19. Huth J.F., Dawson E.G., Eilber F.R. Abdominosacral resection for malignant tumors of the sacrum. Am J Surg. 1984;148:157.
20. Johnson R.N., McGuire E.J. Urogenital complications of anterior approaches to the lumbar spine. Clin Orthop. 1981;154:114.
21. Watkins R. Anterior lumbar interbody fusion surgical complications. Clin Orthop. 1992;284:47.
22. Eisenstein S., O’Brien J.P. Chylothorax: a complication of Dwyer’s anterior instrumentation. Br J Surg. 1977;64:339.