LOWER LEG, ANKLE, AND FOOT
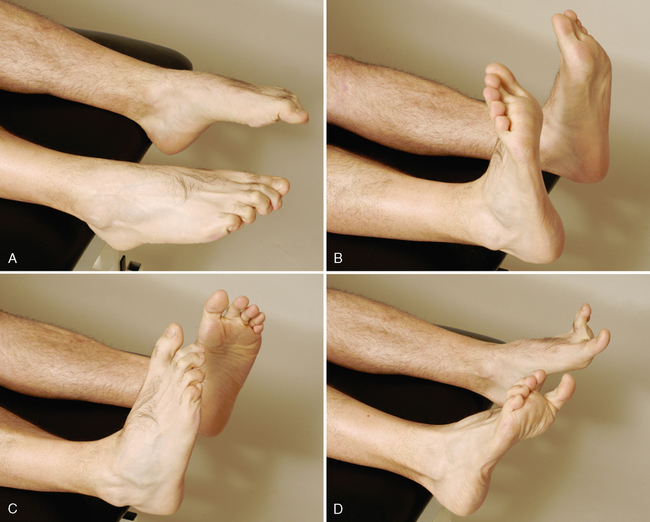
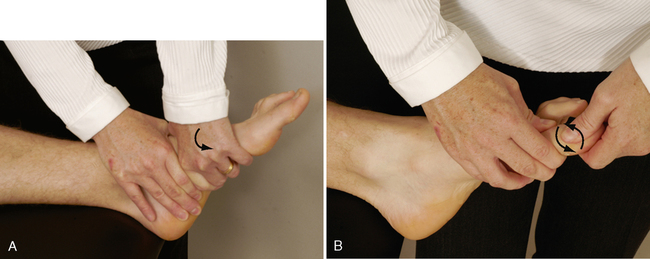
SPECIAL TESTS FOR NEUTRAL POSITION OF THE TALUS
Relevant Special Tests
Suspected Injury
• Talar position tests are not designed to identify specifically any particular pathological condition; rather, they identify anatomical and biomechanical abnormalities that contribute to a pathological condition. That pathology may occur locally at the foot and ankle or remotely at areas such as the back, knee, or hip.
Epidemiology and Demographics
The overall prevalence of malalignment reported in the literature ranges from 10% in the Cheshire Foot Pain and Disability Survey in the United Kingdom to 28% in the Framingham Foot Study in the United States. Clinically, it has been hypothesized that abnormal talar alignment and mechanics can result in pathological conditions of the foot. Regardless of the prevalence of foot pain, the cause-and-effect relationship between talar position and pathological conditions has yet to be definitively determined.6–10
Mechanism of Injury
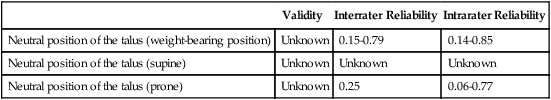
RELIABILITY/SPECIFICITY/SENSITIVITY COMPARISON11–16
| Validity | Interrater Reliability | Intrarater Reliability | |
| Neutral position of the talus (weight-bearing position) | Unknown | 0.15-0.79 | 0.14-0.85 |
| Neutral position of the talus (supine) | Unknown | Unknown | Unknown |
| Neutral position of the talus (prone) | Unknown | 0.25 | 0.06-0.77 |
SPECIAL TESTS FOR ALIGNMENT
Relevant Special Tests
Epidemiology and Demographics
Few population-based studies have examined the prevalence of foot pain in the general population. Causal relationships between specific malalignments and injuries have been difficult to verify. In a random sampling of people in Australia, foot pain affected nearly 1 in 5 individuals. The pain was associated with increased age, female gender, obesity, and pain in other body regions, and it had a significant detrimental impact on health-related quality of life. The overall prevalence reported in this study was higher than that reported in the Cheshire Foot Pain and Disability Survey in the United Kingdom (10%). However, it was lower than the prevalence rates reported in two studies in the United States: the National Health Interview Survey in the United States (24%) and the Framingham Foot Study (28%).6–10
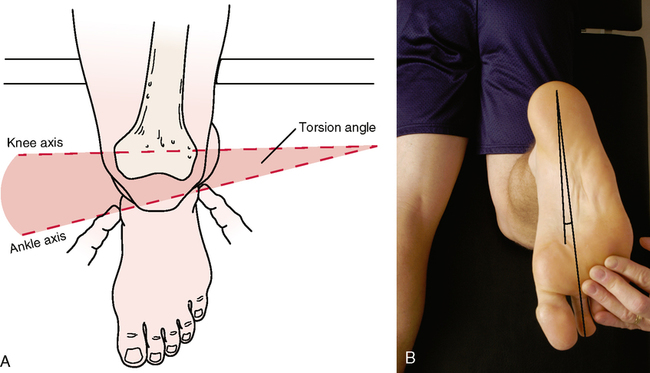
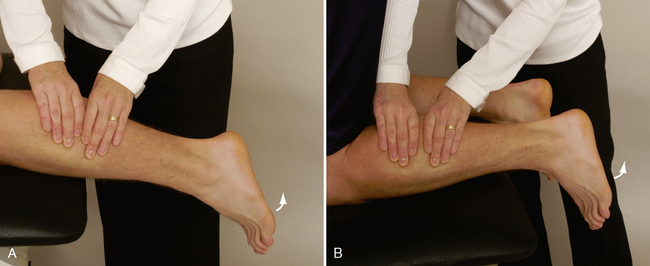
SPECIAL TEST FOR TIBIAL TORSION
Relevant Special Test
Epidemiology and Demographics
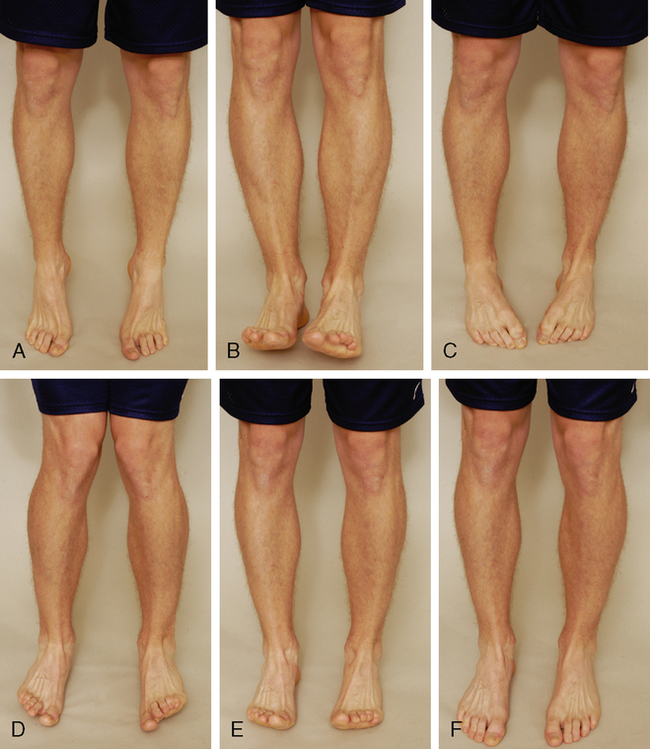
Tibial torsion usually is first noticed in children as they approach 2 years of age. Some tibial medial rotation is normal in newborns. This medial rotation usually straightens during the first year of life. In the case of excessive tibial torsion, the tibial rotation fails to straighten or the amount of rotation is too great to correct totally. It becomes more apparent as the child begins to walk, although it usually is present before then. No gender preference is apparent; males and females are equally affected. It is more common for patients to be affected bilaterally. Two-thirds of patients with tibial torsion are affected in both tibias.25–27
Relevant Signs and Symptoms
Tibial torsions usually are painless. Functionally, severe in-toeing or out-toeing may result in abnormal gait mechanics. Patients may appear “knock-kneed,” “pigeon-toed,” or “bow-legged.” Over time, the abnormal mechanics alter the forces placed on associated joints and structures, resulting in a pathological condition. At this point, the patient’s signs and symptoms reflect the resultant condition.28,29
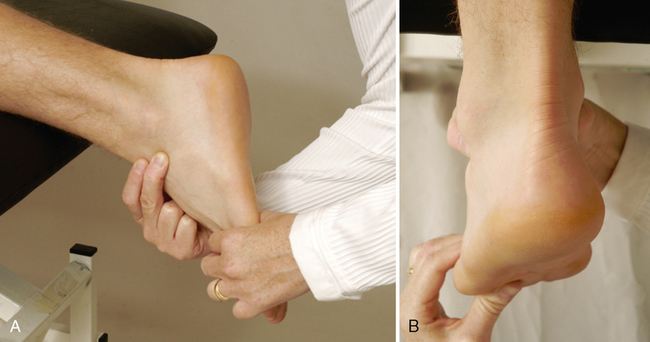
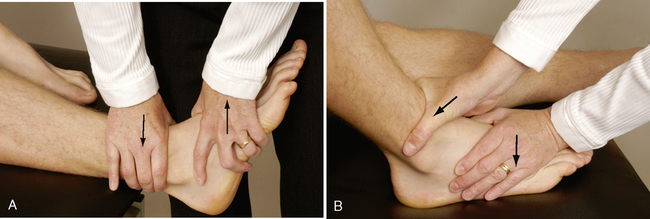
SPECIAL TESTS FOR LIGAMENTOUS INSTABILITY
Relevant Special Tests
Definition
Ankle sprains are classified into three categories:32–35
• Lateral (low ankle) sprains occur when the ligaments on the lateral portion of the ankle are injured. The most common ligaments injured are the anterior talofibular ligament and the calcaneofibular ligament.
• Syndesmotic (high ankle) sprains are synonymous with anterior tibiofibular ligaments sprains. These sprains occur when the ligaments between the two major bones of the lower leg (the tibia and the fibula) are injured at the level of the ankle.
• Medial ankle sprains are the rarest and occur when the deltoid ligament is injured.
Mechanism of Injury
Lateral (low ankle) sprain: Lateral ankle ligament injuries usually are the result of a rapid inversion movement at the ankle. The patient commonly reports that the ankle “rolled,” or the person states that a pop was heard during activities such as planting the foot when running, stepping up or down, or stepping or landing on an uneven surface.
Syndesmosis (high ankle) sprain: Syndesmotic sprains are believed to occur when the ankle is planted in dorsiflexion with lateral rotation of the lower leg. Most syndesmotic ankle sprains are believed to be the result of direct contact between individuals.
Medial ankle sprain: Medial ankle sprains occur with plantar flexion with eversion.