188 Local and Regional Anesthesia
• Alternatives to local infiltration for anesthesia include topical anesthesia and regional nerve blocks.
• Comfortable wound repair requires adequate anesthesia.
• Local infiltration may be inadequate or suboptimal in certain situations.
• For the safety and efficacy of regional anesthesia, the clinician must have a detailed understanding of the local anatomy.
• Ultrasound is a very useful adjunct to regional anesthesia.
Selection of Anesthetic Agents
Mechanism of Action
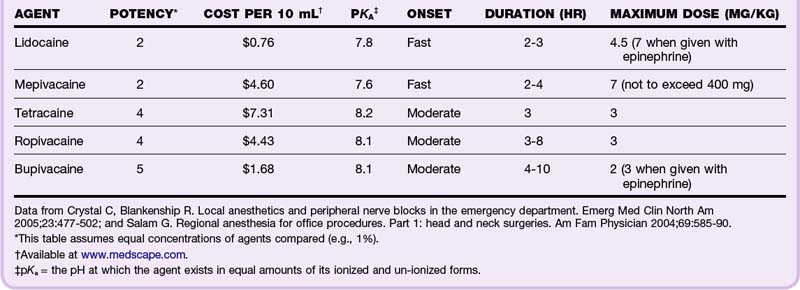
Local anesthetics usually have an aromatic ring structure connected to a tertiary amine by either an ester or an amide link. This link determines the class of the agent, ester or amide. Local anesthetics work by reversibly binding to and blocking neuronal sodium channels, thereby blocking conduction of the nerve impulse. Their potency, onset, and duration of action are determined by their ability to access and bind these sodium channels. The higher the lipid solubility, the higher the potency of the anesthetic. The higher their protein binding, the longer the duration of action. Onset of action is determined by the pKa, or the pH at which the agent exists in equal amounts of its ionized and un-ionized forms. The closer the pKa is to physiologic pH, the faster the onset of action.1 Most local anesthetic agents are associated with a burning sensation that lasts several seconds before the onset of anesthesia. Patients should be warned of this sensation before administration (Table 188.1).
Toxicity
An intercostal block has the highest potential for toxicity; therefore, the maximum amount of anesthetic agent recommended for this location is only one tenth of the maximum for peripheral nerve blocks.1 All sites are associated with a certain degree of risk, especially when accidental intravascular injection is likely.
Signs of CNS toxicity with local anesthetics are presented in Box 188.1.
If exposure is not halted, toxicity can progress to seizures, coma, respiratory depression, and cardiorespiratory arrest. Higher doses result in cardiovascular toxicity and lead to tachycardias, sinus arrest, atrioventricular dissociation, hypotension, and full arrest. Premedication with benzodiazepines may blunt the CNS toxicity, and in these cases the first sign of toxicity to develop may be cardiovascular collapse.2,3 Amides are metabolized by the liver, and patients with hepatic dysfunction may be predisposed to systemic toxicity. Esters are metabolized by plasma pseudocholinesterase, and therefore patients with pseudocholinesterase deficiency, such as those with myasthenia gravis, are at higher risk for systemic toxicity. In addition, metabolites of prilocaine (a component of EMLA cream) and benzocaine have been associated with methemoglobinemia.
Systemic Agents
Lidocaine
Lidocaine is the most commonly used local anesthetic agent. Its low cost, rapid onset, duration, and toxicity profile make it ideal for most routine applications. The maximum dose of lidocaine is 4 to 4.5 mg/kg (e.g., a 70-kg patient should receive no more than 300 mg, or 30 mL of a 1% solution). The maximum dose may be increased to 7 mg/kg when lidocaine is given with epinephrine but will also cause an increase in sympathomimetic side effects (tachycardia and hypertension) and a theoretically higher risk for infection because of diminished blood supply to the affected area. The pain of injection can be reduced either by warming lidocaine to body temperature before administration4 or by buffering it with sodium bicarbonate (1 mL sodium bicarbonate to 9 mL of 1% lidocaine).2,5
Allergic Reactions
True allergic reactions to local anesthetics are relatively rare. They are usually secondary to the preservative rather than to the agent itself. If an allergy is reported but not verified, the emergency physician should consider using a preservative-free agent, such as cardiac lidocaine from the “code” cart. Other options include switching classes (allergy to esters is more common than allergy to amides, and cross-reactivity is common within the class) or using benzyl alcohol,6 diphenhydramine,7 ice, or normal saline injection. An easy way to determine the class of an agent is to remember that all amides have two i’s in their names and the esters only have one. If a patient is truly allergic to lidocaine, none of the anesthetic agents with two i’s should be used (diphenhydramine is an exception to this rule of thumb because it is not classically considered an anesthetic agent).
Topical Agents
Lidocaine, Epinephrine, and Tetracaine
LET (lidocaine 4%, epinephrine 0.1%, tetracaine 0.5%) is an excellent and safe topical anesthetic agent. It can be premixed by the hospital pharmacy and stored in the refrigerator for use in the ED. It is applied to wounds by soaking a cotton ball in LET and then securing the cotton ball to the wound for 15 to 30 minutes. Blanching of the skin around the wound indicates adequate anesthesia. Additional injected anesthetic may be required, but its application should be much more comfortable for the patient after LET pretreatment. LET (or any mixture containing epinephrine) should, by convention, not be used on the ear, nose, penis, or digits because of its vasoconstrictor effects.8,9
EMLA
EMLA (eutectic mixture of local anesthetics: 2.5% lidocaine and 2.5% prilocaine) is approved by the FDA only for use on intact skin, although successful use in open wounds has been reported in the medical literature. Approximately 1 hour of topical application of EMLA is required to achieve local anesthesia, a characteristic that limits its usefulness in emergency cases. Infants younger than 3 months are at theoretically higher risk for the development of methemoglobinemia from EMLA because of inadequate levels of methemoglobin reductase.1,8,9
Liposomal Lidocaine
ELA-Max is a relatively new proprietary mixture of 4% liposomal lidocaine that has been approved by the FDA for the temporary relief of pain from minor cuts and abrasions. Its onset of action is much shorter than that of EMLA (only 30 minutes), and it carries a much lower risk for methemoglobinemia because it does not contain prilocaine. This formulation may replace EMLA for most topical indications.8,9
Regional Nerve Blocks
General Technique
1. Prepare the skin with povidone-iodine or other antiseptic skin solution.
2. Identify the area’s landmarks.
3. Induce a superficial skin wheal at the injection site to reduce the discomfort of further manipulation.
4. Advance the needle to the target area while asking the patient to report any paresthesias.
5. If the patient does report paresthesias, thus indicating that the needle is within the nerve sheath, withdraw the needle 1 to 2 mm, aspirate to ensure that the needle is not in a vessel, and inject the agent slowly.
Upper Extremity Blocks
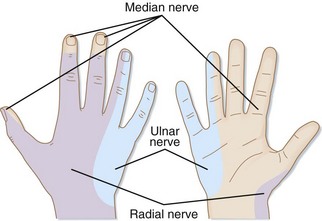
Median Nerve
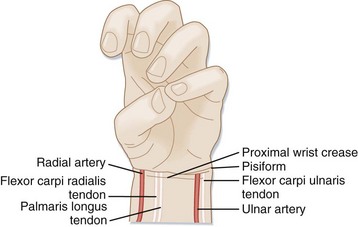
The median nerve provides sensation to the palmar surface of the radial half of the hand and the first through fourth fingers (Fig. 188.1). The median nerve is accessed between the palmaris longus tendon and the flexor carpi radialis tendon at the proximal wrist crease (Fig. 188.2). The patient should be instructed to oppose the thumb and fifth digit with the wrist flexed to allow visualization of these landmarks. The needle is inserted perpendicularly between the palmaris longus and flexor carpi radialis tendons and is then advanced until a “pop” is felt as the flexor retinaculum is penetrated. The needle is then advanced 0.5 cm past the retinaculum, aspiration is performed to verify that the needle is not in a vessel, and 5 mL of anesthetic agent is injected slowly as the needle is withdrawn.
Ulnar Nerve
The ulnar nerve provides sensation to the palmar surface of the ulnar half of the hand and the fourth and fifth fingers (see Fig. 188.1). The ulnar nerve travels very close to the ulnar artery, deep to the flexor carpi ulnaris, so extra care must be taken to avoid intraarterial injection. The landmarks for this block are the flexor carpi ulnaris and the proximal wrist crease (see Fig. 188.2). The patient should be instructed to flex the wrist, and the operator should palpate the tendon proximal to the pisiform. With the lateral approach, the needle is advanced 1 to 1.5 cm horizontally under the flexor carpi ulnaris tendon, aspiration is performed to ensure that the needle is not located intraarterially, and 5 mL of anesthetic agent is slowly injected while the needle is withdrawn.
The ulnar nerve also gives off several subcutaneous branches that travel from the lateral border of the flexor carpi ulnaris to the dorsal midline. These branches are blocked by subcutaneous injection of an additional 5 to 10 mL in a superficial ringlike wheal from the lateral aspect of the proximal wrist crease to the dorsal midline (see Fig. 188.2).
Radial Nerve
The radial nerve provides sensation to the dorsal radial aspect of the hand and the first through third digits (see Fig. 188.1). The radial nerve travels lateral to the radial artery at the wrist and gives off superficial cutaneous branches that travel laterally to the dorsal midline. The landmarks for this block are the proximal wrist crease and the radial pulse (see Fig. 188.2). The needle is inserted perpendicularly, just lateral to the radial pulse and 1 to 2 mm below the depth of the artery. Aspiration is performed and 3 to 5 mL of anesthetic agent is injected as the needle is slowly withdrawn. The subcutaneous branches are blocked with a superficial ringlike wheal, starting at the initial injection site and tracking to the dorsal midline (see Fig. 188.2).
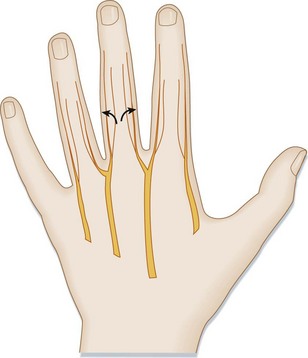
Digital Nerves
Each finger has two sets of nerves, called the dorsal and palmar digital nerves, that travel in the 2-, 4-, 8-, and 10-o’clock positions around the digit (Fig. 188.3). These four branch form two root nerves at the metacarpal-metatarsal heads. The most common approach for a digital nerve block is the proximal-most aspect of the finger or toe, where the nerves travel in the most consistent path. A skin wheal is formed on the dorsal surface of the finger or toe. The needle is then directed to the 2-, 4-, 8-, and 10-o’clock positions, respectively. After aspiration is performed, 0.5 to 1 mL of agent is injected at each site. Epinephrine and other vasoconstricting agents should not be used in this location because of the risk for critical ischemia.
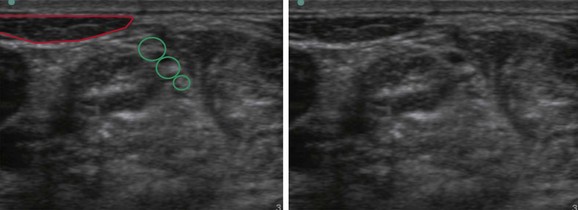
Interscalene Nerve
An ultrasound-guided interscalene nerve block is a useful method of inducing anesthesia for shoulder dislocations and is especially useful in patients who have a contraindication to procedural sedation or high opiate tolerance.10 Deep to the sternocleidomastoid muscle on the lateral anterior aspect of the neck is where the anterior and middle scalene muscles lie. The interscalene nerve bundle appears between the anterior and middle scalene muscles and has the appearance of three small round pealike structures (Fig. 188.4). Under direct visualization with ultrasound, 30 mL of 1% lidocaine should be injected adjacent to the nerve bundle. Use of a 20-gauge spinal needle is recommended because its noncutting nature may be less likely to result in nerve laceration. Of note, it is important to visualize the needle tip throughout the entire procedure to ensure proper positioning and avoid damage to surrounding structures. After approximately 10 to 30 minutes, shoulder anesthesia should allow painless reduction. Temporary paralysis of the hemidiaphragm will occur and is usually asymptomatic; however, this procedure would be contraindicated in anyone who cannot tolerate a 30% reduction in pulmonary function. Occasionally, the cervical sympathetic chain may be affected and result in hoarseness and Horner syndrome. Patients should be advised of these possibilities when consent is obtained for the procedure.
Bier Block
At the completion of the procedure and waiting period, the tourniquet should be deflated for 5 seconds and reinflated for 1 to 2 minutes; this cycle should be repeated three or four times to ensure slow release of the anesthetic into the systemic circulation. The patient should then be monitored for at least 30 minutes for signs of toxicity.1
Lower Extremity Blocks
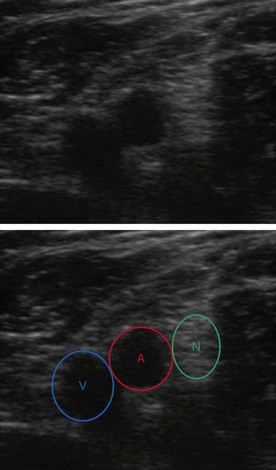
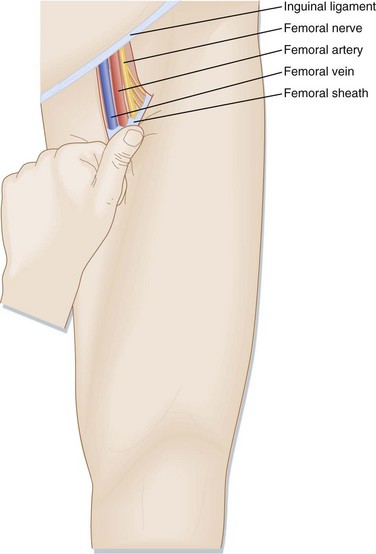
Femoral Nerve and Three-in-One Block
The femoral nerve block and the three-in-one block (femoral, obturator, and lateral femoral cutaneous nerves) are useful for patients with fractures of the femur or hip. In view of the proximity of the femoral artery and vein to the target nerve, careful palpation of the pulse and aspiration are crucial to the safety of this procedure. Ultrasound can greatly improve the safety and accuracy of this procedure and has been shown to reduce the need for opiate analgesia and the amount of anesthetic required11 (Fig. 188.5). The landmarks for this procedure are the inguinal ligament and the femoral artery (Fig. 188.6). The femoral artery is palpated 1 to 2 cm distal to the inguinal ligament. The operator’s nondominant hand is kept on the femoral pulse throughout the procedure to reduce the likelihood of intraarterial injection, especially if ultrasound is not being used to visualize the injection. With a perpendicular and slightly cephalad approach, the needle is inserted 0.5 to 1 cm lateral to the pulse until paresthesias are elicited, the patella moves involuntarily, or the needle begins to pulsate laterally. To anesthetize only the femoral nerve, 10 to 20 mL of agent should be injected. To anesthetize all three nerves, 30 mL of agent should be injected in a cephalad direction into the femoral sheath while distal pressure is maintained to ensure proximal tracking of the anesthetic agent.1,3,11,12
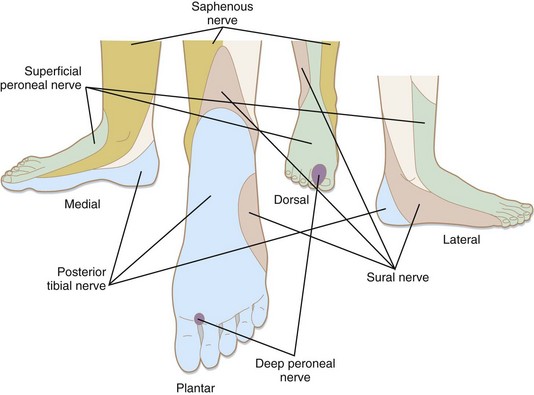
Sural Nerve
The sural nerve supplies sensation to the heel and lateral aspect of the foot (Fig. 188.7). Landmarks for this block are the lateral malleolus and the Achilles tendon (see Fig. 188.7). The needle is inserted just lateral to the Achilles tendon, 1 cm above the lateral malleolus, and directed toward the fibula. When contact with the fibula is made, the needle is withdrawn 1 mm, aspiration is performed, and 5 mL of agent is injected as the needle is withdrawn slowly.
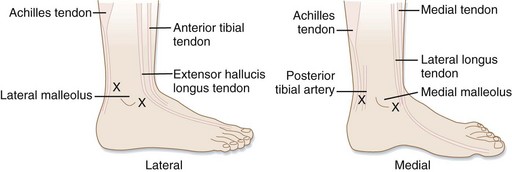
Peroneal Nerves (Superficial and Deep)
The superficial peroneal nerve supplies sensation to the dorsum of the foot and toes, whereas the deep peroneal nerve supplies the first web space (see Fig. 188.7). The landmarks for these blocks are the extensor hallucis longus tendon, the anterior tibialis tendon, and the anterior lip of the tibia (see Fig. 188.8). The superficial peroneal nerve travels anteriorly between the extensor hallucis longus tendon and the lateral malleolus. The deep peroneal nerve travels under the extensor hallucis longus tendon. For a superficial peroneal nerve block, the needle is inserted just lateral to the hallucis longus tendon and is directed toward the lateral malleolus. The agent is injected in a ringlike fashion from the extensor hallucis longus to the lateral malleolus. For a deep peroneal nerve block, the needle is inserted between the anterior tibialis tendon and the extensor hallucis longus tendon, 1 cm above the base of the medial malleolus, and directed 30 degrees laterally under the tendon. The needle is advanced until it touches the tibia (less than 1 cm) and then withdrawn 1 mm, and 5 mL of agent is injected while the needle is slowly withdrawn.
Saphenous Nerve
The saphenous nerve provides sensation to the medial aspect of the foot and the arch (see Fig. 188.7). The landmarks for this block are the medial malleolus and the anterior tibialis tendon (see Fig. 188.8). The patient is instructed to dorsiflex the foot to enable the anterior tibialis tendon to be located at the anterior lip of the tibia. The saphenous nerve travels superficially between the anterior tibialis tendon and the medial malleolus. The needle is inserted at the anterior lip of the distal end of the tibia, just lateral to the tibialis tendon, and directed toward the medial malleolus. Five milliliters of agent is injected subcutaneously, in a ringlike fashion, from the anterior tibialis tendon to the medial malleolus.
Posterior Tibial Nerve
The posterior tibial nerve supplies sensation to the distal two thirds of the plantar surface of the foot (see Fig. 188.7). The landmarks for this block are the medial malleolus, the posterior tibial artery, and the Achilles tendon (see Fig. 188.8). The needle is inserted just anterior to the Achilles tendon at a level 1 cm above the medial malleolus. The needle is directed just posterior to the posterior tibial artery toward the posterior aspect of the tibia. It is advanced until it hits the tibia and is then withdrawn 1 mm. Five milliliters of agent is then injected while the needle is slowly withdrawn.
Facial and Oral Blocks
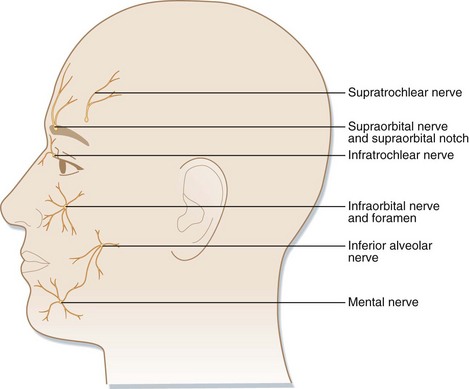
Supraorbital Nerve
The supraorbital nerve exits the supraorbital notch along the supraorbital rim. Along with the supratrochlear and infratrochlear nerves, it supplies sensation to the forehead (Figs. 188.9 and 188.10). For a nerve block, the supraorbital notch is palpated, and 1 to 3 mL of agent is injected at this location. If inadequate anesthesia is obtained, a subcutaneous wheal is made down the supraorbital rim with 5 mL of agent to anesthetize branches of the supratrochlear and infratrochlear nerves. Placing a finger just below the eyebrow decreases the incidence of eyelid swelling.2
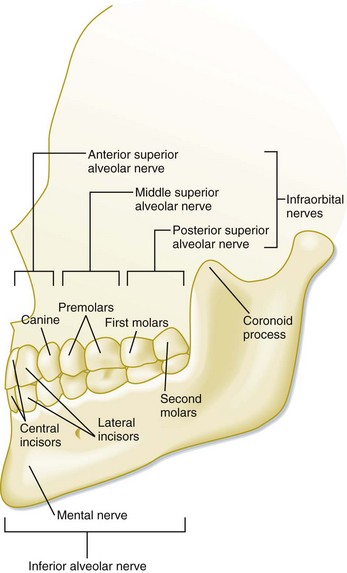
Infraorbital Nerve
The infraorbital nerve exits the infraorbital foramen and branches into the superior alveolar nerves supplying sensation to the midface region (see Figs. 188.9 and 188.10). The intraoral approach is recommended. While holding one finger externally over the inferior border of the infraorbital rim, the physician inserts the needle into the labial mucosa, opposite the apex of the first premolar. The needle is advanced parallel to the long axis of the tooth until it is palpated near the foramen. After aspiration, 2 to 3 mL of agent is injected slowly near but not into the foramen.
Anterior Superior Alveolar Nerve
The anterior superior alveolar nerve supplies sensation to the ipsilateral central and lateral incisors, as well as the canine tooth and half the upper lip (see Fig. 188.10). For block of this nerve, the needle is inserted with the bevel facing bone, superior to the apex of the canine, and directed to the canine fossa. After aspiration, 2 mL of agent is injected (see Fig. 188.10).
![]() Red Flags
Red Flags
Be wary of allergy to anesthetic agents; consider applying a preservative-free agent, crossing an anesthetic class, or using benzoyl alcohol.
Always aspirate before injecting to avoid accidental intravascular injection.
Perform a thorough neurologic evaluation before initiating local anesthesia.
Ask the patient to tell you whether paresthesias develop.
If paresthesias develop, withdraw the needle 1 to 2 mm before making the injection.
Monitor the patient closely for any signs of toxicity.
To reduce the incidence of toxicity, use the smallest effective dose of an anesthetic agent.
Tips and Tricks
Inject anesthetic agents slowly, in increments of no more than 3 mL, and aspirate before injecting.
Maintain verbal contact with the patient to help screen for dysarthria and changes in mental status.
Use a small needle (27- to 30-gauge for local infiltration, 25- or 27-gauge for nerve blocks).
Use warmed or buffered lidocaine.
Use a small-caliber syringe to reduce the pressure and pain associated with injection.
Administer 1 to 2 mL of anesthetic for digital blocks, 5 mL for most other blocks.
Posterior Superior Alveolar Nerve
The posterior superior alveolar nerve provides sensation to the ipsilateral maxillary molars (see Fig. 188.10). After the cheek is retracted laterally, the needle is inserted into the mucosal reflection, just distal to the distal buccal root of the upper second molar. The needle is advanced 2 to 2.5 cm along the curvature of the maxillary tuberosity, at which point 2 to 3 mL of agent is injected to effect a nerve block. The operator should beware of the pterygoid plexus and must be sure to perform aspiration before making an injection.
Middle Superior Alveolar Nerve
The middle superior alveolar nerve provides sensation to the ipsilateral premolars and sometimes the first maxillary molars (see Fig. 188.10). For a block of this nerve, the needle is inserted with the bevel facing bone, superior to the apex of the upper second premolar tooth, and 2 mL of agent is injected.
Inferior Alveolar Nerve
The inferior alveolar nerve supplies sensation to the ipsilateral mandibular teeth, lower lip, and chin (see Figs. 188.9 and 188.10). The coronoid process of the mandible is palpated, and the cheek is retracted laterally. A triangle is visualized in the mucosa posterior to the molars. The needle is inserted into this triangle, 1 cm above the occlusal surface of the molars, and advanced until it contacts the mandible. The needle is retracted slightly, aspiration is performed, and 2 mL of agent is injected slowly. If the needle does not contact the mandible and is directed posteriorly toward the parotid gland, temporary Bell palsy may be elicited if the facial nerve is unintentionally anesthetized. Injection of more agent while the needle is withdrawn will anesthetize the lingual nerve as well.
Mental Nerve
The mental nerve branches off the inferior alveolar nerve to supply sensation to the ipsilateral part of the chin (see Figs. 188.9 and 188.10). This nerve emerges from the mental foramen inferior to the second premolar (see Fig. 188.10). For a mental nerve block the foramen is palpated, and then through an intraoral approach, the needle is inserted in the mucobuccal fold and advanced until it can be palpated over the foramen. After aspiration is performed, 1 to 3 mL of agent is slowly injected.
Miscellaneous Nerve Blocks
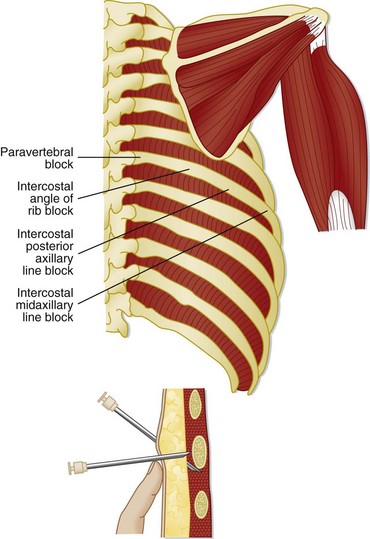
Intercostal Nerve Block
An intercostal nerve block is perhaps one of the most dangerous nerve blocks because of greater systemic absorption of agent injected in this area and a 1.4% incidence of pneumothorax.13 However, significant pain relief from rib fractures can be obtained with this method. In most cases, opiate analgesia is probably a safer method of pain control. The injured rib is palpated posterior to the posterior axillary line, and the skin is retracted superiorly over the rib. The needle is inserted 5 mm over the rib, the retracted skin released, and the needle walked gently down the inferior edge of the rib. The needle is then advanced 2 to 3 mm, aspiration is performed, and 2 to 5 mL of agent is injected. If pain control is inadequate, this procedure can be repeated for two ribs above and two below the injured area (Fig. 188.11).
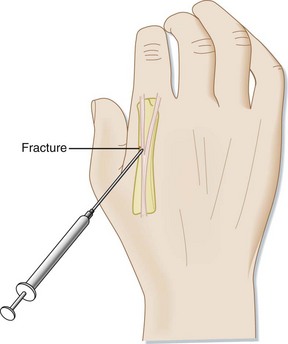
Hematoma Block
The hematoma of a fracture can be locally anesthetized to relieve the pain associated with relocation of a displaced fracture. This block is most commonly used for metacarpal fractures. Two milliliters of agent is usually sufficient. In this case, if aspiration of blood confirms placement of the needle within the hematoma, care should be taken to avoid anatomic locations of known vessels (Fig. 188.12).3
Christos S, Chiampas G, Offman R, et al. Ultrasound-guided three-in-one nerve block for femur fractures. West J Emerg Med. 2010;11:310–313.
Crystal C, Blankenship R. Local anesthetics and peripheral nerve blocks in the emergency department. Emerg Med Clin North Am. 2005;23:477–502.
Eidelman A, Weiss J, Lau J, et al. Topical anesthetics for dermal instrumentation: a systematic review of randomized, controlled trials. Ann Emerg Med. 2005;46:343–351.
Fletcher A, Rigby A, Heyes F. Three-in-one femoral nerve block as analgesia for fractured neck of femur in the emergency department: a randomized controlled trial. Ann Emerg Med. 2003;41:227–233.
Wedmore I, Johnson T, Czarnik J, et al. Pain management in the wilderness and operational setting. Emerg Med Clin North Am. 2005;23:585–601.
1 Crystal C, Blankenship R. Local anesthetics and peripheral nerve blocks in the emergency department. Emerg Med Clin North Am. 2005;23:477–502.
2 Salam G. Regional anesthesia for office procedures. Part 1: head and neck surgeries. Am Fam Physician. 2004;69:585–590.
3 Wedmore I, Johnson T, Czarnik J, et al. Pain management in the wilderness and operational setting. Emerg Med Clin North Am. 2005;23:585–601.
4 Waldbillig D, Quinn J, Steill I, et al. Randomized double-blind controlled trial comparing room-temperature and heated lidocaine for digital nerve block. Ann Emerg Med. 1995;26:677–681.
5 Brogan G, Giarrusso E, Hollander J, et al. Comparison of plain, warmed and buffered lidocaine for anesthesia of traumatic wounds. Ann Emerg Med. 1995;26:121–125.
6 Bartfield J, Jandreau S, Raccio-Robak N. Randomized trial of diphenhydramine versus benzoyl alcohol with epinephrine as an alternative to lidocaine local anesthesia. Ann Emerg Med. 1998;32:650–654.
7 Pollack C, Swindle G. Use of diphenhydramine for local anesthesia in “caine”-sensitive patients. J Emerg Med. 1989;7:611–614.
8 Zempsky W, Cravero JP, American Academy of Pediatrics Committee on Pediatric Emergency Medicine and Section on Anesthesiology and Pain Medicine. Relief of pain and anxiety in pediatric patients in emergency medical systems. Pediatrics. 2004;114:1348–1356.
9 Eidelman A, Weiss J, Lau J, et al. Topical anesthetics for dermal instrumentation: a systematic review of randomized, controlled trials. Ann Emerg Med. 2005;46:343–351.
10 Blavais M, Lyon M. Ultrasound-guided interscalene block for shoulder dislocation reduction in the ED. Am J Emerg Med. 2006;24:293–296.
11 Christos S, Chiampas G, Offman R, et al. Ultrasound-guided three-in-one nerve block for femur fractures. West J Emerg Med. 2010;11:310–313.
12 Fletcher A, Rigby A, Heyes F. Three-in-one femoral nerve block as analgesia for fractured neck of femur in the emergency department: a randomized controlled trial. Ann Emerg Med. 2003;41:227–233.
13 Shanti C, Carlin A, Tyburski G. Incidence of pneumothorax from intercostal nerve block for analgesia in rib fractures. J Trauma. 2001;51:536–539.