CHAPTER 29 Ligament Reconstruction/Sigmoid Notch Plasty for DRUJ Instability
The bony or ligamentous structures of the distal radioulnar joint (DRUJ) are often disrupted in association with a distal radius fracture, which is the most common cause for DRUJ instability. In some studies, up to 10% of patients with distal radius fractures had a DRUJ injury necessitating primary operative repair.1 In addition, arthroscopy at the time of fracture identified the presence of triangular fibrocartilage complex (TFCC) injury in 43 of 51 patients examined by Lindau and colleagues.2 The TFCC lesions were associated with DRUJ instability in 17 patients. Younger patients and those sustaining high-energy injuries are more likely to have DRUJ injuries in association with distal radius fractures.2
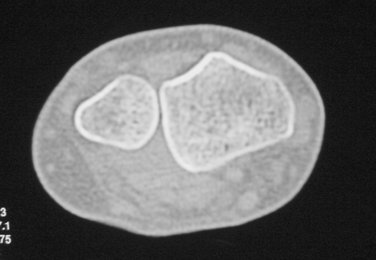
Failure to recognize and treat DRUJ disruption can contribute to a poor outcome. In particular, residual DRUJ instability after distal radius fracture is associated with worse objective and subjective outcome measures.3 When treated acutely by either closed reduction or soft tissue or bony repair, most patients will not develop DRUJ instability. However, some patients with distal radius fractures will go on to develop chronic DRUJ instability owing to failure of the soft tissues to heal or to malunion of the radius or ulna (Fig. 29-1). Multiple techniques have been described to restore stability to the chronically unstable DRUJ. These techniques can be divided into three categories: (1) a direct radioulnar tether that is extrinsic to the joint, (2) an indirect radioulnar link through an ulnocarpal sling or tenodesis, or (3) reconstruction of the distal radioulnar ligaments.

FIGURE 29-1 Chronic DRUJ instability after a distal radius fracture. Arrow points to the prominent ulnar head on the affected side.
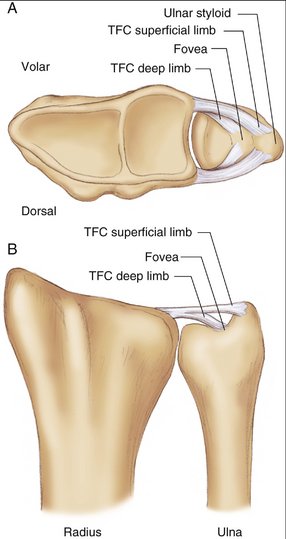
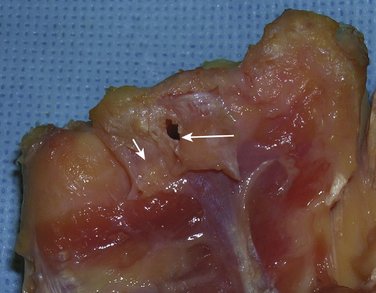
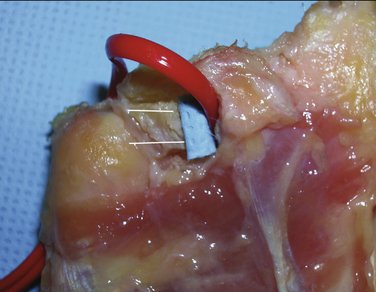
Multiple biomechanical studies have shown that the dorsal and palmar radioulnar ligaments are key stabilizers of the DRUJ.4,5 The radioulnar ligaments are condensations of fibers at the combined junctures of the triangular fibrocartilage articular disc, DRUJ capsule, and ulnocarpal capsule. As they pass toward the ulna, each ligament divides into superficial and deep fibers (Fig. 29-2). The superficial fibers insert on the ulnar styloid near its midportion. Disruption of the superficial fibers in the absence of other injury does not result in DRUJ instability. The deep radioulnar ligament fibers insert into the fovea on the ulnar head, which is a bony depression between the base of the styloid and the articular cartilage on the dome of the ulnar head. Disruption of these fibers can result in DRUJ instability.
Because of the importance of the dorsal and palmar radioulnar ligaments for DRUJ stability, reconstruction of these ligaments offers the best anatomical restoration of joint stability. The technique described in this chapter uses a tendon graft that nearly mimics the native ligaments. The two limbs of the tendon graft pass from the volar and dorsal margins of the sigmoid notch and converge to insert on the ulnar head at the fovea (Fig. 29-3). A recent biomechanical study by Gofton and coworkers6 found that this radioulnar ligament reconstruction nearly restored the kinematics of the unstable DRUJ, and it provided better joint stability than the nonanatomical reconstruction described by Fulkerson-Watson, which has been shown to provide the best stability among the radioulnar tether methods.
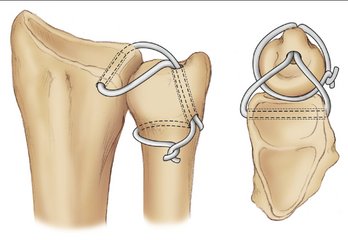
FIGURE 29-3 Final graft placement mimics the native insertion sites of the distal radioulnar ligaments.
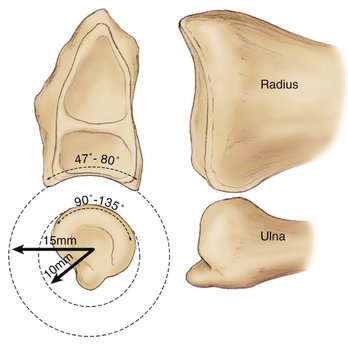
Reconstruction of the soft tissue DRUJ restraints, however, will be insufficient in the presence of a substantial osseous abnormality. The articular surfaces of the DRUJ are not congruent in the normal wrist. The sigmoid notch has a radius of curvature that is much larger than that of the ulnar head (Fig. 29-4). It is a combination of ligament tension and joint compression between the ulnar head and rims of the notch that provides joint stability. The dorsal and particularly the volar rims of the notch often have fibrocartilaginous extensions or labrums that augment its relatively flat surface, which improves joint congruency and capture and thus substantially increases DRUJ stability.7 A developmentally flat notch or one that is deficient from injury poses greater risks to develop DRUJ instability and for the failure of a ligament reconstruction (Fig. 29-5). Sigmoid notch osteoplasty increases the prominence of the rim and improves joint stability.
Extra-articular deformity of the radius alone is sufficient to substantially impair DRUJ function. In cadaver studies, dorsal angulation of the distal radius or loss of radial inclination alters DRUJ mechanics and reduces forearm rotation.8,9 Corrective osteotomy of the radius can be performed in conjunction with a radioulnar ligament reconstruction.
Indications
Computed tomography (CT) should be performed if there is any question regarding the competency of the sigmoid notch or the presence of arthritis. CT is performed on both wrists in equivalent neutral, pronation, and supination positions. The comparison between sides will help assess direction of instability and if the shape of the notch has been altered by injury. If the notch is developmentally flat or a rim has been traumatically damaged, a sigmoid notch osteoplasty at the time of ligamentous reconstruction may be necessary.
Surgical Technique
The patient is positioned supine with the operative arm extended on a hand table. An upper arm tourniquet is applied. A 4-cm longitudinal skin incision is made over the interval between the fifth and sixth extensor compartments. The fifth compartment is entered, and the extensor digiti minimi is retracted. The DRUJ is identified by palpation. An L-shaped capsulotomy is made overlying the DRUJ. Its longitudinal limb extends along the dorsal rim of the sigmoid notch, stopping just short of the radiocarpal joint to preserve any remnant of the dorsal radioulnar ligament. The transverse limb extends ulnarward from the sigmoid notch, just proximal and parallel to the normal location of the dorsal radioulnar ligament (Fig. 29-6).

FIGURE 29-6 An L-shaped capsulotomy allows visualization of the sigmoid notch (arrow) and ulnar head.
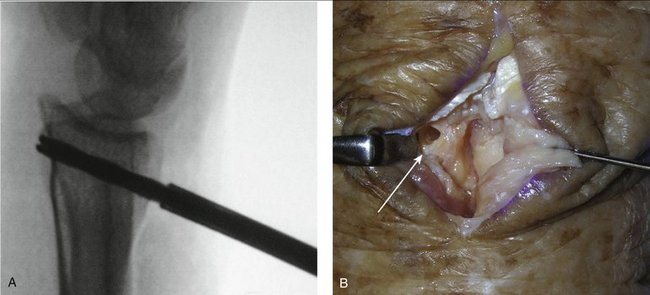
The periosteum is elevated from the dorsal distal radius adjacent to the sigmoid notch. A small back-cut along the dorsal rim of the distal radius may be necessary to provide sufficient elevation and retraction of the fourth extensor compartment. A guidewire for a 3.5-mm cannulated drill is driven from dorsal to volar through the distal radius several millimeters from the articular surfaces of the lunate fossa and sigmoid notch. The distance between the guidewire and the articular surfaces must be sufficient to allow a drill hole of sufficient size that will accommodate the graft. Guidewire position is confirmed with fluoroscopy. The cannulated drill is used over the guidewire with care not to drive the guidewire into the volar tissues. If necessary, the hole is enlarged with standard drill bits (Fig. 29-7).
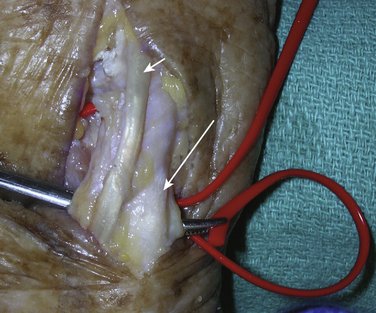
The distal ulna tunnel extends between the fovea and the subcutaneous border of the ulnar neck just volar to the extensor carpi ulnaris tendon. If sufficient exposure cannot be obtained by flexing the wrist and retracting the TFCC remnant, the guidewire is inserted through the fovea to exit the ulnar neck. Alternatively, in patients with stiff wrist flexion or a large wrist, the guidewire can be passed more easily in the opposite direction, that is, from the ulnar neck to the fovea. Using this latter method, a 4- to 5-mm drill hole is first made in the ulnar neck at its subcutaneous border. A guidewire is inserted in the hole and driven through the fovea. Regardless of the direction of guidewire placement, the cannulated drill should be passed from proximal (ulnar neck) to distal (fovea) to prevent damage to the carpus. One should begin with a 3.5-mm cannulated drill bit and if necessary enlarge the tunnel with standard drill bits to accommodate both limbs of the graft (Fig. 29-8).
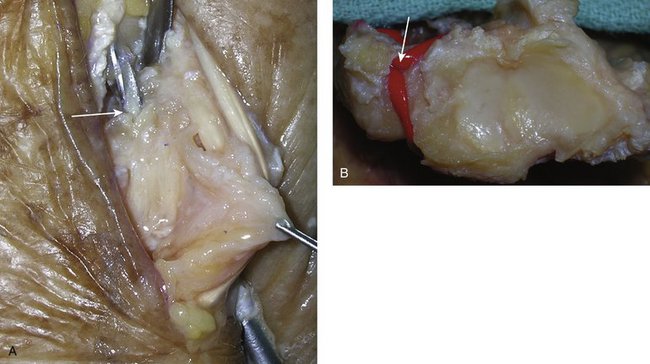
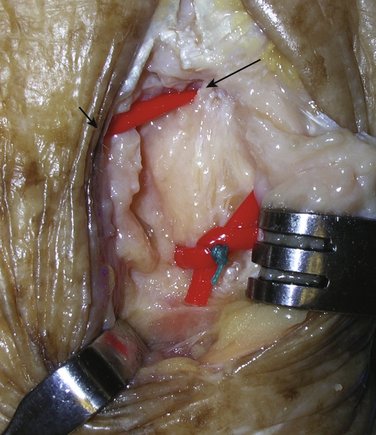
The volar opening of the radius tunnel is exposed through a 3- to 4-cm longitudinal incision extending proximally from the proximal wrist crease between the ulnar neurovascular bundle and finger flexor tendons. Careful dissection between the ulnar neurovascular bundle and finger flexors reveals the pronator quadratus and distal portion of the volar DRUJ capsule. A suture retriever is passed through to the radius tunnel from dorsal to volar. The retriever is used to pull one end of the graft from volar to dorsal through the radius. From dorsal to volar, a straight hemostat is passed just distal to the ulnar head and proximal to the residual TFCC. The volar DRUJ capsule is punctured, and the volar limb of the graft is grasped and pulled back into the dorsal wrist wound (Fig. 29-9). One should be careful not to entrap any nervous, vascular, or tendinous structures in the graft loop. Both ends of the tendon graft should now lie in the dorsal wrist exposure (Fig. 29-10).

FIGURE 29-9 Suture passer is seen to the right in this image, while the tip of the hemostat is to the left. Hemostat grasps one end of the graft (long arrow) while the other graft end is placed in the suture retriever loop (short arrow). (A red vessel loop has been used instead of tendon graft in this cadaver specimen for illustrative purposes.)
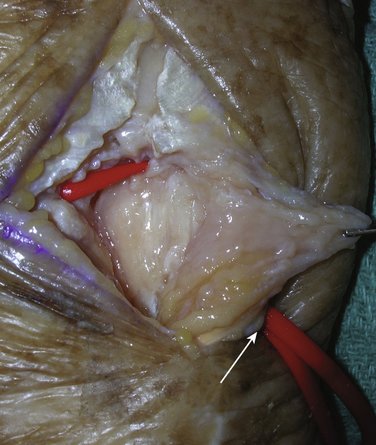
The suture retriever is passed through the distal ulna tunnel from the neck to fovea, exiting in the dorsal wound. Both limbs of the tendon graft are pulled back through the ulna to exit at the ulnar neck (Fig. 29-11). A hemostat is passed ulnarward under the extensor carpi ulnaris sheath at the ulnar neck and used to pull one limb of the graft toward the radius (Fig. 29-12). From the dorsal exposure, a right-angled clamp is passed volarly around the ulnar neck to grasp the second graft limb and pull it back around the neck. Both limbs of the tendon graft should now be resting on the dorsal ulnar neck (Fig. 29-13).
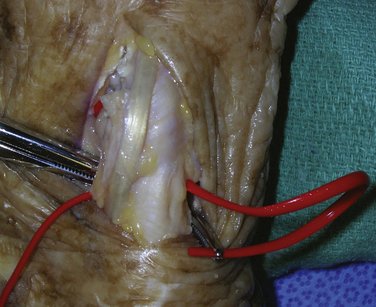
FIGURE 29-13 A right-angled clamp passes around the volar ulnar neck to retrieve the other end of the tendon graft.
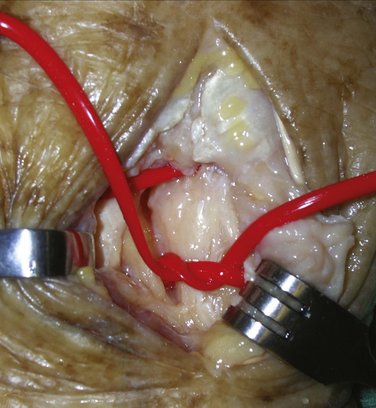
The two graft limbs are pulled taut and tied in a half-hitch while the forearm is held in neutral rotation and manual pressure is applied to compress the DRUJ (Fig. 29-14). The half-hitch is secured with 3-0 nonabsorbable sutures (Fig. 29-15). The dorsal DRUJ capsule and the extensor retinaculum are closed in a single layer, with care to avoid the extensor tendons (see Fig. 29-20). The extensor digiti minimi tendon is left superficial over the DRUJ. A temporary large-diameter Kitschner wire (K-wire) may be placed across the DRUJ if desired but I very rarely do this.
The patient is then converted to a removable wrist brace to be used for an additional 2 more months as motion and strength are recovered. Therapy begins with active and gentle passive wrist flexion, extension, pronation, and supination. No limitations are placed on active motion, but only gentle passive motion should be used during the first month of therapy. Strengthening is started early, but high forces with the arm in full pronation and supination are avoided. At 4 months after the surgical procedure, more aggressive passive range of motion and strengthening exercises are added. No use of the hand for sports or other stressful activities is allowed until at least the fourth month after surgery.
If the sigmoid notch is flat or deformed, then an osteoplasty may be performed at the same setting as the DRUJ ligament reconstruction. Sigmoid notch osteoplasty augments the volar or dorsal rim of the sigmoid notch to increase DRUJ stability. Wallwork and Bain10 originally described the sigmoid notch osteoplasty for the volar rim, but the same technique may also be used to augment the dorsal rim.
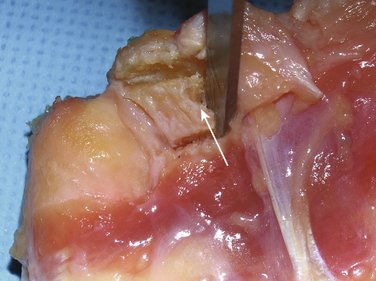
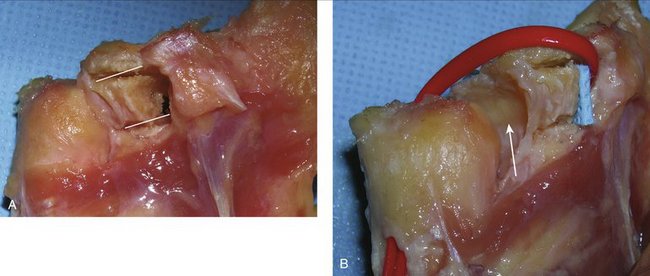
The osteoplasty may be performed through the same volar or dorsal approach used for DRUJ ligament reconstruction. For the volar side, the periosteum is incised and raised 3 to 4 mm radial to the rim of the sigmoid notch (see Fig. 29-16). For the dorsal side, the previously incised capsule is raised in continuity with the adjacent periosteum. With the use of a small osteotome, a transverse cut about 4 mm deep is made in the rim of the notch at its proximal edge (Fig. 29-17). A second parallel osteotomy is made 2 to 3 mm proximal to the radiocarpal joint. A longitudinal cut about 4 mm from the margin of the rim connects the two transverse limbs. If a simultaneous ligament reconstruction is part of the surgical plan, the radial drill hole is made first. The longitudinal limb of the osteotomy passes through the ulnar margin of the radial drill hole (Fig. 29-18). The osteotome is slowly advanced to the depth of the longitudinal cut (one-fourth to one-third the width of the radius) and used to gently lever the rim a few millimeters toward the ulna. The articular cartilage and subchondral bone are bent but not broken through. The gap is filled with bone graft harvested from the nearby distal radius (Fig. 29-19). The tendon graft should be passed through the distal radius drill hole but not tensioned before bone graft placement. Because the tendon graft will pass directly over the bone graft when tensioned in its final position, it will typically secure the bone graft, but sutures through the nearby periosteum can be added (Fig. 29-20).
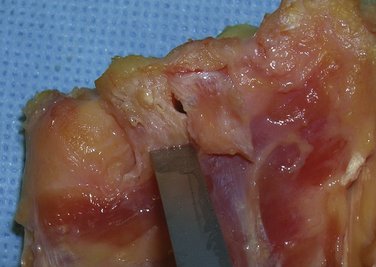
FIGURE 29-17 A small osteotome is used to make the proximal cut of the osteoplasty at the proximal margin of the sigmoid notch.
Results
The majority of patients treated with DRUJ ligament reconstruction will maintain near-full forearm rotation and have restored DRUJ stability and improved grip strength. This procedure successfully restored stability in 12 of 14 patients in Adams and Berger’s original series,11 and 9 of 14 patients had complete relief of pain at minimum 1 year follow-up. Patients averaged 72 degrees of pronation and 70 degrees of supination. One of the patients with recurrent instability was later noted to have a deficient sigmoid notch volar rim, whereas the other had only ulnocarpal residual instability. A later follow-up with an additional 8 patients showed maintained stability in the first 12 successful procedures and good stability in the additional 8 patients.
Teoh and Yam reported similar results in their series of 9 patients treated with a slight variation of this technique. Seven of 9 patients had restored DRUJ stability and regained 90% of forearm rotation when compared with the normal side.12
1. Geissler WB, Fernandez DL, Lamey DM. Distal radioulnar joint injuries associated with fractures of the distal radius. Clin Orthop Relat Res.. 1996;327:135-146.
2. Lindau T, Adlercreutz C, Aspenberg P. Peripheral tears of the triangular fibrocartilage complex cause distal radioulnar joint instability after distal radial fractures. J Hand Surg [Am].. 2000;25:464-468.
3. Lindau T, Hagberg L, Adlercreutz C, et al. Distal radioulnar instability is an independent worsening factor in distal radial fractures. Clin Orthop Relat Res. 2000;376:229-235.
4. Kihari H, Short WH, Werner FW, et al. The stabilizing mechanism of the distal radioulnar joint during pronation and supination. J Hand Surg [Am].. 1995;20:930-936.
5. Ward LD, Ambrose CG, Masson MV, Levaro F. The role of the distal radioulnar ligaments, interosseous membrane, and joint capsule in distal radioulnar joint stability. J Hand Surg [Am].. 2000;25:341-351.
6. Gofton WT, Gordon KD, Dunning CE, et al. Comparison of distal radioulnar joint reconstructions using an active joint motion simulator. J Hand Surg [Am].. 2005;30:733-742.
7. Tolat AR, Stanley JK, Trail IA. A cadaveric study of the anatomy and stability of the distal radioulnar joint in the coronal and transverse planes. J Hand Surg [Br].. 1996;21:587-594.
8. Adams BD. Effects of radial deformity on distal radioulnar joint mechanics. J Hand Surg [Am].. 1993;18:492-498.
9. Kihari H, Palmer AK, Werner FW, et al. The effect of dorsally angulated distal radius fractures on distal radioulnar joint congruency and forearm rotation. J Hand Surg [Am].. 1996;21:40-47.
10. Wallwork NA, Bain GI. Sigmoid notch osteoplasty for chronic volar instability of the distal radioulnar joint: a case report. J Hand Surg [Am].. 2001;26:454-459.
11. Adams BD, Berger RA. An anatomic reconstruction of the distal radioulnar ligaments for posttraumatic distal radioulnar joint instability. J Hand Surg [Am].. 2002;27:243-251.
12. Teoh LC, Yam AKT. Anatomic reconstruction of the distal radioulnar ligaments: long-term results. J Hand Surg [Br]. 2005;30:185-193.