Nerve lesions and entrapment neuropathies of the upper limb
Disorders of the spinal accessory nerve
Disorders of the brachial plexus
Disorders of the long thoracic nerve
Disorders of the suprascapular nerve
Disorders of the axillary nerve
Lesions at the proximal and middle part of the upper arm
Lesions at the distal part of the upper arm
Peripheral nerve lesions in the neck, shoulder girdle and upper limb can occur anywhere along the extraspinal extent of the nerve – between the intervertebral foramen and the most distal nerve endings in the extremities. The function of the nerve becomes impaired either as the result of an entrapment phenomenon, or as the outcome of an injury causing bruising or elongation of the nerve tissue.
Entrapment phenomena occur typically at four different sites giving rise to four different mechanisms (see Chapter 2):
• Pressure on a distal nerve causes mainly analgesia as well as some paraesthesia in the territory of the nerve.
• When a nerve trunk or plexus becomes compressed, the release phenomenon – paraesthesia when the pressure ceases – is found.
• Nerve root compression is characterized by pain and paraesthesia, felt in the corresponding dermatome, and often followed by sensory and motor deficit in the same segment.
• Pressure on the cervical spinal cord is painless. An early symptom is paraesthesia with multisegmental distribution. When the compression becomes more severe, numbness, incoordination, spasticity and hyperreflexia may occur.
Disorders of the spinal cord and nerve roots are discussed in Chapters 2 and 8.
Disorders of the spinal accessory nerve
Anatomy
The accessory nerve is a cranial nerve (XI) and consists of two parts. Its main part is the spinal root; the other is the cranial root.
The spinal root takes origin in the spinal cord from a small pillar of nuclei in the anterolateral part of the anterior horn of the levels C1–C5/C6. The fibres leave the cord between the anterior and posterior rami of the nerve root. They join and form a strand that ascends parallel to the spinal cord and enters the skull through the foramen magnum.
The cranial root takes its origin in the caudal part of the nucleus ambiguus in the medulla oblongata.
Both parts accompany the glossopharyngeal (IX) and vagus (X) nerves in their exit through the jugular foramen. The fibres originating from the nucleus ambiguus then join the vagus nerve and the other fibres – the real spinal accessory nerve – descend towards the muscles they innervate (Fig. 1).
Innervation
The spinal accessory nerve is a pure motor nerve and innervates the sternocleidomastoid and the trapezius muscles (Fig. 2).
Disorders
A lesion of the spinal accessory nerve may be either idiopathic or result from a compression along its course. Idiopathic spinal accessory neuropathy may occur in isolation or in combination with a disorder of other nerves (glossopharyngeal, vagus, long thoracic or dorsal scapular).1
Mechanical lesions of the spinal accessory nerve can occur at different levels:
• Within the skull where the cause is usually tumourous.2,3 This is uncommon.
• At the level of the exit through the jugular foramen where again, rarely, metastases or schwannomas may affect the nerve.4,5
• At the level of the neck where iatrogenic trauma, for example biopsy of lymph nodes in the posterior triangle, forms the commonest cause of isolated paralysis.6–12 Injury rates from these procedures are reportedly 3–8%.13,14 External traumas may also damage the nerve.
Mononeuropathy of the spinal accessory nerve
The patient initially complains of intermittent pain in the shoulder girdle area, which soon may become permanent.15,16 At the same time, the arm starts to feel weak and heavy, which leads to some functional loss.17 Exceptionally, pain is absent. Pain normally lasts for about 3 weeks, after which it disappears spontaneously.
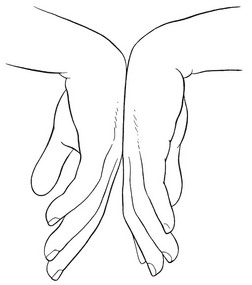
Inspection elicits an asymmetrical neckline with drooping of the effected shoulder. This may be accompanied with lateral displacement and winging of the scapula.18 Typically, winging is minimal and is accentuated during arm elevation, with the scapula moving upwards with the superior angle more lateral to the midline than the inferior angle. Limitation of active elevation of the arm is a consistent finding, and in one series of patients, the majority could only elevate to 80–90°.19 Passive neck, scapular and arm movements do not influence the pain. Resisted elevation of the shoulder girdle is weak. Resisted external rotation of the arm makes the scapula more prominent medially.20 In severe cases the trapezius muscle may be wasted. The diagnosis is confirmed by asking the patient to adduct both scapulae while the therapist applies counterpressure at the medial border of the inferior scapular angle (Fig. 3). In neuritis of the accessory nerve, the scapula on the affected side can easily be pushed away at the side.
Spontaneous cure of motor function of the trapezius is the rule and usually takes about 4–8 months.21,22 If inadequate functional recovery is seen after a year, additional conservative treatment is unlikely to be beneficial and surgery is indicated. In a recent review of the literature, authors have reported good or excellent results in approximately two-thirds of patients treated with nerve surgery.23
Disorders of the brachial plexus
Anatomy
The ventral rami of the spinal nerves C5, C6, C7, C8 and T1 unite to form the brachial plexus. Occasionally a prefixed (C4) or postfixed (T2) ramus takes part in the formation of the plexus. Several interconnections lead to the formation of trunks, divisions, cords and branches.
Trunks
There are three trunks: superior, middle and inferior. The superior trunk is created by the fusion of the ventral rami of C5 and C6. The middle trunk is the continuation of the ventral ramus of C7. The inferior trunk is formed by the ventral rami of C8 and T1.
Divisions
The three trunks divide into an anterior and a posterior part. The posterior parts form the posterior cord. The anterior parts form the other cords: the superior trunk continues in the lateral cord and the inferior trunk in the medial cord. The superior and inferior trunks also give off branches for the middle trunk, thus forming interconnections.
Cords
The cords are lateral, posterior and medial according to their relation to the subclavian/axillary artery. The lateral cord is formed from fibres of the superior trunk, together with fibres from the middle trunk. The posterior cord results from the fusion of fibres originating from the three trunks. The medial cord is the continuation of the inferior trunk.
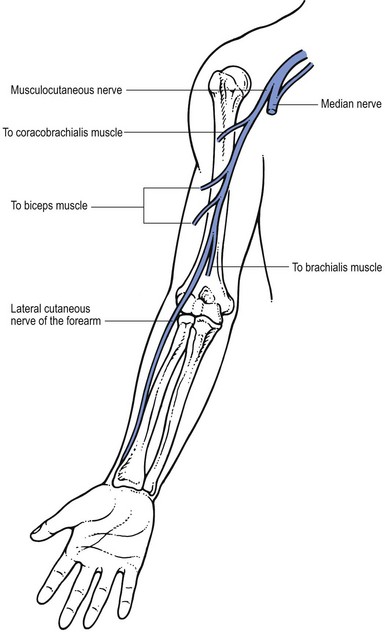
Peripheral nerve
From the three cords the major peripheral nerves of the upper limb are formed. The lateral cord continues into the musculocutaneous nerve. The posterior cord forms a branch that divides into two separate nerves: the radial nerve and the axillary nerve. The medial cord forms the ulnar nerve. From an anastomosis between the lateral cord and the medial cord the median nerve is formed.
Several other nerves emerge directly from the brachial plexus, either from its supraclavicular or its infraclavicular part.
From the supraclavicular part of the plexus originate: the dorsal scapular nerve (innervating the levator scapulae, major rhomboid and minor rhomboid muscles); the long thoracic nerve (innervating the serratus anterior muscle); the thoracodorsal nerve (innervating the latissimus dorsi muscle); the suprascapular nerve (innervating the supraspinatus and infraspinatus muscles); the inferior subscapular nerve (innervating the teres major muscle); the subclavian nerve (innervating the subclavian muscle); the lateral pectoral nerve (innervating the upper part of the pectoralis major muscle); and the medial pectoral nerve (innervating the lower part of the pectoralis major muscle as well as the pectoralis minor muscle).
From the infraclavicular part of the plexus the following nerves originate: the medial cutaneous nerve of the arm (supplying the anteromedial and posteromedial part of the arm); and the medial cutaneous nerve of the forearm (its anterior ramus supplying the anteromedial aspect of the forearm, and its cubital ramus supplying the posteromedial aspect of the forearm) branches of the medial cord of the brachial plexus (Fig. 4).
Traumatic disorders
The brachial plexus lies quite superficially within a very mobile shoulder girdle and is closely related to the different bony structures of neck, shoulder girdle, shoulder and thorax. This situation makes it very vulnerable. Traumatic disorders are therefore one of the commonest causes of brachial plexus dysfunction. As the result of traction injuries (e.g. motorcycle accidents), compression by dislocated (e.g. shoulder luxation24,25) or fractured bones (e.g. fracture of the clavicle26) or by haematomas, and intraoperative or birth injuries, larger or smaller parts of the plexus may become damaged, leading to total or partial syndromes.27
Upper brachial plexus palsy
This is called Erb–Duchenne’s paralysis and is defined as a palsy of C5 and C6 and sometimes of C7. There is a motor deficit of the muscles innervated by the nerves originating from these fibres and possibly a sensory deficit in the C5 and C6 dermatomes (lateral and anterior aspects of arm and forearm and radial aspect of hand and fingers) (Table 1).
Table 1
Affected nerves and muscles in a palsy of the upper part of the brachial plexus
| Nerve | Muscle |
| Long thoracic | Serratus anterior |
| Dorsal scapular | Rhomboids |
| Suprascapular | Supraspinatus |
| Infraspinatus | |
| Axillary | Deltoid |
| Teres minor | |
| Musculocutaneous | Coracobrachialis |
| Biceps | |
| Radial | Brachioradialis |
| Supinator |
The patient cannot bring the arm up and has difficulty in bending the elbow; there is a visible atrophy of the deltoid, supraspinatus and infraspinatus muscles.
Middle brachial plexus palsy
If the middle part of the brachial plexus becomes damaged by trauma, the serratus anterior and rhomboid muscles remain unaffected. There is slight weakness of the deltoid and supraspinatus muscles, which results in the patient not being able to elevate the arm above the horizontal. Elbow flexion is weak because of paresis of the biceps muscle. Sensation remains normal.
Lower brachial plexus palsy
This is known as Dejerine–Klumpke paralysis and is not so common but it causes severe disability. The lesion affects the C8 and T1 segments, and quite often also C7. As a result, there is a palsy of the muscles supplied by the ulnar and median nerves as well as the finger extensors and the extensor carpi ulnaris muscle (radial nerve). A complete inability to use the hand follows. There is also sensory deficit in the C8 segment (ulnar aspect of hand and distal forearm).
Space-occupying lesions
Metastatic tumours – usually originating from the breast, the lung or the lymphatic system – may invade the brachial plexus.
The superior pulmonary sulcus tumour (Pancoast) typically invades the lower trunk of the plexus as well as the sympathetic ganglia at the base of the neck.28 A lower brachial plexus dysfunction is then accompanied by Horner’s syndrome (see p. 3 of online chapter Disorders of the thoracic cage and abdomen).
Aneurysm of the subclavian artery and pseudoaneurysm of the axillary artery are other possible causes of compression of the brachial plexus.
Thoracic outlet syndrome
Thoracic outlet syndrome (TOS) is a vague term, only suggesting the presence of a disorder within the area of the thoracic outlet. Although it is generally accepted that the aetiology is compression of the plexus and vascular bundle in the thoracic outlet, different opinions exist about the pathogenesis. This is expressed in the various names that have been given to the syndrome (see Box 1).29 The consequence of disagreement on the aetiology is that numerous methods of treatment are advocated.
Anatomy
The thoracic outlet is the space bounded by the upper part of the sternum, clavicle, first rib and the first thoracic vertebra.30 Towards the centre, it is limited by the trachea and oesophagus. It forms the communicating area at the base of the neck for the passage of blood vessels and nerves from mediastinum and neck to the axilla and into which the dome of the pleura rises upward.31 The vagus, phrenic nerves, sympathetic trunk and thoracic duct also pass through the same openings.
The first rib has a flat upper surface. In its anterior portion there are two grooves, which are separated by the tubercle at which the anterior scalene muscle inserts. The more medial groove accommodates the subclavian vein. Behind the muscle, in the posterior groove, both subclavian artery and brachial plexus are found (Fig. 5).
The clavicle overlies the first rib just cranial to the posterior groove. At this site, compression of the neurovascular structures between first rib and clavicle is possible; this mainly happens to the most medially localized trunks, which contain fibres of C8 and T1, so causing symptoms in the territory of the median and the ulnar nerve.
Types
According to Cyriax, the syndrome is the outcome of a compression of the most medial branches of the brachial plexus, usually occurring between the clavicle and first rib, seldom as the result of a cervical rib. The compression is usually bilateral, intermittent or continuous and may or may not involve the subclavian artery and vein.32 It gives rise to a set of neurovascular symptoms, which are rarely present all together. Symptoms of neurological disturbances are usually found but sometimes only features of vascular compression.33 The brachial plexus is involved in 98% of cases, the subclavian vein in 1.5%, and the artery in 0.5%.34,35
Cyriax recognized two main groups of thoracic outlet syndromes based on anatomical and clinical grounds: the cervical rib syndrome and the first rib syndrome. We prefer to substitute for these terms. We make a distinction between the thoracic outlet syndrome caused by anatomical changes and that from postural factors. This approaches the growing agreement about the use of four terms to indicate the presence of the thoracic outlet syndrome;36,37 true neurologic, arterial and venous TOS – those syndromes that result from compression by a cervical rib (anatomical variety); and non-specific neurologic TOS38,39 – the postural variety.
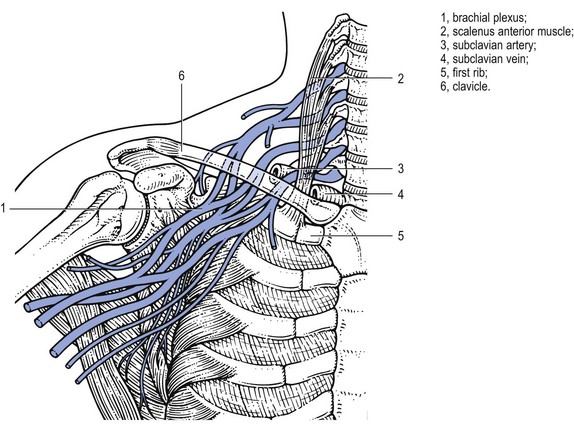
Fig 5 A slightly schematic representation of the relationship of neurovascular structures in the thoracic outlet.
Anatomical variety
This is caused by structural changes – the presence of a bony cervical rib or a band of fibrous tissue which is found in 0.5% of a normal population. Only 5% of them will ever suffer from a thoracic outlet syndrome.40 In a fibrous band, the corresponding transverse process of C7 is larger than usual – a rudimentary cervical rib. A cervical rib sometimes gives rise to a palpable mass at the base of the neck.
Interference with the neurovascular structures usually begins at between 20 and 30 years of age and is thereafter continuous. Structural change and clinical features are frequently bilateral, although often more pronounced at one side.41 The symptoms are the result of compression of both neurological and vascular structures.
Neurocompression
Compression of a nerve trunk can give rise to pain felt at the base of the neck, radiating unilaterally towards the shoulder and arm and even towards the chest. The pain is not very severe and is often associated with pins and needles and numbness, which may be felt in all five digits, although most frequently the fourth and fifth fingers are affected together with the ulnar side of the arm and hand.
The symptoms often appear or increase shortly after having carried a heavy object, but exceptionally they can occur during the activity itself. Some patients complain of disturbed fine motor coordination together with weakness and dysfunction of the hand.
On clinical examination, atrophy of the hypothenar (T1) or of the thenar muscles (C8), together with weakness of the interossei (T1), can be present.
Once a cervical rib has started to interfere with a nerve, the compression does not resolve. Therefore, the symptoms are continuously present and tend to increase.
Vascular compression
The compression can be venous and/or arterial.
Compression of the subclavian artery (Fig. 6) results in coldness, pallor and easy tiredness of the hand.42 Especially after the arm has been hanging down for a while, the hand may turn white and cold over a period of hours. A diminished pulse may be found.
In more severe cases, chronic compressive stenosis of the artery may give rise to claudication of the upper extremity. It may further lead to a poststenotic dilation, sometimes to the formation of an aneurysm. Atheromata arising from these aneurysms or from chronic compression injury of the artery can result in peripheral embolization, which may lead to irreversible damage to the hand and even to the entire arm.34,43–45
The presence of an acute ischaemic syndrome of the upper extremity, usually in a young female, suggests the possibility of a thrombosis in a poststenotic aneurysm.
Postural variety
This category comprises cases that have an almost identical clinical pattern but in which there is no cervical rib or fibrous band. It is characterized by neurological symptoms typically present after lying down for, say, 2–3 hours. It is a benign disorder seldom resulting in vascular disturbance or in muscular atrophy.
There are two types, depending on the clinical features.
Acute onset
This is unusual, but the diagnosis is important although difficult to make. Frequently the patient is admitted to the hospital suspected of having had a heart attack.49
Young patients with acute onset of symptoms after carrying a heavy load are typical. They complain of a sudden and severe thoracic pain, radiating down the arm, feel faint and have pain on breathing. All such features draw attention to serious visceral disorders (heart attack, pneumothorax). A short time later, the arm and hand blanche. This situation resolves after a few hours, so that by the time investigations, such as electrocardiography, radiography of the thorax and possibly laboratory tests, have been done, the symptoms have disappeared and the patient is perfectly normal again.
Slow onset
This is the more common type. It is very slow in progression and has a benign evolution, seldom giving rise to neurological deficit. The diagnosis is often missed, although not difficult to establish.
It affects the middle aged or elderly, more frequently females. It sometimes occurs in pregnancy. The onset is with pins and needles in the hand and fingers, mainly at night and usually after 2–3 hours of sleep. The process is often bilateral, although worse on one side. Paraesthesia may be felt in all digits but may predominate in the median or ulnar distribution. It wakes the patient, who finds that she has to sit up or walk around for a short period of time, rubbing and moving the hands and fingers, to make the symptoms go. The symptoms disappear after a few minutes, allowing sleep to be continued, although recurrence may take place in the early morning hours. The more physical activity during the preceding day, the worse the symptoms at night.50 In periods of rest or sickness, when the patient lies down for the whole day, no pins and needles are felt. Some patients also experience symptoms during the day, on activities such as knitting, holding a newspaper in front of the eyes or bicycling, all of which require some degree of shoulder elevation. Augmenting the pressure by carrying a heavy object may exceptionally provoke the symptoms as well, but normally only to a mild degree.
Cyriax explained this pattern as being the consequence of a diminishing tone in the shoulder muscles, starting in middle age. As a result, the shoulder girdle droops down during the day, resulting in compression of the most medial trunks of the brachial plexus, between the first rib and clavicle. Compression occurs during the day but the symptoms come on mainly at night after the pressure on the nerve has disappeared. He called this the ‘release phenomenon’ (see p. 26). The process seldom leads to damage of the nerve parenchyma with subsequent muscular atrophy because the brachial plexus can recover every night when the pressure is released.
Functional examination
The diagnosis is based mainly on the typical history, all passive movements of neck, shoulder and shoulder girdle being normal.51 The resisted movements are of normal strength and painless, except for C8 or T1 structures in the hand, which may be weakened when the compression is the outcome of a cervical rib. This type of characteristic history should always be followed up with the following additional tests.
Sustained elevation of the shoulders
The patient sits in a comfortable position and is asked to shrug the shoulders for about 3 minutes (Fig. 7). This causes maximum release of pressure and therefore may bring on the pins and needles and abolish vascular symptoms if present. However, this test is not always positive when thoracic outlet syndrome is present; in this case, release of pressure must be tried in different positions, either fully raising the arms above the head and maintaining this position for 3 minutes (Fig. 8) or lying supine with both hands on the head for the same length of time (Fig. 9).
Auscultation, pulse and blood pressure
The subclavian area should always be auscultated for a bruit, the radial pulse must be checked and blood pressure must be measured. The diagnostic significance, however, is not certain.
Other tests
Other tests for thoracic outlet syndrome have been advocated classically. Although we regard them as less specific and reliable, they are mentioned here for completeness. Adson’s test,52 the modified Adson’s test and Roos’ test (elevated arm stress test)53 are regarded by some as totally unreliable, because about 50–60% of the normal population have positive findings.54,55
Adson’s test
The patient stands with the arm resting at the side. In this position the examiner feels the patient’s radial pulse. Then the patient is asked to take a deep breath and to turn the head towards the involved side. Any change in pulse degree or in blood pressure, preferably measured by a Doppler probe, is noted. If there is a change, it means that the subclavian artery is compressed and probably also the brachial plexus. Adson considered a positive test to indicate vascular compression by the scalenus anterior.
Modified Adson’s test
This is similar to Adson’s test but the patient turns the head away from the involved side. In this test, the scalenus medius puts pressure on the vessels. A positive test is thought to imply scalenus medius compression.
Roos’ test
The patient abducts the arms to 90°, then opens and closes the hands slowly for 3 minutes. Those who are unable to keep their arms and hands elevated because of pins and needles are regarded as suffering from thoracic outlet syndrome. However, in carpal tunnel syndrome, active flexion of the fingers can bring on the pins and needles, and therefore this test does not differentiate between these two disorders (Fig. 10).
Examination of the cervical spine
If pins and needles are present in the upper extremities, a full examination of the cervical spine must always be carried out. In thoracic outlet syndrome, the passive movements of the neck are painless and of full range. When a cervical rib is present, weakness and atrophy of the thenar, hypothenar and interosseous muscles may be found.
Technical investigations
It should be emphasized that thoracic outlet syndrome is primarily a clinical diagnosis, based on a full history and a complete clinical examination.
Electromyography (EMG) and conduction studies are of little value, for two reasons.56,57 First, the range is quite variable in normal patients. Second, because the stimulating electrode can not be placed proximal to the level of the compression, the compound action potential which is measured does not cross the site of the nerve compression. But EMG is helpful for differential diagnosis, in excluding nerve compression at other levels, such as ulnar nerve impingement at the elbow or carpal tunnel syndrome.
A radiograph of both the cervical spine and thorax can help to detect a cervical rib, a hypertrophic transverse process of C7 (suggesting a fibrous band) or the formation of a clavicular callus.58 It also helps to exclude a Pancoast’s tumour. A CT scan may demonstrate an abnormal fibrous band.
Angiography (arteriography and/or phlebography) must be considered but is only indicated when the vascular symptoms are so severe that surgery is contemplated. Such can be the case when signs and symptoms of arterial embolism or arterial and/or venous occlusion are present.
Differential diagnosis
Cervical disc protrusions
When a posterolateral cervical disc compresses a nerve root, the cervicobrachial pain is very severe, often worse at night, coming and going without apparent reason. Some articular movements of the cervical spine increase the pain, although, surprisingly enough, their influence may be only very slight.
In posterocentral cervical protrusion with cord compression, pins and needles are felt in both hands and feet and are brought on or increased by neck flexion.
Compression of the ulnar nerve
A lesion of the ulnar nerve provokes pins and needles felt only in the fifth finger and at the ulnar half of the fourth. In compression at the cubital tunnel, some local pain around the elbow may also occur (see p. e138 of this chapter).
Compression of the radial nerve
Pins and needles may be felt at the dorsal aspect of the lower arm, and of the  radial digits. Resisted extension of the hand is weak but painless. Sometimes a drop hand is found (see p. e132 of this chapter).
radial digits. Resisted extension of the hand is weak but painless. Sometimes a drop hand is found (see p. e132 of this chapter).
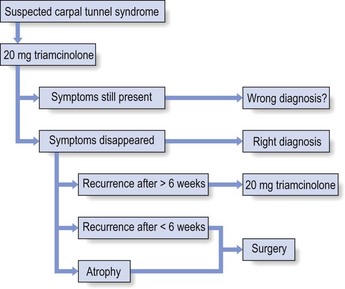
Carpal tunnel syndrome
Compression of the median nerve in the carpal tunnel causes paraesthesia felt on the palmar aspect of the thumb, index and middle finger and the radial half of the ring finger. Carpal tunnel tests may be positive, although in 50% they remain negative (see p. e155 of this chapter).
Carcinoma of the superior sulcus of the lung (Pancoast’s tumour)
The coexistence of pins and needles and Pancoast’s tumour implies invasion of the brachial plexus, which may give rise to a palsy of the interosseous muscles at the hand. Very often a palsy of the recurrent nerve, causing hoarseness, is also present. Clinical inspection of the face may reveal Horner’s syndrome (ptosis of the upper eyelid, enophthalmia and myosis; see p. 3 of online chapter Disorders of the thoracic cage and abdomen).
Treatment
Anatomical variety
Thoracic outlet syndrome due to a cervical rib or a fibrous band can only be treated surgically. Paraesthesia and pain mostly disappear but wasting and weakness seldom resolve completely.
Postural variety
Because of the lack of consensus about the aetiology of this syndrome, various forms of treatment have been described (see Box 2). In the light of the mechanism that we consider responsible for the symptoms, the following approach is proposed.
Posture and exercise
Cases caused by the first rib can be helped by conservative management. However, the first step in the treatment is a clear explanation to the patient of the pressure and release mechanism of the disorder. He or she should understand that the pins and needles at night are the result of compression during daytime and that they come on when the nerve is liberated from the pressure. He or she also should realize that, to get rid of the complaints, pressure on the nerve during the day must always be avoided.
To achieve the latter, the patient is asked to keep the shoulders slightly shrugged all day. Carrying loads and wearing heavy coats must be avoided.
For some weeks, the following daily exercise must be done in the evening. Seated in an armchair, elbows resting on the arms, both shoulders are kept shrugged passively (Fig. 11). This brings the pins and needles on after a while but the position is maintained, even if symptoms become more severe. Once they diminish and disappear spontaneously, usually in half an hour, the shoulders are let down.
If the exercise is repeated daily, the patient soon finds that the paraesthesia comes on later and later at night and then appears only in the early morning hours and, after some more weeks of exercising at night, finally disappears completely. Exercises can then be stopped. But the patient must remember to continue indefinitely to keep the shoulders slightly shrugged during the day.
As mentioned previously, it is important to explain the release phenomenon in clear terms to the patient, so that he/she understands that the pins and needles are due to the nerve being fully liberated from the pressure. Lacking such understanding, the patient will mistakenly regard the exercise as harmful and discontinue it.
An orthosis designed to elevate the shoulder has been described. It has good results in 77% of patients.59
Surgery
In cases refractory to conservative treatment, resection of the normal first rib can be performed.60–63 However, this is major surgery and not always successful in relieving symptoms. This approach also carries potential dangers, because of the close relationship to the brachial plexus and subclavian/axillary artery.64,65
Table 2 provides a summary and differential diagnosis of the anatomical and postural varieties of thoracic outlet syndrome.
Table 2
Differential diagnosis and summary of anatomical and postural varieties of thoracic outlet syndrome
| Anatomical | Postural | |
| Age | 20–30 years | Middle-aged and elderly |
| Release phenomenon? | At first | All the time |
| Pins and needles? | All day | At night |
| Atrophy and weakness? | Thenar/hypothenar/interossei | None |
| Cold hands? | Possible | None |
| Cynosis and swelling? | Possible | No |
| Treatment | Surgery | Keeping shoulders slightly shrugged at all times; daily exercises in the evening |
Plexitis
Acute or subacute neuritis of the brachial plexus has been described under different headings: amyotrophic neuritis, neuralgic amyotrophy, Parsonage–Turner syndrome, idiopathic brachial plexus neuropathy, brachial neuritis. There is a tendency to use the term ‘acute brachial plexus neuropathy’.
This rather uncommon parenchymatous disorder of the peripheral nerves, described by Parsonage and Turner,66,67 has no specific cause.68 However, two biopsy studies, mentioned by Stewart,36 may clarify the pathology and pathogenesis of this syndrome. They suggest that the disorder is the result of immune-mediated nerve damage following a previous viral infection or autoimmune process.69,70
It may develop at any age.71 The onset is with quite sudden central neck pain or pain in one or both scapulae. After some hours to some days the pain radiates to one or both upper limbs, sometimes as far as the hands. Even in bilateral distribution the picture is asymmetrical and paraesthesia is uncommon. The pain is extreme during the first weeks, continues for 2–3 months and then gradually diminishes. Sometimes coughing or taking a deep breath may also be painful. It takes another 2 or 3 months before the patient is comfortable.
Examination in the early stage may show that the neck movements influence the cervicoscapular pain even though the lesion is not articular, but a clear pattern is not found.
Once the acute stage of an attack is over and the initial pain has disappeared, a patchy paresis and atrophy will become evident. There is visible atrophy in shoulder and shoulder girdle72 and isometric testing reveals gross weakness in several muscles. All kinds of combinations of weakness may be possible. A typical feature of neuralgic amyotrophy is the patchiness of the motor and sensory symptoms. Histological studies have already shown that the pathologic process can cause very focal damage to one or a few of the fascicles that make up a brachial plexus trunk or cord, while simultaneously affecting several parts of the plexus as a whole.73,74 This is clinically reflected by a wide variety in the possible distribution – and severity – of paresis. Any part of the brachial plexus, and clinically any muscle or skin area can be involved, in all sorts of combinations. It is precisely the recognition of this patchiness that is a very important clue to the diagnosis of neuralgic amyotrophy.75 The muscles most often involved are: serratus anterior, deltoid, supraspinatus and infraspinatus, followed in frequency by biceps and triceps. The infraspinatus muscle seems to be always affected. Sensory abnormalities are much less pronounced than pain and weakness.
Analgesics may be necessary during the pain period but the other symptoms and signs recover spontaneously. In the majority of patients, the weakness abates in the next few months after the disappearance of the pain.76
Disorders of the long thoracic nerve
Anatomy
The long thoracic nerve takes origin in the upper trunk of the brachial plexus from the ventral rami C5, C6 and often C7. It courses behind the brachial plexus and follows the lateral wall of the thorax where it divides into several branches (Fig. 12).
Innervation
The long thoracic nerve is a pure motor nerve and innervates the serratus anterior muscle. The serratus anterior is a broad flattened sheet of muscle originating from the first nine ribs and passes posteriorly around the thoracic wall before inserting into the costal surface of the medial border of the scapula (Fig. 13).77 The main function of the serratus anterior is to protract and rotate the scapula, keeping it closely opposed to the thoracic wall and optimizing the position of the glenoid for maximum efficiency for upper extremity motion.78
Disorders
The nerve can become affected:
• As the result of iatrogenic causes, such as axillary or first rib surgery79,80
• As the result of direct compression (‘backpack injuries’) because of its long course along the thorax81
• As the result of excessive shoulder activity.82,83 Although the association is well established, there is no consensus of exactly how trauma injures the long thoracic nerve. Work on cadavers suggests that injury may take place as the nerve exits the fascial sheath that encompasses it, either in the form of a traction injury 84 or in a ‘bow-stringing’ effect85
Mononeuropathy of the long thoracic nerve
The patient presents with pain around the affected shoulder, which either arises spontaneously or is linked to some traumatic event.86 This pain may radiate down the arm and to the scapula. In addition, he typically complains of shoulder weakness. The pain usually resolves spontaneously over the next several weeks, but the patient is left with weakness and a winged scapula.87
Upon inspection, medial scapular winging is evident, with the medial and inferior borders closer to the spine and lifted superiorly when compared to the normal side.88
Examination of the shoulder shows a limitation on active elevation of the arm of about 45–90°. Passive movements are of full range; resisted movements are normal. The diagnostic manūuvre is to ask the patient to push against a wall with the arms stretched out horizontally in front of the body (Fig. 14).89 In this position, the vertebral border of the scapula lifts further from the thoracic wall due to the loss of serratus anterior scapular protraction.
In most cases spontaneous recovery occurs in 4–8 months.90 However, in approximately 25% of patients the paralysis and scapular winging will persist and such patients are then candidates for surgical reconstruction.91,92
Disorders of the suprascapular nerve
Anatomy
The suprascapular nerve takes origin from the upper trunk of the brachial plexus with fibres from the C4 to C6 ventral rami. It courses through the posterior triangle of the neck, underneath the trapezius muscle. The nerve passes through the suprascapular notch of the scapula, which is bridged by the thick transverse scapular ligament93 (Fig. 15). After entering the supraspinatus fossa the nerve gives off two motor branches to the supraspinatus muscle and then passes laterally within the fossa, providing sensory branches to the posterior capsule of the glenohumeral joint and acromioclavicular joint. It then goes around the lateral border of the base of the spinous process to the infraspinatus fossa, where the nerve terminates by supplying motor branches to the infraspinatus muscle.
Innervation
The nerve innervates the supraspinatus and infraspinatus muscles and receives sensory and proprioceptive branches from the glenohumeral and acromioclavicular joints, as well as the subacromial bursa and posterior aspect of the capsule.
Disorders
The suprascapular nerve has a short course and several sites of relative fixation, making it vulnerable to both traction and compression forces. The nerve is fixed at both its origin at the Erb point on the brachial plexus and at its terminal insertion on the infraspinatus. The nerve is relatively fixed at the suprascapular notch, and anatomical studies have shown that motion does not occur at this point.94 Suprascapular nerve dysfunction can be caused by:
• Entrapment of the nerve by a ganglion,95,96 or a tight ligament at the level of the suprascapular notch
• Entrapment at the spinoglenoid notch97,98,99
• Acute brachial plexitis (the suprascapular nerve is involved in 97% of the cases)100
• Trauma, e.g. shoulder luxation or scapular fracture101
A lesion at the suprascapular notch is either the result of a ganglion cyst or a traction trauma. Downward traction of the scapula can result in opposition of the suprascapular nerve against the sharp inferior border of the transverse scapular ligament. Cross-body abduction or protraction with forward flexion, as seen in fencing, throwing sports,102 racquet sports, and weight lifting, have also been found to maximally stretch the suprascapular nerve.
Entrapment can also occur more distally at the spinoglenoid notch, which is more commonly seen in athletes whose sports require rapid forceful external rotation movements, such as volleyball.103,104 The cocking motion for the smash results in rapid external rotation of the shoulder; this rapid motion of the infraspinatus muscle is thought to pull the suprascapular nerve against the base of the scapular spine, resulting in nerve injury at this level. Injury to nerves in the spinoglenoid area has also been noted secondary to ganglion cysts.
Patients complain of a fatigue-like posterior shoulder pain which may be aggravated by activities that stretch or mobilize the nerve, such as combing one’s hair or moving the scapulae. Patients with pathology at the spinoglenoid notch may also present with painless and isolated wasting of the infraspinatus muscle as the nerve fibres at the notch contain no sensory afferents.
Inspection shows atrophy of the supraspinatus and/or infraspinatus muscles. On clinical examination, full passive lateral rotation of the arm may provoke some pain, as may all active and passive scapular movements. Passive horizontal adduction of the arm is also painful. Depending on the level of nerve involvement, there is weakness in abduction or external rotation, or both. Proximal injury of the suprascapular nerve at the level of the suprascapular notch causes the weakness of both abduction and external rotation, while nerve injury at the level of the spinoglenoid notch affects only the infraspinatus and results in isolated weakness of external rotation.
An EMG shows a denervation of the infra- and supraspinatus which, together with the history of an injury, confirms the diagnosis. Ultrasonography can be used to show a ganglion. Magnetic resonance imaging is appropriate to diagnose entrapment.105
The management for suprascapular nerve entrapment includes a conservative regimen of observation, rest, analgesics, and cortisone injections into the suprascapular notch.106,107 If this treatment is unsuccessful, surgical decompression of the nerve at the suprascapular ligament is necessary. In most patients it leads to full relief.108,109
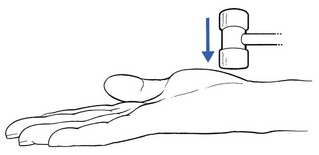
Technique: injection
The patient sits on a chair. The entire spine of the scapula is marked from the medial to the lateral edge. This line is bisected and a second line drawn at a 45° angle in an anterolateral direction. A 2.5 cm mark is made on this second line and a 7 cm needle, fitted to a syringe containing 2 ml of steroid, is inserted vertically downwards at this point until it hits the bone at the base of the scapular spine (Fig. 16). The tip of the needle is then moved further anteriorly until it slips in the suprascapular notch. The steroid is injected here.
Disorders of the axillary nerve
Anatomy
The axillary nerve takes origin in the posterior cord of the brachial plexus from fibres derived from C5–C6. It curves around the neck of the humerus and passes through the quadrilateral space close to the inferior shoulder joint capsule. This quadrilateral space is bounded by the teres minor superiorly, the long head of the triceps medially, the teres major inferiorly, and the humeral neck laterally and forms a potential site of compression for the axillary nerve as it passes from the anterior to the posterior aspects of the shoulder.110 After passing through the quadrilateral space, the axillary nerve divides into anterior and posterior branches, which supply the anterior and posterior portions of the deltoid muscle. The posterior branch of the axillary nerve also supplies the teres minor and supplies cutaneous sensation overlying the deltoid (the upper lateral cutaneous nerve of the arm). The short length of the axillary nerve renders it vulnerable to stretch injuries, especially during shoulder dislocation 111 (Fig. 17).
Innervation
The axillary nerve is mixed. The motor branches innervate the deltoid muscle and the teres minor muscle. The sensory branch innervates the skin over the deltoid region and the upper and lateral part of the arm.
Disorders
• Most axillary nerve lesions occur after anterior shoulder dislocation,73 the exact incidence ranging between 9% and 18%.112 Blunt trauma to the anterior aspect of the shoulder without dislocation has also been implicated in axillary nerve trauma in contact sports.113,114
• Acute axillary neuropathy is also associated with backpacking, usually in inexperienced hikers. The cause of axillary nerve injury in ‘rucksack palsy’ is thought to be traction caused by depression of the shoulder from the excessively weighted backpack.
• Quadrilateral space syndrome represents a chronic compression syndrome of the axillary nerve in throwing athletes.115 Axillary nerve entrapment then occurs insidiously in the quadrilateral space without history of trauma. Fibrous bands at the inferior edge of the teres minor have been implicated, as have randomly oriented fibrous bands found in the quadrilateral space.116,117
• The axillary nerve sits approximately 2 cm inferior to the usual posterior portal for arthroscopy, putting this nerve at risk during routine arthroscopic procedures.118 An unintentional local infiltration with steroid into the axillary nerve on infiltrating too far distally for infraspinatus tendinitis may cause the same problem.
Symptoms are often vague, consisting of a dull ache and/or pins and needles over the deltoid area. Sometimes extensive visible wasting of the deltoid is present, together with an area of cutaneous analgesia in the mid-deltoid region. According to Cyriax,119 (his p. 153) some patients tend to relax the axillary nerve as much as possible by elevating the scapula at the same side during the first few weeks after the injury. The process is a consequence of spasm of the trapezius and leads to pain on passive side flexion of the neck towards the contralateral side. Deltoid weakness is often masked by the activity of supraspinatus and pectoralis major.120 Because the supraspinatus muscle is not involved, active elevation of the arm remains possible, and weakness is only found on resisted abduction. The diagnostic test is to ask the patient to abduct the arm to 90° and to bring it further backwards into horizontal extension (Fig. 18). This is impossible with an axillary nerve lesion.
Spontaneous cure is possible, but takes about 6 months. Care should be taken to mobilize the shoulder during the recovery so as to avoid an immobilizational arthritis. If no improvement has occurred after 6 months, surgical decompression is needed via a release of the teres minor and major tendinous insertions.121
Disorders of the radial nerve
Anatomy
The radial nerve takes origin in the posterior trunk of the brachial plexus and thus contains fibres from C5–T1. It reaches the lateral wall of the axilla and winds around the posterior aspect of the humerus in the groove for the radial nerve. It then pierces the lateral intermuscular septum to enter the anterior compartment of the arm. It lies lateral to the biceps and continues between the biceps tendon and the proximal part of the brachioradialis muscle. At the level of the elbow it divides into a superficial sensory branch (the superficial radial nerve) and a deep motor branch (the deep radial nerve). The latter continues to become the posterior interosseous nerve.
The superficial radial nerve lies under the brachioradialis muscle and follows the lateral border of the radius until at the wrist it divides into terminal digital branches to the dorsoradial part of the hand and the three radial digits.
The posterior interosseous nerve winds around the neck of the radius and goes into the dorsal compartment of the forearm. It pierces the supinator muscle through the arcade of Fröhse and runs deeply under the extensors as far as the wrist (Fig. 19).
Innervation
The motor part of the radial nerve innervates mainly the extensors of the arm and forearm: triceps and anconeus muscles, brachioradialis, extensors of the wrist, supinator and extensors of thumb and fingers.
The sensory part supplies the skin of the lateral arm, the posterior part of the forearm, the radial dorsum of the hand and the skin of the dorsal aspect of the proximal and middle phalanges of  radial digits.
radial digits.
Disorders
The radial nerve is quite frequently affected by pathological conditions. This happens in more generalized diseases, such as poisoning by heavy metals (e.g. lead), but also in more localized lesions, either traumatic or following entrapment of the nerve tissue. The symptoms and signs depend on where, along the nerve, the lesion lies. The radial nerve may become affected at five different sites: the proximal and middle part of the upper arm, the distal part of the upper arm, the proximal part of the forearm and the distal part of the forearm (Table 3).
Lesions at the proximal and middle part of the upper arm
When the lesion results from an injury – fracture or dislocation of the humerus – it is usually combined with an axillary palsy.101 Space-occupying lesions in the axilla or the use of old-fashioned axillary crutches are other (rare) causes.122,123
Examination reveals weakness of extension and supination of the elbow, together with weakness of extension of wrist, fingers and thumb. This results in a characteristic position of elbow and hand – porter’s hand or drop hand. Because of the anastomoses between the posterior cutaneous nerve of the arm – first branch of the radial nerve – and other neighbouring nerves, sensory deficit is not common but when it occurs it is found at the lateral aspect of the arm and posterior aspect of the forearm as far as the dorsum of the wrist.
Differential diagnosis must be made from spinal cord, intraspinal and radicular lesions (C7), as well as conditions affecting the brachial plexus, neuritises or myopathies.
Lesions at the distal part of the upper arm
Lesions are more common at the distal than the middle and proximal part of the arm. The palsy may be traumatic – fracture of the humerus,124,125 fracture or dislocation of the elbow – or may result from a sustained pressure just proximal to the elbow. This is typically the case in a patient who has fallen asleep with the arm over the edge of a chair or has lain all night with the arm resting against the hard edge of a bunk – ‘Saturday night paralysis’. The full radial syndrome develops, except that the triceps and anconeus muscles are unaffected, as is the brachioradialis muscle. The patient awakes with a painless dropped wrist.
Sensory disturbances may occur at the dorsal aspect of the forearm when the posterior cutaneous nerve of the forearm is involved, although this area may have overlapping supply from neighbouring sensory nerves – the lateral and medial cutaneous nerves of the forearm. The superficial sensory branch of the radial nerve is responsible for cutaneous deficit at the radial and dorsal aspect of the hand, except when anastomoses with either the lateral cutaneous nerve of the forearm – a sensory branch of the musculocutaneous nerve – or the dorsal branch of the ulnar nerve at the hand provide an alternative pathway.
Lesions at the upper part of the forearm
Level with the head of the radius, the radial nerve divides in its two terminal branches – the superficial (sensory) and deep (motor) branches (see Fig. 19). The latter then forks off into (1) muscular rami running towards the supinator, extensor digitorum, extensor digiti minimi and extensor carpi ulnaris muscles, and (2) the posterior interrosseous nerve of the forearm, which supplies the long abductor and extensors of the thumb as well as the extensor indicis proprius. When a lesion occurs proximal to this division, symptoms of both are combined. As the branches supplying the brachioradialis, extensor carpi radialis longus and brevis, and brachialis escape the compression, there is only weakness of supination, extension of the fingers, ulnar deviation of the wrist and extension and abduction of the thumb.
Deep branch of the radial nerve
Conditions such as fracture and/or luxation of the head of the radius or local inflammatory processes, for example chronic bicipitoradial bursitis, may cause compression of the deep branch of the radial nerve where it turns around the head of the radius. The result is weakness of supination, ulnar deviation of the wrist and finger extension.
Posterior interosseous nerve of the forearm
Just below the point where the deep radial nerve comes to lie at the dorsal aspect of the forearm, the posterior interrosseous nerve of the forearm branches off and passes through the deep and superficial heads of the supinator brevis muscle126 (Fig. 21). When the edge of the upper border of the superficial head has become fibrous, this opening forms the arcade of Fröhse,127 also called the radial tunnel. The nerve then passes further down along the interrosseous membrane and innervates the abductor pollicis longus, extensor pollicis longus and brevis, and extensor indicis proprius muscles.
The posterior interosseous nerve can be compressed as the result of: (1) an injury, usually a fracture (or the hardware used to fix fractures),128,129 or elbow joint dislocation;130 (2) space-occupying lesions, such as synovial proliferations from the elbow joint in rheumatoid arthritis131,132 or soft tissue tumours,133,134 for example lipomas;135 or (3) fibrous bands, which can be traumatic in origin (e.g. Volkmann’s contracture) or developmental (arcade of Fröhse).136–140
Many authors believe that compression of the posterior interosseous nerve at the point where it passes through the arcade of Fröhse is a cause of lateral elbow pain and they therefore consider it as a type of tennis elbow. We do not agree that this condition should be considered to be a (resistant) type of tennis elbow, because the lesion does not lie in the extensors of the wrist. Hagert et al141 also regarded epicondylitis and posterior interosseous nerve entrapment as ‘two different disorders, which have nothing to do with each other, and which should therefore not be mixed up’.
Radial tunnel syndrome
In 1883, Winckworth stated that the posterior interosseous nerve could become compressed where it passes through the supinator muscle.142 Since Roles and Maudsley described the radial tunnel syndrome in 1972,143 this pathology has become recognized as a cause of resistant tennis elbow.133,136,144–146 This idea is based on the reports of good results after surgical decompression of the posterior interosseous nerve at the radial tunnel.147,148
Nerve compression by the edge of the superficial supinator muscle seems to occur on passive pronation of the forearm. On active supination the increase in pressure is much greater, which has led to the conclusion that dynamic compression of the posterior interosseous nerve by the edge of the superficial supinator muscle is probably a cause of local nerve irritation and pain.
In compression of a predominantly motor nerve, such as the posterior interosseous nerve, the main symptom would be paralysis. Kopell and Thompson, however, state that entrapment of a motor nerve may cause diffusely localized dull aching pain.149 The pain would originate from the nociceptive thin or non-myelinated afferent nerve fibres of muscular and extramuscular origin.150
However, the symptoms described by different authors are very similar to those found in tennis elbow: pain at the lateral side of the elbow, radiating distally along the posterior aspect of the forearm. The pain may be constant and can be brought on or aggravated by exertion, especially rotation movements, and the symptoms continue for some time after the causative strain has ceased. There is also diffusely localized pain on resisted supination and/or pronation as well as on resisted extension of the middle finger. Local tenderness is present over the proximal and posterior aspect of the forearm, at the suspected entrapment site. These symptoms and signs correspond with the clinical picture of what we have described as type IV (muscular) tennis elbow (see p. 313).
Treatment consists of surgical decompression. After surgery, the pain seems to disappear gradually, in the course of 6–12 months.
Werner analysed the hypothesis that posterior interosseous nerve entrapment can be a cause of lateral elbow pain.151 The following investigations were carried out: patients with suspected posterior interosseous nerve entrapment were operated on by decompression of the nerve and then subjected to a follow-up for 2 years; the topographical anatomy was compared with observations at dissections; the epidemiology and symptomatology were compared with that in a series of cases of lateral epicondylitis. He concluded that lateral elbow pain may indeed be caused by dynamic compression of the posterior interosseous nerve and that it can be relieved by decompression of the nerve where it enters through the supinator muscle. The diagnosis is based solely on palpation and on positive resisted supination. Pain on resisted extension of the middle finger seems to be an unreliable test. Electrophysiological examinations (EMG) are of limited diagnostic value.
Using Cyriax’s methods to examine lateral elbow pain, we have some difficulties in accepting the existence of a radial tunnel syndrome, giving rise to pain. If the main symptom is pain at the lateral aspect of the elbow and the pain is clearly aggravated by a resisted movement, one should think of a lesion of a contractile structure and try to find out what structure is at fault:
• Pain on resisted supination draws attention to the supinator brevis muscle.
• Pain on resisted extension of the middle finger does not exclude a tennis elbow, because this test also implicates the extensors of the wrist.
Differential diagnostic tests should be included (see p. 313). Pain on palpation is not reliable: the lateral aspect of the elbow is always tender to the touch and therefore the response to the palpatory manūuvres may be false-positive.
We conclude that the diagnosis of radial tunnel syndrome is probably made too often. A clear distinction should be made between the two different conditions: (1) tennis elbow, a lesion in the radial extensors of the wrist, and (2) radial tunnel syndrome (Table 4). Other authors share this view.152,153
Table 4
Differential diagnosis: type IV tennis elbow and radial tunnel syndrome
| Tennis elbow type IV | Radial tunnel syndrome | |
| Elbow pain | Lateral pain on hand movements | Ache at elbow, especially at rest or after repetitive pronation and supination |
| Resisted test | Pain on wrist extension and radial deviation | Negative |
| Tenderness | In deep muscles overlying neck of radius | In supinator |
| Weakness | No muscular weakness | Possible weakness of thumb and index finger |
We believe that what has been described in the literature as radial tunnel syndrome very often has nothing to do with the posterior interosseous nerve at all, but is simply a lesion of an extensor of the wrist, the symptoms of which have erroneously been attributed to that nerve. We speculate that the good results claimed for surgery may be the outcome of either spontaneous recovery or incidental permanent lengthening of some muscular fibres during operation. In the latter instance, the operation, ostensibly for radial tunnel syndrome, unintentionally becomes an operation for tennis elbow.
When entrapment of the posterior interosseous nerve at the elbow occurs it should give rise to a dull ache over the lateral aspect of the elbow, eventually radiating down the posterior aspect of the forearm. In due course, weakness will be found of abduction and extension of the thumb and of extension of the index finger. Paraesthesiae are absent.
Stewart confirms our view.154 His ideas are also based on clinical findings and have been reinforced following the publication of three studies showing that, in this group of patients in whom pain is the main symptom, there is little evidence for a focal nerve lesion.155–157
Lesions at the distal part of the forearm
The superficial sensory branch of the radial nerve runs under the brachioradialis muscle along the radial artery and further towards the hand. At the level of the wrist it divides into five dorsal digital nerves (Fig. 22) and supplies the skin at the dorsal aspect of the thumb, index, middle and radial half of the fourth finger but not the terminal phalanges, which are supplied by the median nerve.
In the distal part of the forearm the nerve may rarely become affected as the result of external pressure (e.g. damage by handcuffs);158,159 the result is paraesthesia and sensory deficit over the radial and dorsal aspect of the hand. If the pressure involves the medial and dorsal branch to the thumb, for example after the protracted use of small scissors, the ulnar aspect of the thumb becomes numb.
Disorders of the ulnar nerve
Anatomy
The ulnar nerve takes origin in the lower trunk of the brachial plexus from the spinal nerves C8–T1. It runs from the axilla down the medial aspect of the upper arm. At mid-humerus it pierces the medial intermuscular septum towards the posterior compartment. It follows the medial head of the triceps onto the retrocondylar groove at the elbow. It then courses under the aponeurotic arch joining the two heads of the flexor carpi ulnaris muscle – the cubital tunnel – and follows its course towards the wrist, under this muscle (Fig. 23). At the wrist it runs through Guyon’s tunnel before it divides into its terminal branches.
Innervation
There are no branches in the upper arm. In the forearm motor branches supply the flexor carpi ulnaris muscle and the ulnar half of the deep flexor digitorum. Sensory branches supply the skin of the ulnar half of the hand. At the wrist the ulnar nerve, as it leaves Guyon’s tunnel, divides into a superficial and a deep branch. The deep branch is motor and innervates the hypothenar muscles, the interossei, the two ulnar lumbricals and, on the thenar side of the hand, the adductor pollicis and the deep head of the flexor pollicis brevis. The superficial branch is sensory and supplies the skin of the little finger and the ulnar half of the ring finger.
Disorders
Ulnar nerve entrapment is one of the most frequent peripheral neuropathies, especially compression of the nerve at the level of the elbow. As it is a combined motor and sensory structure (Table 5) entrapment leads to a gamut of symptoms and signs.
The two most frequent localizations of compression are pressure in the cubital tunnel at the inner side of the elbow, and pressure in the area of Guyon’s tunnel at the wrist.
Lesions at the elbow
In 1877, Panas160 was the first to describe ulnar nerve palsy, in a paper to the Académie de Médecine. Since then, several authors have described this lesion as well as the possible surgical treatments.
The ulnar nerve courses under the medial head of the triceps muscle towards the posterior aspect of the medial epicondyle (see Fig. 23) where it lies superficially in a shallow groove behind this bone (sulcus for the ulnar nerve) and is, therefore, very vulnerable to direct contusion. It becomes stretched during flexion of the elbow. The nerve runs further distally in between the two heads of the flexor carpi ulnaris muscle, which form an aponeurotic arch. Together with the medial epicondyle, the olecranon and the medial collateral ligament, this arch forms the cubital tunnel (Fig. 24).
Aetiology
Entrapment of the ulnar nerve – cubital tunnel syndrome – is the second most common compressive neuropathy of the upper extremity, with only carpal tunnel syndrome presenting more frequently. Entrapment of the ulnar nerve at the elbow has several different causes, summarized in Box 3:
• Friction may be the result of recurrent dislocation of the nerve.161,162 The patient notices that from time to time the nerve comes out of its groove and then replaces spontaneously. This phenomenon is sometimes accompanied by a paraesthetic twinge felt in the ulnar aspect of the hand and the ulnar one and a half fingers. Recurrent dislocation may in the end lead to ulnar palsy.
• A fall on the elbow or a direct blow to the medial aspect of the elbow may bruise the nerve sheath which becomes irritated. The condition is self-perpetuating, as flexion movements continue the trauma.
• Structural changes may alter the stress on the nerve and thus cause friction on certain movements. These changes are excessive cubitus valgus or alterations of the position of the elbow after malunited fractures of the medial condyle.163 Humeral trochlear hypoplasia has been described as a rare condition that may result in ulnar nerve palsy.164
• Positions of prolonged flexion (e.g. during the night) may in the end set up the known symptoms.165 This type of ulnar nerve lesion is sometimes known as cubital tunnel syndrome.166,167 Flexion at the elbow may have the following consequences resulting in external compression of the ulnar nerve:
 The volume in the cubital tunnel is reduced.
The volume in the cubital tunnel is reduced.
 The arcuatum ligament stretches and comes under tension as the olecranon moves away from the medial epicondyle.168,169
The arcuatum ligament stretches and comes under tension as the olecranon moves away from the medial epicondyle.168,169
 The ulnar collateral ligament relaxes and bulges slightly.170
The ulnar collateral ligament relaxes and bulges slightly.170
 The ulnar nerve elongates and is moved medially because it lies some distance from the axis of rotation of the elbow joint.
The ulnar nerve elongates and is moved medially because it lies some distance from the axis of rotation of the elbow joint.
• A loose body causing compression of the ulnar nerve is quite uncommon. If a loose fragment in the elbow joint displaces medially at the posterior aspect of the joint, it can compress the ulnar nerve and cause paraesthesia in its territory. A non-capsular pattern will be found on examination.
• Osteophytes, tumours or ganglia of the nerve may compress the nerve in the cubital tunnel.
• Idiopathic: the aetiology very often remains unknown.171 In as many as 50% of cases a precipitating cause is not apparent.172
Diagnosis
The history is obvious. The patient describes paraesthesia and/or numbness in the ulnar half of the fourth and the entire fifth finger and eventually weakness or clumsiness of the hand. A slight ache may also be felt at the elbow. A history of trauma may be elicited or merely that the symptoms came on spontaneously. In spontaneous onset, further questioning may determine whether the cause is postural.
On inspection there may be signs of joint abnormality. Furthermore, there may be wasting of the intrinsic muscles of the hand, the hypothenar muscles or some forearm muscles – flexor carpi ulnaris and deep flexors of the fingers. In severe cases, the patient may present with an ulnar palsy leading to weakness of the ulnar half of the deep flexor digitorum and of the flexor carpi ulnaris muscles, with weakness of the intrinsic hand muscles resulting in a claw hand.
On examination, signs are found that immediately draw attention to the ulnar nerve. A few accessory tests may give some further confirmatory information:
• The elbow is brought into maximal flexion and maintained there for a few minutes, which may bring on the pins and needles and indicates a possible postural cause.
• The elbow flexion test:173 with the patient sitting and both shoulders and arms in the anatomical position, both elbows are fully but not forcefully flexed, with full extension of the wrist. This position is maintained for a few minutes and the patient reports to the examiner at regular intervals whether pain, numbness or tingling occur or increase.174 When combined with pressure on the ulnar nerve the test becomes even more sensitive.175
• Tests for the sensitivity to light touch and two-point discrimination in the peripheral distribution of the ulnar nerve.
• Specific testing of the motor function of the abductor digiti minimi, the flexors digitorum profundi to the little and ring fingers and the flexor carpi ulnaris muscles.
On palpation of the inner aspect of the elbow, tenderness in the nerve sheath may be found and should be compared with the other elbow. A positive finding suggests frictional neuritis. Thickening of the nerve sheath indicates recurrent dislocation. Because it is not always clear whether the cause lies either at the elbow or at the wrist, tenderness should also be sought at Guyon’s tunnel at the wrist.176
Failure to find a local cause may indicate a neuritis from metabolic problems such as diabetes mellitus, alcoholism, hypothyroidism or lead poisoning.
According to McGowan, cited by some authors,177,178 ulnar entrapment neuropathy can be classified into three grades:
• Grade I: subjective symptoms combined with hypoaesthesia in ulnar fingers.
• Grade II: weakness and wasting of the interossei, combined with subjective symptoms.
• Grade III: marked weakness and wasting of the interossei, adductor pollicis and hypothenar muscles, combined with anaesthesia in the ulnar fingers.
A differential diagnosis must be made with other possible proximal causes: cervical myelopathies, anterior horn lesions, polyneuropathies, myopathies, cervical nerve root problems (C7, C8) and thoracic outlet syndrome;179 or a more distal cause, which is compression in Guyon’s tunnel.180
Electromyography can be useful;181 and alternatively, an infiltration with a local anaesthetic may prove diagnostic.
Treatment
A diagnosis of cubital tunnel syndrome does not in itself necessitate surgery. In mild cases, patient education and avoidance of strains often leads to spontaneous cure.182
Avoidance of postural strains or pressure
The patient’s daily activities should be studied to see what causes or influences symptoms. Precipitating or aggravating postures or movements which stretch or compress the ulnar nerve should be avoided. It may be necessary to explain this in some detail to the patient. Some patients can be helped by the use of a night splint, worn for several months.183,184
Infiltration
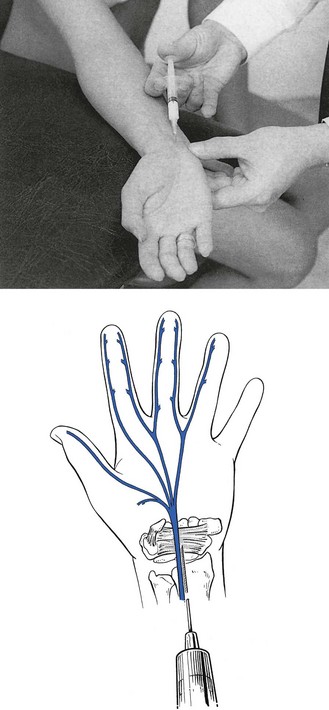
An injection of 1 ml of triamcinolone suspension about the nerve, not into it, will desensitize the nerve sheath and lead to lasting relief in those cases in which the only symptom is paraesthesia and in which conduction has not yet become impaired (Fig. 25).
Surgery
Surgical treatment is offered for more severe cases and where conservative management is deemed to have failed.185 Simple decompression involves incising longitudinally over the cubital tunnel to release the surrounding retinacular fibres. This procedure must be performed with some care, as damage to small branches of the nerve may lead to painful neuroma.186 Some authors believe that a release should be supplemented by medial epicondylectomy.187,188 This eliminates the medial epicondyle as a source of compression. The remaining options involve transposition of the ulnar nerve, in which the surgeon moves the nerve anteriorly to a subcutaneous,189,190 intramuscular191–193 or submuscular194 position. In the past decade, various authors have described endoscopic release of the ulnar nerve a safe and reliable treatment for the condition.195,196
Lesions at the wrist
Three different types of compression of the ulnar nerve at the wrist have been described: purely motor, purely sensory and a mixed form, dependent on the site of the compression.197 Consequently, the diagnosis may not be easy. Furthermore, there is the possibility of a Martin-Grüber anastomosis (see p. e96 of online chapter Applied anatomy of the elbow) which again makes the diagnosis more difficult.
The ulnar nerve, together with the ulnar artery, passes through the tunnel of Guyon. This tunnel lies between two dynamic structures, the pisiform and hamate bones, and is covered by the pisohamate ligament (Fig. 26), which is a continuation of the flexor carpi ulnaris tendon.
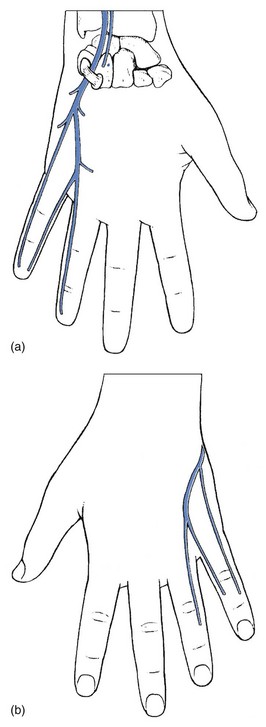
Fig 26 The ulnar nerve passes through the tunnel of Guyon (a); but the dorsal cutaneous branch (b) does not.
Proximal to the wrist, the palmar cutaneous branch arises and runs over the palmar aspect of the forearm and wrist outside the tunnel of Guyon to supply the proximal part of the ulnar side of the palm. A few centimetres more distally the dorsal cutaneous branch arises and supplies the ulnar side of the dorsum of the hand, the dorsal aspect of the fifth finger and the ulnar half of the fourth finger (see Fig. 26).
As it leaves the tunnel of Guyon, the nerve divides into a mainly sensory superficial terminal branch, which supplies the distal ulnar border of the palm of the hand and the palmar surfaces of the fifth and ulnar half of the fourth finger (Fig. 27), and a deep terminal branch, which is entirely motor and innervates nearly all of the small muscles of the hand: palmaris brevis, abductor digiti minimi, opponens digiti minimi, flexor digiti minimi brevis, dorsal interossei, palmar interossei, third and fourth lumbricals, adductor pollicis and the deep head of the flexor pollicis brevis.198
Aetiology
The cause may be either intrinsic or extrinsic. Intrinsic causes are a ganglion, the most common cause;199 a lipoma; an abnormal position of the abductor digiti minimi muscle;200 or anatomical variation in the flexor carpi ulnaris tendon.201 Extrinsic conditions are an injury with or without fractures of the pisiform or hamate bones and professional or sporting overuse (handlebar palsy).202–204
Symptoms
The symptoms may be compared with those resulting after compression of the nerve at the elbow. Because the ulnar nerve divides into a superficial and a deep branch at the wrist, the symptoms may be purely motor (deep branch) or purely sensory (superficial branch). Sensation over the dorsal aspect of the fingers remains unaltered, because the dorsal sensory branch has an origin proximal to the wrist (see Fig. 26).
Four localizations are possible:205
• Proximal to Guyon’s tunnel, at the pisiform bone. This causes compression of the superficial and deep branches with sensory and motor deficit (hypothenar and intrinsic hand muscles).
• Within Guyon’s tunnel, with compression of the deep motor branch, which results in a motor deficit of the hypothenar and intrinsic hand muscles. There is no sensory deficit.
• Distal to Guyon’s tunnel, at the hook of the hamate bone; as a result of compression of the deep palmar branch the intrinsic hand muscles are weak.
• In the palmaris brevis muscle at the distal part of Guyon’s tunnel; the superficial branch is compressed and gives rise to a purely sensory deficit.
A fifth type of compression with motor deficit of the first dorsal interosseous and the adductor pollicis muscles has been reported by Yu-Sung et al.206
Disorders of the median nerve
Anatomy
The median nerve arises from the junction of the medial and lateral cords of the brachial plexus and thus from the segments C5–T1. In the upper arm the nerve lies superficial to the brachial muscle and arches around the brachial artery. In the proximal part of the forearm the nerve leaves the artery and innervates the pronator teres, flexor carpi radialis, palmaris longus, and flexor digitorum superficialis muscles. It then passes under the bicipital aponeurosis and between the two heads of the pronator teres to enter the anterior compartment of the lower arm. Just distal to that point, it gives off the anterior interosseous (ante-brachial) nerve branch that supplies the flexor digitorum profundus, flexor pollicis longus, and pronator quadratus muscles. The nerve then courses between the flexor digitorum superficialis and profundus muscles. As the muscles change to the tendons in the lower half of the arm, the median nerve runs with the tendons of index and middle fingers to the carpal tunnel. Before passing under the flexor retinaculum and into the carpal tunnel, it gives off the superficial palmar branch. Distal to the carpal tunnel, it divides into its terminal branches to: the thenar, the radial lumbricals and the palmar aspect and the radial side of the hand and the  radial fingers (Fig. 28).
radial fingers (Fig. 28).
Innervation
There are no branches in the upper arm. Just distal to the elbow the first branches arise for the pronator teres, the flexor carpi radialis, the palmaris longus and the superficial flexor digitorum. The anterior interosseous nerve of the forearm innervates the pronator quadratus, the flexor pollicis longus and the radial half of the deep flexor digitorum. A sensory branch innervates the skin over the thenar and the radial half of the palm of the hand. After passing the carpal tunnel the digital nerves divide to supply the skin over the  radial digits and the muscles of the thenar eminence, except those innervated by the ulnar nerve (see Fig. 28).
radial digits and the muscles of the thenar eminence, except those innervated by the ulnar nerve (see Fig. 28).
Disorders
The median nerve (Table 6, Fig. 29) is the most important nerve of the hand, because it renders opposition of the thumb possible, combined with a circular pronation movement, as well as flexion of the radial fingers. Palsy of this nerve leads to total incapacity of the hand.
Lesions at the lower part of the arm and around the elbow
The median nerve can become damaged as the result of supracondylar fractures or elbow dislocation. It can also become compressed above the elbow by a supracondylar process and the ligament of Struthers, if the latter is present. Thickening or fibrosis of the bicipital aponeurosis may also cause compression. Below the elbow, the problem is most common at the point where the median nerve and its anterior interosseous branch dip between the two heads of the pronator teres. Thickening of the fascia that holds these two heads together can cause compression – the pronator teres syndrome.207,208
Pronator syndrome results from entrapment or compression of the median nerve between the humeral (superficial) and the ulnar (deep) heads of the pronator teres muscle, at the bicipital aponeurosis (lacertus fibrosus), or at the arch of the origin of the flexor digitorum superficialis (Fig. 30). Compression and entrapment may result from anatomic constraints due to congenital abnormalities in the involved tendons or muscles, such as hypertrophy of the pronator teres muscle bellies or aponeurotic prolongation of the biceps brachii muscle.209 These conditions may be clinically silent for years and then suddenly become evident after repetitive pronation–supination stress. Less common causes of pronator syndrome include post-traumatic haematoma, soft-tissue masses and prolonged external compression.
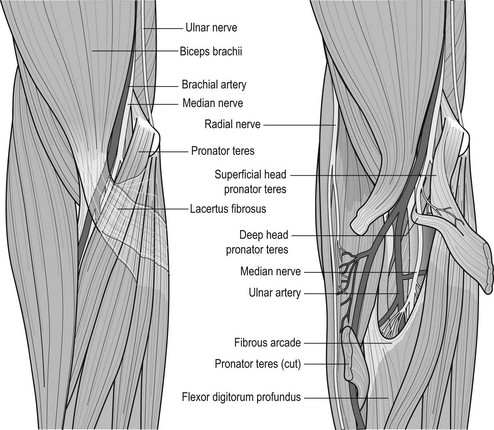
The clinical picture includes weakness of the median innervated muscles distal to the pronator teres muscle – the flexor pollicis longus and the thenar muscles. Sensory deficit is often present. Pain is certainly not the main complaint.
The following accessory tests have been described:
• A resisted pronation during thirty seconds may provoke the symptoms.
• Sustained isometric flexion of the middle finger causes the symptoms
• Tinel’s sign: percussion in the area of the pronator teres muscle.
Infiltration of steroid solution in the area of compression is usually curative. If not, surgical release is performed.
Pronator teres syndrome is probably a tunnel syndrome that is easily overestimated. The picture should be confirmed objectively by sensory and electrophysiological examination.210 When the tentative diagnosis cannot be confirmed, possible compartment syndrome or lesion of the pronator teres muscle should be considered.
Lesions at the forearm: anterior interosseous nerve
Compression of the anterior interosseous nerve – a branch of the median nerve – is known as the Kiloh–Nevin syndrome.211,212 The most frequent causes of anterior interosseous nerve syndrome are direct traumatic damage and external compression. Traumatic nerve damage may be the result of surgery, venous puncture and injection. External compression of the anterior interosseous nerve may be caused by a soft-tissue mass such as lipoma or ganglion, an accessory muscle, a vascular abnormality or cast pressure.213
Clinical findings
Typically, patients with anterior interosseous nerve syndrome experience a dull pain in the volar aspect of the proximal forearm, which sometimes worsens at night, combined with an acute onset of muscle weakness. The muscle weakness affects the thumb, the index finger, and occasionally the middle finger because the deep flexor muscles of these fingers are innervated by the anterior interosseous nerve. Since the anterior interosseous nerve does not innervate the skin, numbness is not associated with the syndrome.
Patients with anterior interosseous nerve syndrome have difficulties in writing and are not able to form an ‘O’ with the thumb and index finger. This characteristic finding, called the circle sign, is due to a lack of innervation of the flexor pollicis longus muscle and the flexor digitorum profundus muscles: the distal interphalangeal joints stay in extension during the pinch. Diagnosis must be based on clinical findings214–217 and electrodiagnostic studies.218
Lesions in the carpal tunnel
The palmar aspect of the carpus is concave and covered with the transverse carpal ligament. An osteofibrous canal, the carpal tunnel, is thus formed, of which the boundaries are the scaphoid and pisiform bones proximally and the trapezium and hamate bones distally. The canal thus lies more distally and more towards the ulnar aspect than is often thought (Fig. 31).
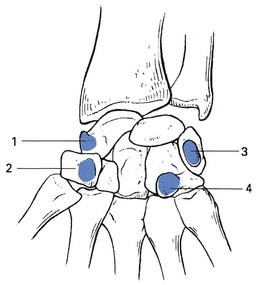
Fig 31 The boundaries of the carpal tunnel (right hand, palmar view): 1, scaphoid; 2, trapezium; 3, pisiform; 4, hamate.
Within the carpal tunnel are found the median nerve, the tendons of the flexor carpi radialis and the flexor pollicis longus, in separate sheets, and the superficial and deep flexors of the digits within a common tendon sheath (Fig. 32).
Carpal tunnel syndrome is the most common peripheral entrapment neuropathy219,220 with an incidence between 1.5 and 3.5 per 1000 subjects per year.221–223 It affects mostly women (68%) between 40 and 60 years.224
While first recognized by Sir James Paget in 1854,225 it was not until 1942 that Cyriax226 described irritation of the median nerve under the heading ‘median perineuritis’. The condition remained further unrecognized until 1946, when more detailed description was given.227,228 Full appreciation of how common the lesion is followed Phalen’s article.229
Aetiology
Clinical carpal tunnel syndrome is caused by a raised intracarpal pressure which results from an increase in content or a decrease in size of the carpal canal, or some combination of the two. The cause may either be local or systemic. On the basis of observation, two types are distinguished: a full syndrome (symptoms in the entire territory of the nerve) and a partial syndrome (symptoms in only a part of the nerve’s territory) (Box 4).
Full syndrome
Idiopathic
Half of all cases are idiopathic.230 Recent research suggests a multi-factorial cause. Ultrasound imaging of the carpal tunnel during dynamic stress testing manūuvres demonstrates notching, flattening, or compression of the nerve. The roof of the tunnel tightens and lowers at the same time the floor (flexor tendons) of the tunnel tightens and raises, thereby compressing the nerve.231,232
Traumatic
Subluxation of the lunate bone following a (possibly minor) trauma suddenly fixes the wrist in flexion, immediately followed by paraesthesia in the territory of the median nerve. After some days the patient also experiences numbness and some weeks later may even develop severe weakness of the thenar muscles.
It has been stated that occupations involving exposure to high pressure, high force, vibrating tools and repetitive work (in particular frequent flexion and extension and sustained force of the wrist) increase the risk for carpal tunnel syndrome (CTS).233,234 With respect to keyboard use, however, the frequency of CTS in computer users seems to be similar to that of the general population.235,236
Friction of the nerve may also occur after wrist fracture, especially a Colles’ fracture, as it becomes caught either by the callus or by the displaced bone.
Inflammatory
This occurs in conditions causing thickening of the transverse carpal ligament and the tendons in the carpal tunnel, such as rheumatoid arthritis.237 Gout and pseudogout are also possible causes. The former gives rise to so much swelling that the nerve becomes severely compressed; the main symptom is then cutaneous analgesia. Other causes are amyloidosis, haematoma and rubellar polyarthritis.
Endocrine
Possible causes are hypothyroidism,238 with accumulation of myxomatous deposits within the carpal tunnel;239 acromegaly;240,241 pregnancy242 (20% of pregnant women develop a carpal tunnel syndrome after the 6th month243); and menopause.
Generalized peripheral neuropathy
This can occur in patients suffering from diabetes244 or uraemia.
Partial syndromes
These occur when pressure is exerted on one or several of the most distal terminal branches of the nerve. This can be the result of an injury, incorrect use of a walking stick or a trigger finger (see p. e149 of this chapter).
History and symptoms
The condition starts in one hand, very often the dominant one, but becomes bilateral in 30% of cases. The first symptoms are pins and needles felt in the territory of the median nerve (see Figs 28 and 33): the palmar aspect of the thumb, index, middle and radial half of the ring finger, as well as the dorsal aspect of the distal phalanges of these fingers. Symptoms often are worse at night and are exacerbated by repetitive flexion and extension of the wrist, strenuous gripping, or exposure to vibration. Nocturnal paraesthesiae rarely occur as the only symptom but are mentioned more often in combination with the other complaints (see below). At onset, the symptoms may be vague and diffuse and may involve only one finger – usually the middle one. After a while, the typical distribution becomes clear.
After some months a burning wrist pain develops, which may radiate distally into the fingers and proximally to the forearm.249 The pins and needles, however, do not have this proximal reference but remain distal to the point of compression.
Slight numbness in the radial fingers is sometimes present and, therefore, mentioned by the patient but it is often only detected when sensory deficit is sought during the examination.
In some long-standing or severe cases, the patient may complain of weakness and inability to use the hand: things slip from his or her fingers without noticing (loss of grip, dropping things).
In the assessment of carpal tunnel syndrome the history is most relevant. The precision of the patient’s account very strongly implies the possibility of the presence of the syndrome. The area of paraesthesia described is exactly that of the median nerve and mention is made of the intermittent appearance and activity dependence of the symptoms.
Findings during inspection and examination
Inspection may reveal structural changes – post-fracture, deformities in rheumatoid arthritis, ganglia, bony subluxations – conditions that could be relevant when the overall clinical picture is considered.
In long-standing cases, and very occasionally early in the course of the condition, muscular atrophy of the thenar eminence may occur, involving the opponens pollicis and abductor pollicis brevis muscles.250 The lateral aspect of the thenar eminence becomes flattened and gives rise to a so-called ape hand.
The standard examination of the wrist is usually negative and some accessory tests may then be performed:
• The carpal compression test:251 the wrist is held in supination and extension. The examiner presses at the carpal tunnel while the patient actively flexes and extends his fingers. A positive test is indicated by paraesthesia in the  fingers.
fingers.
• Phalen’s test:229,252 the wrist is kept passively flexed for a minute. A positive test is indicated by pins and needles in thumb, index finger, middle finger and radial half of the ring finger (Fig. 34).
• Modified Phalen’s test:253 the wrist is held passively flexed and the thumb, index and long fingers are forcefully flexed as well.
• Tinel’s test:254 percussion of the carpal tunnel gives rise to pins and needles felt in the median nerve distribution (Fig. 35).
In longstanding and/or severe compression, some weakness of the thumb can be detected: abduction (abductor pollicis brevis), flexion (flexor pollicis brevis, superficial head) and opposition (opponens pollicis) may be weak.
The two main physical examination signs, Tinel sign and Phalen sign, have only a moderate sensitivity (20 to 70%) and specificity (70 to 83%).255,256,257 However, in combination with the typical history and localization of the symptoms, they give a useful clinical indication of the probability of a carpal tunnel syndrome. The best way to confirm the tentative diagnosis is a trial injection with triamcinolone which should ease the symptoms for at least 2 weeks.
Technical investigations
During the last decades, nerve conduction studies have been considered the gold standard test for the confirmation of diagnosis of carpal tunnel syndrome with sensitivities between 49% and 84%, and specificities between 90% and 95%.258,259 Thus, approximately 10% of patients suspected of having clinical carpal tunnel syndrome have normal electrodiagnostic studies.260 Moreover, abnormal results in a working asymptomatic population occur between 9 and 16%.261 Therefore, some authors advise the use of the clinical diagnosis for carpal tunnel syndrome as the criterion standard.262,263 For the majority of patients who are considered to have carpal tunnel syndrome on the basis of their history and physical examination alone, electrodiagnostic tests do not change the probability of diagnosing this condition to an extent that is clinically relevant.264
Attempts have been made with cross-sectional imaging of the carpal tunnel, both with CT and MRI.265 However, the sensitivity and specificity of both techniques are low (sensitivity, 23%–96%; specificity, 39%–87%), and for this reason they do not play a role in the clinical assessment of carpal tunnel syndrome.266 Nevertheless, MR imaging does have clinical utility when the cause of carpal tunnel syndrome is a neoplasm (e.g. neurofibroma), arthritis, or a congenital anomaly and in evaluating the postoperative wrist.267,268
High-resolution sonography is a low-cost alternative to MRI, and has gained increasing popularity.269 Sonography measures the cross-sectional area of the median nerve and bowing/flattening of the flexor retinaculum.270 There seems to be a high degree of correlation between the US findings and the nerve conduction studies in diagnosing carpal tunnel syndrome.271
Diagnostic infiltration
A much simpler, and very reliable, diagnostic approach is the infiltration of 20 mg of triamcinolone suspension into the carpal tunnel. If diagnosis is right, all symptoms should disappear for at least a few weeks. When symptoms have not disappeared some days after the injection, the diagnosis must be reconsidered.
Differential diagnosis
Carpal tunnel syndrome must be differentiated from a cervical disc protrusion that compresses a nerve root and from thoracic outlet syndrome with compression of a part of the brachial plexus. Both are often difficult.
When distal paraesthesiae are the result of a cervical disc lesion, the symptoms usually come and go in an erratic fashion during the day as well as at night. They are transient and not particularly activity related. The distribution within the fingers is related to a dermatome, but the patient cannot localize the paraesthesia exactly. They are preceded and accompanied by severe root pain and often followed by segmental motor and/or sensory deficit. On examination of the cervical spine, a partial articular pattern is found. The symptoms disappear spontaneously in the course of a few weeks to a few months (see pp. 152–157).
In the early stage of thoracic outlet syndrome, pins and needles are strictly nocturnal and wake the patient – usually a middle-aged woman – after some hours’ sleep as a result of the decompression of the nerve. The paraesthesia are felt in all the fingers and do not have any particular distribution. Decompression tests of the thoracic outlet are positive (see p. e122 of this chapter and Ch. 2).
Other differential diagnoses are cervical myelopathy, anterior horn lesions, polyneuropathies, myopathies and arthrosis of the trapezium–first metacarpal joint.
Treatment
Treatment is conservative and consists of one or more injections into the carpal tunnel. Surgery is called for in refractory or recurrent cases.
Wrist splint
Splinting with the wrist in the neutral position, especially at night, leads to good but possibly only temporary results in about 70% of patients.272,273
More recent studies show best results with a full-time splint.274
Injection
As a diagnosis of carpal tunnel syndrome can be made in spite of a negative examination, it remains provisional until therapeutic confirmation has been obtained. Relief, even if it is only temporary, after injection with triamcinolone acetonide is diagnostic. If paraesthesia is not relieved by injection, the diagnosis must be wrong. If the symptoms do not reappear for several months or years, a later recurrence can be treated with a further injection.
The patient sits next to the couch. The physician stands medial to the affected hand, that lies palm upwards on the couch. The wrist is held in 45° of extension. The proximal border of the carpal tunnel (pisiform and scaphoid) and the palmar tendons of the wrist are easily detectable in this position. A 2 ml syringe is filled with 20 mg triamcinolone and fitted to a 5 cm needle. The tip of the needle is inserted between the tendons (usually ulnar of the palmaris longus) at a point 2 cm proximal to the proximal border of the carpal tunnel and inserted in the direction of the base of the fourth metacarpal bone. It slips, without resistance, between the tendons and under the transverse ligament into the carpal tunnel (Fig. 36). At 4 cm depth, the needle lies at the distal aspect of the carpal tunnel. Some fluid is injected and no resistance or painful sensation should be felt. The needle is then slowly withdrawn while the syringe is further emptied.
All cases of carpal tunnel syndrome respond immediately,275 but 60% recur within 3 to 6 months and at 2 years only 8% remain cured.276 Several studies have demonstrated that for the first 3 months, local injections with steroids are equally good or better than surgical decompression for the symptomatic relief of mild carpal tunnel syndrome.277,278–281 However, recurrences after injections are frequent282,283 and, although steroid injections are safe and effective for temporary relief, most patients will eventually require surgery for long-term control of their symptoms.284 We advise that if the symptoms recur more than 6 weeks after the injection, one or two further attempts may be made. When the result is still not sufficient or the recurrence is too rapid – within 6 weeks, or more than twice in 6 months – surgical treatment is required (Fig. 37).
Cases with severe symptoms and evidence of motor atrophy respond poorly.
Surgery
Carpal tunnel release is one of the most common surgical procedures with an annual incidence in the US of 134 per 100 000.285 Although carpal tunnel release is an effective treatment, supported by high-quality evidence,286,287 it has several disadvantages, including surgery-related pain and hand weakness.288,289 In addition, surgery is associated with direct and indirect costs related to work absence.290 Therefore, patients with mild symptoms should be treated first with steroid injections. Surgery is indicated in the case of rapid or frequent recurrence291,292 and in those patients who show objective neurologic deficit.293–295
The two major types of surgery are open carpal tunnel release and endoscopic carpal tunnel release (ECTR). Regardless of selection of these treatment options, the most important aspect is complete division of the flexor retinaculum. The long-term results of endoscopic release are similar to those of open release, but the former leads to quicker functional recovery.296–298 Endoscopic release was invented to address the potential complications of the open release by using smaller incisions placed away from the middle of the palm.299,300 It is assumed that preservation of the superficial fascia and adipose tissue over the flexor retinaculum allows faster recovery of grip strength, less scar tenderness and pillar pain, and earlier return to work.301 However, the decision to perform ECTR is influenced by the surgeon’s experience and patient factors, including occupation, socioeconomic status, and preference.302
Partial syndrome
Distal to the carpal tunnel the common palmar digital nerve divides into terminal motor and sensory palmar digital branches. In the hand one of these can become compressed, with the result that only part of the territory of the median nerve is involved. There are a number of possible causes.
Traumatic
As the result of a direct blow, usually a fall on the hand, the sensory palmar digital branch to the thumb at the level of its carpometacarpal joint may be bruised. The symptoms are painful pins and needles in the thumb only and there is little tendency to spontaneous cure.
‘Stick palsy’
In elderly people, the sensory palmar digital branches to the index and middle fingers may become compressed in the palm of the hand, just distal to the carpal tunnel, by incorrect use of a walking stick. This results in pins and needles, felt in these two fingers. Instruction in how to use a walking stick correctly is given.
Swelling on a digital flexor tendon
A trigger lesion that has formed on the proximal part of a flexor tendon in the palm of the hand, just distal to the carpal tunnel, may rarely cause compression of the branch of the median nerve that supplies the middle and ring fingers and give rise to pins and needles at the adjacent surfaces of these two digits. Infiltration or surgery are the possible therapeutic measures.
Disorders of the musculocutaneous nerve
Anatomy
The musculocutaneous nerve takes origin in the lateral cord of the brachial plexus and contains fibres from C5 to C7. It pierces the coracobrachialis muscle and descends in the anterior compartment of the arm between the biceps and brachialis muscles. It runs lateral to the distal biceps tendon and then continues as the lateral cutaneous nerve of the forearm (Fig. 38).
Innervation
The musculocutaneous nerve supplies the coracobrachialis, biceps and brachialis muscles. The lateral cutaneous nerve of the forearm innervates the skin at the anterolateral aspect of the forearm.
A lesion of the musculocutaneous nerve is rare and occurs as the result of an injury in the upper arm. This causes motor deficit with weakness of the flexors of the elbow and sensory deficit over the radial aspect of the forearm. When the lesion is at the forearm, it involves the sensory branch – the lateral cutaneous nerve of the forearm – and leads to a similar sensory deficit. This sometimes occurs after a paravenous injection.303
References
1. Teboul, F, Bizot, P, Kakkar, R, Sedel, L, Surgical management of trapezius palsy. J Bone Joint Surg 2004; 86:1884–1890. ![]()
2. Christoferson, LA, Leech, RW, Grossman, M, Intracranial neurilemoma of the spinal accessory nerve. Surg Neurol 1982; 18:18–20. ![]()
3. Ohkawa, M, Fujiwara, N, Takashima, H, et al, Radiologic manifestation of spinal accessory neurinoma: a case report. Radiat Med 1996; 14:269–273. ![]()
4. Kaye, AH, Jugular foramen schwannomas. J Neurosurg 1984; 60:1045–1053. ![]()
5. Chong, VF, Fan, YF, Jugular foramen involvement in nasopharyngeal carcinoma. J Laryngol Otol 1996; 110:987–990. ![]()
6. King, RJ, Motta, G, Iatrogenic spinal accessory nerve palsy. Ann Roy Coll Surg Engl 1983; 65:35–37. ![]()
7. Berry, H, MacDonald, EA, Mrazek, AC, Accessory nerve palsy: a review of 23 cases. Can J Neurol Sci 1991; 18:337–341. ![]()
8. London, J, London, NJ, Kay, SP, Iatrogenic accessory nerve injury. Ann Roy Coll Surg Engl 1996; 78:146–150. ![]()
9. Matz, PG, Barbaro, NM, Diagnosis and treatment of iatrogenic spinal accessory nerve injury. Ambulatory Surg. 1996;62(8):682–685. ![]()
10. Nakamichi, K, Tachibana, S, Iatrogenic injury of the spinal accessory nerve. Results of repair. J Bone Joint Surg. 1998;80A(11):1616–1621. ![]()
11. Wiater, JM, Bigliani, LU, Spinal accessory nerve injury. Clin Orthop Rel Res 1999; 368:5–16. ![]()
12. Salerno, G, Cavaliere, M, Foglia, A, et al, The 11th nerve syndrome in functional neck dissection. Laryngoscope. 2002;112(7 Pt 1):1299–1307. ![]()
13. Kizilay, A, Kalcioglu, MT, Saydam, L, et al, A new shoulder orthosis for paralysis of the trapezius muscle after radical neck dissection: a preliminary report. Eur Arch Otorhinolaryngol. 2006;263(5):477–480. ![]()
14. Prim, MP, De Diego, JI, Verdaguer, JM, et al, Neurological complications following functional neck dissection. Eur Arch Otorhinolaryngol. 2006;263(5):473–476. ![]()
15. Shone, GR, Yardley, MP, An audit into the incidence of handicap after unilateral radical neck dissection. J Laryngol Otol 1991; 105:760–762. ![]()
16. Williams, WW, Twyman, RS, Donell, ST, Birch, R, The posterior triangle and the painful shoulder: spinal accessory nerve injury. Ann Roy Coll Surg Engl 1996; 78:521–525. ![]()
17. Remmler, D, Byers, R, Sheetz, J, et al, A prospective study of shoulder disability resulting from radical and modified neck dissections. Head Neck Surg 1986; 8:280–286. ![]()
18. Bigliani, JU, Compito, CA, Duralde, XA, Wolfe, IN, Transfer of the levator scapulae, rhomboid major, and rhomboid minor for paralysis of the trapezius. J Bone Joint Surg 1996; 78:1534–1540. ![]()
19. Williams, WW, Donell, ST, Twymann, RS, Birch, R. The posterior triangle and the painful shoulder. Ann R Coll Surg Engl. 1996; 78:521–525.
20. Kelley, MJ, Kane, TE, Leggin, BG, Spinal accessory nerve palsy: associated signs and symptoms. J Orthop Sports Phys Ther. 2008;38(2):78–86. ![]()
21. Friedenberg, SM, Zimprich, T, Harper, CM, The natural history of long thoracic and spinal accessory neuropathies. Muscle Nerve. 2002;25(4):535–539. ![]()
22. Petrera, JE, Trojaborg, W, Conduction studies along the accessory nerve and follow-up of patients with trapezius palsy. J Neurol Neurosurg Psychiatry 1984; 47:630–636. ![]()
23. Wiater, JM, Bigliani, LU, Spinal accessory nerve injury. Clin Orthop Relat Res 1999; 368:5–16. ![]()
24. Volpin, G, Langer, R, Stein, H, Complete infraclavicular brachial plexus palsy with occlusion of axillary vessels following anterior dislocation of the shoulder joint. J Orthop Trauma 1990; 4:121–123. ![]()
25. Travlos, J, Goldberg, I, Boome, RS, Brachial plexus lesions associated with dislocated shoulders. J Bone Joint Surg 1990; 72B:68–71. ![]()
26. Hansky, B, Murray, E, Minami, K, Korfer, R, Delayed brachial plexus paralysis due to subclavian pseudoaneurysm after clavicular fracture. Eur J Cardiothor Surg 1993; 7:497–498. ![]()
27. Dyck, PJ, Thomas, PK, Lambert, EH, Bunge, R. Peripheral Neuropathy, 2nd ed. Philadelphia: Saunders; 1984.
28. Pitz, CC, de la Rivière, AB, van Swieten, HA, Duurkens, VA, Lammers, JW, van den Bosch, JM, Surgical treatment of Pancoast tumours. Eur J Cardiothorac Surg. 2004;26(1):202–208. ![]()
29. Moore, J. Thoracic outlet syndrome. Experience in a metropolitan hospital. Clin Orthop Rel Res. 1986; 207:29–30.
30. Atasoy, E, Thoracic outlet syndrome: Anatomy. Hand Clin 2004; 20:7–14. ![]()
31. Nichols, H, Anatomic structures of the thoracic outlet. Clin Orthop Rel Res 1986; 207:13–20. ![]()
32. Cyriax, J. Textbook of Orthopaedic Medicine, vol I, Diagnosis of Soft Tissue Lesions, 8th ed. London: Baillière Tindall; 1982.
33. Riddell, D, Smith, B, Thoracic and vascular aspects of thoracic outlet syndrome. Clin Orthop Rel Res 1986; 207:31–36. ![]()
34. Ruckley, C, Thoracic outlet syndrome. BMJ 1983; 287:447–448. ![]()
35. Bauwens, F, Duprez, D, Clement, D. Thoracic outlet syndrome. Med Trends. 1990; 5:252–257.
36. Stewart, JD. Focal Peripheral Neuropathies, 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2000.
37. Nichols, AW, Diagnosis and management of thoracic outlet syndrome. Curr Sports Med Rep 2009; 8:240–249. ![]()
38. Wilbourn, AJ, Thoracic outlet syndrome: thoracic outlet syndrome is overdiagnosed. Muscle Nerve 1999; 22:130–138. ![]()
39. Dawson, DH, Hallett, M, Wilbourn, AJ, et al. Entrapment Neuropathies, 3rd ed. Philadelphia: Lippincott-Raven; 1999.
40. Gilliatt, R, Thoracic outlet syndromesDyck PJ, Thomas PK, Lambert EH, Bunge R, eds. Peripheral Neuropathy. 2nd ed. Saunders, Philadelphia, 1984:1409–1424. ![]()
41. Bateman, J. Neurological pain conditions affecting the shoulder. Clin Orthop Rel Res. 1983; 173:48.
42. Fechter, J, Kuschner, S, The thoracic outlet syndrome. Orthopedics. 1993;16(11):1243–1251. ![]()
43. Pecina, M, Krmpotic-Nemanic, J, Markiewitz, A. Tunnel Syndromes. Boca Raton: CRC; 1991.
44. Hood, DB, Kuehne, J, Yellin, AE, Weaver, FA, Vascular complications of thoracic outlet syndrome. Am J Surg 1997; 63:913–917. ![]()
45. Green, RM, Vascular manifestations of the thoracic outlet syndrome. Sem Vasc Surg 1998; 11:67–76. ![]()
46. McCleery, R, Kesterson, J, Kirtley, J, Love, R, Subclavius and anterior scalenus muscle compression as a cause of intermittent obstruction of the subclavian vein. Ann Surg 1951; 133:588. ![]()
47. Etheredge, S, Wilbur, B, Stoney, R. Thoracic outlet syndrome. Am J Surg. 1979; 138:175.
48. Sanders, RJ, Haug, C, Subclavian vein obstruction and thoracic outlet syndrome: a review of etiology and management. Ann Vasc Surg 1990; 4:397–410. ![]()
49. Wood, V, Twito, R, Verska, J, Thoracic outlet syndrome. The results of first rib resection in 100 patients. Orthop Clin North Am. 1988;19(1):131–146. ![]()
50. Brantigan, CO, Roos, DB, Diagnosing thoracic outlet syndrome. Hand Clin 2004; 20:27–36. ![]()
51. Parziale, JR, Akelman, E, Weiss, AP, Green, A, Thoracic outlet syndrome. Am J Orthop. 2000;29(5):353–360. ![]()
52. Adson, A, Surgical treatment for symptoms produced by cervical ribs and the scalene anticus muscle. Surg Gynecol Obstet 1947; 85:687. ![]()
53. Roos, DB, Congenital anomalies associated with thoracic outlet syndrome: anatomy, symptoms, diagnosis, and treatment. Am J Surg 1976; 132:771–778. ![]()
54. Rayan, GM, Jensen, C, Thoracic outlet syndrome: provocative examination maneuvers in a typical population. J Shoulder Elbow Surg 1995; 4:113–117. ![]()
55. Plewa, MC, Delinger, M, The false-positive rate of thoracic outlet syndrome shoulder maneuvers in healthy subjects. Acad Emerg Med 1998; 5:337–342. ![]()
56. Aminoff, MJ, Olney, RK, Parry, GJ, Raskin, NH, Relative utility of different electrophysiologic techniques in the evaluation of brachial plexopathies. Neurology 1988; 38:546–550. ![]()
57. Tolson, TD, ‘EMG’ for thoracic outlet syndrome. Hand Clin 2004; 20:37–42. ![]()
58. Painful shoulder and the reflex sympathetic dystrophy syndrome. In: Kozin F, ed. Arthritis and Allied Conditions. 9th ed. Philadelphia: Lea & Febiger; 1979:1091–1120.
59. Nakatsuchi, Y, Saitoh, S, Hosaka, M, Matsuda, S, Conservative treatment of thoracic outlet syndrome using an orthosis. J Hand Surg 1995; 20B:34–38. ![]()
60. Hawkes, C, Neurosurgical considerations in thoracic outlet syndrome. Clin Orthop Rel Res 1986; 207:24–28. ![]()
61. Luoma, A, Nelems, B, Thoracic outlet syndrome: thoracic surgery perspective. Neurosurg Clin North Am 1991; 2:187–226. ![]()
62. Sanders, RJ, Results of the surgical treatment for thoracic outlet syndrome. Sem Thoracic Cardiovasc Surg 1996; 8:221–228. ![]()
63. Hempel, GK, Shutze, WP, Anderson, F, Bukhari, HI, 770 consecutive supraclavicular first rib resections for thoracic outlet syndrome. Ann Vasc Surg 1996; 10:456–463. ![]()
64. Wilbourn, AJ, Thoracic outlet syndrome: a plea for conservatism. Neurosurg Clin North Am 1991; 2:235–245. ![]()
65. Cherington, M, Cherington, C, Thoracic outlet syndrome: reimbursement patterns and patient profiles. Neurology 1992; 42:943–945. ![]()
66. Parsonage, MJ, Turner, JWA, Neuralgic amyotrophy: the shoulder-girdle syndrome. Lancet 1948; 1:973–978. ![]()
67. Turner, JWA, Parsonage, MJ, Neuralgic amyotrophy (paralytic brachial neuritis): with special reference to prognosis. Lancet 1957; 2:209–212. ![]()
68. McCarty, EC, Tsairis, P, Warren, RF, Brachial neuritis. Clin Orthop Rel Res 1999; 368:37–43. ![]()
69. Cusimano, MD, Bilbao, JM, Cohen, SM, Hypertrophic brachial plexus neuritis: a pathological study of two cases. Ann Neurol 1988; 24:615–622. ![]()
70. Suarez, GA, Giannini, C, Bosch, EP, et al, Immune brachial plexus neuropathy: suggestive evidence of an inflammatory-immune pathogenesis. Neurology 1996; 46:559–561. ![]()
71. Zeharia, A, Mukamel, M, Frishberg, Y, Weitz, R, Mimouni, M, Benign plexus neuropathy in children. J Pediatr 1990; 116:276–278. ![]()
72. Koster, JB, Images in clinical medicine. Neuralgic amyotrophy. N Engl J Med. 2010;362(24):2304. ![]()
73. Klein, CJ, Dyck, PJB, Friedenberg, SM, et al, Inflammation and neuropathic attacks in hereditary brachial plexus neuropathy. J Neurol Neurosurg Psychiatry 2002; 73:45–50. ![]()
74. van Alfen, N, Gabreels-Festen, AA, Ter Laak, HJ, et al, Histology of hereditary neuralgic amyotrophy. J Neurol Neurosurg Psychiatry 2005; 76:445–447. ![]()
75. van Alfen, N, van Engelen, BG, The clinical spectrum of neuralgic amyotrophy in 246 cases. Brain. 2006;129(Pt 2):438–450. ![]()
76. Misamore, GW, Lehman, DE, Parsonage–Turner syndrome (acute brachial neuritis). J Bone Joint Surg 1996; 78A:1405–1408. ![]()
77. Drake, RL, Vogl, W, Mitchell, AWM. Gray’s anatomy for students. Philadelphia: Elsevier Inc; 2005.
78. Wiater, JM, Flatow, EL, Long thoracic nerve injury. Clin Orthop Relat Res 1999; 368:17–27. ![]()
79. Kauppila, LI, Vastamaki, M, Iatrogenic serratus anterior paralysis: long-term outcome in 26 patients. Chest 1996; 109:31–34. ![]()
80. Wilmot, C, Watemberg, S, Landau, O, Litwin, D, Of balloon axilloscopy and avoidance of iatrogenic injury to the long thoracic nerve. Arch Surg 1997; 132:1121–1124. ![]()
81. Mumenthaler, M. Neurology, 3rd ed. New York: Thieme; 1990.
82. Schultz, JS, Leonard, JAJ, Long thoracic neuropathy from athletic activity. Arch Phys Med Rehabil 1992; 73:87–90. ![]()
83. Packer, GJ, McLatchie, GR, Bowden, W, Scapula winging in a sports injury clinic. Br J Sports Med 1993; 27:90–91. ![]()
84. Hester, P, Caborn, D, Nyland, J, Cause of long thoracic nerve palsy: a possible dynamic fascial sling cause. J Shoulder Elbow Surg 2000; 9:31–35. ![]()
85. Ebraheim, NA, Lu, J, Porshinsky, B, Heck, BE, Yeasting, RA, Vulnerability of the long thoracic nerve: an anatomic study. J Shoudler Elbow Surg 1998; 7:458–561. ![]()
86. Gregg, JR, Labosky, D, Harty, M, Lotke, P, Ecker, M, DiStefano, V, Das, M, Serratus anterior paralysis in the young athlete. J Bone Joint Surg 1979; 61:825–832. ![]()
87. Foo, CL, Swann, M, Isolated paralysis of the serratus anterior: a report of 20 cases. J Bone Joint Surg 1983; 65:552–556. ![]()
88. Warner, JJP, Navarro, RA, Serratus anterior dysfunction: recognition and treatment. Clin Orthop Relat Res 1998; 349:139–148. ![]()
89. Paljarvi, L, Partanen, J, Biting palsy of the accessory nerve. J Neurol Neurosurg Psychiatry 1980; 43:744–746. ![]()
90. Goodman, CE, Kenrick, MM, Blum, MV, Long thoracic nerve palsy: a follow-up study. Arch Phys Med Rehabil 1975; 56:352–355. ![]()
91. Novak, CB, Mackinnon, SE, Surgical treatment of a long thoracic nerve palsy. Ann Thorac Surg 2002; 73:1643–1645. ![]()
92. Connor, PM, Yamaguchi, K, Manifold, SG, et al, Split pectoralis major transfer for serratus anterior palsy. Clin Orthop Rel Res 1997; 341:134–142. ![]()
93. Rengachary, SS, Burr, D, Lucas, S, Hassanein, KM, Mohn, MP, Matzke, H, Suprascapular entrapment neuropathy: a clinical, anatomical and comparative study, part II: anatomical study. Neurosurgery 1979; 5:447–451. ![]()
94. Sunderland, S. Nerves and Nerve Injuries, 2nd ed. New York, NY: Churchill Livingstone; 1978.
95. Fehrman, DA, Orwin, JF, Jennings, RM, Suprascapular nerve entrapment by ganglion cysts: a report of six cases with arthroscopic findings and review of the literature. Arthroscopy 1995; 11:727–734. ![]()
96. Moore, TP, Fritts, HM, Quick, DC, Buss, DD, Suprascapular nerve entrapment caused by supraglenoid cyst compression. J Shoulder Elbow Surg 1997; 6:455–462. ![]()
97. Kiss, G, Komar, J, Suprascapular nerve compression at the spinoglenoid notch. Muscle Nerve 1990; 13:556–557. ![]()
98. Holzgraefe, M, Kukowski, B, Eggert, S, Prevalence of latent and manifest suprascapular neuropathy in high-performance volleyball players. Br J Sports Med 1994; 28:177–178. ![]()
99. Van Zandijcke, M, Casselman, J, Suprascapular nerve entrapment at the spinoglenoid notch due to a ganglion cyst. J Neurol Neurosurg Psychiatry. 1999;66(2):245. ![]()
100. Gaskin, CM, Helms, CA, Parsonage-Turner syndrome: MR imaging findings and clinical information of 27 patients. Radiology. 2006;240(2):501–507. ![]()
101. De Laat, EA, Visser, CP, Coene, LN, Pahlplatz, PV, Tavy, DL, Nerve lesions in primary shoulder dislocations and humeral neck fractures: a prospective clinical and EMG study. J Bone Joint Surg 1994; 76B:381–383. ![]()
102. Moore, TP, Fritts, HM, Quick, DC, Buss, DD, Suprascapular nerve entrapment caused by supraglenoid cyst compression. J Shoulder Elbow Surg 1997; 6:455–462. ![]()
103. Witvrouw, E, Cools, A, Lysens, R, et al, Suprascapular neuropathy in volleyball players. Br J Sports Med. 2000;34(3):174–180. ![]()
104. Ferretti, A, Cerullo, G, Russo, G, Suprascapular neuropathy in volleyball players. J Bone Joint Surg Am 1987; 69:260–263. ![]()
105. Filler, AG, Kliot, M, Howe, FA, et al, Application of magnetic resonance neurography in the evaluation of patients with peripheral nerve pathology. J Neurosurg 1996; 85:299–308. ![]()
106. Martin, SD, Warren, RF, Martin, TL, et al, Suprascapular neuropathy. Results of non-operative treatment. J Bone Joint Surg Am 1997; 79:1159–1165. ![]()
107. Post, M, Mayer, J, Suprascapular nerve entrapment: diagnosis and treatment. Clin Orthop 1987; 223:126–136. ![]()
108. Callahan, JD, Scully, TB, Shapiro, SA, Worth, RM, Suprascapular nerve entrapment: a series of 27 cases. J Neurosurg 1991; 74:893–896. ![]()
109. Antoniadis, G, Richter, HP, Rath, S, Braun, V, Moese, G, Suprascapular nerve entrapment: experience with 28 cases. J Neurosurg 1996; 85:1020–1025. ![]()
110. Aval, SM, Durand, P, Jr., Shankwiler, JA, Neurovascular injuries to the athlete’s shoulder: part II. J Am Acad Orthop Surg 2007; 15:281–289. ![]()
111. Burkhead, WZ, Scheinberg, RR, Box, G, Surgical anatomy of the axillary nerve. J Shoulder Elbow Surg 1992; 1:31–36. ![]()
112. Pasila, M, Jaroma, H, Kaviluoto, O, Sundholm, A, Early complications of primary shoulder dislocations. Acta Orthop Scand 1978; 49:260–263. ![]()
113. Berry, H, Bril, V, Axillary nerve palsy following blunt trauma to the shoulder region: a clinical and zlectrophysiological review. J Neurol Neurosurg Psychiatry 1982; 45:1027–1032. ![]()
114. Mcllveen, SJ, Duralde, XA, D’Alessandro, DF, Bigliani, LU, Isolated nerve injuries about the shoulder. Clin Orthop 1994; 306:54–63. ![]()
115. Hoskins, WT, Pollard, HP, McDonald, AJ, Quadrilateral space syndrome: a case study and review of the literature. Br J Sports Med. 2005;39(2):e9. ![]()
116. Linker, CS, Helms, CA, Fritz, RC, Quadrilateral space syndrome: findings at MR imaging. Radiology 1993; 188:675–676. ![]()
117. Bonnard, C, Anastakis, DJ, van Melle, G, Narakas, AO, Isolated and combined lesions of the axillary nerve: a review of 146 cases. J Bone Joint Surg Br 1999; 81:212–217. ![]()
118. Boileau, P, Richou, J, Lisai, A, Chuinard, C, Bicknell, RT, The role of arthroscopy in revision of failed open anterior stabilization of the shoulder. Arthroscopy. 2009;25(10):1075–1084. ![]()
119. Cyriax, J. Textbook of Orthopaedic Medicine, vol I, Diagnosis of Soft Tissue Lesions, 8th ed. London: Baillière Tindall; 1982.
120. Staples, OS, Watkins, AL. Full active abduction in traumatic paralysis of the deltoid. J Bone Joint Surg. 1943; 25:85–89.
121. Steinman, SP, Moran, EA, Axillary nerve injury: diagnosis and treatment. J Am Acad Orthop Surg 2001; 9:328–335. ![]()
122. Poddar, SB, Gitelis, S, Heydemann, PT, Piasecki, P, Bilateral predominant radial nerve crutch palsy: a case report. Clin Orthop Rel Res 1993; 297:245–246. ![]()
123. Raikin, S, Froimson, MI, Bilateral brachial plexus compressive neuropathy (crutch palsy). J Orthop Trauma 1997; 11:136–138. ![]()
124. Ogawa, K, Ui, M, Humeral shaft fracture sustained during arm wrestling: report on 30 cases and review of the literature. J Trauma 1997; 42:243–246. ![]()
125. Ogawa, K, Yoshida, A, Throwing fracture of the humeral shaft: an analysis of 90 patients. Am J Sports Med 1998; 26:242–246. ![]()
126. Hazani, R, Engineer, NJ, Mowlavi, A, Neumeister, M, Lee, WP, Wilhelmi, BJ, Anatomic landmarks for the radial tunnel. Eplasty 2008; 8:e37. ![]()
127. Fröhse, F, Frankel, M. Die Muskel des menschlichen Armes. In: Bardelben’s Handbuch der Anatomie des Menschen. Jena: Fisher; 1908.
128. Lichter, R, Jacobson, T, Tardy palsy of the posterior interosseous nerve with Monteggia fracture. J Bone Joint Surg 1975; 57A:124. ![]()
129. Olney, BW, Menelaus, MB, Monteggia and equivalent lesions in childhood. J Pediatr Orthop 1989; 9:219–223. ![]()
130. Morris, AH, Irreducible Monteggia lesion with radial nerve entrapment. J Bone Joint Surg 1974; 56A:1744. ![]()
131. Sjostrand, J, McLean, WG, Frizell, M. The application of axonal transport studies to peripheral nerve problems. In: Omer G, Jr., Spinner M, eds. Management of Peripheral Nerve Problems. Philadelphia: Saunders, 1980.
132. Malipeddi, A, Reddy, VR, Kallarackal, G, Posterior interosseous nerve palsy: an unusual complication of rheumatoid arthritis: case report and review of the literature. Semin Arthritis Rheum. 2010;40(6):576–579. ![]()
133. Wu, KT, Jordon, FR, Eckert, C, Lipoma: a cause of paralysis of the deep radial nerve. Surgery 1974; 75:790. ![]()
134. Werner, CO, Paralysis of the posterior interosseous nerve caused by tumour: brief report. J Bone Joint Surg 1987; 69B:670–671. ![]()
135. Salama, H, Kumar, P, Bastawrous, S, Posterior interosseous nerve palsy caused by parosteal lipoma: a case report. Case Report Med 2010; . ![]()
136. Spinner, M, The arcade of Fröhse and its relationship to posterior interosseous nerve paralysis. J Bone Joint Surg 1968; 50B:808. ![]()
137. Goldman, S, Honet, JC, Sobel, R, Goldstein, AS, Posterior interosseous nerve palsy in the absence of trauma. Arch Neurol 1969; 21:435–441. ![]()
138. Bryan, FS, Miller, LS, Panijayanond, P, Spontaneous paralysis of the posterior interosseous nerve. A case report and review of the literature. Clin Orthop Rel Res 1971; 80:9–12. ![]()
139. Nielsen, HO, Posterior interosseous nerve paralysis caused by fibrous band compression at the supinator muscle. A report of four cases. Acta Orthop Scand 1976; 47:304–307. ![]()
140. De Zanche, L, Negrin, P, Fardin, P, Carteri, A, Paralysis of the deep branch of the radial nerve due to entrapment neuropathy. Eur Neurol 1978; 17:56–58. ![]()
141. Hagert, CG, Lundborg, G, Hansen, T, Entrapment of the posterior interosseous nerve. Scand J Plast Reconstr Surg 1977; 11:205–212. ![]()
142. Winckworth, CE. Lawn-tennis elbow. BMJ. 1883; 2:708.
143. Roles, NC, Maudsley, RH, Radial tunnel syndrome: resistant tennis elbow as a nerve entrapment. J Bone Joint Surg 1972; 54B:499–508. ![]()
144. Capener, N, The vulnerability of the posterior interosseous nerve of the forearm. A case report and an anatomical study. J Bone Joint Surg 1966; 48B:770. ![]()
145. Lister, GD, Belsole, RB, Kleinert, HE, The radial tunnel syndrome. J Hand Surg 1979; 4A:52. ![]()
146. Barnum, M, Mastey, RD, Weiss, AP, Akelman, E, Radial tunnel syndrome. Hand Clin 1996; 12:679–688. ![]()
147. Ritts, GD, Wood, MB, Lindscheid, RL, Radial tunnel syndrome: a ten year surgical experience. Clin Orthop Rel Res 1987; 219:201–205. ![]()
148. Minami, Y, Yamazaki, J, Kato, S, Lateral elbow pain syndrome and entrapment of the radial nerve. Nippon Seikeigeka Gakkai Zasshi. 1992;66(4):222–227. ![]()
149. Kopell, HP, Thompson, WAL. Peripheral Entrapment Neuropathies. Baltimore: Williams & Wilkins; 1963.
150. Matthews, PBC. Mammalian Muscle Receptors and Their Central Actions. London: Edward Arnold; 1972.
151. Werner, CO, Lateral elbow pain and posterior interosseous nerve entrapment. Acta Orthop Scand. 1979;174(suppl):352–355. ![]()
152. De Smet, L, Van Raebroeckx, T, Van Ransbeeck, H, Radial tunnel release and tennis elbow: disappointing results? Acta Orthop Belg. 1999;65(4):510–513. ![]()
153. Rosenbaum, R, Disputed radial tunnel syndrome. Muscle Nerve. 1999;22(7):960–967. ![]()
154. Stewart, JD. Focal Peripheral Neuropathies, 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2000.
155. Van Rossum, J, Buruma, OJ, Kamphuisen, HA, Tennis elbow: a radial tunnel syndrome. J Bone Joint Surg 1978; 60B:197–198. ![]()
156. Rosén, I, Werner, CO, Neurophysiological investigation of posterior interosseous nerve entrapment causing lateral elbow pain. Electroencephalogr Clin Neurophysiol 1980; 50:125–133. ![]()
157. Verhaar, J, Spaans, F, Radial tunnel syndrome: an investigation of compression neuropathy as a possible cause. J Bone Joint Surg 1991; 73A:539–543. ![]()
158. Appel, H, Handcuff neuropathy. Neurology 1991; 41:955. ![]()
159. Cook, AA, Handcuff neuropathy among U.S. prisoners of war from Operation Desert Storm. Mil Med 1993; 158:253–254. ![]()
160. Panas, AL. Sur une cause peu connue de paralysie du nerf cubital. Arch Gen Med. 1878; 2:5.
161. Lazaro, L, 3rd., Ulnar nerve instability: ulnar nerve injury due to elbow flexion. Southern Med J. 1977;70(1):36–40. ![]()
162. Childress, HM, Recurrent ulnar-nerve dislocation at the elbow. Clin Orthop Rel Res 1975; 108:168–173. ![]()
163. Prietto, CA, Supracondylar fractures of the humerus. J Bone Joint Surg 1979; 51A:130. ![]()
164. Minami, A, Sugawara, M, Humeral trochlear hypoplasia secondary to epiphyseal injury as a cause of ulnar nerve palsy. Clin Orthop Rel Res 1988; 228:227. ![]()
165. Darowish, M, Lawton, JN, Evans, PJ, Q:What is cell phone elbow, and what should we tell our patients? Cleve Clin J Med. 2009;76(5):306–308. ![]()
166. Feindel, W, Stratford, J, The role of the cubital tunnel in tardy ulnar palsy. Can J Surg 1958; 1:287. ![]()
167. Osborne, GV. The surgical treatment of tardy ulnar neuritis. J Bone Joint Surg. 1957; 39B:782.
168. Toby, EB, Hanesworth, D, Ulnar nerve strains at the elbow. J Hand Surg. 1998;23A(6):992–997. ![]()
169. O’Driscoll, SW, Horii, E, Carmichael, SW, et al, The cubital tunnel and ulnar neuropathy. J Bone Joint Surg [Br] 1991; 73:613–617. ![]()
170. Wadsworth, TG, Williams, JR, Cubital tunnel external compression syndrome. BMJ 1973; i:662. ![]()
171. Janes, PC, Mann, RJ, Farnworth, TK, Submuscular transposition of the ulnar nerve. Clin Orthop Rel Res 1989; 238:225. ![]()
172. MacNicol, MF, The results of operation for ulnar neuritis. J Bone Joint Surg 1979; 61B:158. ![]()
173. Buehler, MJ, Thayer, DT, The elbow flexion test. A clinical test for the cubital tunnel syndrome. Clin Orthop Rel Res 1988; 233:213–216. ![]()
174. Rosati, M, Martignoni, R, Spagnolli, G, Nesti, C, Lisanti, M, Clinical validity of the elbow flexion test for the diagnosis of ulnar nerve compression at the cubital tunnel. Acta Orthop Belg. 1998;64(4):366–370. ![]()
175. Novak, CB, Lee, GW, Mackinnon, SE, Lay, L, Provocative testing for cubital tunnel syndrome. J Hand Surg. 1994;19A(5):817–820. ![]()
176. Bednar, MS, Ulnar tunnel syndrome. Hand Clin. 1996;12(4):657–664. ![]()
177. Alnot, JY, Frajman, JM. Syndrome de compression chronique du nerf cubital au niveau du coude: à propos de 74 cas. Ann Chir Main Memb Super. 1992; 11(1):5–13.
178. Bartels, RH, Menovsky, T, Van Overbeeke, JJ, Verhagen, WI, Surgical management of ulnar nerve compression at the elbow: an analysis of the literature. J Neurosurg. 1998;89(5):722–727. ![]()
179. Rayan, GM, Proximal ulnar nerve compression. Cubital tunnel syndrome. Hand Clin. 1992;8(2):325–336. ![]()
180. Gumucio, CA, Lund, H, Young, VL, Young, AE, Diagnosis and management of ulnar nerve entrapment. Mo Med. 1992;89(4):231–240. ![]()
181. Weinstein, SM, Herrin, SA, Nerve problems and compartment syndromes in the hand, wrist and forearm. Clin Sports Med. 1992;11(1):161–188. ![]()
182. Padua, L, Aprile, I, Caliandro, P, et al, Natural history of ulnar entrapment at the elbow. Clin Neurophysiol 2002; 113:1980–1984. ![]()
183. Seror, P, Treatment of ulnar nerve palsy at the elbow with a night splint. J Bone Joint Surg. 1993;75B(2):322–327. ![]()
184. Hong, CZ, Long, HA, Kanakamedala, RV, Chang, YM, Yates, L, Splinting and local steroid injection for the treatment of ulnar neuropathy at the elbow: clinical and electrophysiological evaluation. Arch Phys Med Rehabil. 1996;77(6):573–577. ![]()
185. Nathan, PA, Myers, LD, Keniston, RC, Meadows, KD, Simple decompression of the ulnar nerve: an alternative to anterior transposition. J Hand Surg. 1992;17B(3):251–254. ![]()
186. Nathan, PA, Istvan, JA, Meadows, KD, Intermediate and long term outcomes following simple decompression of the ulnar nerve at the elbow. Chir Main 2005; 24:29–34. ![]()
187. Hicks, D, Toby, EB, Ulnar nerve strains at the elbow: the effect of in situ decompression and medial epicondylectomy. J Hand Surg [Am] 2003; 27:1026–1031. ![]()
188. Popa, M, Dupert, T, Treatment of cubital tunnel syndrome by frontal partial medial epicondylectomy. A retrospective study of 55 cases. J Hand Surg [Br] 2004; 295:63–567. ![]()
189. Stuffer, M, Jungwirth, W, Hussl, H, Schmutzhardt, E, Subcutaneous or submuscular anterior transposition of the ulnar nerve? J Hand Surg. 1992;17B(3):248–250. ![]()
190. Manske, PR, Johnston, R, Pruitt, DL, Strecker, WB, Ulnar nerve decompression at the cubital tunnel. Clin Orthop Rel Res 1992; 274:231–237. ![]()
191. Gelberman, RH, Eaton, R, Urbaniak, JR, Peripheral nerve compression. J Bone Joint Surg. 1993;75A(12):1854–1878. ![]()
192. Plancher, KD, McGillicuddy, JO, Kleinman, WB, Anterior intramuscular transposition of the ulnar nerve. Hand Clin. 1996;12(2):435–444. ![]()
193. Glowacki, KA, Weiss, AP, Anterior intramuscular transposition of the ulnar nerve for cubital tunnel syndrome. J Shoulder Elbow Surg. 1997;6(2):89–96. ![]()
194. Siegel, DB, Submuscular transposition of the ulnar nerve. Hand Clin. 1996;12(2):445–448. ![]()
195. Hoffmann, R, Siemionow, M, The endoscopic management of cubital tunnel syndrome. J Hand Surg [Br] 2006; 31:23–29. ![]()
196. Tsai, TM, Chen, IC, Majd, ME, et al, Cubital tunnel release with endoscopic assistance: results of a new technique. J Hand Surg [Am] 1999; 24:21–29. ![]()
197. Dupont, C, Cloutier, GE, Prevost, Y, Dion, MA, Ulnar-tunnel syndrome at the wrist. J Bone Joint Surg 1965; 47A:757. ![]()
198. Sunderland, S. Nerves and Nerve Injuries. Edinburgh: Churchill Livingstone; 1978.
199. Inaparthy, PK, Anwar, F, Botchu, R, Jähnich, H, Katchburian, MV, Compression of the deep branch of the ulnar nerve in Guyon’s canal by a ganglion: two cases. Arch Orthop Trauma Surg. 2008;128(7):641–643. ![]()
200. Fahrer, M, Milroy, PJ, Ulnar compression neuropathy due to anomalous abductor digiti minimi: clinical and anatomic study. J Hand Surg 1981; 6:266. ![]()
201. al-Qattan, MM, Duerksen, F, A variant of flexor carpi ulnaris causing ulnar nerve compression. J Anat. 1992;180(1):189–190. ![]()
202. Capitani, D, Beer, S, Handlebar palsy – a compression syndrome of the deep terminal (motor) branch of the ulnar nerve in biking. J Neurol. 2002;249(10):1441–1445. ![]()
203. Murata, K, Shih, JT, Tsai, TM, Causes of ulnar tunnel syndrome: a retrospective study of 31 subjects. J Hand Surg (Am). 2003;28(4):647–651. ![]()
204. Noth, J, Dietz, V, Mauritz, KH, Cyclist’s palsy: neurological and EMG study in 4 cases with distal ulnar lesions. J Neurol Sci 1980; 47:111. ![]()
205. Oh, SJ. Clinical Electromyography: Nerve Conduction Studies. Baltimore: University Park Press; 1984.
206. Yu-Sung, Wu, Morris, JD, Hogan, GR. Ulnar neuropathy at the wrist: case report and review of literature. Arch Phys Med Rehabil. 1985; 66:785.
207. Morris, HH, Peters, BH, Pronator syndrome: clinical and electrophysiological features in seven cases. J Neurol Neurosurg Psychiatry 1976; 39:461–464. ![]()
208. Aiken, BM, Moritz, MJ, Atypical electromyographic findings in pronator teres syndrome. Arch Phys Med Rehabil 1987; 68:173–175. ![]()
209. Rehak, DC, Pronator syndrome. Clin Sports Med 2001; 20:531–540. ![]()
210. Bridgeman, C, Naidu, S, Kothari, MJ, Clinical and electrophysiological presentation of pronator syndrome. Electromyogr Clin Neurophysiol. 2007;47(2):89–92. ![]()
211. Kiloh, LG, Nevin, S, Isolated neuritis of the anterior interosseous nerve. BMJ 1952; i:850. ![]()
212. Stern, MB, The anterior interosseous nerve syndrome (the Kiloh–Nevin syndrome). Clin Orthop Rel Res 1984; 187:223. ![]()
213. Spinner, RJ, Amadio, PC, Compressive neuropathies of the upper extremity. Clin Plast Surg 2003; 30:155–173. ![]()
214. Solnitsky, O, Pronator syndrome: compression neuropathy of the median nerve at level of pronator teres muscle. Georgetown Med Bull 1960; 13:232. ![]()
215. Johnson, RK, Spinner, M, Shrewsbury, MM, Median nerve entrapment syndrome in the proximal forearm. J Hand Surg 1979; 4:48. ![]()
216. Hartz, CR, Linscheid, RL, Gramse, RR, Daube, JR, The pronator teres syndrome: compression neuropathy of the median nerve. J Bone Joint Surg 1981; 63A:885. ![]()
217. Werner, CO, Rosén, I, Thorngren, KG, Clinical and neurophysiologic characteristics of the pronator syndrome. Clin Orthop Rel Res 1985; 197:231. ![]()
218. Kaufman, MA, Differential diagnosis and pitfalls in electrodiagnostic studies and special tests for diagnosing compressive neuropathies. Orthop Clin North Am 1996; 27:245–252. ![]()
219. Bora, FW, Jr., Osterman, AL, Compression neuropathy. Clin Orthop Rel Res 1982; 100:20. ![]()
220. Howard, FM, Controversies in nerve entrapment syndromes in the forearm and wrist. Orthop Clin North Am 1986; 17:375. ![]()
221. , Incidence of carpal tunnel syndrome in the US military population. Hand (NY). 2009;4(3):289–293. ![]()
222. de Krom, MC, Knipschild, PG, Kester, AD, et al, Carpal tunnel syndrome: prevalence in the general population. J Clin Epidemiol. 1992;45(4):373–376. ![]()
223. Atroshi, I, Gummesson, C, Johnsson, R, et al, Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999;282(2):153–158. ![]()
224. Stevens, JC, Sun, S, Beard, CM, O’Fallon, WM, Kurland, LT, Carpal tunnel syndrome in Rochester, Minnesota, 1961 to 1980. Neurology 1988; 38:134–138. ![]()
225. Paget, J. Lectures on Surgical Pathology. Philadelphia: Lindsay & Blakiston; 1854.
226. Cyriax, JH. Perineuritis. BMJ. 1942; i:578.
227. Cannon, BW, Love, JG, Tardy median palsy: median neuritis: median thenar neuritis amenable to surgery. Surgery 1946; 20:210. ![]()
228. Brain, WR, Wright, AD, Wilkinson, M, Spontaneous compression of both median nerves in carpal tunnel: 6 cases treated surgically. Lancet 1947; i:227. ![]()
229. Phalen, GS, The carpal tunnel syndrome: 17 years’ experience in diagnosis and treatment. J Bone Joint Surg 1966; 48A:211. ![]()
230. Rosenbaum, RB, Ochoa, JL. Carpal tunnel syndrome and other disorders of the median nerve. 2. Amsterdam: Butterworth Heinemann; 2002.
231. Beekman, R, Visser, LH, Sonography in the diagnosis of carpal tunnel syndrome: a critical review of the literature. Muscle Nerve 2003; 27:26–33. ![]()
232. Hobson-Webb, LD, Padua, L, Median nerve ultrasonography in carpal tunnel syndrome: findings from two laboratories. Muscle Nerve 2009; 40:94–97. ![]()
233. Fung, KK, Chan, KY, Lam, LY, et al, Study of wrist posture, loading and repetitive motion as risk factors for developing carpal tunnel syndrome. Hand Surg 2007; 12:13–18. ![]()
234. Dias, JJ, Burke, FD, Wildin, CJ, Heras-Palou, C, Bradley, MJ, Carpal tunnel syndrome and work. J Hand Surg Br 2004; 29:329–333. ![]()
235. Stevens, J, Witt, JC, Smith, BE, Weaver, AL, The frequency of carpal tunnel syndrome in computer users in a medical facility. Neurology 2001; 56:1568–1570. ![]()
236. Andersen, JH, Thompson, JF, Overgaard, E, et al, Computer use and carpal tunnel syndrome: A 1 year follow-up study. JAMA 2003; 289:2963–2969. ![]()
237. Spinner, M. Management of nerve compression lesions. In: Instructional Course Lectures, The American Academy of Orthopaedic Surgeons. St Louis: Mosby; 1984:489–512.
238. Palumbo, CF, Szabo, RM, Olmsted, SL, The effects of hypothyroidism and thyroid replacement on the development of carpal tunnel syndrome. J Hand Surg. 2000;25A(4):734–738. ![]()
239. Purnell, DC, Daly, DD, Lipscomb, PR, Carpal-tunnel syndrome associated with myxedema. Arch Intern Med 1961; 108:751–756. ![]()
240. O’Duffy, JD, Randall, RV, MacCarty, CS, Median neuropathy (carpal-tunnel syndrome) in acromegaly: a sign of endocrine overactivity. Ann Intern Med 1973; 78:379–383. ![]()
241. Jenkins, PJ, Sohaib, SA, Akker, S, et al, The pathology of median neuropathy in acromegaly. Ann Intern Med. 2000;133(3):197–201. ![]()
242. McLennan, HG, Outs, JN, Walstab, JE, Survey of hand symptoms in pregnancy. Med J Aust 1987; 147:542–544. ![]()
243. Gould, JS, Wissinger, HA, Carpal tunnel syndrome in pregnancy. Southern Med J 1978; 71:144. ![]()
244. Wilbourn, AJ. Diabetic entrapment and compression neuropathies. In: Dyck PJ, Thomas PK, eds. Diabetic neuropathy. 2nd ed. Philadelphia: Saunders; 1999:481–508.
245. Nakamichi, K, Tachibana, S, Unilateral carpal tunnel syndrome and space-occupying lesions. J Hand Surg [Br] 1993; 18:48–49. ![]()
246. Kremchek, TE, Kremchek, EJ, Carpal tunnel syndrome caused by flexor tendon sheath lipoma. Orthop Rev 1988; 17:1083–1085. ![]()
247. Pai, CH, Tseng, CH, Acute carpal tunnel syndrome caused by tophaceous gout. J Hand Surg [Am] 1993; 18:667–669. ![]()
248. Kerrigan, JJ, Bertoni, JM, Jaeger, SH, Ganglion cysts and carpal tunnel syndrome. J Hand Surg 1988; 13A:763–765. ![]()
249. Crymble, B. Brachial neurologia and CTS. BMJ. 1968; 3:470.
250. Jarvik, JG, Yuen, E, Kliot, M, Diagnosis of carpal tunnel syndrome: electrodiagnostic and MR imaging evaluation. Neuroimaging Clin N Am 2004; 14:93–102. ![]()
251. Durkan, JA, A new diagnostic test for carpal tunnel syndrome. J Bone Joint Surg Am 1991; 73:535–538. ![]()
252. Tsai, CY, Yu, CL, Tsai, ST, Bilateral carpal tunnel syndrome secondary to tophaceous compression of the median nerves. Scand J Rheumatol 1996; 25:107–108. ![]()
253. Smith, EM, Sonstegard, DA, Anderson, WH, Carpal tunnel syndrome: contribution of flexor tendons. Arch Phys Med Rehabil. 1977;158(58):378. ![]()
254. Moldover, J, Tinel’s sign: its characteristics and significances. J Bone Joint Surg 1978; 60A:412. ![]()
255. Gellman, H, Gelberman, RH, Tan, AM, Botte, MJ, Carpal tunnel syndrome: an evaluation of the provocative diagnostic tests. J Bone Joint Surg 1986; 68A:735. ![]()
256. Katz, JN, Larson, MG, Sabra, A, et al, The carpal tunnel syndrome: diagnostic utility of the history and physical examination findings [see comments]. Ann Intern Med 1990; 112:321–327. ![]()
257. Kuhlman, KA, Hennessey, WJ, Sensitivity and specificity of carpal tunnel syndrome signs. Am J Phys Med Rehabil. 1997;76(6):451–457. ![]()
258. Jablecki, CK, Andary, MT, So, YT, Wilkins, DE, Williams, FH, Literature review of the usefulness of nerve conduction studies and electromyography for the evaluation of patients with carpal tunnel syndrome. AAEM Quality Assurance Committee. Muscle Nerve. 1993;16(12):1392–1414. ![]()
259. Wertsch, JJ, Melvin, J, Median nerve anatomy and entrapment syndromes: a review. Arch Phys Med Rehabil 1982; 63:623. ![]()
260. Jablecki, CK, Andary, MT, So, YT, Wilkins, DE, Williams, FH, Literature review of the usefulness of nerve conduction studies and electromyography for the evaluation of patients with carpal tunnel syndrome. AAEM Quality Assurance Committee. Muscle Nerve 1993; 16:1392–1414. ![]()
261. Nathan, PA, Takigawa, K, Keniston, RC, Meadows, KD, Lockwood, RS, Slowing of sensory conduction of the median nerve and carpal tunnel syndrome in Japanese and American industrial workers. J Hand Surg [Br] 1994; 19:30–34. ![]()
262. Szabo, RM, Slater, RR, Jr., Farver, TB, Stanton, DB, Sharman, WK, The value of diagnostic testing in carpal tunnel syndrome. J Hand Surg Am. 1999;24(4):704–714. ![]()
263. Atroshi, I, Gummesson, C, Johnsson, R, Ornstein, E, Diagnostic properties of nerve conduction tests in population-based carpal tunnel syndrome. BMC Musculoskelet Disord 2003; 4:9. ![]()
264. Graham, B, The value added by electrodiagnostic testing in the diagnosis of carpal tunnel syndrome. J Bone Joint Surg Am. 2008;90(12):2587–2593. ![]()
265. Zucker-Pinchott, B, Hermann, G, Srinivasan, R, Computed tomography of the carpal tunnel: a radioanatomical study. J Comput Assist Tomogr 1981; 5:525. ![]()
266. Fleckenstein, JL, Wolfe, GI, MRI vs EMG: which has the upper hand in carpal tunnel syndrome? Neurology 2002; 58:1583–1584. ![]()
267. John, V, Nam, HE, Nahzer, HC, CT of carpal tunnel syndrome. Am J Neuroradiol 1983; 4:770. ![]()
268. Jetzer, T, Erickson, D, Webb, A. Computed tomography of the carpal tunnel with clinical and surgical correlation. CT Clin Symp. 1984; 7:2.
269. Keles, I, Karagulle Kendi, AT, Aydin, G, Zog, SG, Orkun, S, Diagnostic precision of ultrasonography in patients with carpal tunnel syndrome. Am J Phys Med Rehabil. 2005;84(6):443–450. ![]()
270. Koyuncuoglu, HR, Kutluhan, S, Yesildag, A, Oyar, O, Guler, K, Ozden, A, The value of ultrasonographic measurement in carpal tunnel syndrome in patients with negative electro diagnostic tests. Eur J Radiol. 2005;56(3):365–369. ![]()
271. El Miedany, YM, Aty, SA, Ashour, S, Ultrasonography versus nerve conduction study in patients with carpal tunnel syndrome: substantive or complementary tests? Rheumatology (Oxford). 2004;43(7):887–895. ![]()
272. Kruger, VL, Kraft, GH, Deitz, JC, Ameis, A, Polissar, L, Carpal tunnel syndrome: objective measures and splint use. Arch Phys Med Rehabil 1991; 72:517–520. ![]()
273. Burke, DT, Burke, MM, Stewart, GW, Cambre, A, Splinting for carpal tunnel syndrome: in search of the optimal angle. Arch Phys Med Rehabil 1994; 75:1241–1244. ![]()
274. Walker, WC, Metzler, M, Cifu, DX, Swartz, Z, Neutral wrist splinting in carpal tunnel syndrome: a comparison of night-only versus full-time wear instructions. Arch Phys Med Rehabil. 2000;81(4):424–428. ![]()
275. McColl, GJ, Dolezal, H, Eizenberg, N, Common corticosteroid injections. An anatomical and evidence based review. Aust Fam Phys. 2000;29(10):922–926. ![]()
276. Girlanda, P, Dattola, R, Venuto, C, et al, Local steroid treatment in idiopathic carpal tunnel syndrome: short- and long-term efficacy. J Neurol 1993; 240:187–190. ![]()
277. Marshall, S, Tardif, G, Ashworth, N, Local corticosteroid injection for carpal tunnel syndrome (Cochrane review). Cochrane Database Syst Review. 2000;(4). ![]()
278. Demirci, S, Kutluhan, S, Koyuncuoglu, HR, et al, Comparison of open carpal tunnel release and local steroid treatment outcomes in idiopathic carpal tunnel syndrome. Rheumatol Int. 2002;22(1):33–37. ![]()
279. Ly-Pen, D, Andréu, JL, de Blas, G, Sánchez-Olaso, A, Millán, I, Surgical decompression versus local steroid injection in carpal tunnel syndrome: a one-year, prospective, randomized, open, controlled clinical trial. Arthritis Rheum. 2005;52(2):612–619. ![]()
280. Agarwal, V, Singh, R, Sachdev, A, Wiclaff Shekhar, S, Goel, D, A prospective study of the long-term efficacy of local methyl prednisolone acetate injection in the management of mild carpal tunnel syndrome. Rheumatology (Oxford). 2005;44(5):647–650. ![]()
281. Marshall, S, Tardif, G, Ashworth, N, Local corticosteroid injection for carpal tunnel syndrome. Cochrane Database Syst Rev. 2007;(2). ![]()
282. Gelberman, RH, Aronon, D, Weisman, MH, Carpal tunnel syndrome: a prospective trial of steroid injection and splinting. J Bone Joint Surg 1980; 62A. ![]()
283. Peters-Veluthamaningal, C, Winters, JC, Groenier, KH, Meyboom-de Jong, B, Randomised controlled trial of local corticosteroid injections for carpal tunnel syndrome in general practice. BMC Fam Pract 2010; 11:54. ![]()
284. Armstrong, T, Devor, W, Borschel, L, Contreras, R, Intracarpal steroid injection is safe and effective for short-term management of carpal tunnel syndrome. Muscle Nerve. 2004;29(1):82–88. ![]()
285. Concannon, MJ, Brownfield, ML, Puckett, CL, The incidence of recurrence after endoscopic carpal tunnel release. Plast Reconstr Surg. 2000;105(5):1662–1665. ![]()
286. Atroshi, I, Gummesson, C, Johnsson, R, Sprinchorn, A, Symptoms, disability, and quality of life in patients with carpal tunnel syndrome. J Hand Surg [Am] 1999; 24:398–404. ![]()
287. Keith, MW, Masear, V, Amadio, PC, et al, Treatment of carpal tunnel syndrome. J Am Acad Orthop Surg. 2009;17(6):397–405. ![]()
288. Ahlberg, J, Johansson, H, Widenfalk, B, Disabling injuries following carpal tunnel syndrome surgery. Lakartidningen 2007; 104:2884–2886. ![]()
289. Benson, LS, Bare, AA, Nagle, DJ, Harder, VS, Williams, CS, Visotsky, JL, Complications of endoscopic and open carpal tunnel release. Arthroscopy 2006; 22:919–924. ![]()
290. Atroshi, I, Larsson, GU, Ornstein, E, Hofer, M, Johnsson, R, Ranstam, J, Outcomes of endoscopic surgery compared with open surgery for carpal tunnel syndrome among employed patients: randomised controlled trial. BMJ 2006; 332:1473–1476. ![]()
291. McConnell, JR, Bush, DC, Intraneural steroid injection as a complication in the management of carpal tunnel syndrome. Clin Orthop Rel Res 1990; 250:181. ![]()
292. Szabo, RM, Madison, M, Carpal tunnel syndrome. Orthop Clin North Am. 1992;23(1):103–108. ![]()
293. Pagnanelli, DM, Barrer, SJ, Bilateral carpal tunnel release at one operation: report of 228 patients. Neurosurgery. 1992;31(4):1030–1033. ![]()
294. Haupt, WF, Wintzer, G, Schop, A, Löttgen, J, Pawlik, G, Long-term results of carpal tunnel decompression. Assessment of 60 cases. J Hand Surg. 1993;18B(4):471–474. ![]()
295. Delaere, O, Bouffioux, N, Hoang, P, Endoscopic treatment of the carpal tunnel syndrome: review of the recent literature. Acta Chir Belg. 2000;100(2):54–57. ![]()
296. Lindau, T, Karlsson, MK, Complications and outcome in open carpal tunnel release. A 6-year follow-up in 92 patients. Chir Main. 1999;18(2):115–121. ![]()
297. Brief, R, Brief, LP, Endoscopic carpal tunnel release: report of 146 cases. Mt Sinai J Med. 2000;67(4):274–277. ![]()
298. Atroshi, I, Hofer, M, Larsson, GU, Ornstein, E, Johnsson, R, Ranstam, J, Open compared with 2-portal endoscopic carpal tunnel release: A 5-year follow-up of a randomized controlled trial. J Hand Surg Am. 2009;34(2):266–272. ![]()
299. Wong, KC, Hung, LK, Ho, PC, Wong, JM, Carpal tunnel release. A prospective, randomised study of endoscopic versus limited-open methods. J Bone Joint Surg Br. 2003;85(6):863–868. ![]()
300. Mackenzie, DJ, Hainer, R, Wheatley, MJ, Early recovery after endoscopic vs short-incision open carpal tunnel release. Ann Plast Surg. 2000;44(6):601–604. ![]()
301. Ferdinand, RD, MacLean, JG, Endoscopic versus open carpal tunnel release in bilateral carpal tunnel syndrome. A prospective, randomised, blinded assessment. J Bone Joint Surg Br. 2002;84(3):375–379. ![]()
302. Scholten, RJ, Mink van der Molen, A, Uitdehaag, BM, et al, Surgical treatment options for carpal tunnel syndrome. Cochrane Database Syst Rev. 2007;(4). ![]()
303. Horowitz, SH, Iatrogenic causalgia: classification, clinical findings, and legal ramifications. Arch Neurol 1984; 41:821–824. ![]()

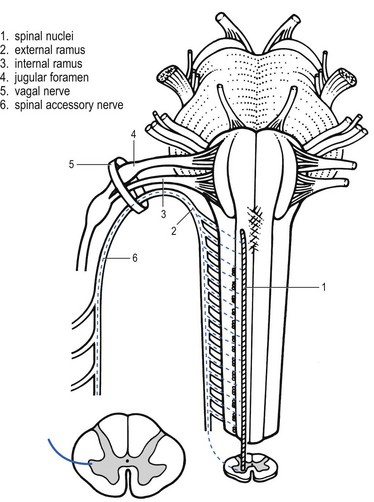
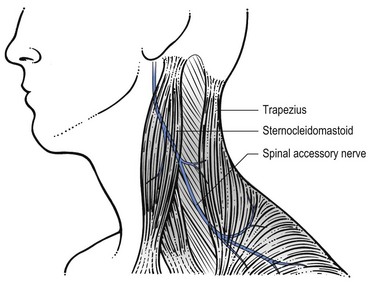
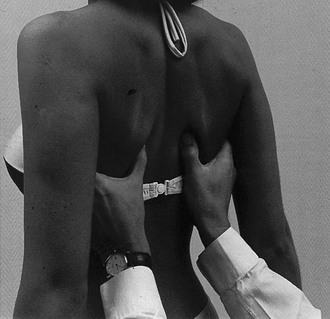
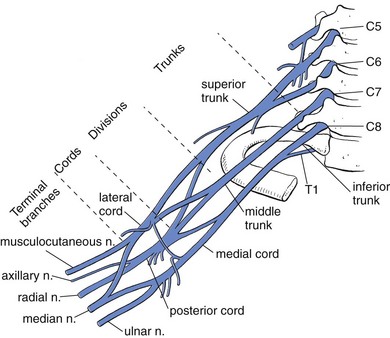
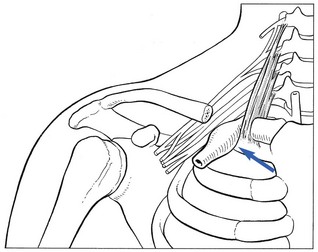



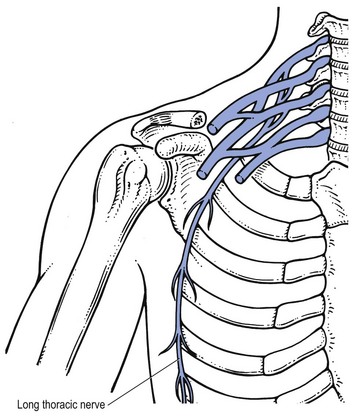
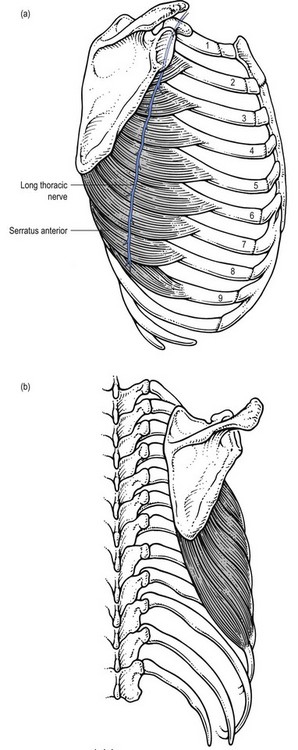
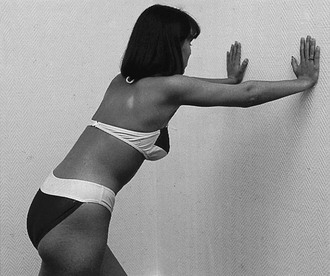
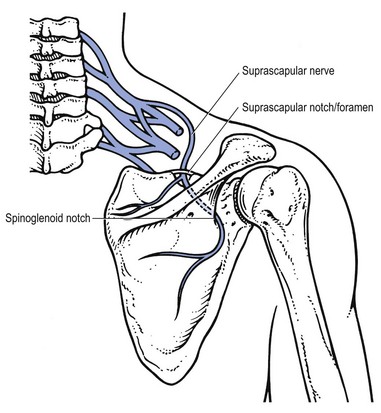

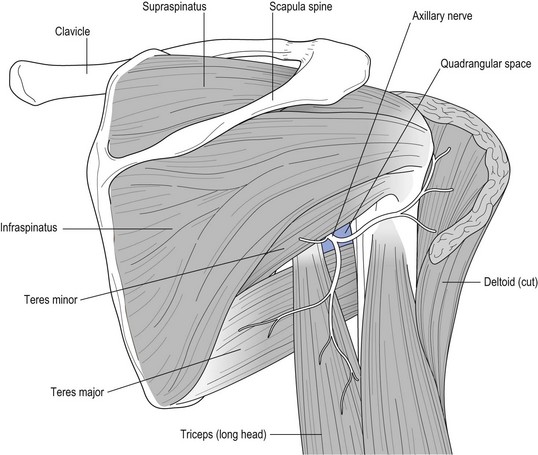
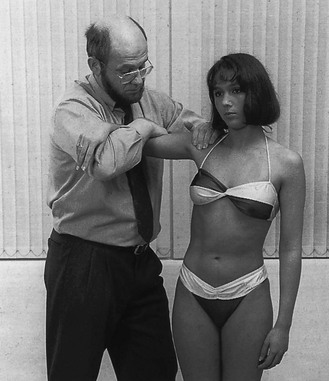
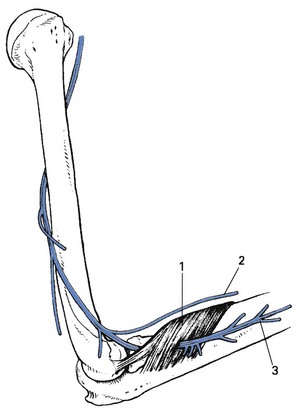
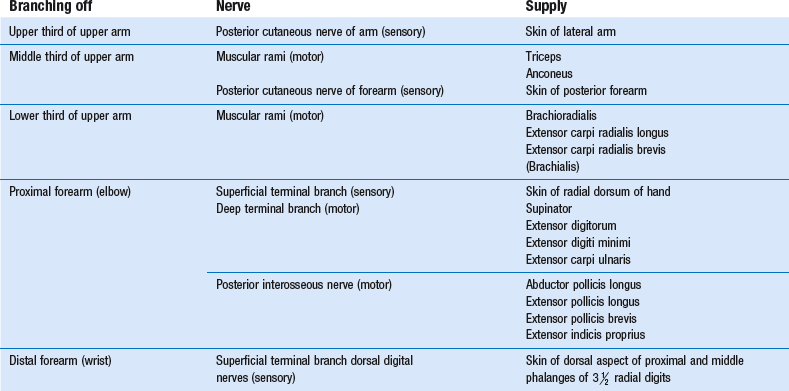
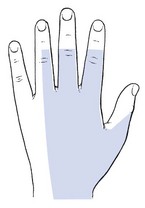
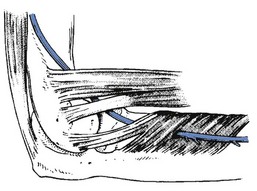
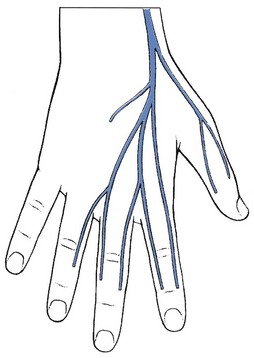
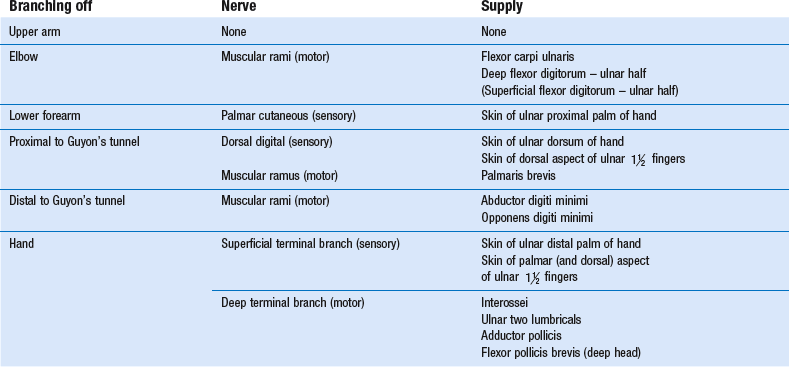
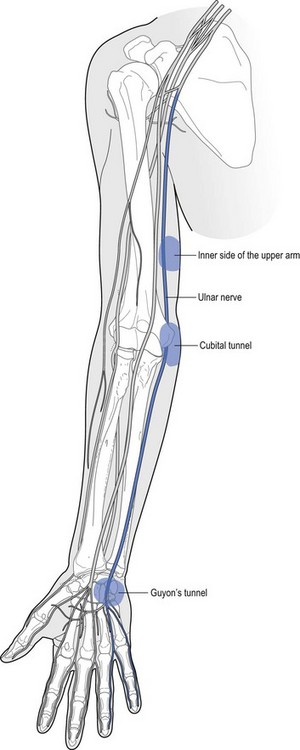
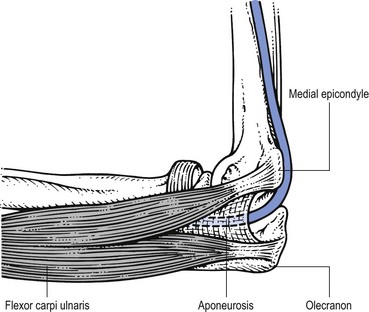
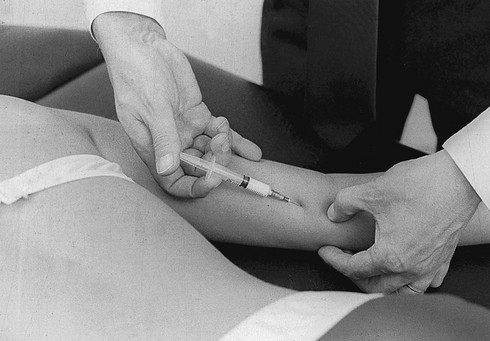
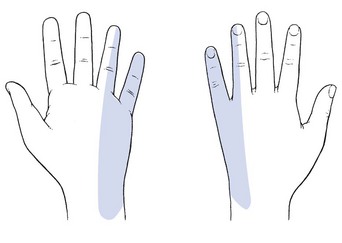
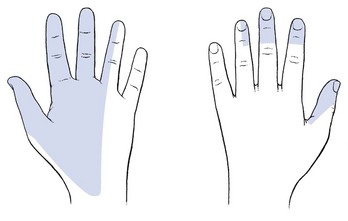
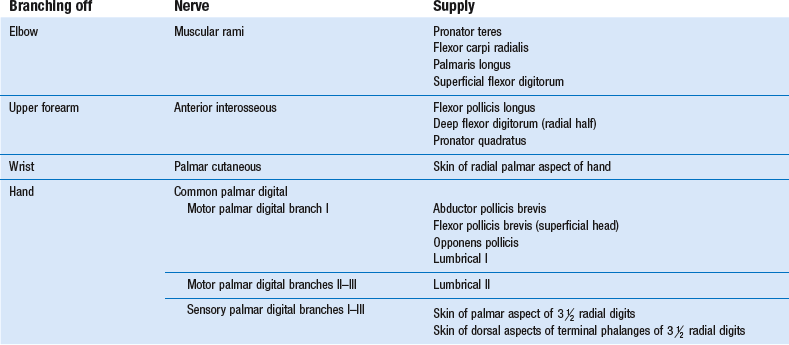
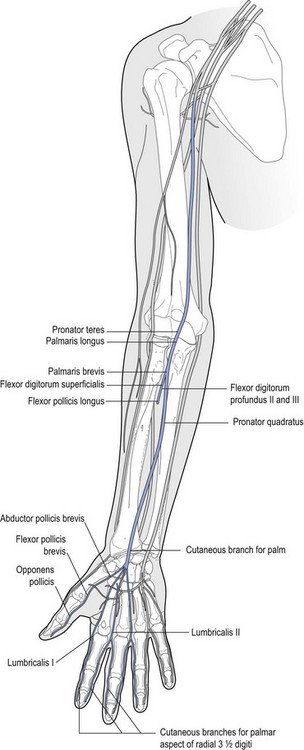
 digiti
digiti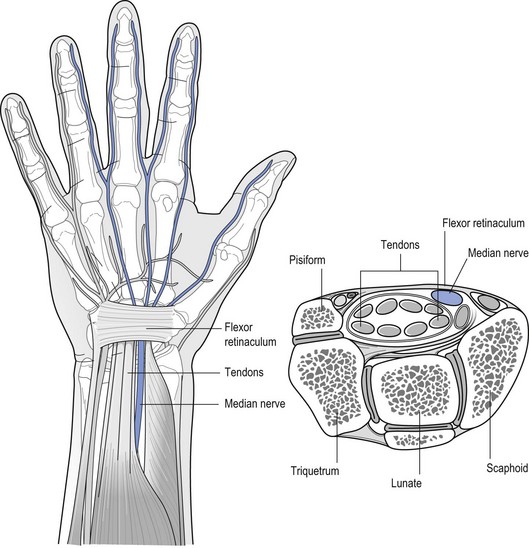
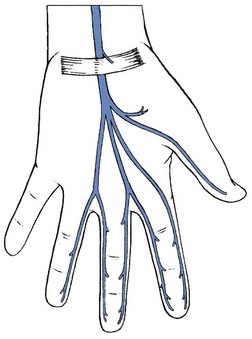
 digits.
digits.