Nerve lesions and entrapment neuropathies of the lower limb
Introduction
The main symptom of pressure on nerves is paraesthesia. Depending on the level of the compression, paraesthesia is accompanied by pain and numbness. The combination of these three symptoms and their interrelation are of importance in localizing the site of compression.1
Pressure on the distal spinal cord induces painless pins and needles in both feet, soon followed by numbness, incoordination and abnormal reflexes. This mechanism has been discussed in the chapters on the cervical and thoracic spine.
Pressure on a nerve root causes segmental pain, paraesthesia at the distal aspect of the respective dermatome and, if the pressure increases, motor and sensory deficit. For detailed descriptions of these pathologies, see the chapters on the lumbar spine.
Pressure on the lumbosacral plexus causes little pain but increasing numbness and weakness. For instance, compression of the plexus by a neoplasm does not cause pain in the limbs but only sacral or coccygeal pain. However, it does give rise to gross weakness of the muscles of one or both legs and feet.
The effects of pressure on the peripheral nerves of leg and foot are discussed in this chapter.
Sciatic nerve
Neurocompression syndromes of the sciatic nerve are not common. Some believe that the nerve can become compressed between the fibres of the piriformis muscle (the piriformis syndrome2).
If the nerve becomes damaged or is chronically irritated, serious deafferentation pain can result and occurs in circumstances in which the sciatic nerve is locally bruised or has undergone damage after local injection of irritating substances. Continuous and burning pain, independent of posture, is then felt in the sensory distribution of the nerve. Local pressure on the nerve can increase the pain considerably.3–4
Lateral cutaneous nerve
Entrapment of the lateral cutaneous femoral nerve is not uncommon and results in meralgia paraesthetica.
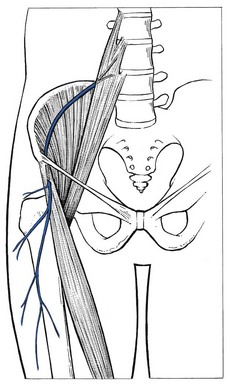
The lateral cutaneous nerve is sensory only. It originates at L2 and runs retroperitoneally to emerge at the outer edge of the psoas and then crosses the iliacus muscle at the lateral border of the pelvis, which it follows to the anterior superior spine of the ilium. It then passes under the lateral aspect of the inguinal ligament to follow the fibres of the sartorius muscle. Its course and the location as it exits the pelvis are very variable. Aszmann et al5 investigated its relation to soft-tissue and bony landmarks in the inguinal region through dissection of 52 human anatomic specimens and identified five different types: type A, posterior to the anterior superior iliac spine, across the iliac crest (4%); type B, anterior to the anterior superior iliac spine and superficial to the origin of the sartorius muscle but within the substance of the inguinal ligament (27%); type C, medial to the anterior superior iliac spine, ensheathed in the tendinous origin of the sartorius muscle (23%); type D, medial to the origin of the sartorius muscle located in an interval between the tendon of the sartorius muscle and thick fascia of the iliopsoas muscle deep to the inguinal ligament (26%); and type E, most medial and embedded in loose connective tissue, deep to the inguinal ligament, overlying the thin fascia of the iliopsoas muscle and contributing the femoral branch of the genitofemoral nerve (20%). Other studies located the nerve most commonly at 10–15 mm medial to the anterior superior iliac spine but in some cases it was located as far medially as 46 mm.6,7 A few centimetres below the anterior superior iliac spine it emerges through the deep fascia and continues its course subcutaneously (Fig. 1).
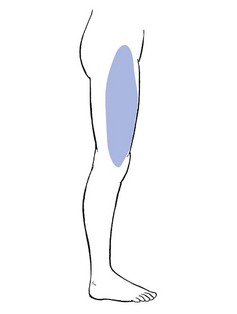
The nerve supplies the anterolateral aspect of the thigh from the upper border of the trochanter to the level of the superior margin of the patella (Fig. 2).
The nerve can become trapped at any point along its course, although most cases result from nipping at the inguinal ligament or beyond the fascial tunnel, usually at the point where the nerve becomes superficial. Occasionally the symptoms stem from an abnormality in the pelvis, the typical example of which is meralgia during pregnancy (Cyriax:1 pp. 297–298), encountered between the fourth and seventh months. In this condition, the symptoms are always unilateral and disappear spontaneously during the pregnancy. They have been ascribed to the pressure of a small fibromyoma against the nerve, close to where it emerges at the lateral border of the psoas. Meralgia paraesthetica has also been reported after pelvic osteotomies for Perthes’ disease,8,9 shelf operations for acetabular insufficiency10 and after the removal of bone from the iliac crest for a graft.11 However, most cases of meralgia paraesthetica are idiopathic, although some external causes such as tight trousers,12 obesity,13 the use of belts, corsets and trusses, or an overtight bandage round the pelvis14 after an operation or during pelvic traction can compress the nerve just medial to the anterior superior iliac spine.
The symptoms are typical of any lesion of a small peripheral sensory nerve: pain, paraesthesia and numbness, confined to its distribution. The patient typically describes a burning or tingling sensation over the anterolateral aspect of the thigh. The edge is well defined and the centre is often completely anaesthetic. A common complaint is hypersensitivity: the patient even dislikes the touch of a cloth in the affected area.15 Clinical examination reveals the extent of anaesthesia, which has a clear edge. Tenderness to pressure can sometimes be evoked distal to the anterior superior iliac spine. In some cases, the paraesthesia can be aggravated by tapping the nerve.16,17
Differentiation of meralgia paraesthetica from a second lumbar root lesion remains the greatest problem in diagnosis18 and relies on the careful delineation of the paraesthetic area, the degree of numbness and a negative MR scan of the lumbar spine.19,20 Although the L2 area and the area supplied by the lateral cutaneous nerve correspond well laterally, the second root also contributes to the innervation of the groin and the inner aspect of the thigh. Furthermore, in L2 root lesions the analgesia is very slight because of the overlap between L2 and L3, whereas in lesions of the lateral cutaneous nerve, there is almost full anaesthesia, with a clear-cut border (Box 1).
Treatment depends on the underlying cause. In external pressure at the fascial tunnel, it is sometimes sufficient to remove the cause. Should this simple action fail, infiltration with anaesthetic at the point of contact is indicated.
Technique: infiltration
A 10 ml syringe is filled with procaine 0.5% and fitted to a thin needle 5 cm long. A point is chosen 5 cm below and medial to the anterior superior iliac spine. The needle is inserted and moved upwards along the anterior and medial side of the sartorius muscle. A fan-wise infiltration is made here.21 Two to four weekly infiltrations may be necessary.
In intractable cases surgery can be considered.22 It should be remembered, however, that in about two-thirds of cases the symptoms subside spontaneously over 2 years.23,24
Femoral nerve
Although the femoral nerve can be compressed by different processes in the psoas region, the pelvis and the groin, neither pain nor paraesthesia ever result.25 The symptoms are a vague numbness in the anterior crural area and increasing weakness of the psoas and quadriceps femoris muscles. A new cause of femoral compression neuropathy has been reported during recent decades – retroperitoneal bleeding resulting from anticoagulant therapy.26–28
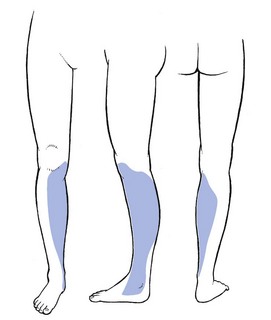
The anterior cutaneous nerve innervates the skin of the front of the thigh as far as the upper border of the patella (Fig. 3). It can be compressed at the point where it emerges through the fascia of the thigh, some 10 cm below the inguinal ligament. Local pressure or friction may cause pins and needles and cutaneous analgesia confined to the anterior aspect of the thigh, with a clear-cut border and almost complete numbness towards the centre of the area.
Treatment is removal of the external pressure and procaine infiltrations.
Saphenous nerve
The saphenous nerve is the largest cutaneous branch of the femoral nerve. It leaves the subartorial canal about 8–10 cm above the medial condyle of the knee. Some of the branches there provide innervation of the medial aspect of the knee. Another branch follows the sartorius muscle and becomes superficial just below the medial condyle of the tibia.29 It then runs down on the leg to follow the great sapheneous vein over the anterior aspect of the medial malleolus (see Fig. 6). Its territory of distribution is the medial side of the leg, the medial malleolus and the medial border of the foot30 (Fig. 4).
Traction on the saphenous nerve as it leaves the subsartorial canal may cause oedema, inflammation and thus compression31–33 (Fig. 5). Direct compression of the nerve may also occur in front of the inner tibial condyle.34,35 However, the usual site of compression is at the ankle, at the anterior aspect of the medial malleolus.
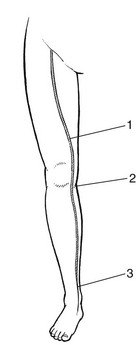
Fig 5 Localization of entrapment along the saphenous nerve: 1, leaving the subsartorial canal; 2, in front of the inner tibial condyle; 3, at the anterior aspect of the medial malleolus.
Saphenous neuralgia is also a well-known and common complication after harvesting of great saphenous vein for coronary artery bypass grafting. The main symptom is anaesthesia which may persist for a considerable time postoperatively.36–38
Paraesthesia over the inner aspect of the ankle and along the medial border of the foot, together with aching and numbness along the subcutaneous border of the tibia, results from either a direct contusion or sustained compression. Combined plantiflexion and eversion of the foot or flexion of the hallux may stretch the nerve and cause sharp neuralgic twinges.39
Procaine infiltrations of the nerve, level with the ankle joint, are often curative. Ten ml of procaine 1% is infiltrated each week, over 3 consecutive weeks.
Common peroneal nerve
The common peroneal nerve emerges at the upper and lateral aspect of the popliteal fossa, through the fascia between the biceps femoris tendon and the lateral head of the gastrocnemius.40 It follows the biceps to the neck of the fibula where, under a fibrous edge beneath the origin of the peroneus longus, it divides into two branches. The superficial peroneal nerve continues under the peroneus longus, first along the fibula and then between peroneus longus and brevis.41 The deep peroneal nerve winds around the fibular neck and runs through the anterior compartment between the extensor hallucis and tibialis anterior muscles until it traverses the ankle deep to the inferior extensor retinaculum.
Compression or elongation of the common peroneal nerve classically occurs where it winds round the lateral aspect of the neck of the fibula.42 Direct compression follows immobilization in an over-tight plaster cast, fracture of the neck of the fibula or externally from pressure of the fibular head against a hard surface such as the side of a desk. Iatrogenic injury of the peroneal nerve can also occur from direct manipulation during orthopaedic surgery or with prolonged compression during lateral hip and leg rotation with knee flexion as occurs in operative positioning.43 Elongation is frequent from sitting with the knees bent and the foot in full passive plantiflexion and inversion44 or from prolonged squatting.45 Long-standing compression causes atrophy and a drop foot. Slight and temporary compression or elongation of the nerve leads to ‘neuropraxis’ – a neurological deficit that recovers spontaneously within the course of 1–2 weeks. Chronic recurrent entrapment of the common peroneal nerve has recently been described in long-distance runners.46,47
There is only slight pain and there is no paraesthesia during the period of compression. Clinical examination reveals numbness of the dorsum of the foot and four inner toes, together with weakness of the tibialis anterior, extensor hallucis longus and peroneal muscles, which combine to produce a drop foot.48
There is no specific treatment but, in stretch or after moderate compression, spontaneous recovery is the rule. The patient must then be told how to prevent recurrence. In recurrent and transient entrapment, neurolysis of the peroneal nerve as it travels under the sharp fibrous edge of the origin of the peroneus longus can be performed and seems to give good results.49 When the condition is caused by the pressure of an over-tight plaster or a direct blow, drop foot is usually permanent.
Deep peroneal nerve
Contusion of the terminal branch of the deep peroneal nerve can occur at the anterior aspect of the ankle, where it is relatively unprotected between the tendons of the tibialis anterior and the extensor hallucis longus, or at the dorsum of the foot50,51 (Fig. 6). Compression neuropathy from tight boots or shoe straps has been called the anterior tarsal tunnel syndrome.52,53 A direct blow produces the same condition.
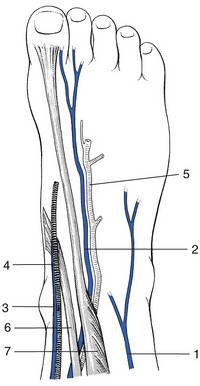
Fig 6 Sites of compression and localization of infiltration of the superficial peroneal nerve (1), deep peroneal nerve (2), and saphenous nerve (3), the saphenous vein (4) and dorsal artery of the root (5) are also shown, (6) is the tendon of the tibialis anterior and (7) extensor hallucis longus.
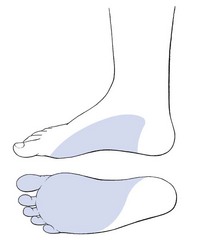
The patient complains of aching deep in the medial and dorsal aspect of the foot and pins and needles at the adjacent borders of the big and second toes (Fig. 7). The symptoms are typically worse on activity and relieved by rest.54
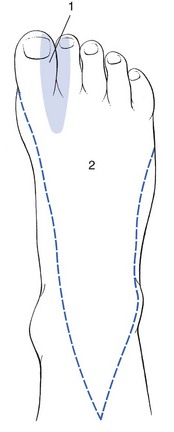
Fig 7 Area within which sensory changes may be found in lesions of the deep (1) and superficial (2) peroneal nerves.
Examination demonstrates diminished touch perception in the web space between the first and second toes. A positive percussion sign (Tinel’s sign) is usually found.55
Treatment consists of wearing better-fitting footwear and three or four weekly procaine infiltrations around the nerve. Surgical intervention is seldom necessary.
Superficial peroneal nerve
The superficial peroneal nerve emerges from the deep fascia at the junction between the middle and lower thirds of the leg. From this point it runs subcutaneously and is sensory only. It supplies the skin of the distal third of the front of the leg and the dorsum of the foot, except the adjacent borders of the big and second toes.
Entrapment can result from fibrosis after a direct blow56 or surgery for chronic lateral compartment syndrome.57 Transient tethering of the nerve during forced inversion and plantiflexion of the foot (ankle sprain) can also result in a momentarily painful stretch.58,59
The symptoms are pain, tingling and numbness over the dorsum of the whole foot and all the toes. Pressure or percussion (Tinel’s sign) at the point of exit causes neuralgic pain and paraesthesia in the same area.60
Treatment consists of repeated injections with procaine at the site of compression. Should these fail, triamcinolone should be substituted. Fasciotomy and neurolysis relieve symptoms in only half of the cases.61,62
Tibial nerve
Entrapment of the posterior tibial nerve is most commonly seen at the medial aspect of the ankle and the midfoot in the so-called ‘tarsal tunnel’.63 The tarsal tunnel is an osteofibrous space bordered by the medial malleolus, the medial aspect of the talus and calcaneus and the flexor retinaculum. It contains the tibialis posterior, the flexor hallucis longus, the flexor digitorum longus and the posterior tibial nerve and artery64 (Fig. 8). Consequently, compression of the posterior tibial nerve behind the medial melleolus and under the flexor retinaculum has been called the tarsal tunnel syndrome.65,66
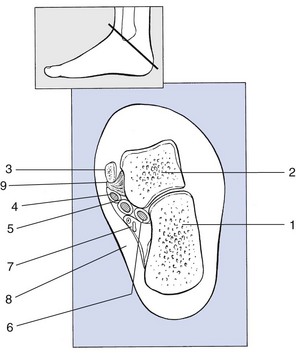
Fig 8 The tarsal tunnel: 1, calcaneus; 2, talus; 3, tibia; 4, tibialis posterior tendon; 5, flexor digitorum longus tendon; 6, flexor hallucis longus tendon; 7, tibial nerve and artery; 8, flexor retinaculum; 9, deltoid ligament.
The causes of compression are a space-occupying lesion (such as a bony exostosis), callus formation67 or an inflamed and enlarged tendon sheath.68 Excessive valgus deformity of the calcaneus with tension across the flexor retinaculum has been blamed.69 Diseases such as rheumatoid arthritis, diabetes or a varicose vein have also been implicated.70–72
Patients with tarsal tunnel syndrome present with paraesthesia, burning pain and numbness in the plantar aspect of the foot and the toes73,74 (Fig. 9).
These symptoms are frequently exacerbated during weight bearing, especially when valgus deformity causes the compression.75 Many patients complain of nocturnal symptoms, which has been attributed to venous engorgement because the symptoms disappear when the foot is elevated. Symptoms can be reproduced by forced eversion and dorsiflexion of the foot.76 Sometimes Tinel’s sign is positive.77 Pain and paraesthesia may also be reproduced by inflating a pneumatic tourniquet around the affected ankle.78
Treatment is first by correction of the underlying disorder. Infiltration with procaine or triamcinolone can be tried. If these measures fail, surgical release of the flexor retinaculum is considered.79 However, the neurophysiological and clinical outcome of surgical decompression is only successful in half of the operations80,81. Recently, endoscopic techniques for the decompression of the tibial nerve and its branches have been used with acceptable results.82
Plantar nerves
These are branches of the posterior tibial nerve, running behind the medial aspect of the tuber calcanei, under the abductor hallucis and quadratus plantae. In valgus deformity of the ankle they can be compressed between the sharp calcaneal border and the shoe, to cause pain and burning sensation in the heel and foot.83 Compression of the lateral nerve causes pain and paraesthesia at the outer side of the foot, medial nerve compression at the medial side.84
Treatment is correction of the valgus deformity and infiltrations with triamcinolone.85 Should these conservative measures fail, surgery can be considered.86
References
1. Cyriax, JH, 8th ed. Textbook of Orthopaedic Medicine; vol. 1. Baillière Tindall, London, 1982.
2. Nakano, KK. Sciatic nerve entrapment: the piriformis syndrome. Musculoskeletal Med. 1987; 4:33–37.
3. Asbury, AK, Fields, HL, Pain due to peripheral nerve damage: a hypothesis. Neurology 1984; 34:1587–1592. ![]()
4. Tasker, RR, Tsudat, T, Hawrylyshyn, P. Clinical neurophysiological investigation of de-afferentation pain. Adv Pain Res Ther. 1983; 5:713–738.
5. Aszmann, OC, Dellon, ES, Dellon, AL, Anatomical course of the lateral femoral cutaneous nerve and its susceptibility to compression and injury. Plast Recontr Surg. 1977;100(3):600–604. ![]()
6. Hospodar, PP, Ashman, ES, Traub, JA, Anatomic study of the lateral femoral cutaneous nerve with respect to the ilioinguinal surgical dissection. J Orthop Trauma. 1999;13(1):17–19. ![]()
7. Surucu, HS, Tanyeli, E, Sargon, MF, Karahan, ST, An anatomic study of the lateral femoral cutaneous nerve. Surg Radiol Anat. 1997;19(5):307–310. ![]()
8. Grossbard, GD. Meralgia paraesthetica after Perthes’ disease. J Bone Joint Surg. 1981; 63B:572.
9. Macnicol, MF, Thompson, WJ, Idiopathic meralgia paresthetica. Clin Orthop 1990; 254:270–274. ![]()
10. King, BB. Meralgia paraesthetica: report of five cases. Am J Surg. 1941; 52:364.
11. Weikel, AM, Habal, MB, Meralgia paraesthetica: a complication of iliac bone procurement. Plast Reconstr Surg 1977; 60:572. ![]()
12. Boyce, JR, Meralgia paresthetica and tight trousers [letter]. JAMA 1984; 251:1533. ![]()
13. Deal, CL, Canosa, JJ, Meralgia paraesthetica and large abdomens. Ann Intern Med 1982; 96:787. ![]()
14. Segers, M, Vandendriessche, G, Vanderstraeten, G, Meralgia paresthetica. Med Phys 1986; 9:281–285. ![]()
15. Dureja, GP, Gulaya, V, Jayalakshmi, TS, Mandal, P, Management of meralgia paresthetica: a multimodality regimen. Anesth Analg. 1995;80(5):1060–1061. ![]()
16. Streiffer, RH, Meralgia paresthetica. Am Fam Physician. 1986;33(3):141–144. ![]()
17. Warfield, CA, Meralgia paresthetica: causes and cures. Hosp Pract. 1986;21(2):40A. ![]()
18. Jiang, Guo-Xiang, Xu, Wei-Dong, Wang, Al-Hao, Spinal stenosis with meralgia paraesthetica. J Bone Joint Surg 1983; 70B:272–273. ![]()
19. Kallgren, MA, Tingle, LJ, Meralgia paresthetica mimicking lumbar radiculopathy. Anesth Analg 1993; 76:1367–1368. ![]()
20. Trummer, M, Flaschka, G, Unger, F, Eustacchio, S, Lumbar disc herniation mimicking meralgia paresthetica: case report. Surg Neurol. 2000;54(1):80–81. ![]()
21. Eriksson, E. Atlas der Lokalanästhesie. Berlin: Springer; 1980.
22. Keegan, JJ, Holyoke, EA, Meralgia paraesthetica. An anatomical and surgical study. J Neurosurg 1962; 19:341. ![]()
23. Ivins, GK, Meralgia paresthetica, the elusive diagnosis: clinical experience with 14 adult patients. Ann Surg. 2000;232(2):281–286. ![]()
24. Ecker, AD, Woltman, HW. Meralgia paresthetica: a report of one hundred and fifty cases. JAMA. 1938; 110:1650.
25. Letourneau, L, Dessureault, M, Carette, S, Rheumatoid iliopsoas bursitis presenting as unilateral femoral nerve palsy. J Rheumatol. 1991;18(3):462–463. ![]()
26. Holm, P, Roehr, C. An important complication of anticoagulation therapy: a case presentation. South Dakota J Med. 1985; 38:5–8.
27. Young, MR, Norris, JW, Femoral neuropathy during anticoagulant therapy. Neurology 1976; 26:1173–1175. ![]()
28. Nusselder, FA, Franke, CL, Uitval van de nervus femoralis ten gevolge van bloeding bij gebruik van anticoagulantia. Ned Tijdschr Geneeskd 1990; 134:808–811. ![]()
29. Ebraheim, NA, Mekhail, AO, The infrapatellar branch of the saphenous nerve: an anatomic study. J Orthop Trauma. 1997;11(3):195–199. ![]()
30. Aszmann, OC, Ebmer, JM, Dellon, AL, Cutaneous innervation of the medial ankle: an anatomic study of the saphenous, sural, and tibial nerves and their clinical significance. Foot Ankle Int. 1998;19(11):753–756. ![]()
31. Lee, BY, Lapointe, DG, Madden, JL. The adductor canal syndrome. Am J Surg. 1978; 65:465–466.
32. Romanoff, ME, Cory, PC, Kalenak, A, Keyser, GC, Marshall, WK, Saphenous nerve entrapment at the adductor canal. Am J Sports Med 1989; 17:478–481. ![]()
33. Tennent, TD, Birch, NC, Holmes, MJ, Birch, R, Goddard, NJ, Knee pain and the infrapatellar branch of the saphenous nerve. J R Soc Med. 1998;91(11):573–575. ![]()
34. Mens, JMA, Pseudo-artritis van de knie ten gevolge van compressieneuropathie van de nervus saphenus. Ned Tijdschr Geneeskd 1987; 131:1215–1218. ![]()
35. Hemler, DE, Ward, WK, Karstetter, KW, Bryant, PM, Saphenous nerve entrapment caused by pes anserine bursitis mimicking stress fracture of the tibia. Arch Phys Med Rehabil. 1991;72(5):336–337. ![]()
36. Mondelli, M, Reale, F, Cavallaro, T, Neuroma of the sural nerve as a complication of stripping of the small saphenous vein. Surg Neurol. 1997;48(4):330–332. ![]()
37. Mountney, J, Wilkinson, GA, Saphenous neuralgia after coronary artery bypass grafting. Eur J Cardiothorac Surg. 1999;16(4):440–443. ![]()
38. Seror, P, Sural nerve neuropathy (external saphenous) linked to a disease of the small saphenous vein. Apropos of 5 cases. J Mal Vasc. 2000;25(2):128–131. ![]()
39. Brügger, A. Die Erkrankungen des Bewegungsapparates und seines Nervensystems. Stuttgart: Fisher; 1982.
40. Vloka, JD, Hadzic, A, April, E, Thys, DM, The division of the sciatic nerve in the politeal fossa: anatomical implications for popliteal nerve blockade. Anesth Analg. 2001;92(1):215–217. ![]()
41. Hollinshead, WH. Anatomy for Surgeons: The Back and Limbs; vol. 3. Harper & Rowe, Philadelphia, 1982.
42. Möller, BN, Kadin, S, Entrapment of the common peroneal nerve. Am J Sports Med 1987; 15:90–91. ![]()
43. Baima, J, Krivickas, L. Evaluation and treatment of peroneal neuropathy. Curr Rev Musculoskelet Med. 2008; 1(2):147–153.
44. White, J, The result of traction injuries to the common peroneal nerve. J Bone Joint Surg 1968; 50B:346–350. ![]()
45. Togrol, E, Bilateral peroneal nerve palsy induced by prolonged squatting. Mil Med. 2000;165(3):240–242. ![]()
46. Ekelund, EL, Bilateral nerve entrapment in the popliteal space. Am J Sports Med 1990; 18:108. ![]()
47. Leach, RE, Purnell, MB, Saito, A, Peroneal nerve entrapment in runners. Am J Sports Med 1990; 17:287–291. ![]()
48. Aydogdu, S, Cullu, E, Arac, N, Varolgunes, N, Sur, H, Prolonged peroneal nerve dysfunction after high tibial osteotomy: pre- and postoperative electrophysiological study. Knee Surg Sports Traumatol Arthrosc. 2000;8(5):305–308. ![]()
49. Vastamäki, M, Decompression for peroneal nerve entrapment. Acta Orthop Scand 1986; 57:551–554. ![]()
50. Dellon, AL, Deep peroneal nerve entrapment on the dorsum of the foot. Foot Ankle. 1990;11(2):73–80. ![]()
51. Akyuz, G, Us, O, Turan, B, et al, Anterior tarsal tunnel syndrome. Electromyogr Clin Neurophysiol. 2000;40(2):123–128. ![]()
52. Borges, LF, Hullett, M, Selker, DJ, Welsh, K, The anterior tarsal tunnel syndrome. J Neurosurg 1981; 54:89–92. ![]()
53. Marinacci, AA, Neurological syndromes of the tarsal tunnels. Bull Los Angeles Neurol Soc 1968; 33:90–100. ![]()
54. Gessini, L, Jandolo, B, Pietrangeli, A, The anterior tarsal syndrome: report of four cases. J Bone Joint Surg 1984; 66A:786–787. ![]()
55. Krause, KH, Witt Ross, A, The anterior tarsal tunnel syndrome. J Neurol 1977; 217:67–74. ![]()
56. Tibrewall, SB, Goodfellow, JW, Peroneal nerve palsy at the level of the lower third of the leg. J R Soc Med 1984; 77:72–73. ![]()
57. Styf, J, Diagnosis of exercise-induced pain in the lower leg. Am J Sports Med 1988; 16:165–169. ![]()
58. Kernohan, J, Levack, B, Wilson, JN, Entrapment of the superficial peroneal nerve, three case reports. J Bone Joint Surg 1985; 67B:172–173. ![]()
59. Hayes, DW, Jr., Mandracchia, VJ, Webb, GE, Nerve injury associated with plantarflexion–inversion ankle sprains. Clin Podiatr Med Surg. 2000;17(2):361–369. ![]()
60. Sridhara, CA, Izzo, KL, Terminal sensory branches of the superficial peroneal nerve: an entrapment syndrome. Arch Phys Med Rehabil 1985; 66:789–791. ![]()
61. Styf, J, Entrapment of the superficial peroneal nerve. Diagnosis and results of decompression. J Bone Joint Surg 1989; 71B:131–135. ![]()
62. Johnston, EC, Howell, SJ, Tension neuropathy of the superficial peroneal nerve: associated conditions and results of release. Foot Ankle Int. 1999;20(9):576–582. ![]()
63. Oh, SJ, Meyer, RD, Entrapment neuropathies of the tibial (posterior tibial) nerve. Neurol Clin. 1999;17(3):593–615. ![]()
64. Heimkes, B, Posel, P, Stotz, S, Wolf, K, The proximal and distal tarsal tunnel syndromes: an anatomical study. Int Orthop. 1987;11(3):193–196. ![]()
65. Lam, SJS, Tarsal tunnel syndrome. Lancet 1962; 2:1354. ![]()
66. Keck, C. The tarsal tunnel syndrome. J Bone Joint Surg. 1962; 44A:180.
67. Puelo, D, Knudsen, HA, Sharon, SM, Talar exostosis as a cause of tarsal tunnel syndrome. JAMA 1987; 77:147. ![]()
68. Sammarco, GJ, Stephens, MM, Tarsal tunnel syndrome caused by the flexor digitorum accessorius longus. J Bone Joint Surg. 1990;72A(3):453–454. ![]()
69. Radin, EL, Tarsal tunnel syndrome. Clin Orthop 1983; 181:167–170. ![]()
70. Baylan, SP, Paik, SW, Barnert, AL, Ko, KH, Yu, J, Persellin, RH, Prevalence of the tarsal tunnel syndrome in rheumatoid arthritis. Rheum Rehab. 1981;20(3):148–150. ![]()
71. Oloff, L, Jacobs, AM, Jatte, S, Tarsal tunnel sydrome: a manifestation of systemic disease. J Foot Surg 1985; 22:302. ![]()
72. Gould, N, Alvarez, R, Bilateral tarsal tunnel syndrome caused by varicosities. Foot Ankle 1983; 3:290. ![]()
73. Jackson, DC, Tarsal tunnel syndrome in athletes. Am J Sports Med 1991; 1:61–65. ![]()
74. Menon, J, Dorfman, HD, Renbaum, J, Friedler, S, Tarsal tunnel syndrome secondary to neurolemoma of the medial plantar nerve. A case report and review of the literature. J Bone Joint Surg 1980; 62:301–303. ![]()
75. Trepman, E, Kadel, NJ, Chisholm, K, Razzano, L, Effect of foot and ankle position on tarsal tunnel compartment pressure. Foot Ankle Int. 1999;20(11):721–726. ![]()
76. Mondelli, M, Giannini, F, Reale, F, Clinical and electrophysiological findings and follow-up in tarsal tunnel syndrome. Electroencephalogr Clin Neurophysio. 1998;109(5):418–425. ![]()
77. Hammerschlag, WA, Goldner, JL, Bassett, FH. Posterior tibial nerve entrapment: a thirty-three year review. Am Orthop Foot Ankle Soc. 1988; Jul:436–439.
78. Stearn, DS, Joyce, MT, Tarsal tunnel syndrome: a review of 15 surgical procedures. J Foot Surg. 1989;28(4):290–294. ![]()
79. Kaplan, P, Kerham, W, Tarsal tunnel syndrome. J Bone Joint Surg 1981; 63A:96–99. ![]()
80. Ward, PJ, Porter, ML, Tarsal tunnel syndrome: a study of the clinical and neurophysiological results of decompression. J R Coll Surg Edin. 1998;43(1):35–36. ![]()
81. Turan, I, Rivero-Melian, C, Guntner, P, Rolf, C, Tarsal tunnel syndrome. Outcome of surgery in longstanding cases. Clin Orthop 1997; 343:151–156. ![]()
82. Krishnan, KG, Pinzer, T, Schackert, G, A novel endoscopic technique in treating single nerve entrapment syndromes with special attention to ulnar nerve transposition and tarsal tunnel release: Clinical application. Neurosurgery 2006; 59:89–100. ![]()
83. Doxey, GE. Calcaneal pain: a review of various disorders. J Orthop Sport Phys Ther. 1987; 9:25–32.
84. Henricson, AS, Westlin, NE, Chronic calcaneal pain in athletes: entrapment of the calcaneal nerve? Am J Sports Med. 1984;12(2):152–154. ![]()
85. Baxter, DE, Pfeffer, GB, Thigpen, M, Chronic heel pain: treatment rationale. Orthop Clin North Am 1989; 20:563–569. ![]()
86. Kenzora, JE, The painful heel syndrome: an entrapment neuropathy. Bull Joint Dis Orthop Inst. 1987;47(2):178–189. ![]()