Chapter 668 Leg-Length Discrepancy
Leg-length discrepancy (LLD), or anisomelia, in children can result from a variety of congenital or acquired conditions (see Table 668-1 on the Nelson Textbook of Pediatrics website at www.expertconsult.com ![]() ). Congenital conditions include asymmetrical growth from hemihypertrophy, vascular and lymphatic anomalies, Beckwith-Wiedemann syndrome, hemiatrophy, bone dysplasias (proximal femoral focal deficiency [PFFD]), fibular and tibial hemimelia (see Fig. 668-1 on the Nelson Textbook of Pediatrics website at www.expertconsult.com
). Congenital conditions include asymmetrical growth from hemihypertrophy, vascular and lymphatic anomalies, Beckwith-Wiedemann syndrome, hemiatrophy, bone dysplasias (proximal femoral focal deficiency [PFFD]), fibular and tibial hemimelia (see Fig. 668-1 on the Nelson Textbook of Pediatrics website at www.expertconsult.com ![]() ), and Proteus syndrome. Associated acquired causes of limb length inequality include physeal fractures, infections involving the growth plate, fractures whose healing process stimulates growth, juvenile rheumatoid arthritis, and coxa vara. Neurologic diseases including spina bifida, cerebral palsy, head injury, and spinal dysraphisms, can also lead to LLD. These etiologies lead to structural limb length discrepancies, but soft tissue contractures of the lower extremity can also cause functional limb discrepancies even though the bones are of symmetrical length. Hip dysplasia can cause apparent limb length inequality of a functional type.
), and Proteus syndrome. Associated acquired causes of limb length inequality include physeal fractures, infections involving the growth plate, fractures whose healing process stimulates growth, juvenile rheumatoid arthritis, and coxa vara. Neurologic diseases including spina bifida, cerebral palsy, head injury, and spinal dysraphisms, can also lead to LLD. These etiologies lead to structural limb length discrepancies, but soft tissue contractures of the lower extremity can also cause functional limb discrepancies even though the bones are of symmetrical length. Hip dysplasia can cause apparent limb length inequality of a functional type.
Table 668-1 CAUSES OF LEG-LENGTH DISCREPANCY
CONGENITAL CAUSES
Defects in Growth
Bone Tumors and Bone Disease
Vascular
Miscellaneous
ACQUIRED CAUSES
Trauma
Developmental
Developmental dysplasia of the hip
Neoplastic
Neurologic
Infections and inflammatory
Miscellaneous
Diagnosis and Clinical Findings
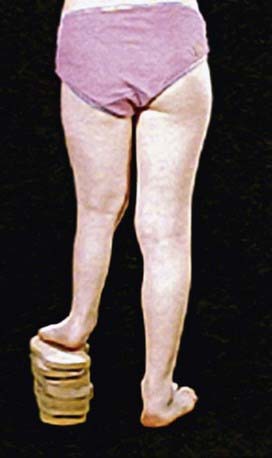
A diagnosis of leg-length inequality can be made by a pediatrician at a regular visit in infancy or early childhood or by a pediatric orthopaedic surgeon at a referral for an obvious limp in an older child. The initial diagnosis of LLD is made on physical examination, with gait asymmetry being the most common complaint. The traditional measurements of real and apparent leg-length inequality (measuring with a tape measure from the medial malleolus to the umbilicus or iliac crest) have led to inaccurate measurements. A more reliable method of clinically testing for limb length inequality is simple visual assessment of the posterior iliac crest level while the child is standing with his or her knees and hips in an extended fashion. Blocks of various sizes can then be placed under the short limb until the pelvis is level to give an estimate of the leg-length inequality (Fig. 668-2). Physical examination can also identify joint contractures and angular deformities that cause errors in clinical and radiologic measurements.
Radiographic Evaluation
Coupled with clinical examination, radiologic evaluation is used to guide the appropriate treatment decisions. Four different techniques are the most commonly used (Fig. 668-3): teleoroentgenogram, orthoroentgenogram, scanogram, and CT. Whichever method is initially used should remain consistent in all future studies in order to maximize accuracy and validity.
Treatment
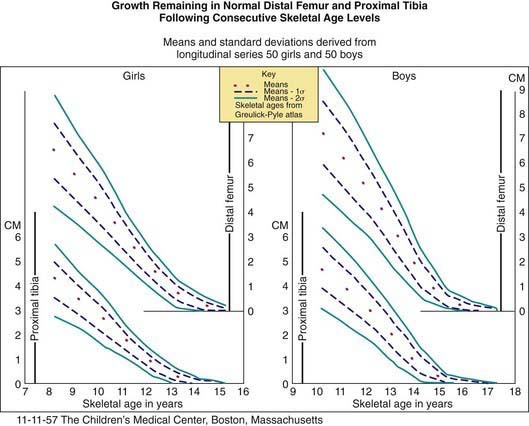
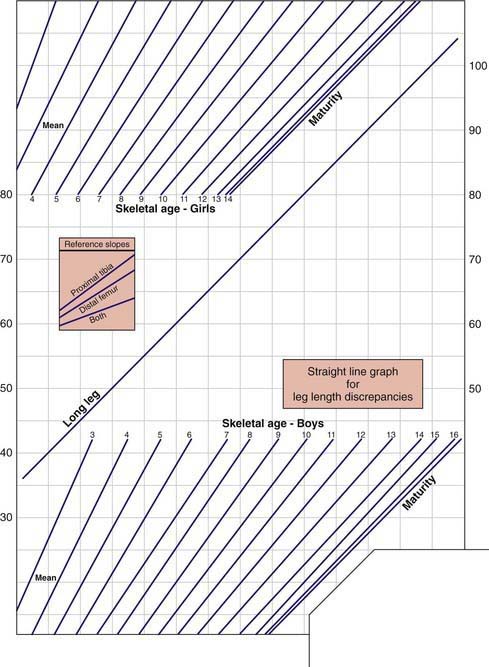
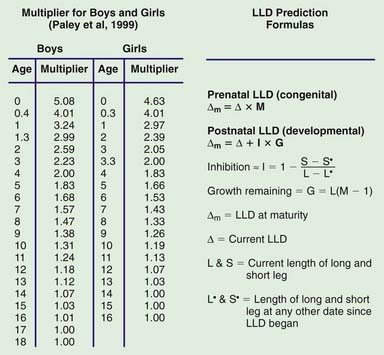
Certain techniques can be used to determine the appropriate timing of epiphysiodesis. These consist of the Menelaus method [estimated discrepancy = current discrepancy + (years remaining × discrepancy per year)], the Green and Anderson method (Fig. 668-4), the Moseley straight-line graph method (Fig. 668-5), and the Paley multiplier method (Fig. 668-6). The most common surgical technique used is the percutaneous drill epiphysiodesis. In this outpatient procedure with very few complications, the physis is either ablated with a drill and curette under high image intensification or screws are inserted across the physis. Temporary epiphyseodesis can also be obtained using plates and screws across a growing physis. Once the amount of correction has been achieved, the staples or screws and plates are removed, thus allowing growth to resume. After skeletal maturity and for corrections of 2-5 cm, acute shortening can be performed at the femur or tibia and fibula by resection and internal fixation. This method is rarely used for correction of >3 cm because of permanent weakness of the surrounding muscles.
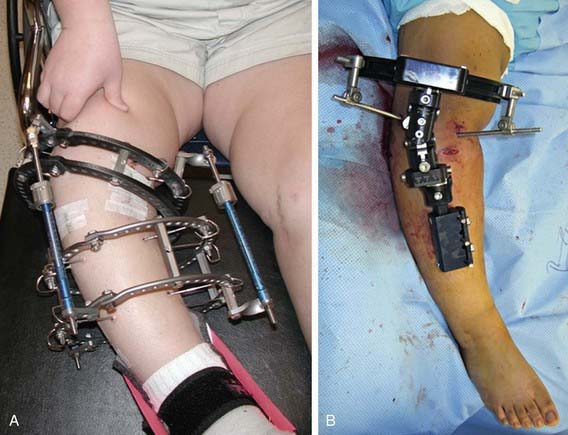
Discrepancy >5-8 cm may be treated with lengthening of the short limb. This technique would not be used if the discrepancy were secondary to overgrowth of a limb, in which case a limb-shortening method would be favored in order to preserve the original body proportions. Children with expected discrepancies >5-6 cm, though, often require one or more limb-lengthening procedures conducted several years apart with or without an epiphysiodesis of the longer limb. The most common technique used for limb-lengthening involves placing an external fixator, either a monolateral or a ring fixator (Fig. 668-7). An external fixator is then applied to the limb to be lengthened and an osteotomy is performed, through which distraction is obtained. The usual rate of lengthening is about 1 mm per day (i.e., approximately 30 mm per month), and it takes approximately 1 mo in the external fixator for each centimeter lengthened. A maximum of about 15-25% of the original length of the bone may be gained during each lengthening session depending on the etiology. More length is achieved from the normal bone shortened by physeal injury, whereas less is achieved from congenital deficiencies. Simultaneous correction of angular, translational, and rotational deformities can also be obtained with both the circular and the newer generation of monolateral fixators. Complications include pin tract infection or wound infection, hypertension, joint subluxation, dislocation of the hip and knee, muscle contracture, premature consolidation, delayed union of bone, stiffness of adjacent joints, implant-related problems, slight over- or undercorrection of the bone’s length, and fatigue fractures following the removal of the lengthening apparatus. To prevent some of the complications, regular follow-up visits to the clinician’s office, meticulous cleaning of the area around the pins and wires, careful adjustment of the frame several times weekly, and physical rehabilitation to further stretch and maintain joint flexibility are essential to improving the quality of care.
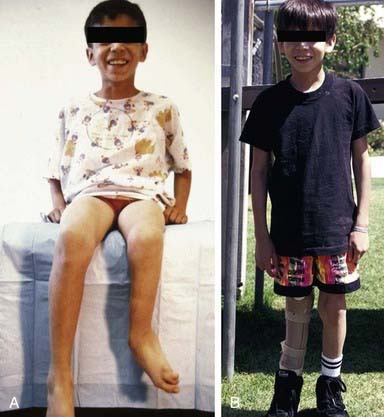
Children with projected discrepancies >18-20 cm (requiring >3 limb lengthenings), especially when there are coexisting deformities or deficiencies of the ipsilateral foot (Fig. 668-8), might benefit from early amputation, rotation of the ankle to function as a knee, and prosthetic fitting for the best long-term function. The other alternative would be multiple reconstructive procedures throughout childhood and adolescence. The potential impact on the child’s psychosocial development, combined with his or her emotional and physical challenges and future restrictions of activities or abilities must be kept in mind when formulating an individualized treatment plan in these complex cases.
Friend L, Widmann RF. Advances in management of limb length discrepancy and lower limb deformity. Curr Opin Pediatr. 2008;20(1):46-51.
Lampasi M, Launay F, Jouve JL, et al. Femoral lengthening over elastic stable intramedullary nailing in children using the monolateral external fixator. Musculoskelet Surg. 2009;93:57-64.
Little DG, Nigo L, Aiona MD. Deficiencies of current methods for the timing of epiphysiodesis. J Pediatr Orthop. 1996;16:173-179.
Menelaus MB. Correction of leg length discrepancy by epiphyseal arrest. J Bone Joint Surg Br. 1996;48:336-339.
Moraal JM, Elzinga-Plomp A, Jongmans MJ, et al. Long-term psychosocial functioning after Ilizarov limb lengthening during childhood. Acta Orthop. 2009;80(6):704-710.
Moseley CF. Leg length discrepancy, ed 6. Morrissey RT, Weinstein SL, editors. Lovell and Winter’s pediatric orthopaedics, vol 2. Lippincott Williams & Wilkins, Philadelphia, 2006;1251-1256.
Niemelä BJ, Tiernström B, Andersson G, et al. Does leg lengthening pose a threat to a child’s mental health? An interim report one year after surgery. J Pediatr Orthop. 2007;27(6):611-617.
Paley D, Bhave A, Herzenberg JE, et al. Multiplier method for predicting limb-length discrepancy. J Bone Joint Surg Am. 2000;82:1432-1446.
Perttunen JR, Anttila E, Södergård J, et al. Gait asymmetry in patients with limb length discrepancy. Scand J Med Sci Sports. 2004;14(1):49-56.
Pritchett JW. Comparison of methods for prediction of lower-extremity growth. J Bone Joint Surg Am. 2001;83:1108-1110.
Sabharwal S, Kumar A. Methods for assessing leg length discrepancy. Clin Orthop Relat Res. 2008;466(12):2910-2922.
Sabharwal S, Zhao C, McKeon J, et al. Reliability analysis for radiographic measurement of limb length discrepancy: full-length standing anteroposterior radiograph versus scanogram. J Pediatr Orthop. 2007;27(1):46-50.
Stanitski DF. Limb-length inequality: assessment and treatment options. J Am Acad Orthop Surg. 1999;7:143-153.
Stricker SK, Hunt T. Evaluation of leg length discrepancy in children. Int Pediatr. 2004;19(3):134-142.
Vitale MA, Choe JC, Sesko AM, et al. The effect of limb length discrepancy on health-related quality of life: is the “2 cm rule” appropriate? J Pediatr Orthop B. 2006;15(1):1-5.
Weiner DS. Leg length discrepancy. In: Weiner DS, Jones K, editors. Pediatric orthopedics for primary care physicians. ed 2. New York: Cambridge University Press; 2004:118-121.