CHAPTER 48 Lateral Collateral Ligament Insufficiency
INTRODUCTION
The lateral collateral ligament complex is one of the main structures implicated in the stability of the elbow joint. Insufficiency of the lateral collateral ligament com-plex is present in many patients with elbow instability. Several basic science and clinical studies have im-proved our understanding of the contributions of the lateral collateral ligament complex to elbow stability, the etiology of lateral collateral ligament insufficiency, the value of different clinical and imaging tests for identification of this entity, and the outcome of surgical repair or reconstruction. The term posterolateral rotatory instability has been coined to describe the clinical condition that results from lateral collateral ligament complex insufficiency.25
BASIC SCIENCE
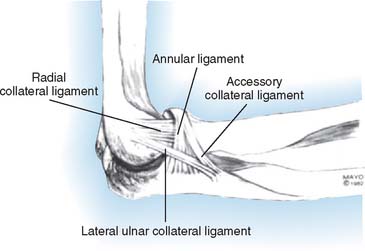
Several ligamentous structures may be identified on the lateral aspect of the elbow joint (see Chapter 2). The ligamentous fibers connecting the lateral humeral epicondyle with the lateral aspect of the ulna seem to be the most important for elbow stability on the lateral side. These fibers, commonly referred to as lateral ulnar collateral ligament,22 attach distally into the tubercle of the supinator crest (Fig. 48-1). More anterior fibers originated at the lateral humeral epicondyle, named by some as radial collateral ligament, blend with the fibers of the annular ligament. Unlike the medial side of the joint, morphologic and histologic studies have not been able to show distinct ligaments on the lateral side of the joint consistently.5,14
Lateral collateral ligament complex insufficiency allows excessive posterolateral displacement of the proximal forearm relative to the distal humerus. The contribution of the lateral collateral ligament complex to elbow stability has been investigated in several cadaveric models. Release of the whole lateral collateral ligament complex has been required in most experimental settings to produce a significant increase in varus and posterolateral displacements.5,8,13,27,29,35 Isolated section of the ulnar insertion of the lateral ulnar collateral ligament has not been shown to promote dramatic elbow instability in all cadaveric studies.5,27–29 However, reconstruction of the lateral ulnar collateral ligament with a tendon graft restores varus and posterolateral stability in the laboratory.17 The overlying common extensor-supinator group has also been shown to play a major role in elbow stability.5,9 There is a complex interplay be-tween the lateral collateral ligament complex and other elbow structures, including the coronoid and radial head.6,7,15,34
ETIOLOGY
TRAUMA
The lateral collateral ligament complex may be damaged as a result of trauma to the elbow, resulting in elbow dislocation, fracture-dislocation, subluxation, or ligamentous sprain (Box 48-1). McKee et al.21 reported on the soft tissue injury patterns identified in 10 dislocations and 52 fracture-dislocations treated surgically. The lateral collateral ligament complex was disrupted in all cases; proximal avulsion was the most common failure mode, followed by midsubstance rupture. The common extensor-supinator group was injured in 66% of the cases. The anterior bundle of the medial collateral ligament was injured in approximately 50% of the cases. Less severe injuries causing dislocation or an elbow sprain (usually hyperextension or varus stress) may also damage the lateral collateral ligament complex if they place substantial strain on the ligament fibers.
When injured, the medial collateral ligament seems to heal without residual clinically significant medial-sided instability in most patients.10 On the contrary, persistent lateral-sided instability seems to be more frequent, but the reasons are unclear: It may be related to a decreased healing potential, as seen in other anatomic locations such as the lateral side of the knee joint; the constant tensile gravitational loads imposed on the injured lateral side with elbow use; or the more common association with additional injuries such as radial head or coronoid fractures. Lateral collateral ligament insufficiency should be suspected in patients with recurrent dislocation, subjective instability, lateral-sided pain, and a history of elbow trauma.
CHRONIC ATTRITION
Chronic attrition secondary to repetitive valgus stress is a well-known mechanism leading to medial collateral ligament insufficiency. Chronic attrition of the lateral collateral ligament complex may occur in rare situations such as long-term crutch-walkers (paraplegics, poliomyelitis). Post-traumatic or congenital cubitus varus deformity is recognized as a risk factor for chronic attrition of the lateral collateral ligament complex and tardy posterolateral rotatory instability.1,26 With varus malalignment, triceps contraction has been hypothesized to force posterolateral rotatory subluxation and eventually lead to attenuation of the lateral collateral ligament complex. In addition, one cadaveric study has shown increased strain on the lateral collateral ligament complex with more than 25 degrees of varus deformity and lateral joint line opening with more than 20 degrees of varus deformity.3 In this setting, corrective osteotomy should be considered as an adjunct to lateral collateral ligament reconstruction to prevent failure. Insufficiency of the lateral collateral ligament has also been identified in patients with tennis elbow and no prior surgery16; insufficiency in this setting may be secondary to ligamentous involvement by the same pathologic process affecting the common extensor group4 or the detrimental side effects on collagen fibers of repeated steroid injections.4,16
IATROGENIC INJURY
Inadvertent damage of the lateral collateral ligament may occur during surgical procedures on the lateral side of the joint. Surgical treatment of tennis elbow may compromise the lateral collateral ligament complex if the release or débridement of the common extensor origin are too extensive, especially when the lateral epicondyle is denuded off soft tissues. Exposure of the radial head or capitellum for fracture fixation or chronic reconstruction may also jeopardize the lateral collateral ligament complex, especially when Köcher’s interval is used or the joint needs to be subluxed or dislocated in order to complete the surgical procedure.12,23,33 Special attention is required when performing surgery on the lateral side of the elbow joint to avoid damage to the lateral collateral ligament complex. Formal repair of the damaged ligament should always be part of the wound closure.
DIAGNOSIS
PRESENTATION
The clinical expression of lateral collateral ligament complex insufficiency varies considerably depending on the etiology, severity, associated pathology, previous surgery, and activity level (Box 48-2). Some patients may complain of recurrent episodes of frank elbow dislocation. However, most commonly patients complain of more subtle symptoms, including lateral-sided elbow pain, mechanical symptoms (clicking, catching, snapping, locking) or subjective instability.33 Patients with ligamentous insufficiency after a fracture-dislocation may present with more severe pain or stiffness secondary to the associated injuries. Commonly, most patients with lateral collateral ligament complex insufficiency report a previous history of trauma or surgery. In patients with previous surgery, it is important to determine if the preoperative symptoms were corrected by the surgery or if on the contrary surgery had no effect or occasioned a whole new constellation of symptoms.
Subtle elbow instability is reflected by the inability of the patient to push with the affected upper extremity to stand up from a seat,31 open a heavy door, or similar activities that require active elbow extension against resistance with forearm supination. However, instability episodes are difficult to identify as such by the patient, who often reports pain when attempting to perform the above-mentioned activities.
PHYSICAL EXAMINATION
A detailed physical examination should help identify basic information such as the specific location of the pain and elbow range of motion (see Chapter 4). The location of previous skin incisions and the presence of deformity should be noted. As mentioned earlier, cubitus varus predisposes to tardy posterolateral rotatory instability. In addition, lateral skin incisions centered posterior to the midcoronal plane may be associated with inadvertent ligamentous damage. The integrity of the medial and lateral collateral ligament complex should be tested in all cases. Examination maneuvers for instability may be masked by associated pathology (stiffness or an absent radial head, for example). In the author’s experience, pure varus stress does not allow reliable assessment of the competency of the lateral structures. Several other physical examination maneuvers have been described to specifically test the lateral collateral ligament complex:
Posterolateral Rotatory Drawer Test
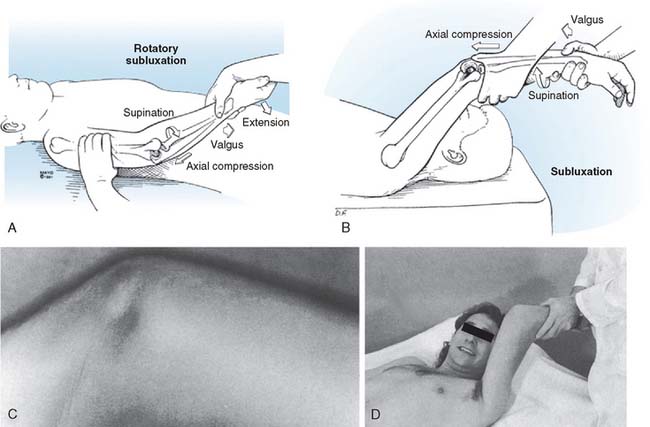
This test demonstrates posterolateral subluxation of the proximal radius and ulna with forced supination. It is best performed with the patient laying supine and the upper extremity overhead to lock the shoulder in internal rotation (Fig. 48-2). Forced supination of the forearm in approximately 45 degrees of flexion will induce abnormal excessive posterolateral subluxation of the elbow. The test is best demonstrated when forced supination is combined with valgus torque and axial compression. In some cases, subluxation may not be demonstrated but patients show apprehension with the maneuver.24
Posterolateral Rotatory Pivot-Shift Test
This test demonstrates posterolateral subluxation and relocation of the elbow joint with elbow flexion and extension while applying a valgus and supination moment to the forearm. The patient is examined in the same position described earlier (Fig. 48-3). Application of valgus, axial compression, and hypersupination to the elbow in approximately 20 degrees of flexion induces posterolateral subluxation seen as prominence of the radial head and dimpling of the skin between the proximal radius and ulna. Progressive elbow flexion while maintaining the valgus, compression, and supination torque is accompanied by a sudden rotatory shift and clunk as the elbow is reduced with flexion.24 Again, the shift cannot be demonstrated in every patient, but most report apprehension. In patients with an absent radial head, the clunk is less pronounced.
Chair and Push-Up Apprehension
The chair sign involves having the patient stand up from a chair while pushing with the upper extremities and keeping the forearms in supination and the arms abducted to greater than the shoulder width.31 The test is considered positive if there is reluctance to extend the elbow fully as the patient raises his body using exclusively upper extremity force or a dislocation occurs. The push-up sign involves having the patient perform an active floor or wall push-up with the forearms supinated and the arms abducted to greater than the shoulder width. The test is considered positive if the patient shows reluctance to fully extend the elbow or a dislocation occurs. A similar test has been described with the patient pushing against the top of a table.2 Patients report apprehension when asked to perform a press-up with the elbow pointing laterally; pain and apprehension occurs as the elbow reaches approximately 40 degrees of flexion. Symptoms improve when the test is repeated using the thumb of the examiner to push over the radial head, giving support and preventing posterior subluxation.
IMAGING STUDIES
Stress Radiographs and Fluoroscopy
Radiographic or fluoroscopic imaging of the elbow subjected to stress is an invaluable diagnostic tool in patients with posterolateral rotatory instability, especially when the patient is under anesthesia. The status of the medial collateral ligament should be documented first by applying a valgus load to the extended elbow with the forearm in pronation28; more than 2 mm of medial joint line opening on the anteroposterior view indicates medial collateral ligament insufficiency. The forearm is then placed in full supination and a varus load is applied to determine the amount of lateral joint line opening; again, more than a 2-mm of opening usually indicates lateral collateral ligament insufficiency. However, posterolateral rotatory instability is best demonstrated on the lateral views (Fig. 48-4); with forced supination and valgus, the radius and ulna are subluxed posteriorly so that the center of the radial head does no longer align with the center of the capitellum and there is asymmetry and widening of the ulnohumeral joint.
Magnetic Resonance Imaging
The different components of the lateral collateral ligament complex may be visualized on magnetic resonance imaging.30 Although insufficiency of this ligament com-plex is diagnosed in most patients based on the history, physical examination and stress radiographs or fluoroscopy, magnetic resonance may confirm the presence of a torn or attenuated complex. Some studies have identified selective deficiency of the posterior fibers of the complex lateral ulnar collateral ligament.30 However, negative findings on magnetic resonance imaging does not exclude the diagnosis of posterolateral rotatory instability.11 Magnetic resonance imaging may be especially useful in patients with tennis elbow and coexistent ligamentous insufficiency.4
TREATMENT
ACUTE INJURIES
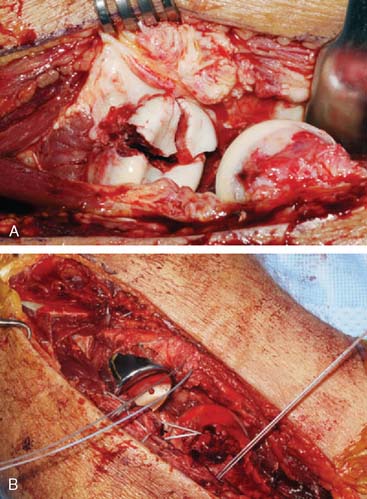
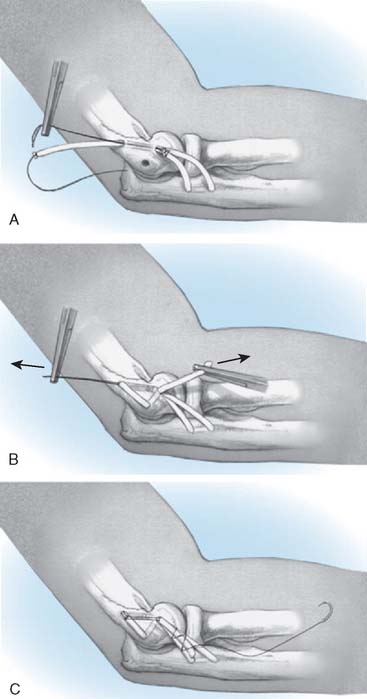
Injury to the lateral collateral ligament complex is found in most elbow fracture-dislocations that are treated surgically (Fig. 48-5A). In these circumstances, formal repair is recommended. The lateral collateral ligament complex is usually avulsed from the epicondyle or torn in its midsubstance.21 Our preferred technique for surgical repair of acute injuries involves the use of a heavy nonabsorbable suture through the substance of the lateral collateral ligament complex and into the humeral epicondyle.
The suture follows the line of tension of the lateral ulnar collateral ligament. One #2 Fiberwire (Arthrex Inc., Naples, FL) or #5 Ethibond (Ethicon Johnson and Johnson, New Brunswick, NJ) suture is placed on the anterior half of the capsuloligamentous fibers in a running locking configuration18 from proximal to distal, and then from distal to proximal, turning at the ulnar supinator crest (see Fig. 48-5B). A second suture is placed in the same fashion on the posterior half of the capsuloligamentous fibers. These sutures may be passed through the overlying common extensor-supinator fibers to augment the repair. The isometric point of humeral attachment is then located at the geometric center of the capitellum and bone tunnels are created starting at that point and aiming anteriorly and posteriorly. The sutures are passed through the tunnels and tied on the proximal aspect of the lateral epicondyle. Postoperative management should follow the same general principles described for reconstruction in the chronic setting.
CHRONIC INSUFFICIENCY
Symptomatic insufficiency of the lateral collateral ligament complex is best addressed surgically by reconstruction using a tendon graft. Ligament repair or imbrication have been shown to provide inferior results in the chronic setting.19,33
Surgical Technique
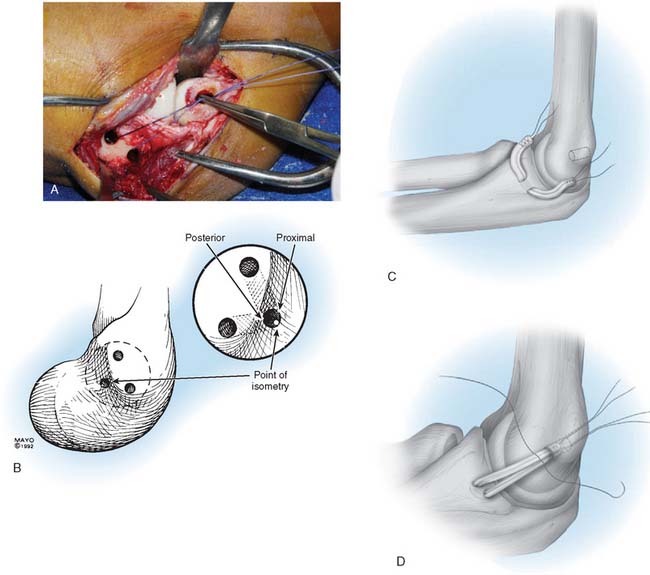
The tunnels for insertion of the tendon graft into the ulna and humerus are created next (Fig. 48-6A). One hole of the ulnar tunnel is centered over the tubercle of the supinator crest, which can easily be felt by palpation. The second hole is placed proximally and posteriorly leaving a bone bridge wide enough to avoid fracture (usually between 1 and 1.5 cm). A towel clip or angled curette may be used to clear the tunnel of bone debris.
The site for humeral attachment of the tendon graft is selected so that the reconstruction will be isometric and maintain the same tension throughout the flexion-extension arc.22 The first humeral hole is centered slightly proximal and posterior to the point of isometry. Usually, the point of isometry is located at the geometric center of the capitellar articular surface; this is confirmed with a suture placed through the ulnar tunnel and grasped with a point used to select the point on the surface of the humeral epicondyle, where the suture will maintain the same approximate tension with elbow flexion and extension (see Fig. 48-6A). Next, two proximal exit holes are created on the anterior and posterior aspect of the lateral humeral column, and the anterior and posterior humeral tunnels are created (see Fig. 48-6B).
Several options exist for tendon graft selection. Palmaris longus autograft was used in the first reports of the technique.23 Tendon allografts seem to be associated with the same outcome and eliminate the morbidity and additional surgical time associated with autograft harvesting. We currently favor the use of plantaris or semitendinosus allograft depending on the size of the patient. Two #2 Fiberwire can be placed at the ends of the tendon graft in a running locking configuration to pull the tendon through the tunnels and assist in graft attachment.
The graft may be looped through the tunnels in different ways, which seem to be equally effective as long as they allow adequate tensioning of the reconstruction.17 The tendon graft is passed first through the ulnar tunnel. Depending on the size of the graft as well as surgeon preferences, the two ends of the tendon graft can be then docked into the anterior and posterior humeral tunnels, tying the sutures over the proximal aspect of the humeral epicondyle (see Fig. 48-6C). Alternatively, one end of the tendon graft may be sutured to the opposite limb at the entrance into the humeral tunnels creating a yoke-like structure. The longer limb is passed though the posterior tunnel, over the top, and into the anterior tunnel. Traction is then placed at the end of the yoke and the end of the longer limb to tension the graft (Fig. 48-7).
Whenever possible, any remaining capsule should be sutured to seal the joint before the graft reconstruction is completed so that the graft remains extra-articular. The graft should be tensioned with the joint in a reduced position, the forearm in full pronation, and the elbow in approximately 45 degrees of flexion. Tensioning may be increased by suturing the two limbs of the graft together in one or more points.
Treatment of Associated Pathology
Associated pathology is addressed as needed. Commonly, lateral collateral ligament complex insufficiency is associated to radial head nonunion, malunion or resection, as well as coronoid deficiency. Radial head replacement or coronoid reconstruction may be required to completely restore elbow stability and function.6,7,15,34 Patients with posterolateral rotatory instability and associated tennis elbow require débridement and repair of the area of tendinosis at the time of ligamentous reconstruction. Interestingly, some patients may present with a combination of stiffness and ligamentous insufficiency, and require ligamentous reconstruction and contracture release as a single or staged procedure. It is important to understand the need to consider reconstruction of the radial head to improve the outcome of treatment.
Underlying Deformity
As mentioned earlier, posterolateral rotatory instability may be secondary to chronic ligamentous attrition secondary to cubitus varus deformity. Depending on the severity of the deformity and the cosmetics concerns of the patient, a valgus-producing distal humerus osteotomy may need to be associated to the ligamentous reconstruction. Otherwise, the reconstruction may fail by chronic attrition of the tendon graft subjected to abnormal forces. Osteotomy should probably be considered in patients with more than 15 degrees of varus angulation.26 Experimental data in cadavers has shown increased strain on the lateral collateral ligament complex with more than 25 degrees of varus angulation and increased opening of the joint line space with more than 20 degrees of varus angulation.3
Postoperative Management
The ligamentous reconstruction needs to be protected for the first few weeks after surgery in order to prevent graft stretching and recurrent instability. Elbow extension and forearm supination increase tension on the graft; pronation5 and active muscle contraction protect the graft.9 Initially after surgery, the elbow is immobilized in 90 degrees of flexion and forearm pronation. Motion may be initiated in a few days, as long as a brace is used to neutralize the forces across the elbow, maintain the forearm in pronation, and block extension beyond 30 degrees. However, cast immobilization for three to six weeks should be considered when compliance with postoperative protection is questionable, and it is recommended by some surgeons for most patients, provided they do not show a tendency to develop stiffness. Neutralization using a dynamic external fixator during 3 to 6 weeks should be considered for those cases in which more protection is needed; external fixation has occasionally been used as the main treatment modality.20,32 Postoperative management may need to be changed to accommodate associated surgical procedures such as contracture release, in which early motion is more critical.
The patient should understand the detrimental role of gravitational stresses on the lateral collateral ligament complex. Most activities of daily living place the lateral side of the elbow facing upward; the weight of the forearm and any additional weight held by the hand will result in tensile stresses on the lateral elbow structures. During the first 3 months after surgery, the patient should learn how to protect the elbow against gravitational stresses. Active overhead flexion and extension exercises with the forearm in pronation protect the lateral collateral ligament reconstruction by avoiding gravitational stresses and increasing joint stability through active muscle contraction.9 Exercises to increase the strength of the extensor-supinator group also help stabilize the joint, and they may be initiated during the first few days after surgery. Unrestricted activities are usually allowed 6 months after surgery.
Outcome
Nestor et al.23 reported the initial experience at the Mayo Clinic with 11 consecutive cases followed for a mean of 3.5 years (range, 2 to 5.6 years). The lateral collateral ligament complex was imbricated in three patients and reconstructed with a tendon graft (seven patients) or triceps fascia (one patient). Stability was obtained in 10 patients, and seven were considered to have an excellent functional result.
More recently, Sanchez-Sotelo et al.33 updated the Mayo Clinic experience with 44 cases followed for a mean of 6 years (2 to 15 years). Ligament repair or imbrication was performed in 12 cases and formal ligament reconstruction in 32. Surgery restored stability in all but five patients. Results were considered satisfactory in 73% of the cases, and 86% of the patients were subjectively satisfied with the procedure. Interestingly, the results were better in patients with traumatic etiology and subjective instability. Tendon reconstruction provided a better result than ligament repair.
Other authors have reported similar outcomes in the treatment of this condition. Lee et al.19 reported on 10 patients with posterolateral rotatory instability treated with ligament repair (four cases) or reconstruction (six cases). Instability was corrected in all cases, and results were graded as satisfactory in eight patients. All patients with an excellent result had reconstruction with a tendon graft, a finding consistent with the above-mentioned study from the Mayo Clinic. When patients present with posterolateral rotatory instability and a resected radial head, reconstruction of the lateral collateral ligament complex combined with radial head replacement seems to provide satisfactory results.12,23,33 Arthroscopic capsular plication37 and arthroscopic electrothermal shrinkage36 have been reported as an alternative to tendon reconstruction, but the findings of better overall results with tendon reconstruction versus ligament repair19,33 and the concerns raised by the use of electrothermal shrinkage of the shoulder make arthroscopic surgery less attractive for the treatment of posterolateral rotatory instability.
O’Driscoll et al.26 specifically reported on the outcome of surgical treatment for tardy posterolateral rotatory instability associated with cubitus varus. Twenty-one elbows were treated with osteotomy combined with reconstruction of the lateral collateral ligament complex (seven patients), ligament reconstruction alone (10 patients), or osteotomy alone (four patients) and followed for a mean of 3 years. Ulnar nerve transposition with or without triceps transposition was required in five patients. At most recent follow-up, three patients had persistent posterolateral rotatory instability, and two of these were rated as poor due to associated arthritis with severe pain.
1 Abe M., Ishizu T., Morikawa J. Posterolateral rotatory instability of the elbow after posttraumatic cubitus varus. J. Shoulder Elbow Surg. 1997;6:405.
2 Arvind C.H., Hargreaves D.G. Table top relocation test—New clinical test for posterolateral rotatory instability of the elbow. J. Shoulder Elbow Surg. 2006;15:500.
3 Beuerlein M.J., Reid J.T., Schemitsch E.H., McKee M.D. Effect of distal humeral varus deformity on strain in the lateral ulnar collateral ligament and ulnohumeral joint stability. J. Bone Joint Surg. Am. 2004;86-A:2235.
4 Bredella M.A., Tirman P.F., Fritz R.C., Feller J.F., Wischer T.K., Genant H.K. MR imaging findings of lateral ulnar collateral ligament abnormalities in patients with lateral epicondylitis. Am. J. Roentgenol. 1999;173:1379.
5 Cohen M.S., Hastings H.2nd. Rotatory instability of the elbow. The anatomy and role of the lateral stabilizers. J. Bone Joint Surg. Am. 1997;79:225.
6 Deutch S.R., Jensen S.L., Tyrdal S., Olsen B.S., Sneppen O. Elbow joint stability following experimental osteoligamentous injury and reconstruction. J. Shoulder Elbow Surg. 2003;12:466.
7 Doornberg J., Ring D., Jupiter J.B. Effective treatment of fracture-dislocations of the olecranon requires a stable trochlear notch. Clin. Orthop. Relat. Res. 2004;42:292.
8 Dunning C.E., Zarzour Z.D., Patterson S.D., Johnson J.A., King G.J. Ligamentous stabilizers against posterolateral rotatory instability of the elbow. J. Bone Joint Surg. Am. 2001;83-A:1823.
9 Dunning C.E., Zarzour Z.D., Patterson S.D., Johnson J.A., King G.J. Muscle forces and pronation stabilize the lateral ligament deficient elbow. Clin. Orthop. Relat. Res. 2001;388:118.
10 Eygendaal D., Verdegaal S.H., Obermann W.R., van Vugt A.B., Poll R.G., Rozing P.M. Posterolateral dislocation of the elbow joint. Relationship to medial instability. J. Bone Joint Surg Am. 2000;82:555.
11 Grafe M.W., McAdams T.R., Beaulieu C.F., Ladd A.L. Magnetic resonance imaging in diagnosis of chronic posterolateral rotatory instability of the elbow. Am. J. Orthop. 2003;32:501. discussion 504
12 Hall J.A., McKee M.D. Posterolateral rotatory instability of the elbow following radial head resection. J. Bone Joint Surg. Am. 2005;87:1571.
13 Hannouche D., Begue T. Functional anatomy of the lateral collateral ligament complex of the elbow. Surg. Radiol. Anat. 1999;21:187.
14 Imatani J., Ogura T., Morito Y., Hashizume H., Inoue H. Anatomic and histologic studies of lateral collateral ligament complex of the elbow joint. J. Shoulder Elbow Surg. 1999;8:625.
15 Jensen S.L., Olsen B.S., Tyrdal S., Sojbjerg J.O., Sneppen O. Elbow joint laxity after experimental radial head excision and lateral collateral ligament rupture: efficacy of prosthetic replacement and ligament repair. J. Shoulder Elbow Surg. 2005;14:78.
16 Kalainov D.M., Cohen M.S. Posterolateral rotatory instability of the elbow in association with lateral epicondylitis. A report of three cases. J. Bone Joint Surg. Am. 2005;87:1120.
17 King G.J., Dunning C.E., Zarzour Z.D., Patterson S.D., Johnson J.A. Single-strand reconstruction of the lateral ulnar collateral ligament restores varus and posterolateral rotatory stability of the elbow. J. Shoulder Elbow Surg. 2002;11:60.
18 Krackow K.A., Thomas S.C., Jones L.C. Ligament-tendon fixation: analysis of a new stitch and comparison with standard techniques. Orthopedics. 1988;11:909.
19 Lee B.P., Teo L.H. Surgical reconstruction for posterolateral rotatory instability of the elbow. J. Shoulder Elbow Surg. 2003;12:476.
20 McKee M.D., Bowden S.H., King G.J., Patterson S.D., Jupiter J.B., Bamberger H.B., Paksima N. Management of recurrent, complex instability of the elbow with a hinged external fixator. J. Bone Joint Surg. Br. 1998;80:1031.
21 McKee M.D., Schemitsch E.H., Sala M.J., O’Driscoll S.W. The pathoanatomy of lateral ligamentous disruption in complex elbow instability. J. Shoulder Elbow Surg. 2003;12:391.
22 Morrey B.F., An K.N. Functional anatomy of the ligaments of the elbow. Clin. Orthop. Relat. Res. 1985;201:84.
23 Nestor B.J., O’Driscoll S.W., Morrey B.F. Ligamentous reconstruction for posterolateral rotatory instability of the elbow. J. Bone Joint Surg. Am. 1992;74:1235.
24 O’Driscoll S.W. Classification and evaluation of recurrent instability of the elbow. Clin. Orthop. Relat. Res. 2000;370:34.
25 O’Driscoll S.W., Bell D.F., Morrey B.F. Posterolateral rotatory instability of the elbow. J. Bone Joint Surg. Am. 1991;73:440.
26 O’Driscoll S.W., Spinner R.J., McKee M.D., Kibler W.B., Hastings H.2nd, Morrey B.F., Kato H., Takayama S., Imatani J., Toh S., Graham H.K. Tardy posterolateral rotatory instability of the elbow due to cubitus varus. J. Bone Joint Surg. Am.. 2001;83-A:1358.
27 Olsen B.S., Sojbjerg J.O., Dalstra M., Sneppen O. Kinematics of the lateral ligamentous constraints of the elbow joint. J. Shoulder Elbow Surg. 1996;5:333.
28 Olsen B.S., Sojbjerg J.O., Nielsen K.K., Vaesel M.T., Dalstra M., Sneppen O. Posterolateral elbow joint instability: the basic kinematics. J. Shoulder Elbow Surg. 1998;7:19.
29 Olsen B.S., Vaesel M.T., Sojbjerg J.O., Helmig P., Sneppen O. Lateral collateral ligament of the elbow joint: anatomy and kinematics. J. Shoulder Elbow Surg. 1996;5(2 Pt 1):103.
30 Potter H.G., Weiland A.J., Schatz J.A., Paletta G.A., Hotchkiss R.N. Posterolateral rotatory instability of the elbow: usefulness of MR imaging in diagnosis. Radiology. 1997;204:185.
31 Regan W., Lapner P.C. Prospective evaluation of two diagnostic apprehension signs for posterolateral instability of the elbow. J. Shoulder Elbow Surg. 2006;15:344.
32 Ring D., Hannouche D., Jupiter J.B. Surgical treatment of persistent dislocation or subluxation of the ulnohumeral joint after fracture-dislocation of the elbow. J. Hand Surg. [Am.]. 2004;29:470.
33 Sanchez-Sotelo J., Morrey B.F., O’Driscoll S.W. Ligamentous repair and reconstruction for posterolateral rotatory instability of the elbow. J. Bone Joint Surg. Br. 2005;87:54.
34 Schneeberger A.G., Sadowski M.M., Jacob H.A. Coronoid process and radial head as posterolateral rotatory stabilizers of the elbow. J. Bone Joint Surg. Am. 2004;86-A:975.
35 Seki A., Olsen B.S., Jensen S.L., Eygendaal D., Sojbjerg J.O. Functional anatomy of the lateral collateral ligament complex of the elbow: configuration of Y and its role. J. Shoulder Elbow Surg. 2002;11:53.
36 Spahn G., Kirschbaum S., Klinger H.M., Wittig R. Arthroscopic electrothermal shrinkage of chronic posterolateral elbow instability: good or moderate outcome in 21 patients followed for an average of 2.5 years. Acta Orthop.. 2006;77:285.
37 Yadao M.A., Savoie F.H.3rd, Field L.D. Posterolateral rotatory instability of the elbow. Instr. Course Lect. 2004;53:607.