CHAPTER 30 Lateral canthal suspension techniques
History
Lateral canthorrhaphies were developed to avoid the deformities associated with the tarsorrhaphies. These procedures were various flap transpositions with skin removal to support the lower eyelid to the upper eyelid at the lateral canthus. Denonvilliers (1856, 1863); Kuhnt-Szymanowski (1870, 1912, 1916) and Meller (1953) described procedures which were widely accepted. Modifications of these procedures were described by Smith (1959) and Kazanjian and Converse (1959) with a tarsoconjunctival wedge excised medially. Bick (1966) reported a technique removing the full thickness temporal aspect of the lower eyelid to correct laxity. Edgerton and Wolfert (1969) described a de-epithelialized dermal pennant of lateral canthal tissue that was passed through a drill hole in the lateral orbital wall to correct lower eyelid malposition. Montandon (1978) modified this procedure to include a lateral tarsorrhaphy. Lateral canthal suspensions have also been described by Whitaker (1984) via the facelift; Whitaker (1984), Ortiz-Monastario and Rodriguez (1985) from the coronal and Paterson, Munro and Farkas (1987) from the conjunctival approach. Jelks (1990, 1991, 1993, 1995) and Hinderer (1993) and Flowers (1993) described variations in bony fixation of the lower eyelid.
Physical evaluation
1. Precise documentation of the chief complaint.
2. Complete general and ocular history.
3. Best corrected visual acuity of each eye.
4. Documentation of variation in anatomic morphology:
5. Palpebral apertures (upper eyelid true or mechanical (lash) ptosis, upper eyelid retraction (thyroid ophthalmopathy, non-pathological); lower eyelid scleral show; medial to lateral canthal position (canthal tilt).
6. Cornea magnified examination with fluorescein stain.
7. Tear film evaluation (tear meniscus, lagophthalmos, Bell’s phenomenon, tear break-up time, contact lens wearer).
Anatomy
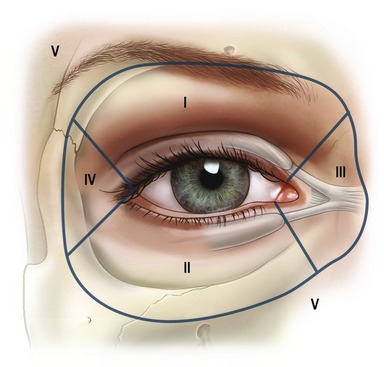
To facilitate a thorough anatomical analysis, the eyelids and surrounding structures are divided into zones (Fig. 30.1).
The lower eyelid (Zone II) extends from the lid margin to the inferior orbital bony rim and is separated into the anterior lamella of skin and orbicularis oculi muscle, the middle lamella consisting of tarsus, orbital septum and retroseptal fat and the posterior lamella with the capsulopalpebral fascia or lower eyelid retractors and the conjunctiva (Fig. 30.2A).
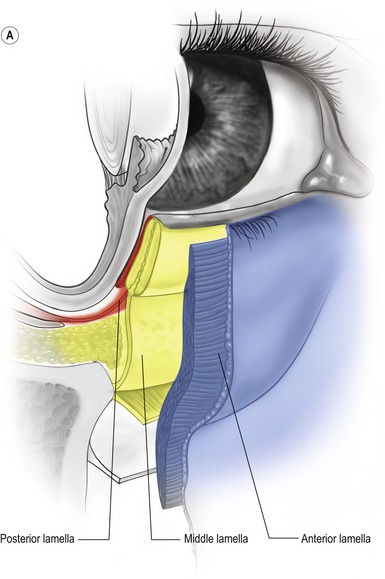
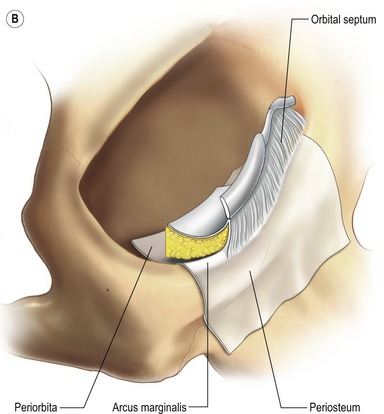
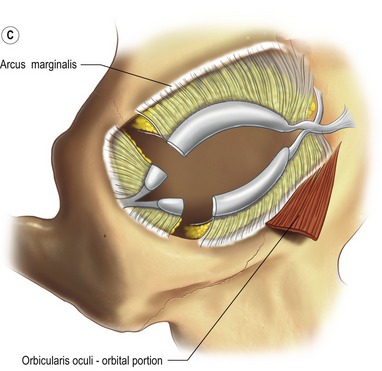
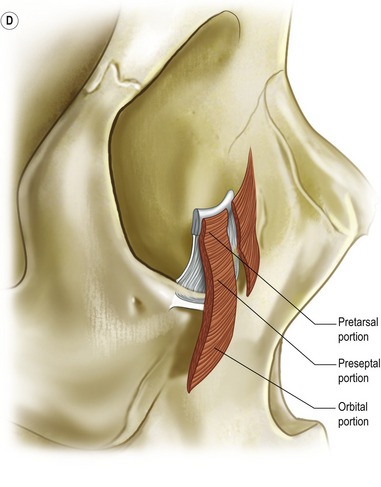
Fig. 30.2 A, The lower eyelid is best represented anatomically as consisting of three lamellae. The anterior lamella is composed of skin and orbicularis oculi muscle. The posterior lamella is the conjunctiva and the capsulopalpebral fascia, an extension of the inferior rectus muscle. The middle lamella is composed of the orbital septum and fat which abuts the inferior border of the tarsus. B, The arcus marginalis is the line of fusion between the periorbita, periosteum and orbital septum. C, The origin of the orbital portion of the orbicularis oculi from the inferior medial orbit. D, The orbicularis oculi muscle is divided into palpebral (pretarsal and preseptal) and orbital portions. Orbital retaining ligaments provide muscle attachment.
The confluence of the orbital septum, orbital floor periorbita and maxillary periosteum at the inferior bony margin is termed the arcus marginalis (Fig. 30.2B). The arcus marginalis in the inferior medial orbit corresponds to the origin of the orbital portion of the orbicularis oculi muscle (Fig. 30.2C).
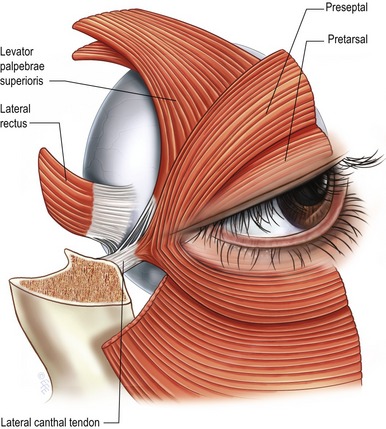
The orbicularis oculi muscle is innervated by the seventh cranial nerve and acts as an antagonist to the levator palpebrae superioris muscle innervated by the third cranial nerve. The orbicularis oculi muscle is divided into palpebral and orbital portions. The palpebral portion is further subdivided into pretarsal and preseptal portions. The orbital portion of the orbicularis oculi arises medially from the superiormedial orbital margin, the maxillary process of the frontal bone, the medial canthal tendon, the frontal process of the maxilla, and the inferiormedial orbital margin (Fig. 30.2C, D). The peripheral fibers sweep across the eyelid over the orbital margin in a series of concentric loops, the more central ones forming almost complete rings. In the lower eyelid, the orbital portion covers the origins of the elevator muscles of the upper lip and nasal ala and continues temporally to cover part of the origin of the masseter muscle. Occasionally, the lower orbital portion may actually continue as low as the corner of the mouth. The inferior orbital orbicularis oculi constitutes the nasojugal, cheek and malar area of the facial anatomy.
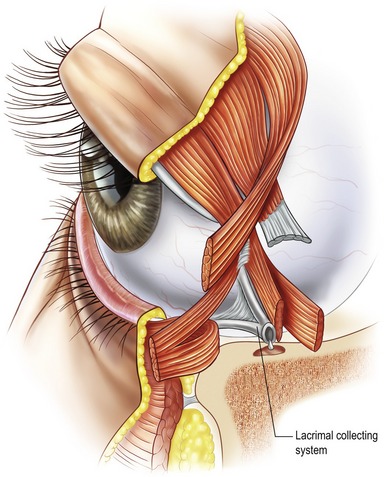
The preseptal portion diverges from its origin on the medial canthal tendon and posterior lacrimal diaphragm and passes across the lid as a series of half ellipses to meet at the lateral palpebral raphe (Fig. 30.3A). The muscle bundles are not interrupted and do not interdigitate at the raphe. The pretarsal muscles form a more superficial common lateral canthal tendon 7 mm from the lateral orbital tubercle where it inserts (Fig. 30.3B).
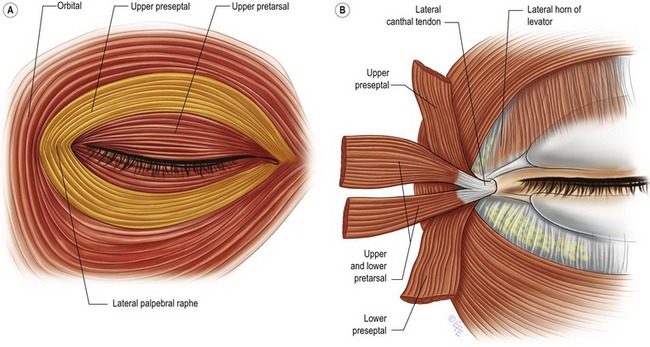
Fig. 30.3 A, The lateral palpebral raphe. B, The lateral canthal tendon and the anatomy of the structures of the lateral canthus.
From Jelks, GW, Smith, BC. Reconstruction of the eyelids and associated structures. In: McCarthy JG, ed. Plastic surgery. Philadelphia: WB Saunders, 1990, p. 1671.
The medial canthus (Zone III) is a complex region containing the origins of the orbicularis oculi muscle (and the lacrimal collecting system (Fig. 30.4).
The lateral canthus (Zone IV) is an integral anatomic unit of the temporal aspects of the eyelids. The lateral canthus is more correctly termed a lateral retinaculum which consists of the lateral horn of the levator palpebrae superioris muscle, the continuation of the preseptal and pretarsal orbicularis oculi muscle as the lateral canthal tendon, the inferior suspensory ligament of the globe (Lockwood’s ligament) and the check ligaments of the lateral rectus muscle (Fig. 30.5). The lateral retinaculum structural components attach to a confluent region of the lateral orbital rim known as Whitnall’s tubercle. It is important to note that the lower eyelid lateral fat is immediately inferior to the lower eyelid contribution to the lateral canthal tendon as it inserts into the orbital tubercle confluence of the lateral retinacular structures. This portion of the lateral canthal mechanism is termed the inferior retinacular component and is the anatomical basis for the inferior retinacular lateral canthoplasty.
Technical steps
Careful evaluation of the specific anatomic deformities enables the surgeon to choose the optimal lateral canthal procedure and if necessary, ancillary procedures (Tables 30.1, 30.2). The distance from the bony orbital rim to the palpebral commissure is the single most important measurement in choosing between a canthopexy or canthoplasty (Fig. 30.6B) and a dermal orbicular pennant. If the bone to soft tissue distance is less than 1 cm, tarsal strip, inferior retinacular canthopexy, or canthoplasty procedures are preferred. If the distance is greater than 1 cm (prominent globes, high myopia, thyroid orbitopathy, malar hypoplasia and negative vector relationship), a dermal orbicular pennant lateral canthoplasty is recommended.
| Canthoplasty techniques | Indications |
|---|---|
| IRLCx | LME I, B-STD <1 cm |
| IRLC |
TSLC + HLS + VSG
Technique abbreviations: IRLCx, inferior retinacular lateral canthopexy; IRLC, inferior retinacular lateral canthoplasty; TSLC, tarsal strip lateral canthoplasty; HLS, horizontal lid shortening; VSG, vertical spacer graft; DOPLC, dermal-orbicular pennant lateral canthoplasty; DOP, dermal-orbicular pennant.
Indications abbreviations: LME, lid margin eversion; B-STD, bone to soft tissue distance; HLL, horizontal lid laxity; MLR, midlamellar retraction.
From Jelks GW, Jelks EB, Chiu ES. Secondary Blepharoplasty: Current Techniques. In: Mathes, ed. Plastic Surgery, Vol II, Philadelphia, Saunders 2006.
Table 30.2 Ancillary lower eyelid: reconstructive techniques
| Technique | Indication |
|---|---|
From Jelks GW, Jelks EB, Chiu ES. Secondary Blepharoplasty: Current Techniques. In: Mathes, ed. Plastic Surgery, Vol II, Philadelphia, Saunders 2006.
Inferior retinacular lateral canthal procedure
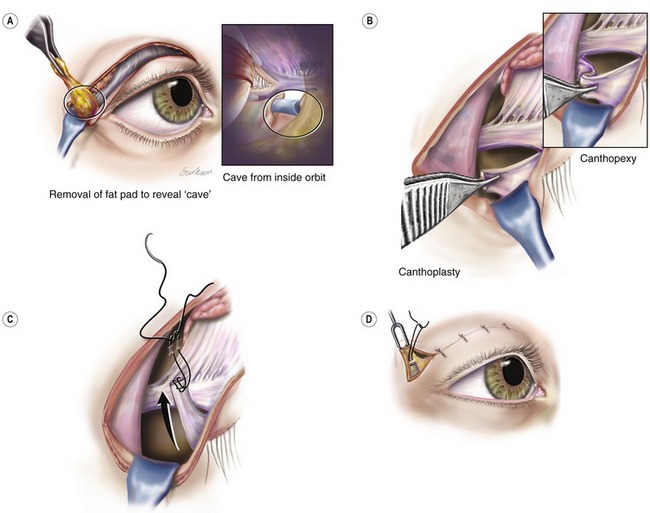
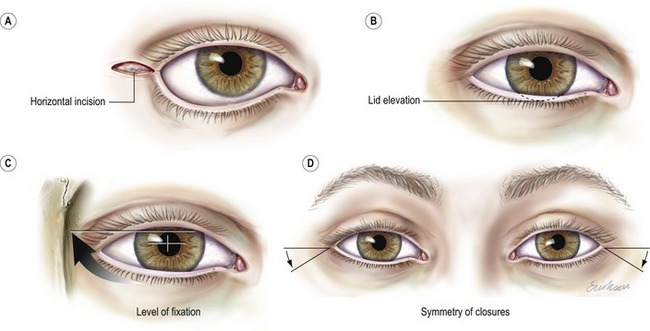
The inferior retinacular lateral canthopexy or canthoplasty was developed for use in the primary blepharoplasty patient to help prevent lower eyelid malposition. It is helpful in correction of lower eyelid malposition associated with a negative vector relationship and mild to moderate lid margin eversion. The main advantage of the inferior retinacular canthal procedure is that it does not separate the lower eyelid from the lateral palpebral commissure. The inferior retinacular lateral canthoplasty procedure is performed through a horizontal lateral canthal incision (Fig. 30.7A) or an upper lateral eyelid incision (Fig. 30.6A).
When the upper lid blepharoplasty is performed in conjunction with lower lid blepharoplasty, the inferior edge of the lateral aspect of the upper eyelid incision is grasped and a submuscular, supraperiosteal skin and muscle flap is elevated 1–2 cm around the lateral canthus and lower eyelid. This is accomplished with a combination of fine point electrosurgical needles and blunt scissor dissection.
An insulated coated Desmarres retractor is inserted as the skin and muscle flap is elevated to expose the lateral canthal retinacular and lateral lower eyelid area. Gentle pressure on the globe produces a bulge in this area which is the excess lateral lower eyelid fat covered by orbital septum. Sharp scissors puncture the orbital septum and expose the fat. The fat is gently removed with forceps and electrocautery to the proper contour (Fig. 30.6A). In our experience, the lower eyelid lateral fat needs to be judiciously removed rather than repositioned.
When the lower eyelid lateral fat is removed, a distinct circular area is created which resembles a “hole” or “cave” from the surgeon’s perspective. The superior aspect or roof of the cave corresponds to the lateral retinacular structures of the lower eyelid inserting into the orbital tubercle of Whitnall (Fig. 30.6A, inset). This tissue is grasped with forceps and a hitching suture is passed through it. Fine point electrocautery is used to release the tissue from the lateral retinacular attachments to the orbital tubercle so the lower eyelid is easily moved superiorly and laterally. The needles are passed into the inner aspect of the orbital rim periosteum at a point corresponding to the upper level of the pupil when the eye is in primary gaze. This procedure is termed a lateral canthoplasty because it releases and repositions the lateral canthus and lower eyelid to a different position (Fig. 30.6B). The inferior retinacular tissue (roof of the “cave”) can be sutured to the lateral orbital rim periosteum without releasing it from the orbital tubercle when the clinical situation does not require significant lower eyelid and lateral canthus repositioning. This is termed a lateral canthopexy (Fig. 30.6B, inset). In both the canthopexy and the canthoplasty, the point of suture fixation is the periorbita of the inner aspect of the orbital rim at the level of the upper pupil in primary gaze (Fig. 30.6D).
The suture is a 5-0 nylon (Ethibond P-3 needle) for cosmetic blepharoplasty cases and 4-0 Polydek (Deknatel ME-2 needle) for reconstructive cases. The lateral canthoplasty is completed by tightening the suture and securing the lower lid lateral retinaculum to an elevated position inside the lateral orbital rim (Fig. 30.6D). The lower eyelid level should cover 1–2 mm of the inferior cornea and appear overcorrected. The lower eyelid settles into a lower position in 2 to 6 weeks. Symmetry of the eyelids at the completion of surgery is imperative (Fig. 30.7D).
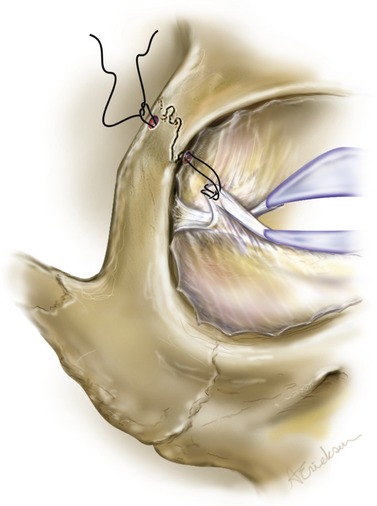
If the fixation of the lateral retinacular tissue to the orbital periosteum is inadequate due to scarring or trauma, a local periosteal flap or fascial graft is used. Occasionally, a drill hole in the lateral orbital bone may be required for secure fixation (Fig. 30.8).
Dermal orbicular pemart lateral canthoplasty
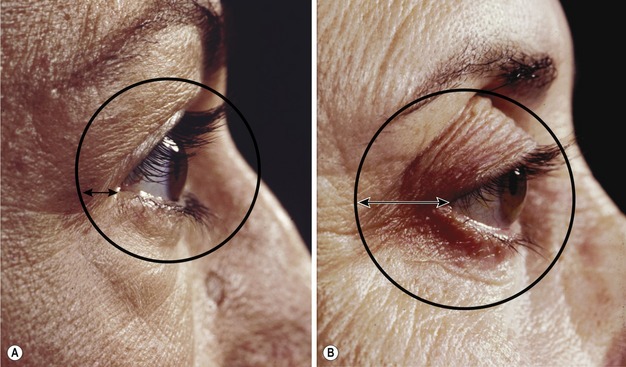
Dermal orbicular pennant lateral canthoplasty was developed for patients with more than 1 cm distance from the lateral canthus and the bony orbit (Fig. 30.10B) and to reduce the incidence of the “beady eye” appearance and lower eyelid contour deformities caused by the tarsal strip technique. This procedure uses an extension of the lower eyelid in the form of a de-epithelialized pennant of skin and orbicularis oculi muscle (Fig. 30.9A–C). A lateral canthotomy may or may not be performed; therefore, lateral palpebral commissure deformities are reduced and shortening of the horizontal palpebral aperture does not occur (Fig. 30.12). A horizontally oriented dermal orbicular pennant of de-epithelialized skin and muscle, 0.5 cm by 1.0 cm, is incised in such a way to add an extension to the lower eyelid without cutting the lateral commissure. The pennant is completely separated from the upper eyelid pretarsal, preseptal and orbital orbicularis oculi muscle. The pennant is separated from the lower eyelid orbital and preseptal orbicularis oculi muscle, but left attached to the pretarsal orbicularis oculi muscle (Fig. 30.9C). Release of the lower eyelid by lysis of the inferior retinaculum (Fig. 30.9D) allows the lower eyelid to be elevated and tightened.
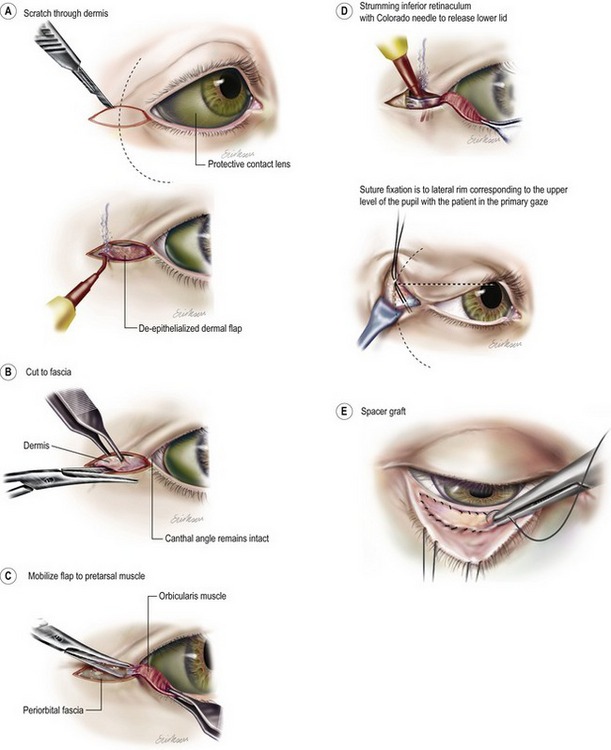
Fig. 30.9 Dermal-orbucular pennant lateral canthoplasty. A, The patient is illustrated with a protective, colored contact lens in place. The dermal-orbicular flap is outlined at the lateral canthus. Note the horizontal alignment and the maintenance of the external commissure. An incision is made through the superficial layers. B, The flap is de-epithelialized, preserving the underlying dermis. The superficial border of the flap is incised to the suborbicularis muscle plane. C, the inferior border of the dermal-orbicular pennant is elevated to maintain the attachment of the pretarsal orbicularis muscle. D, The lower lid component of the lateral retinaculum is divided by “strumming” the structure with a Colorado needle. The fixation of the suture is to the lateral orbital rim, corresponding to the upper level of the pupil with the patient in primary gaze. E, A vertical graft of autogenous auricular cartilage or palatal mucosa is used to correct vertical defects caused by midlamellar cicatricial retraction.
A–D modified from Jelks GW, Jelks EB, Chiu ES. Secondary blepharoplasty: Current techniques. In Mattes, ed. Plastic surgery. Vol II, Philadelphia, Saunders, 2006.
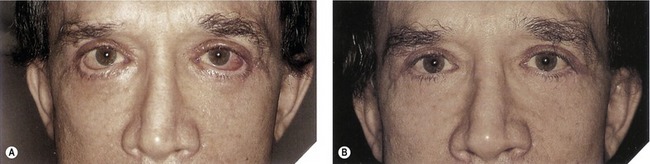
Fig. 30.12 A, Patient with bilateral lower eyelid malposition after blepharoplasty. B, The patient is seen 9 months after bilateral dermal-orbicular pennant lateral canthoplasties.
From Jelks GW, Jelks EB. Blepharoplasty. In: Peck GC, ed. Complications and problems in aesthetic plastic surgery. New York: Gower Medical Publishing, 1992, p. 5.
This technique is useful in postblepharoplasty patients with lower eyelid malposition, especially when there is a negative vector relationship and the soft tissue to bone distance is greater than 1 cm (see Fig. 30.10). The variable amount of orbital rim to lateral palpebral aperture distance can be managed by varying the suture placement for the canthal tightening (Fig. 30.11B).
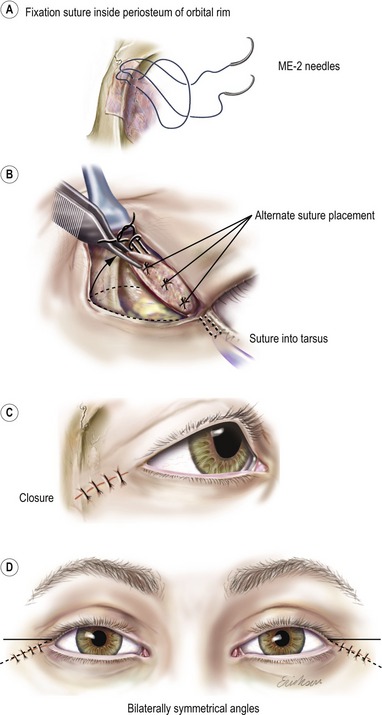
Fig. 30.11 Dermal-orbicular pennant lateral canthoplasty fixation and closure. A, Both arms of ME-e 4-0 Polydek suture are passed through periosteum from the inner to the outer aspect of the orbital rim. The needles are passed through the loop and cinched tightly down, hugging the inner aspect of the orbital rim. B, Most commonly, periosteal fixation if to the lateral edge of the tarsus. Fixation of the lower lid covers 1–2 mm of the inferior cornea. C, On closure, elevation causes inferior angulation of the original horizontal incision. D, When bilateral procedures are performed, care is taken to obtain symmetry of closure.
Modified from Jelks GW, Jelks EB. Repair of lower lid deformities. Clin Plast Surg 1993;20:417.
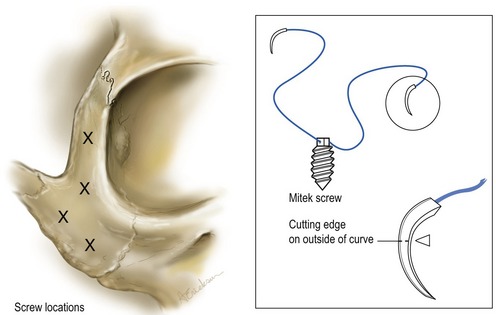
Dermal-orbicular pennant with tarsal strip horizontal lid shortening and midface suspension
After elevation of the dermal-orbicular pennant (see Fig. 30.9), if horizontal lid shortening is necessary, a lateral canthotomy and inferior lid cantholysis is performed. The temporal tarsus is bared of conjunctiva, cilia, skin and muscle creating a tarsal strip which is attached to the dermal orbicular pennant. The amount of tarsal strip developed corresponds to the amount of horizontal lid shortening required. The cheek and midface is elevated from a supraperiosteal or subperiosteal plane by extending the dermal orbicular pennant incision. A titanium fixation screw with attached sutures suspends the cheek and midfacial tissue (Fig. 30.13). The place for screw insertion varies from the lateral orbital rim to the zygoma prominence (Fig. 30.14). Correction of midlamellar cicatricial vertical retraction is performed with a vertical spacer graft (auricular cartilage) that is inserted through the same incision. A separate lower eyelid incision is avoided (Fig. 30.9E).
Complications
Subconjunctival hemorrhage is a collection of blood between the conjunctiva and sclera. It can be a frightening experience for the patient in the early postoperative period. It is rarely dangerous and cold compresses and time result in gradual resolution. A granuloma is an elevation of granulation tissue at the edge of the conjunctival incision. It is often associated with bloody tears at three to five days postoperatively. It is gently removed by scraping with a cotton-tipped applicator or forceps after application of topical ophthalmic anesthesia.
Pearls & pitfalls
Pearls
• When transconjunctival, retroseptal lower blepharoplasty is done with an upper eyelid blepharoplasty, removal of the lower eyelid lateral fat is performed, followed by inferior retinacular lateral canthal tightening.
• The inferior retinacular lateral canthopexy or canthoplasty was developed for use in the primary blepharoplasty patient to help prevent lower eyelid malposition. It is helpful in correction of lower eyelid malposition associated with a negative vector relationship and mild to moderate lid margin eversion.
• The main advantage of the inferior retinacular canthal procedure is that it does not separate the lower eyelid from the lateral palpebral commissure.
• The lower eyelid level should cover 1–2 mm of the inferior cornea and appear overcorrected. The lower eyelid settles into a lower position in 2 to 6 weeks. Symmetry of the eyelids at the completion of surgery is imperative.
• The tarsal strip procedure is useful for correction of moderate to severe lid margin eversion, paralytic ectropion and secondary correction of unrecognized horizontal lid laxity after blepharoplasty.
• Dermal orbicular pennant lateral canthoplasty was developed to reduce the incidence of the “beady eye” appearance and lower eyelid contour deformities caused by the tarsal strip technique.
• With the dermal orbicular pennant lateral canthoplasty a lateral canthotomy is not performed; therefore, lateral palpebral commissure deformities are reduced and shortening of the horizontal palpebral aperture does not occur.
• The dermal orbicular pennant canthoplasty is useful in postblepharoplasty patients with lower eyelid malposition, especially when there is a negative vector relationship and the soft tissue to bone distance is greater than 1 cm.
• The dermal-orbicular pennant flap with or without horizontal lid shortening or vertical spacer grafts with midfacial suspension has become the preferred method of surgical correction for complex lower eyelid malpositions.
Pitfalls
• In the inferior retinacular canthal procedure, if the fixation of the lateral retinacular tissue to the orbital periosteum is inadequate due to scarring or trauma, a local periosteal flap or fascial graft is used. Occasionally, a drill hole in the lateral orbital bone may be required for secure fixation.
• Patients with severe lower eyelid malposition associated with cheek and midfacial descent have often had multiple procedures resulting in deficient lower eyelid muscle and skin. The lower eyelid malposition is due to a combination of vertical restriction and horizontal laxity. The dermal orbicular pennant technique provides access for correction of the midfacial descent and lower eyelid cicatricial retraction. The tarsal strip technique provides management of the horizontal lid laxity. A tension-free lateral canthoplasty is assured by midfacial suspension with or without a titanium screw.
• The combined techniques require separation of the lateral palpebral commissure (lateral canthotomy).
• A horizontal wedge resection is contraindicated when the lateral canthal position is lower than the medial canthal position (negative canthal tilt, prominent globe, negative vector relationship).
• Tarsal strip produces a decrease in the horizontal dimension of the palpebral aperture, giving the appearance of a “beady eye”. Deformity of the lateral lower eyelid at the lateral commissure with lack of contact with the globe, webbing and trichiasis may also occur.
Summary of steps
1. The lateral canthal procedures are performed with the surgeon at the head of the patient looking toward the feet.
2. A focused headlight and 4× loop magnification is recommended.
3. Careful evaluation of the specific anatomic deformities enables the surgeon to choose the optimal lateral canthal procedure and if necessary, ancillary procedures.
4. The distance from the bony orbital rim to the palpebral commissure is the single most important measurement in choosing between a canthopexy, canthoplasty and a dermal orbicular pennant.
5. If the bone to soft tissue distance is less than 1 cm, tarsal strip, inferior retinacular canthopexy, or canthoplasty procedures are preferred.
6. If the distance is greater than 1 cm (prominent globes, high myopia, thyroid orbitopathy, malar hypoplasia and negative vector relationship), a dermal orbicular pennant lateral canthoplasty is recommended.
7. Dermal orbicular pennant canthoplasty can be combined with a tarsal strip for horizontal lid shortening and a cartilage graft for vertical restoration.
8. Use of midfacial suspension with or without titanium screw fixation is necessary to obtain a tension free lateral canthal plasty.
Anderson R, Jordan D. The tarsal strip procedure. Arch Ophthalomol. 1979;97:2191.
DiFranceso L, Codner M, McCord C, et al. Evaluation of conventional subciliary incision used in blepharoplasty: preoperative and postoperative videography and electromyography findings. Plast Reconstr Surg. 2005;116:632.
Enzer Y, Shorr N. Medical and surgical management of chemosis after blepharoplasty. Ophthal Plast Reconstr Surg. 1994;10:57.
Fagien S. Algorithm for canthoplasty: the lateral retinacular suspension: a simplified suture canthopexy. Plast Reconstr Surg. 1999;103:2042.
Flowers R. Canthopexy as a routine blepharoplasty component. Clin Plast Surg. 1993;20:351.
Hirmand H., Codner M., McCord C., et al. Prominent eye: operative management in lower lid and midfacial rejuvenation and the morphologic classification system. Plast Reconstr Surg. 2002;110:620.
Honrado C, Pastorek N. Long-term results of lower-lid suspension blepharoplasty. Arch Facial Plast Surg. 2004;6:150.
Jacobs S. Prophylactic lateral canthopexy in lower blepharoplasty. Arch Facial Plast Surg. 2003;5:267.
Jelks G, Glat P, Jelks E, et al. The inferior retinacular lateral cathoplasty: a new technique. Plast Reconstr Surg. 1997;100:1262.
Klatsky S, Iliff N, Manson P. Blepharoplasty. In: Goldwyn R, Cohen M. The unfavorable result in plastic surgery: avoidance and treatment. 3rd edn. Philadelphia: Lippincott Williams & Wilkins; 2001:847–879.
Patipa M. The evaluation and management of lower eyelid retraction following cosmetic surgery. Plast Reconstr Surg. 2000;106:438.
Putterman A. Cosmetic oculoplastic surgery, 3rd edn. Philadelphia: WB Saunders; 1999.
Rees T. Prevention of ectropion by horizontal shortening of the lower lid during blepharoplasty. Ann Plast Surg. 1983;11:17.
Rees TD, Aston SJ, Thorne CHM, Blepharoplasty and facialplasty, 1st edn. McCarthy JG, ed., Plastic surgery, W.B. Saunders, Philadephia, 1990;Vol. 3:2320–2414.
Rohrich RJ, Pessa JE. The retaining system of the face: histologic evaluation of the septal boundaries of the subcutaneous fat compartments. Plast Reconstr Surg. 2008;121(5):1804–1809.
Shorr N, Perry J. Lower blepharoplasty and midface descent. In: Chen WP, ed. Oculoplastic surgery: the essentials. 1st edn. New York: Thieme Medical Publishers; 2001:147–165.
Spinelli HM, Jelks GW. Periocular reconstruction: a systematic approach. Plast Reconstr Surg. 1993;91:1017–1024.
Zarem H, Resnick J. Expanded applications for transconjunctival lower lid blepharoplasty. Plast Reconstr Surg. 1999;103:1041.
Zide BM, Jelks GW. Surgical anatomy of the orbit. New York: Raven Press; 1985.