CHAPTER 76 Laser resurfacing
Physical evaluation
1. Assess Fitzpatrick skin type (Table 76.1). Skin types I, II, III are acceptable candidates for ablative resurfacing, but extreme caution should be used in skin types IV or V. Higher Fitzpatrick skin types can be safely treated using newer fractionated ablative or nonablative lasers.
3. Dyschromia. Brown lesions present in the superficial dermis will respond whereas deeper dermal lesions will persist. Red dyschromia such as seen with acne rosea can result in copious bleeding during Er:YAG laser treatment.
4. Rhytid location and severity (Table 76.2). Differentiate and document static and dynamic rhytids.
5. Cutaneous disorders such as carcinoma, seborrheic or actinic keratoses, and solar lentigines should be noted.
6. Skin tone, texture, and pore size.
7. Adequate preoperative skin care including sunblocking agents, bleaching agents (hydroquinone), and moisturizing skin care regimen.
| Fitzpatrick skin type | Description |
|---|---|
| I | Extremely fair skin, always burns, never tans |
| II | Fair skin, always burns, sometimes tans |
| III | Medium skin, sometimes burns, always tans |
| IV | Olive skin, rarely burns, always tans |
| V | Moderately pigmented brown skin, never burns, always tans |
| VI | Markedly pigmented black skin, never burns, always tans |
Table 76.2 Glogau rhytid/photoaging classification scheme
| Glogau scale | Age | Description |
|---|---|---|
| Mild | 28–35 years | Little wrinkles, no keratosis, requires little or no makeup for coverage |
| Moderate | 35–50 years | Early wrinkling, sallow complexion with early actinic keratosis, requires little makeup |
| Advanced | 50–60 years | Persistent wrinkling, discoloration of the skin with telangiectasias and actinic keratosis, always wears makeup |
| Severe | 65–70 years | Severe wrinkling, photoaging, gravitational and dynamic forces affecting skin, actinic keratosis with or without cancer, wears makeup with poor coverage |
Anatomy
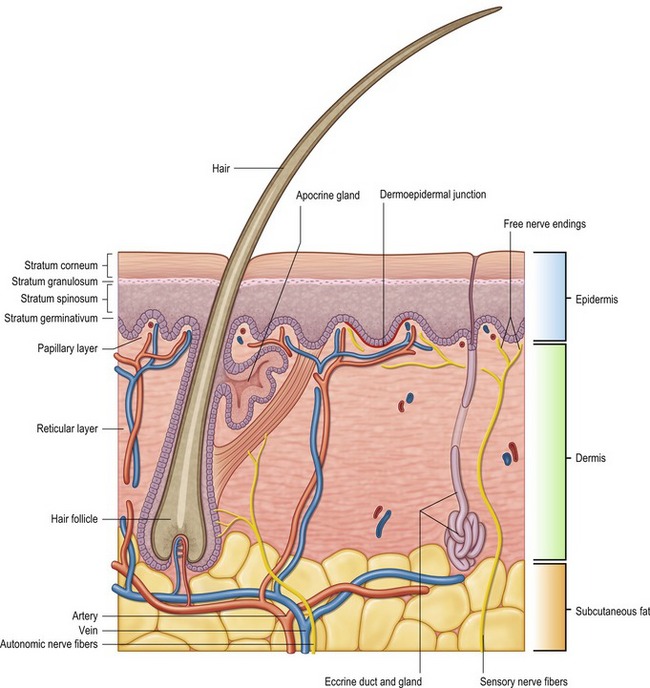
Laser resurfacing demands a precise knowledge of skin histology (Fig. 76.1). The epidermis makes up approximately five percent of skin thickness. The epidermis encompasses five distinct layers: stratum corneum, stratum lucidum, stratum granulosum, stratum spinosum, stratum germinativum. The stratum corneum is composed primarily of nonviable cells, which are turned over frequently and replaced by precursor cells from underlying layers. Nonablative resurfacing techniques by definition leave the epidermis intact, while ablative resurfacing techniques will remove this layer.
The dermis is divided into a papillary and reticular layer. Most ablative resurfacing techniques will remove the papillary and superficial reticular dermis. The papillary dermis begins at the basement membrane and has a high type III collagen content. The papillary dermis is relatively thin measuring about 100 µm in thickness.
Technical steps
Before any laser treatment is undertaken, appropriate safety precautions should be taken by strict application of the guidelines listed in Table 76.3. Wavelength appropriate eyewear should be provided to all operating room personnel and eyeshields should be used for the patient.
With the understanding that each case is unique and poses its own set of circumstances, the following protocol is standard (Table 76.4). The face is first treated with three separate passes at 100 microns of ablation with no coagulation using a scanning pattern. This will result in a uniform depth of ablated tissue of 300 microns. While this laser is collimated for ease of use, the handpiece should be held a constant distance from the skin at a perpendicular angle. Meticulous care should be taken to deliver the energy in a uniform manner, taking care not to skip areas or overlap. After each pass, denuded skin is removed with sterile moist gauze and assessed for depth by using the following clinical endpoints: wrinkle ablation, reticular punctate bleeding pattern, and lacey or fragmented appearance of the midreticular dermis. At the caudal border of the mandible, taper to 200 microns and then to 100 microns at the neck transition. Using a four millimeter spot size, spot treat deeper rhytids with rapid fire 30 micron pulses, paying attention to clinical endpoints with the goal of wrinkle ablation. To blend the laser treated skin with untreated skin, taper these transitional areas by spot treating the margins using 30 microns of ablation. When skin tightening is needed, the surgeon can choose to add 25 microns of coagulation during the third pass with the understanding that this may result in prolonged postoperative erythema. The authors typically reserve this for treatment of the lower eyelids. Smoke evacuation is typically done by the first assistant during all phases of treatment.
Table 76.4 Specific guidelines for Er:YAG laser resurfacing based on skin thickness
| Pass variations | Clinical Guidelines |
|---|---|
| 100 ablate/0 coagulation | Thick skin – 300 microns |
| 30 ablate/0 coagulation | Normal skin – 250 microns |
| 50 ablate/25 coagulation | Thick eyelid |
| 30 ablate spot treatment | Feather margins and smooth deeper rhytids |
NOTE: Acne scars can be treated with a single pass at 100 microns of ablation followed by spot treatment of crater scars.
Postoperative care
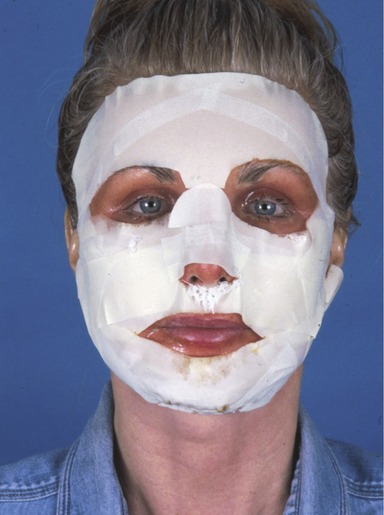
While surgeons debate the efficacy of occlusive and nonocclusive wound care protocols, it is well-established that a moist environment must be maintained. Because occlusive dressings have been shown to accelerate the rate of re-epithelialization and decrease postoperative pain, we advocate using an occlusive wound care regimen. Immediately after surgery, the wound is dressed with Flexan® which is precisely cut to cover as much treated skin as possible. Flexan is a sterile, ultra-thin, highly conformable, semi-occlusive polyurethane foam adhesive dressing that protects wounds while maintaining a moist healing environment. The Flexan dressing is left in place and Bacitracin and Aquaphor ointments are alternated every four hours over exposed areas and lightly over dressing. Eyes can be rinsed as needed, the head is strictly elevated to alleviate swelling, and antiviral prophylaxis is continued until postoperative day seven. Postoperative day three, the patient is seen in the office and the Flexan dressing is removed and replaced. The face is cleaned with mild vinegar soaks and gently debrided of nonviable tissue. Flexan dressing is replaced and Bacitracin and Aquaphor ointment is applied as previously. Postoperative day six, Flexan dressing is removed, the face is washed with mild vinegar soaks and gently debrided. An open wound technique is employed until day ten as follows: clean face with Cetaphil® and apply Aquaphor four times per day with an appropriate sunblocking agent. By day ten, the skin will have re-epithelialized and patients can begin to apply post-treatment makeup. Sun exposure should be strictly avoided during the next several months and preoperative skin care regimens can be slowly introduced keeping the skin moist during this transitional period.
Complications
Pearls & pitfalls
Pearls
• Clinical endpoints for ablative laser technique using the Er:YAG laser are: wrinkle ablation, reticular punctate bleeding pattern, and lacy or fragmented appearance of the mid reticular dermis.
• Appropriate antiviral prophylaxis is mandatory for both ablative and fractionally ablative laser treatments.
• Strict avoidance of sun exposure in the postoperative period using sunblocking agents is mandatory to avoid postoperative hyperpigmentation.
• Initial wound care with an occlusive protocol (Flexan dressing) contributes to moist wound healing and decreases pain.
Pitfalls
• Ablative laser resurfacing distal to the caudal border of the mandible is contraindicated.
• Ablative laser resurfacing in Fitzpatrick skin types IV and V should be undertaken with extreme caution and these patients should always be pretreated with appropriate skin care (hydroquinone).
• Moist wound care should be utilized in postoperative wound care for ablative lasers. Allowing these wounds to desiccate can result in delayed healing and possible scarring.
• Postoperative sun exposure can result in significant postoperative hyperpigmentation.
• Failure to strictly follow specific laser safety guidelines can result in harm to both patient and operating room personnel.
• Possible containdications for fractionated laser treatment include Fitzpatrick types IV and V skin, treatment off face in areas with a paucity of adnexal structures, when rapid healing is desired, and in areas of undermined skin (facelifting procedures).
Summary of steps
1. Appropriate eyewear should be provided to operating room personnel and eyeshields should be used for the patient.
2. Preoperatively, patients should receive antiviral prophylaxis for two days prior to the procedure and postoperatively until the wound has re-epithelialized.
3. Patients should wash their face preoperatively with antibacterial soap and the face should be prepped with Phisohex® cleaner, washed with sterile saline, and blotted dry.
4. The authors preferred method of ablative laser resurfacing uses the Dual Mode Er:YAG laser (Sciton Contour™).
5. The vaporization threshold of the Er:YAG laser is between 0.5 and 1.5 J/cm2.
6. Using a touchscreen panel, the surgeon can program microns of ablation and the microns of coagulative thermal damage to be induced.
7. The face is first treated with three separate passes at 100 microns of ablation with no coagulation using a scanning pattern.
8. After each pass, denuded skin is removed with sterile moist gauze and assessed for depth.
9. For fractionated carbon dioxide resurfacing, we recommend the Fraxel® Repair system.
10. For nonablative skin rejuvenation, the Fraxel Restore utilizes an Erbium glass laser (1550 nm).
Alster TS. Cutaneous resurfacing with CO2 and erbium: YAG lasers: preoperative, intraoperative, and postoperative considerations. Plast Reconstr Surg. 1999;103(2):619–632.
Alster TS. Cutaneous resurfacing with Er:YAG lasers. Dermatol Surg. 2000;26(1):73–75.
Geronemus RG. Fractional photothermolysis: current and future applications. Lasers Surg Med. 2006;38(3):169–176.
Goldberg DJ, Cutler KB. The use of the erbium:YAG laser for the treatment of class III rhytids. Dermatol Surg. 1999;25(9):713–715.
Hughes PS. Skin contraction following erbium:YAG laser resurfacing. Dermatol Surg. 1998;24(1):109–111.
Kim YJ, Lee HS, Son SW, et al. Analysis of hyperpigmentation and hypopigmentation after Er:YAG laser skin resurfacing. Lasers Surg Med. 2005;36:47–51.
Laubach HJ, Tannous Z, Anderson R, et al. Skin responses to fractional photothermolysis. Lasers Surg Med. 2006;38(2):142–149.
Tanzi EL, Alster TS. Single-pass carbon dioxide versus multiple-pass Er:YAG laser skin resurfacing: a comparison of postoperative wound healing and side-effect rates. Dermatol Surg. 2003;29:80–84.
Tanzi EL, Alster TS. Side effects and complications of variable-pulsed erbium:yttrium-aluminum-garnet laser skin resurfacing: extended experience with 50 patients. Plast Reconstr Surg. 2003;111:1524–1529.
Zachary CB. Modulating the Er:YAG laser. Lasers Surg Med. 2000;26(2):223–226.