CHAPTER 12 Laparoscopic Cholecystectomy
Case Study
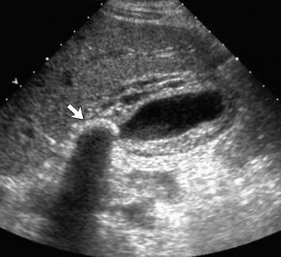
A right upper quadrant ultrasound is obtained, which shows gallstones and gallbladder wall thickening (Fig. 12-1). The common bile duct (CBD) is visualized and is of normal caliber.
INDICATIONS FOR CHOLECYSTECTOMY
PREOPERATIVE EVALUATION
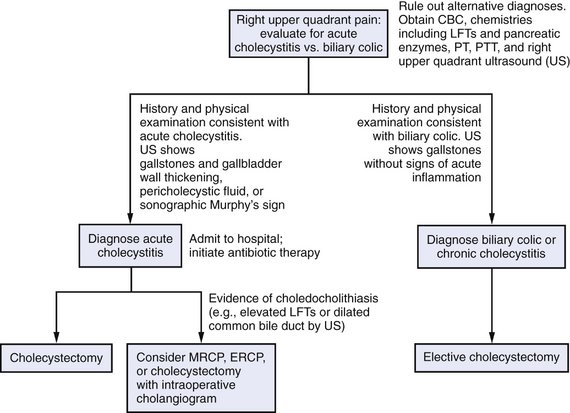
In addition to a review of standard preoperative studies, reassessment of all studies obtained in evaluating a patient with gallbladder pathology is essential because laboratory data and study results significantly influence management (Fig. 12-2). Of particular importance are:
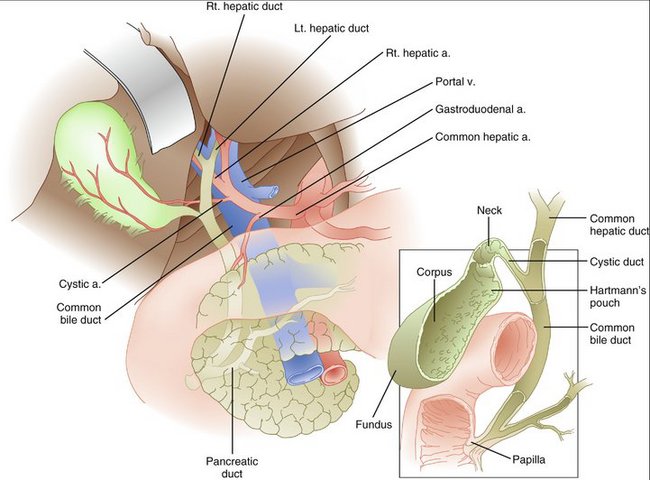
COMPONENTS OF THE PREOCEDURE AND APPLIED ANATOMY
Preoperative Considerations
Port Placement
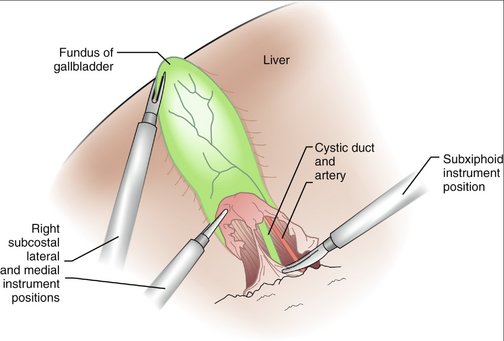
In general, laparoscopic cholecystectomy is performed through four operative ports (Fig. 12-3).
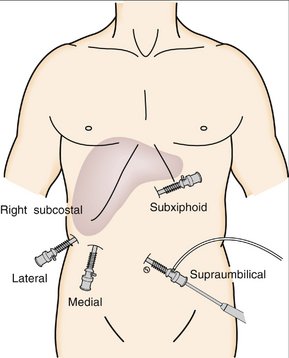
Figure 12-3 Port placement for laparoscopic cholecystectomy.
(From Cameron J: Atlas of Surgery, vol 2. Philadelphia, Decker, 1994.)
Exposure
Dissection
Division of the Cystic Duct and Cystic Artery
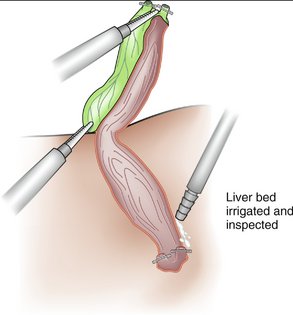
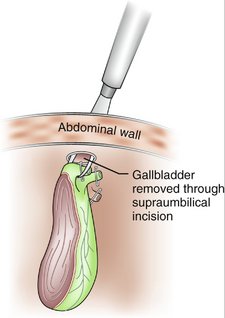
Removal of the Gallbladder from the Liver Bed
ADDITIONAL OPERATIVE CONSIDERATIONS
POSTOPERATIVE COURSE
Complications
Postoperative Evaluation for Suspected Complications
Ahrendt SA, Pitt HA. Biliary tract. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, editors. Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 17th ed. Philadelphia: Saunders; 2004:1597-1622.
Collins C, Maguire D, Ireland A, et al. A prospective study of common bile duct calculi in patients undergoing laparoscopic cholecystectomy: natural history of choledocholithiasis revisited. Ann Surg. 2004;239:28-33.