Laparoscopic Adrenalectomy
Introduction
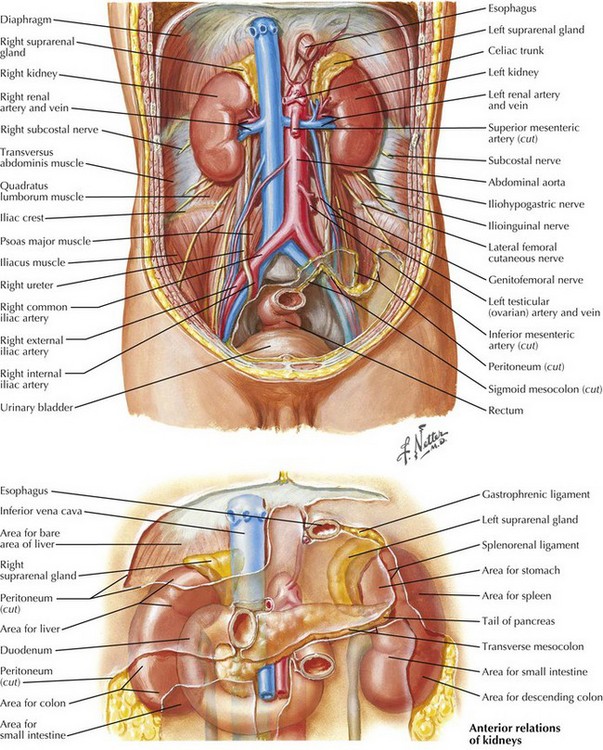
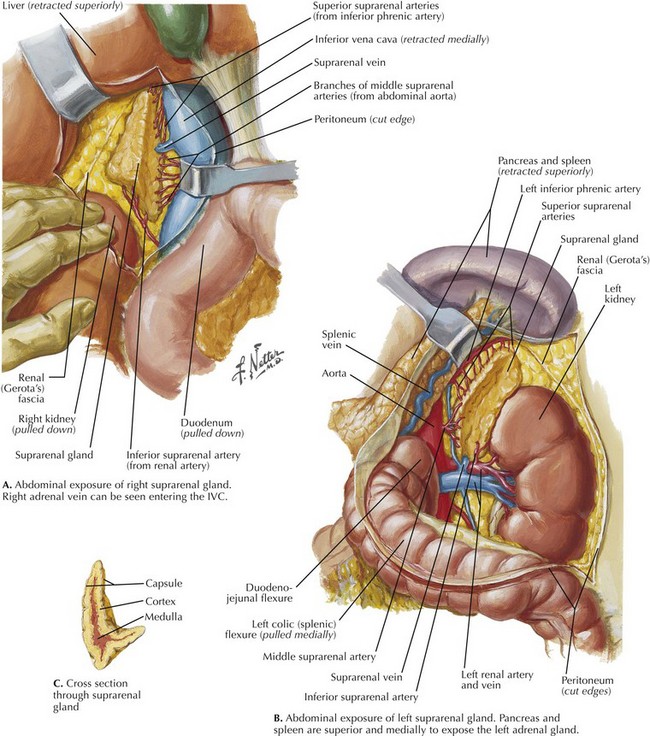
The adrenal glands reside in the retroperitoneum just above the kidneys (Fig. 4-1). Histologically, the adrenal glands are divided into an outer cortex comprising three layers—zona glomerulosa, zona fasciculata, and zona reticularis—and an inner medulla (Fig. 4-2). These histologic layers correspond to various hormones produced by the adrenal glands.
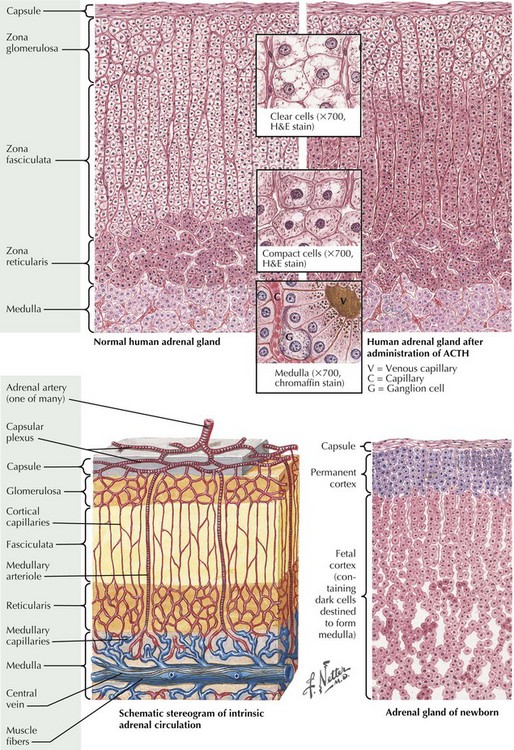
FIGURE 4–2 Histology of adrenal glands.
ACTH, Adrenocorticotropic hormone; H&E, hematoxylin and eosin.
1. Functional tumors based on excessive hormone production: hyperaldosteronism or Conn syndrome, hypercortisolism or Cushing syndrome, sex hormone–producing tumors, or pheochromocytomas, which lead to excess catecholamine production.
2. Tumors suspicious for malignancy: primary adrenocortical cancer (ACC) or adrenal metastases.
3. Tumors that initially do not meet criteria for categories 1 or 2 but continue to increase in size and volume on interval radiographic follow-up at a rate concerning for a malignant process, or become hypersecretory on repeat laboratory testing.
Surgical Principles
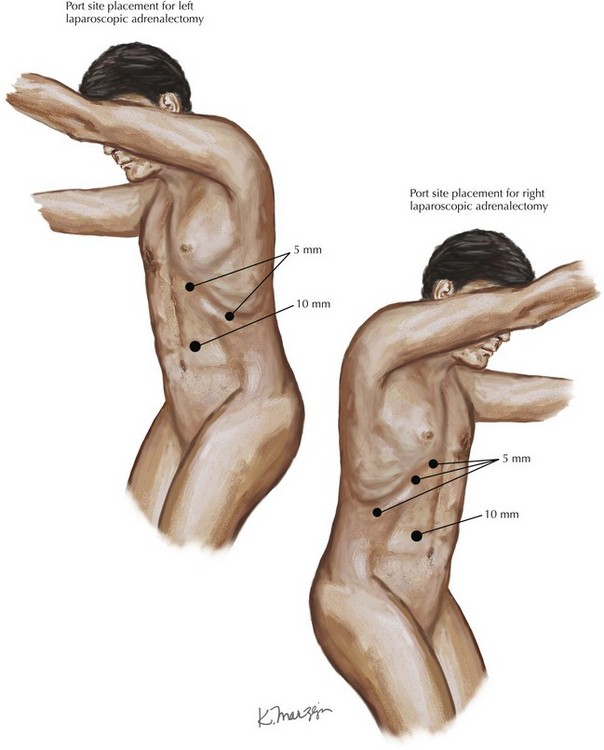
To begin the transabdominal laparoscopic approach, the patient is positioned in the lateral decubitus position to allow gravity to assist with the dissection. A patient requiring right adrenalectomy is placed into a left lateral decubitus position in a jackknife position. Four laparoscopic ports are used, with a 10- to 12-mm port along the lateral border of the right rectus muscle at approximately the level of the umbilicus for the camera and three 5-mm ports along the costal margin. The port closest to the xiphoid process is used for a liver retractor, and two working ports are used for the operative dissection. For left adrenalectomy, the patient is reversed into the right lateral decubitus position, and because there is no need for retraction of the liver, three ports can be triangulated for the operative procedure (Fig. 4-3).
Surgical Technique
Right Laparoscopic Adrenalectomy
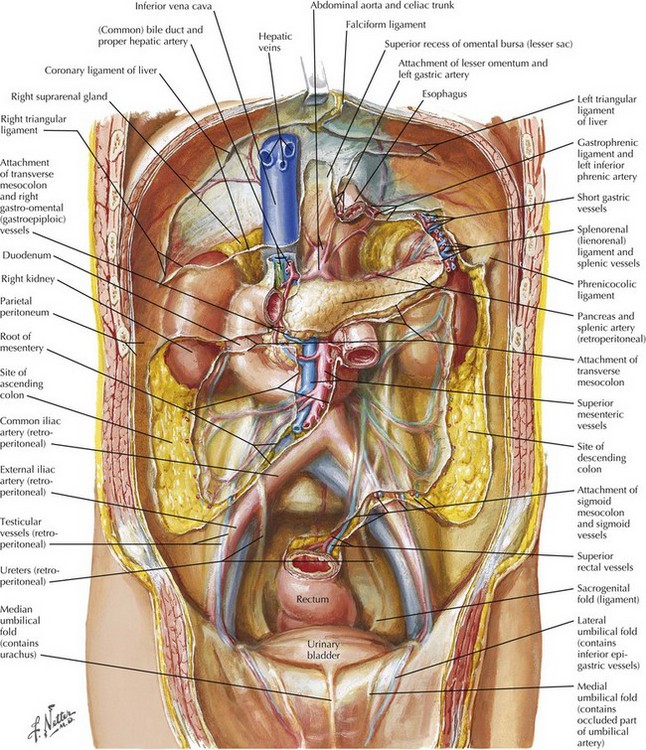
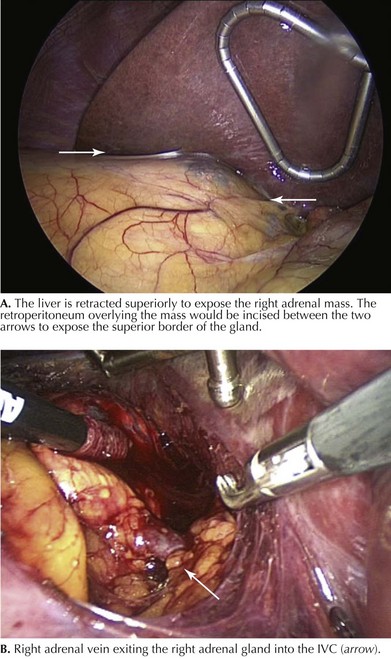
After the ports are placed (Fig. 4-3), a liver retractor is used to elevate the liver superiorly and medially to expose the superior border of the right adrenal gland. The retroperitoneal fascia is then incised from the lateral border of the inferior vena cava (IVC) out to the right triangular ligament of the liver. Figure 4-4 shows a cutaway view of the retroperitoneum with the liver removed to illustrate the right adrenal gland, kidney, and IVC. The line of incision would be just inferior to the liver (Fig. 4-5).
Once the superior border of the adrenal gland is cleared, the next goal is identification of the right adrenal vein as it enters the IVC. The vein generally enters along the medial border of the right adrenal gland at about the 2 o’clock position on the gland, as viewed in a craniocaudal position (Fig. 4-6). The right adrenal vein should then be divided with surgical clips. The remaining adrenal attachments and vasculature can then be divided in the retroperitoneum by standard techniques with surgical clips or an energy device such as the Harmonic scalpel or Ligasure.
Left Laparoscopic Adrenalectomy
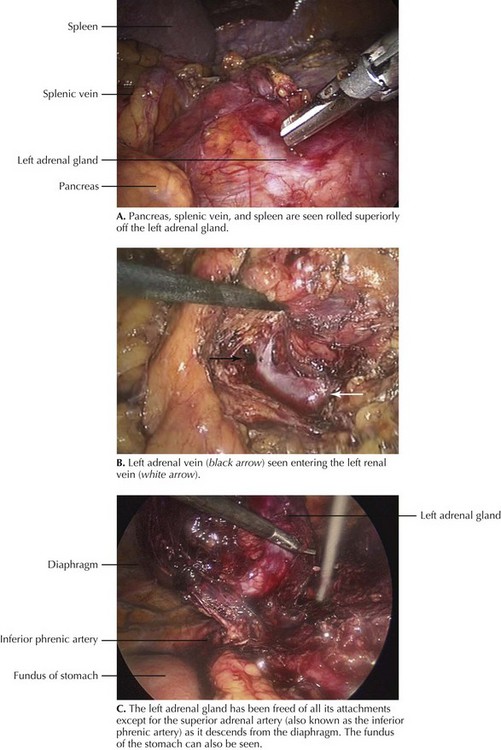
After ports are placed (see Fig. 4-3), the first step is to “take down” the splenic flexure of the colon and divide a portion of the gastrocolic ligament to expose the inferior border of the pancreas and Gerota’s fascia overlying the left adrenal gland and kidney. Next, the lateral attachments of the spleen are divided, allowing the spleen and pancreas to be rotated superiorly off the left adrenal gland as a unit (Fig. 4-7, A).
The left adrenal vein is identified as it exits the left adrenal gland and enters into the left renal vein (Fig. 4-7, B). The left adrenal vein is then divided with surgical clips. The remaining attachments to the retroperitoneum and arterial branches can then be divided with an energy device or surgical clips, as described previously for the right adrenalectomy. It is important to note the left inferior phrenic artery and vein as they descend from the diaphragm to the superior pole of the left adrenal gland, which can be prominent and may need to be divided with surgical clips (Fig. 4-7, C).
Assalia, A, Gagner, M. Laparoscopic adrenalectomy. Br J Surg. 2004;91(10):1259–1274.
Barresi, R, Prinz, RA. Laparoscopic adrenalectomy. Arch Surg. 1999;134:212–217.
Kebebew, E, Siperstein, AE, Clark, OH, Duh, QY. Results of laparoscopic adrenalectomy for suspected and unsuspected malignant adrenal neoplasms. Arch Surg. 2002;137:948–953.
Mazzaglia, PA, Vezeridis, MP. Laparoscopic adrenalectomy: balancing the operative indications with the technical advances. J Surg Oncol. 2010;101(8):739–744.
National Institutes of Health (NIH). Consensus Development program. http://consensus.nih.gov/2002/2002adrenalincidentalomasos021html.htm, 2002.