Chapter 1 Landmarks in the History of Neurosurgery
Prehistoric Period: The Development of Trephination
In many museum and academic collections around the world are examples of the earliest form of neurosurgery—skull trephination.1–4 A number of arguments and interpretations have been advanced by scholars as to the origin and surgical reasons for this early operation—to date no satisfactory answers have been found. Issues of religion, treatment of head injuries, release of demons, and treatment of headaches have all been offered. Unfortunately, no adequate archaeological materials have surfaced to provide us with an answer. In reviewing some of the early skulls the skills of these early surgeons were quite remarkable. Many of the trephined skulls show evidence of healing, proving that these early patients survived the surgery. Figure 1.1 shows examples of two early (Peru circa AD 800) skulls that have been trephined and show evidence of premorbid bone healing. In the Americas the tumi was the most common surgical instrument used to perform a trephination and some examples of these tumis are shown in Figure 1.1. In Figure 1.2 is a fine example of a well-healed gold inlay cranioplasty done by an early South American surgeon.
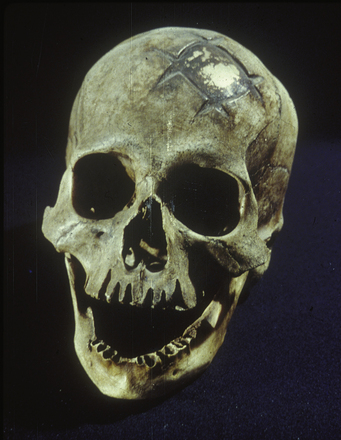
FIGURE 1.2 An early cranioplasty done with a gold inlay which is well healed.
(From the Museum of Gold, Lima, Peru.)
Included in many museum and private collections are examples of terra cotta and stone figures and other carvings that clearly depicted several common neurological disorders. Commonly depicted by contemporary artisans were images of hydrocephalus, cranial deformation, spina bifida, and various forms of external injuries and scarring. We have added two examples from the Olmec and Mayan civilizations, where we see demonstrated a young adult with achondroplasia and a young adult with severe kyphoscolosis likely due to a myelomeningocele5 (Fig. 1-3).
Egyptian and Babylonian Medicine: Embryonic Period
The Egyptian period, covering some 30 successive dynasties, gave us the earliest known practicing physician—Imhotep (I-em-herep) (3000 BC). Imhotep (“he whom cometh in peace”) is considered the first medical demigod, one likely more skilled in magic and being a sage. From this period came three important medical and surgical documents that give us a contemporary view of the practice of surgery. These collections are the Ebers, Hearst, and Edwin Smith papyri, two of which are considered here.6,7
The Egyptians are well remembered for their skills developed in mummification. Historians have now shown that anatomical dissection was also performed in this period. An examination of the existing Egyptian papyri shows that the practice of medicine was based largely on magic and superstition. Therapeutic measures depended on simple principles, most of which allowed nature to provide restoration of health with little intervention. In treating skeletal injury the Egyptians realized that immobilization was important and they prescribed splints for that purpose. Their materia medica was impressive, as their substantial pharmacopeias attest.
Written some 500 years after Hammurabi (1792-1750 BC), and the oldest medical text believed to exist (including about 107 pages of hieratic writing), the Ebers papyrus is of interest for its discussion of contemporary surgical practice.7 The text discusses the removal of tumors, and recommends surgical drainage of abscesses.
The Edwin Smith papyrus, written after 1700 BC is considered to be the oldest book on surgery per se and is a papyrus scroll 15 feet in length and 1 foot in width (4.5 m by 0.3 m; Fig. 1.4).6 The text contains a total of 48 cases including those with injuries involving the spine and cranium. Each case is considered with a diagnosis followed by a formulated prognosis. Owing to the scholarly work of James Breasted this papyrus has been translated from the original Egyptian to English. The original document remains in the possession of the New York Academy of Medicine.6
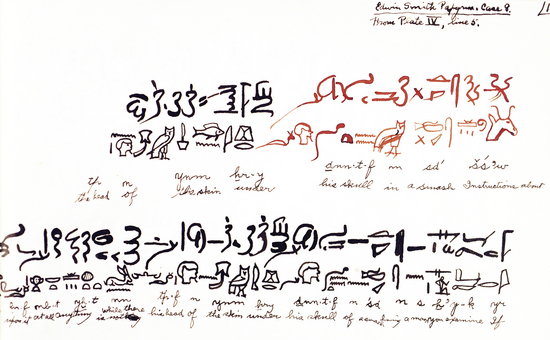
FIGURE 1.4 A manuscript leaf from the Breasted translation of the Hearst papyrus discussing a head injury.
(From Breasted JH. The Edwin Smith Papyrus. Published in Facsimile and Hieroglyphic Transliteration with Translation and Commentary. Chicago: University of Chicago Press; 1930; from the author’s collection.)
Greek and Early Byzantine Period: The Origins of Neurosurgery
The earliest medical writings from this period are those attributed to Hippocrates (460-370 BC), that most celebrated of the Asclepiadae, and his schools (Fig. 1.5).8 To Hippocrates we owe the description of a number of neurological conditions, many of them resulting from battlefield and sport injuries. Hippocrates was the first to develop the concept that the location of the injury to the skull was important in any surgical decision. The vulnerability of the brain to injury was categorized from lesser to greater by location, with injury to the bregma representing a greater risk than injury to the temporal region, which in turn was more dangerous than injury to the occipital region.9
Hippocrates wrote on a number of neurological conditions. From his Aphorisms is one of the earliest descriptions of subarachnoid hemorrhage: “When persons in good health are suddenly seized with pains in the head, and straightway are laid down speechless, and breathe with stertor, they die in seven days, unless fever comes on.”10
Hippocrates provides the first written detailed use of the trephine. Insightful, he argued for trephination in brain contusions but not in depressed skull fractures (the prognosis was too grave) and cautioned that a trephination should never be performed over a skull suture because of the risk of injury to the underlying dura. Hippocrates demonstrated good surgical technique when he recommended “watering” the trephine bit while drilling to prevent overheating and injury to the dura.
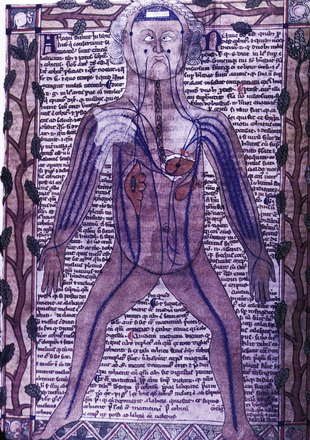
Herophilus of Chalcedon (fl. 335-280 BC) was an important early neuroanatomist who came from the region of the Bosporus and later attended the schools of Alexandria. Unlike his predecessors, Herophilus dissected human bodies in addition to those of animals—more than 100 by his own account. Herophilus was among the first to develop an anatomical nomenclature and form a language of anatomy. Among his contributions was tracing the origin of nerves to the spinal cord. He then divided these nerves into motor and sensory tracts. He made the important differentiation of nerves from tendons, which were often confused at that time. In his anatomical writings are the first anatomical descriptions of the ventricles and venous sinuses of the brain. From him comes the description of confluens sinuum or torcular Herophili. The first description of the choroid plexus occurs here, so named for its resemblance to the vascular membrane of the fetus. Herophilus described in detail the fourth ventricle and noted the peculiar arrangement at its base, which he called the “calamus scriptorius” because it “resembles the groove of a pen for writing.” Among his many other contributions was his recognition of the brain as the central organ of the nervous system and the seat of intelligence, in contrast to Aristotle’s cardiocentric view.11
All was not perfect with this anatomist as Herophilus is also remembered for introducing one of the longest standing errors in anatomical physiology: the rete mirabile (Fig. 1.6),12 a structure present in artiodactyls but not in humans. This structure acts as an anastomotic network at the base of the brain. This inaccurately described structure later became dogma and important in early physiological theories of human brain function. The rete mirabile was later erroneously described in detail by Galen of Pergamon and further canonized by later Arabic and medieval scholars. Scholarship did not erase this anatomical error until the sixteenth century, when the new anatomical accounts of Andreas Vesalius and Berengario da Carpi clearly showed it did not exist in humans.
Entering the Roman era and schools of medicine, we come to Aulus Cornelius Celsus (25 BC to AD 50). Celsus was neither a physician nor a surgeon; rather, he can best be described as a medical encyclopedist who had an important influence on surgery. His writings reviewed, fairly and with moderation, the rival medical schools of his time—dogmatic, methodic, and empiric. As counsel to the emperors Tiberius and Gaius (Caligula), he was held in great esteem. His book, De re Medicina,13 is one of the earliest extant medical documents after the Hippocratic writings. His writings had an enormous influence on early physicians. So important were his writings that when printing was introduced in the fifteenth century, Celsus’ works were printed before those of Hippocrates and Galen.
Celsus made a number of interesting neurosurgical observations. De re Medicina contains an accurate description of an epidural hematoma resulting from a bleeding middle meningeal artery.8 Celsus comments that a surgeon should always operate on the side of greater pain and place the trephine where the pain is best localized. Considering the pain sensitivity of dura and its sensitivity to pressure, this has proved to be good clinical acumen. Celsus provided accurate descriptions of hydrocephalus and facial neuralgia. Celsus was aware that a fracture of the cervical spine can cause vomiting and difficulty in breathing, whereas injury of the lower spine can cause weakness or paralysis of the legs, as well as urinary retention or incontinence.
Rufus of Ephesus (fl. AD 100) lived during the reign of Trajan (AD 98-117) in the coastal city of Ephesus. Many of Rufus’ manuscripts survived and became a heavy influence on the Byzantine and medieval compilers. As a result of his great skill as a surgeon, many of his surgical writings were still being transcribed well into the sixteenth century.14 Rufus’ description of the membranes covering the brain remains a classic. Rufus clearly distinguished between the cerebrum and cerebellum, and gives a credible description of the corpus callosum. He had a good understanding of the anatomy of the ventricular system with clear details of the lateral ventricle; he also described the third and fourth ventricles, as well as the aqueduct of Sylvius. Rufus also provided early anatomical descriptions of the pineal gland and hypophysis, and his accounts of the fornix and the quadrigeminal plate are accurate and elegant. He was among the first to describe the optic chiasm and recognized that it was related to vision. The singular accuracy of Rufus’ studies must be credited to his use of dissection (mostly monkeys) in an era when the Roman schools were avoiding hands-on anatomical dissection.
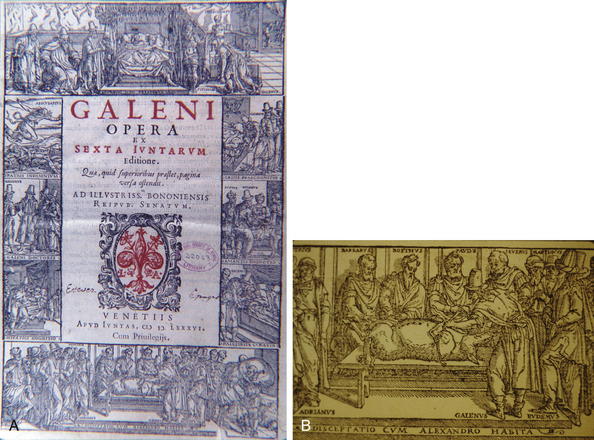
His experience as a physician and his scientific studies enabled Galen to make a variety of contributions to neuroanatomy. Galen was the first to differentiate the pia mater and the dura mater. Among his contributions were descriptions of the corpus callosum, the ventricular system, the pineal and pituitary glands, and the infundibulum. Long before Alexander Monro’s Secundus (1733-1817) eighteenth century anatomical description, Galen clearly described the structure now called the foramen of Monro. He also gave an accurate description of the aqueduct of Sylvius. He performed a number of interesting anatomical experiments, such as transection of the spinal cord, leading him to describe the resultant loss of function below the level of the cut. In a classic study on the pig he sectioned the recurrent laryngeal nerve and clearly described that hoarseness was a consequence (Fig. 1.7). Galen provides the first recorded attempt at identifying and numbering the cranial nerves. He described 11 of the 12 nerves, but by combining several, he arrived at a total of only seven. He regarded the olfactory nerve as merely a prolongation of the brain and hence did not count it.15
In viewing brain function Galen offered some original concepts. He believed the brain controlled intelligence, fantasy, memory, and judgment. This was an important departure from the teaching of earlier schools, for example, Aristotle’s cardiocentric view. Galen discarded Hippocrates’ notion that the brain is only a gland and attributed to it the powers of voluntary action and sensation.
With animal experimentation Galen recognized that cervical injury can cause disturbance in arm function. In a study of spinal cord injury, Galen detailed a classic case of what is today known as Brown-Séquard syndrome—i.e., a hemiplegia with contralateral sensory loss in a subject with a hemisection of the cord.16 Galen’s description of the symptoms and signs of hydrocephalus is classic. This understanding of the disease enabled him to predict which patients with hydrocephalus had a poorer prognosis. Galen was much more liberal in the treatment of head injury than Hippocrates, arguing for more aggressive elevation of depressed skull fractures, fractures with hematomas, and comminuted fractures. Galen recommended removing the bone fragments, particularly those pressing into the brain. Galen was also more optimistic than Hippocrates about the outcome of brain injuries, commenting that “we have seen a severely wounded brain healed.”
Paul of Aegina (AD 625-690), trained in the Alexandrian school, is considered the last of the great Byzantine physicians. He was a popular writer who compiled works from both the Latin and Greek schools. His writings remained extremely popular, being consulted well into the seventeenth century. Beside his medical skills Paul was also a skilled surgeon to whom patients came from far and wide. He venerated the teachings of the ancients as tradition required, but also introduced his own techniques with good results. This author is best remembered for his classic work, The Seven Books of Paul of Aegina, within which are excellent sections on head injury and the use of the trephine.17,18 Paul classified skull fractures in several categories: fissure, incision, expression, depression, arched fracture, and, in infants, dent. In skull fractures he developed an interesting skin incision which involved two incisions intersecting one another at right angles, giving the Greek letter X. One leg of the incision incorporated the scalp wound. To provide comfort for the patient the ear was stuffed with wool so that the noise of the trephine would not cause undue distress. In offering better wound care he dressed it with a broad bandage soaked in oil of roses and wine, with care taken to avoid compressing the brain.18
The hydrocephalic affection … occurs in infants, owing to their heads being improperly squeezed by midwives during parturition, or from some other obscure cause; or from the rupture of a vessel or vessels, and the extravasated blood being converted into an inert fluid … (Paulus Aeginetes).18
An innovative personality, he designed a number of surgical instruments for neurosurgical procedures. Illustrated in his early manuscripts are a number of tools including elevators, raspatories, and bone-biters. An innovation for his trephine bits was a conical design to prevent plunging, and different biting edges were made for ease of cutting. Reviewing his wound management reveals some sophisticated insights—he used wine (helpful in antisepsis, although this concept was then unknown) and stressed that dressings should be applied with no compression to the brain. Paul of Aegina was later to have an enormous influence on Arabic medicine and in particular on Albucasis, the patriarch of Arabic/Islamic surgery.19
Arabic and Medieval Medicine: Scholarship with Intellectual Somnolence
Arabic/Islamic Scholarship
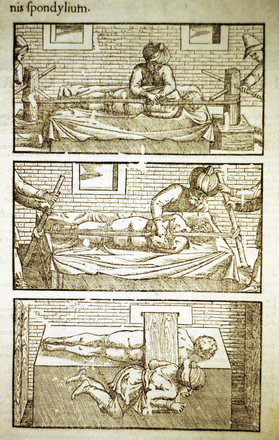
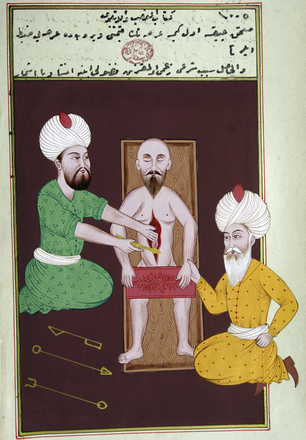
In this era of Islamic medicine we see introduced a now common medical tradition—bedside medicine with didactic teaching. Surgeons, with rare exceptions, remained in a class of low stature. One unfortunate practice was the reintroduction of the Egyptian technique of using a red-hot cautery iron, applied to a wound, to control bleeding. In some cases hot cautery was used instead of the scalpel to create surgical incisions, and this practice clearly led to a burned and subsequent poorly healed wound (Fig. 1.8).
An important Islamic scholar of this period, as reflected in his writings, was Rhazes (Abu Bakr Muhammad ibn Zakariya’ al-Razi, AD 845–925). Reviewing his works one sees clearly a scholarly physician, loyal to Hippocratic teachings, and learned in diagnosis. Although primarily a court physician and not a surgeon, he provided writings on surgical topics that remained influential through the eighteenth century.20 Rhazes was one of the first to discuss and outline the concept of cerebral concussion. Head injury, he wrote, is among the most devastating of all injuries. Reflecting some insight he advocated surgery only for penetrating injuries of the skull as the outcome was almost always fatal. Rhazes recognized that a skull fracture causes compression of the brain and thereby requires elevation to prevent lasting injury. Rhazes also understood that cranial and peripheral nerves have both a motor and sensory component. In designing a surgical scalp flap one needed to know the anatomy and pathways of the nerves so as to prevent a facial or ocular palsy.
Avicenna (Abu ‘Ali al-Husayn ibn ‘Abdallah ibn Sina, AD 980-1037), the famous Persian physician and philosopher of Baghdad, was known as the “second doctor” (the first being Aristotle). During the Middle Ages his works were translated into Latin and became dominant teachings in the major European universities until well into the eighteenth century. With the introduction of the printed book it has been commented that his Canon (Q’anun) was the second most commonly printed book after the Bible. Avicenna disseminated the Greek teachings so persuasively that their influence remains an undercurrent to this day. In his major work, Canon Medicinae (Q’anun), an encyclopedic effort founded on the writings of Galen and Hippocrates, the observations reported are mostly clinical, bearing primarily on materia medica (Fig. 1.9).21 Avicenna’s medical philosophy primarily followed the humoral theories of Hippocrates along with the biological concepts of Aristotle. Within Avicenna’s Canon (Q’anun) are a number of interesting neurological findings, such as the first accurate clinical explanation of epilepsy, for which treatment consisted of various medications and herbals along with the shock of the electric eel. He describes meningitis and recognized it was an infection and inflammation of the meninges. It appears that Avicenna might have conducted anatomical studies inasmuch as he gives a correct anatomical discussion of the vermis of the cerebellum and the “tailed nucleus,” now known as the caudate nucleus. Avicenna introduced the concept of a tracheostomy using a gold or silver tube placed into the trachea and provided a number of innovative techniques for treating spine injuries and included some devices for stabilizing the injured spine. Avicenna also had some insightful thoughts on the treatment of hydrocephalus. He recognized that external hydrocephalus (fluid between the brain and dura) could be drained with low morbidity risk. However, true internal hydrocephalus was more dangerous to treat and best left alone or treated with herbals and medications.22 The Canon (Q’anun) was clearly his greatest contribution, along with his collation and translation of Galen’s collected works, a book that remained a dominant influence until well into the eighteenth century.
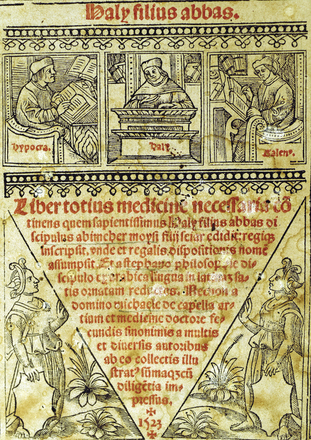
A personality often overlooked in neurosurgical history was a prominent Persian/Islamic physician by the name of Haly Abbas (Abdul-Hasan Ali Ibn Abbas Al Majusi) (?AD 930-944). This writer from the Golden Age of Islamic medicine produced a work called The Perfect Book of the Art of Medicine,23 also known as the Royal Book (Fig. 1.10). Born and educated in Persia, a place he never left, it was here he produced his important writings on medicine. In his book he dedicated 110 chapters to surgical practice. A review of his work shows that his writings on spine injuries were essentially copied from the earlier Greek writers, in particular Paul of Aegina, and consisted mostly of external stabilization of spinal column injuries. Surgical intervention via a scalpel was rarely advocated. In his nineteenth discourse, Chapters 84 and 85 is clearly presented his management of depressed skull fractures. He also described the different types of fractures that can occur along with potential mechanisms of injury. He clearly appreciated that the dura should be left intact and not violated, the exception being those fractures where the skull bone had penetrated through the dural membrane, in which case these fragments needed to be removed. His technique of elevating a bone flap involved drilling a series of closely placed holes and then connecting them with a chisel. He showed some interesting consideration for the patient by advocating placing a ball of wool into the ears so as to block the sounds from the drilling. The head wound was then dressed with a wine-soaked dressing, the wine likely providing a form of antisepsis. In these chapters are also an interesting discussion about intraoperative brain swelling and edema, in which case the surgeon should look further for possible retained bone fragments and remove them. If later swelling occurred from too tight a head dressing, then it should be loosened. Unfortunately, Haly Abbas also advocated cephalic vein bleeding and inducing diarrhea for those who did not respond well; such primitive techniques were not to be abandoned until the mid-nineteenth century.
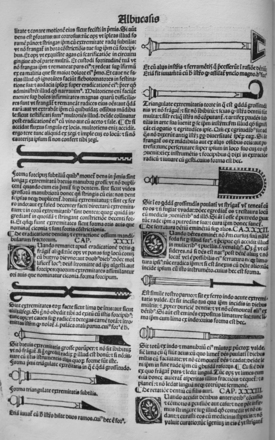
In the Islamic tradition Albucasis (Abu al-Qasim Khalaf ibn al-Abbas Al-Zahrawi, AD 936-1013) was both a great compiler as well as a serious scholar, whose writings (some 30 volumes!) were focused mainly on surgery, dietetics, and materia medica. In the introduction to his Compendium24 there is an interesting discussion of why the Islamic physician had made such little progress in surgery—he attributed this failure to a lack of anatomical study and inadequate knowledge of the classics. One unfortunate medical practice that he popularized was the frequent use of emetics as prophylaxis against disease, a debilitating medical practice that survived, as “purging,” into the nineteenth century.
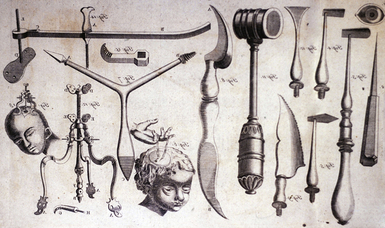
The final section of the Compendium is the most important part for surgeons and includes a lengthy summary of surgical practice at that time.24–26 This work was used extensively in the schools of Salerno and Montpellier and hence was an important influence in medieval Europe. A unique feature of this text was the illustrations of surgical instruments along with descriptions of their use, which Albucasis detailed in the text. Albucasis designed many of the instruments, and some were based on those described earlier by Paul of Aegina. His design of a “nonsinking” trephine is classic (he placed a collar on the trephine to prevent plunging) and was to become the template of many later trepan/trephine designs (Fig. 1.11).
For hydrocephalus (following the teachings of Paul of Aegina, he associated the disorder with the midwife grasping the head too roughly) Albucasis recommended drainage, although he noted that the outcome was almost always fatal. He attributed these poor results to “paralysis” of the brain from relaxation. With regard to the site for drainage, Albucasis noted that the surgeon must never cut over an artery, as hemorrhage could lead to death. In the child with hydrocephalus he would “bind” the head with a tight constricting head wrap and then put the child on a “dry diet” with little fluid—in retrospect a progressive treatment plan for hydrocephalus.25,26
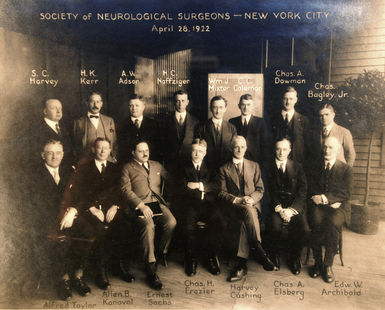
An important figure in the history of surgery, and one who bridged the Islamic and medieval schools, was Serefeddin Sabuncuoglu (1385-1468). Sabuncuoglu was a prominent Ottoman surgeon who lived in Amasya, a small city in the northern region of Asia Minor, part of present-day Turkey. This was a glorious period for the Ottoman Empire and Amasya was a major center of commerce, culture, and art. While working as a physician at Amasya Hospital, and at the age of 83, he wrote a medical book entitled Cerrahiyyetü’l-Haniyye [Imperial Surgery], which is considered the first colored illustrated textbook of Turkish medical literature.27–30 There are only three known copies of this original manuscript, two are in Istanbul and the third at the Bibliothèque Nationale in Paris.27 First written in 1465 the book consists of three chapters dealing with 191 topics, all dealing with surgery. Each topic consists of a single, poetical sentence in which the diagnosis, classification, and surgical technique of a particular disease are described in detail. This book is unique for this period in that virtually all the surgical procedures and illustrations were drawn in color, even though drawings of this type were prohibited in the Islamic religion (Fig. 1.12).
Medieval Europe
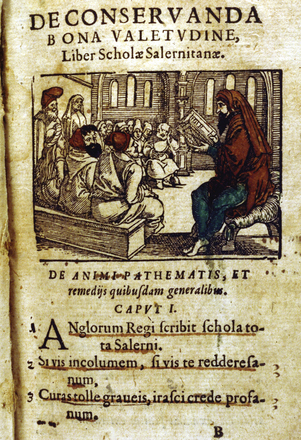
Constantinus Africanus (Constantine the African) (1020-1087) introduced Islamic medicine to the school of Salerno and thus to Europe (Fig. 1.13). Constantine had studied in Baghdad, where he came under the influence of the Islamic/Arabic scholars. Later, he retired to the monastery at Monte Cassino and there translated Arabic manuscripts into Latin, some scholars say rather inaccurately. Thus began a new wave of translation and transliteration of medical texts, this time from Arabic back into Latin.31 His work allows one to gauge how much medical and surgical knowledge was lost or distorted by multiple translations, particularly of anatomical works. It is also notable that Constantine reintroduced anatomical dissection with an annual dissection of a pig. Unfortunately the anatomical observations that did not match those recorded in the early classical writings were ignored! As had been the theme for the previous 400 years surgical education and practice continued to slumber.
Roger of Salerno (fl. 1170) was a surgical leader in the Salernitan tradition, the first writer on surgery in Italy. His work on surgery was to have a tremendous influence during the medieval period (Fig. 1.14). His Practica Chirurgiae offered some interesting surgical techniques.32 Roger introduced an unusual technique of checking for a tear of the dura, i.e., cerebrospinal fluid (CSF) leakage, in a patient with a skull fracture by having the patient hold his breath (Valsalva maneuver) and then watching for a CSF leak or air bubbles. A pioneer in the techniques of managing nerve injury, he argued for reanastomosis of severed nerves. During the repair he paid particular attention to alignment of the nerve fasicles. Several chapters of his text are devoted to the treatment of skull fractures. The following is a discussion of a skull fracture:
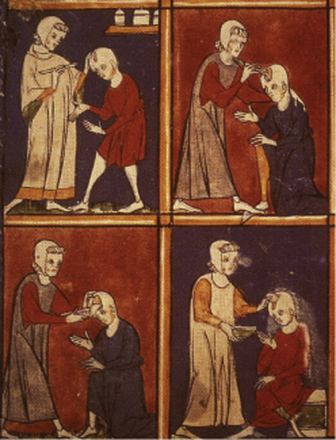
FIGURE 1.14 This early medieval manuscript illustrates a craniotomy being performed by Roger of Salerno.
(From Bodleian Library, Oxford, UK.)
When a fracture occurs it is accompanied by various wounds and contusions. If the contusion of the flesh is small but that of the bone great, the flesh should be divided by a cruciate incision down to the bone and everywhere elevated from the bone. Then a piece of light, old cloth is inserted for a day, and if there are fragments of the bone present, they are to be thoroughly removed. If the bone is unbroken on one side, it is left in place, and if necessary elevated with a flat sound (spatumile) and the bone is perforated by chipping with the spatumile so that clotted blood may be soaked up with a wad of wool and feathers. When it has consolidated, we apply lint and then, if it is necessary (but not until after the whole wound has become level with the skin), the patient may be bathed. After he leaves the bath, we apply a thin cooling plaster made of wormwood with rose water and egg.32
In reviewing the writings of Roger of Salerno we see little offered that is new in the field of anatomy. He contented himself with recapitulating earlier treatises, in particular those of Albucasis and Paul of Aegina. He strongly favored therapeutic plasters and salves; fortunately he was not a strong advocate of the application of grease to dural injuries. Citing the writings of The Bamberg Surgery,33 he advocated trephination in the treatment of epilepsy.
An unusually inventive medieval surgeon, Theodoric Borgognoni of Cervia (1205-1298) is remembered as a pioneer in the use of aseptic technique—not the “clean” aseptic technique of today but rather a method based on avoidance of “laudable pus.” He made a number of attempts to discover the ideal conditions for good wound healing; he concluded that they comprised control of bleeding, removal of contaminated or necrotic material, avoidance of dead space, and careful application of a wound dressing bathed in wine—views that are remarkably modern for the times (Fig. 1.15).
Theodoric’s surgical work, written in 1267, provides a unique view of medieval surgery.34 He argued for meticulous (almost Halstedian!) surgical techniques. The aspiring surgeon was to train under competent surgeons and be well read in the field of head injury. Interestingly, he argued that parts of the brain could be removed through a wound with little effect on the patient. He appreciated the importance of skull fractures, especially depressed ones, recognizing that they should be elevated. He believed that punctures or tears of the dura mater could lead to abscess formation and seizures. To provide comfort for the patient about to undergo surgery, he developed his own “soporific sponge,” which contained opium, mandragora, hemlock, and other ingredients. It was applied to the nostrils until the patient fell asleep. He describes results in improved comfort that were better for both patient and surgeon (Figs. 1.16, 1.17).

FIGURE 1.17 Medieval anatomist performing a dissection of the head.
(From Guido de Papia (Papaya), Anatomia circa 1325. Musèe Condé, Chantilly, France.)
William of Saliceto (1210-1277) might be considered the ablest surgeon of the thirteenth century. A professor at the University of Bologna, William of Saliceto wrote his Chirurgia,35 which many consider to be highly original, though it does carry the strong influence of Galen and Avicenna. To his credit William replaced the Arabic technique of incision by cautery with the surgical knife. He also devised techniques for nerve suture. In neurology, he recognized that the cerebrum governs voluntary motion and the cerebellum involuntary function.
Leonard of Bertapalia (1380?–1460) was a prominent figure in medieval surgery. Leonard came from a small town near Padua and established an extensive and lucrative practice there and in nearby Venice. He was among the earliest proponents of anatomical research—in fact, he gave a course of surgery in 1429 that included the dissection of an executed criminal. Leonard had a strong interest in head injury—he ended up devoting a third of his book to surgery of the nervous system.36,37 He considered the brain the most precious organ, regarding it as the source of voluntary and involuntary functions. He provided some interesting and accurate insights into the management of skull fracture. He argued that the surgeon should always avoid materials that might cause pus, always avoid the use a compressive dressing that might drive bone into the brain, and if a piece of bone pierces the brain, remove it!
Lanfranchi of Milan (c. 1250-1306), a pupil of William of Saliceto, continued his teacher’s practice of using a knife instead of cautery. In his Cyrurgia Parva he pioneered the use of suture for wound repair.38 His guidelines for performing trephination in skull fractures and “release of irritation” of dura are classic. He even developed a technique of esophageal intubation for surgery, a technique not commonly practiced until the late nineteenth century.
Guy de Chauliac (1298-1368) was the most influential surgeon of the fourteenth and fifteenth centuries and a writer of rare learning and fine historical sense. So important to surgical practice did Guy de Chauliac’s Ars Chirurgica become, it was copied and translated into the seventeenth century, a span of nearly 400 years. Most historians consider this surgical manual to be the principal didactic surgical text of this era.39,40
Sixteenth Century: Anatomical Exploration
With the beginnings of the Renaissance profound changes began to occur in surgical practices. To resolve medical and surgical practice issues, both physicians and surgeons reintroduced basic hands-on investigative techniques. Of profound influence was the now routine practice of anatomical dissection of humans. A series of prominent figures including Leonardo da Vinci, Berengario da Carpi, Johannes Dryander, Andreas Vesalius, and others led the movement. Anatomical errors, many ensconced since the Greco-Roman era, were corrected, and a greater interest in surgery developed. This radically inventive period and its personalities laid the foundations of modern neuroanatomy and neurosurgery.
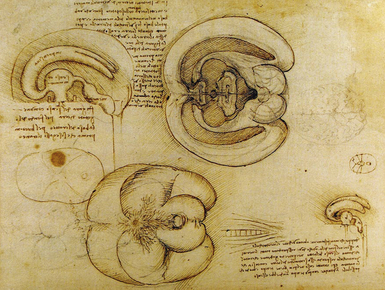
Leonardo da Vinci (1452-1519) was the quintessential Renaissance man. Multitalented, recognized as an artist, an anatomist, and a scientist, Leonardo went to the dissection table so as to better understand surface anatomy and its bearing on his artistic creations. On the basis of these studies he founded iconographic and physiological anatomy.41–43 Leonardo, being a well-read man, was familiar with the writings of Galen, Avicenna, Mondino, and others. From his knowledge of these writings he developed an understanding of their anatomical errors.
To Leonardo’s studies we owe a number of anatomical firsts. Leonardo provided the first crude diagrams of the cranial nerves, the optic chiasm, and the brachial and lumbar plexuses. Leonardo made the first wax casting of the ventricular system and in so doing provided the earliest accurate view of this anatomy. His wax casting technique involved removing the brain from the calvarium and injecting melted wax through the fourth ventricle. Tubes were placed in the lateral ventricles to allow air to escape. When the wax hardened he removed the brain, leaving a cast behind—simple but elegant (Fig. 1.18).
In connection with his art studies he developed the concept of “antagonism” in muscle control. His experimental studies included sectioning a digital nerve and noting that the affected finger no longer had sensation, even when placed in a fire. Leonardo had great plans for publishing a stupendous opus on anatomy, which was to be issued in 20 volumes. The work did not appear owing to the early death of his collaborator, Marcantonio della Tore, who died in 1509.44 From 1519, the year of Leonardo’s death, until the middle of the sixteenth century, his anatomical manuscripts circulated among Italian artists through the guidance of Francesco da Melzi, Leonardo’s associate. Sometime in the mid- to late sixteenth century the anatomical manuscripts were lost, and were rediscovered only in the eighteenth century, by William Hunter.
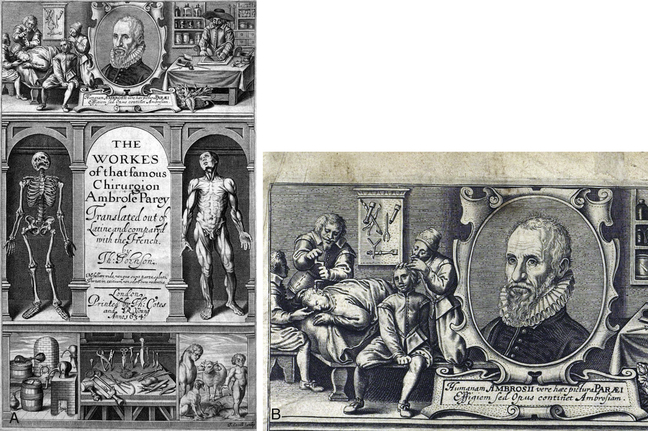
In reviewing Paré’s surgical works,45,46 the part on the brain best reflects a contemporary surgical practice. Book X is devoted to skull fractures. Paré reintroduced the earlier technique of elevating a depressed skull fracture by using the Valsalva maneuver: “… for a breath driven forth of the chest and prohibited passage forth, swells and lifts the substance of the brain and meninges where upon the frothing humidity and sanies sweat forth.”36 This maneuver also assisted in the expulsion of blood and pus (Fig. 1.19).
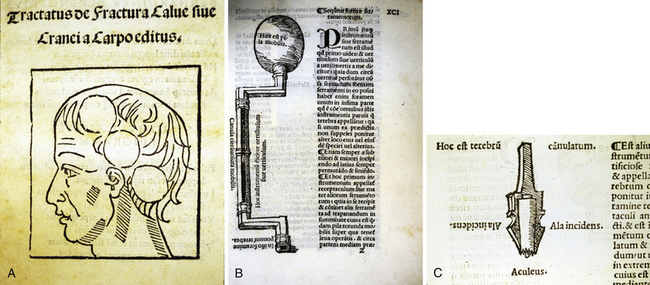
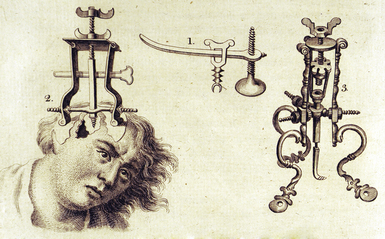
In 1518 a remarkable book by Giacomo Berengario da Carpi (1460-1530) appeared.47 This book came about because of Berengario’s success in treating Lorenzo de’ Medici, Duke of Urbino, who had received a serious cranial injury and survived. In a dream that occurred shortly after this episode Berengario was visited by the god Hermes Trismegistus (Thrice-Great Mercury), who encouraged him to a write a treatise on head injuries. As a result of this dream Berengario’s Tractatus appeared and was the first printed work devoted solely to treating injuries of the head. Not only are original surgical techniques discussed but also illustrations of the cranial instruments for dealing with skull fractures are provided (Fig. 1.20). Berengario introduced the use of interchangeable cranial drill bits for trephination. Included in the text are a number of case histories with descriptions of the patients, methods of treatment, and clinical outcomes. This work remains our best sixteenth century account of brain surgery.
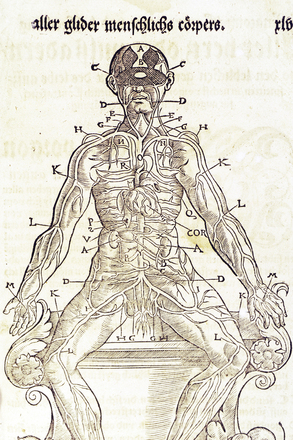
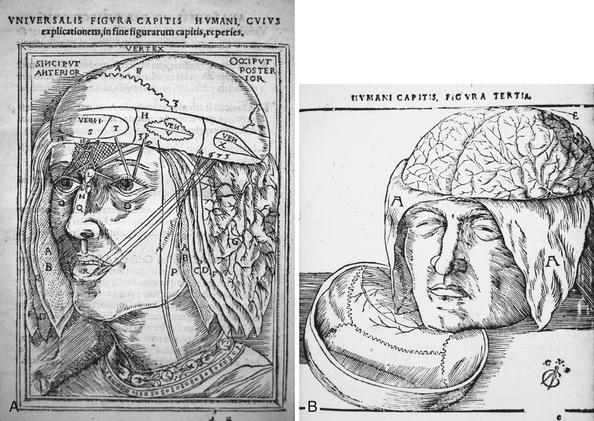
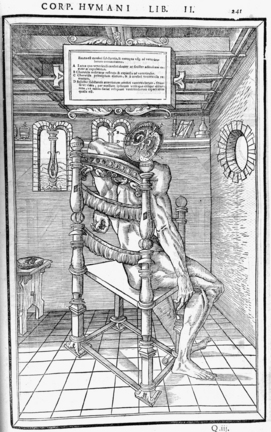
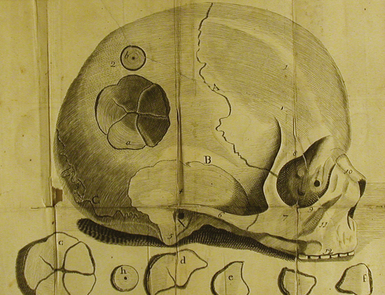
An important book, Anatomiae, is most likely the earliest to deal with “accurate” neuroanatomy and appeared in 1536 (with an expanded version in 1537). The book was written by a professor of medicine from Marburg, Johannes Dryander (Johann Eichmann, 1500-1560).48,49 This work contains a series of full-page plates showing successive Galenic dissections of the brain (Fig. 1.21). Dryander starts with a scalp dissection in layers. He continues a series of “layers,” removing the skull cap. He next illustrates the meninges, brain, and posterior fossa. The first illustration of the metopic suture appears in one of the skull figures. Important to Dryander’s studies was the performance of public dissections of the skull, dura, and brain, the results of which he details in this monograph. In one image is depicted the ventricular system and the cell doctrine theory in which imagination, common sense, and memory are placed within the ventricles. There are a number of inaccuracies in the work, reflecting medieval scholasticism, but despite these errors this book should be considered the first textbook of neuroanatomy.
Volcher Coiter (1534-1576) was an army surgeon and city physician at Nuremberg who had the good fortune to study under Fallopius, Eustachius, and Aldrovandi. These scholars provided the impetus for Coiter’s original anatomical and physiological investigations. He described the anterior and posterior spinal roots and distinguished gray from white matter in the spinal cord. His interest in the spine led him to conduct anatomical and pathological studies of the spinal cord, including a study on the decerebrate model. He performed a number of experiments on living subjects including work that predated William Harvey on the beating heart. He trephined the skulls of birds, lambs, goats, and dogs, and was the first to associate the pulsation of the brain with the arterial pulse. He even opened the brain and removed parts of it, reporting no ill effects—an early, surprising attempt at cerebral localization.50 Because of his enthusiastic anatomical studies via human dissection he ran afoul of the Inquisition and ended up being jailed by the Counter-Reformation, who held great distrust of physicians and anatomists who were challenging already accepted studies.
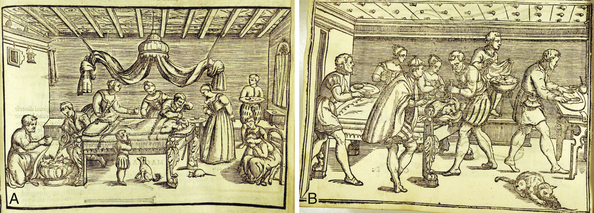
Using a combination of surgical skill and a Renaissance flair for design, Giovanni Andrea della Croce (1509?–1580)51 produced some very early engraved scenes of neurosurgical operations. The scenes are impressive to view as the surgeries were performed in family homes, and typically in the bedrooms. Most of the neurosurgical procedures illustrated were trephinations (Fig. 1.22). Croce also provides a series of newly designed trephines with safety features to prevent plunging. An unusual innovation involved his trephine drill, which was rotated by means of an attached bow, copying the style of a carpenter’s drill. Various trephine bits with conical designs are proposed and illustrated. Included in his armentarium are illustrations of surgical instruments that include some cleverly designed elevators for lifting depressed bone. In reviewing Croce’s book we find it is mainly a compilation of earlier authorities from Hippocrates to Albucasis, but his recommendations for treatment and his instrumentation are surprisingly modern.
Vesalius’s anatomical studies culminated in a masterpiece, De Humani Corporis Fabrica, published in 1543.52 In Book VII is the section on the anatomy of the brain that presents detailed anatomical discussions along with excellent engravings (Fig. 1.23). Vesalius noted that “heads of beheaded men are the most suitable [for study] since they can be obtained immediately after execution with the friendly help of judges and prefects.”53
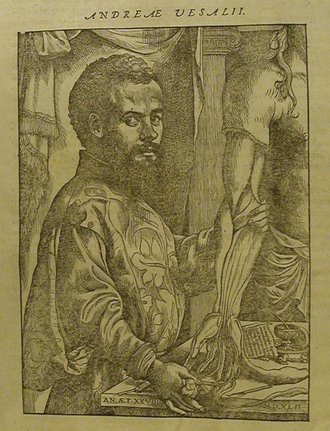
FIGURE 1.23 Portrait of the great anatomist Andreas Vesalius demonstrating a dissection of the arm from his magnum opus.
(From Vesalius A. De Humani Corporis Fabrica Libri Septem. Basel: Joannes Oporinus; 1543.)
Vesalius was primarily a surgeon and the section of text on the brain and the dural coverings discusses mechanisms of injury and how the various membranes and bone have been designed to protect the brain.53 Interestingly, close examination of several of the illustrated initial letters in the text shows little cherubs performing trephinations! For neurosurgeons Vesalius made an interesting early contribution to the understanding of hydrocephalus: In Book 1 is a discussion of “Heads of other shape” wherein he provides the following early description of a child with hydrocephalus:
… at Genoa a small boy is carried from door to door by a beggar woman, and was put on display by actors in noble Brabant in Belgium, whose head, without any exaggeration, is larger than two normal human heads and swells out on either side.52
In the second edition (1555) of his work,54 Vesalius describes a second case, that of hydrocephalus in a young girl whom he noted to have a head “larger than any man’s,” and at autopsy he describes the removal of 9 lb of water. As a result of these studies Vesalius made the important observation that fluid (i.e., cerebrospinal fluid) collects in the ventricles and not between the dura and skull, an earlier Hippocratic error. Vesalius made a number of interesting clinical observations but offered no insight into any effective treatment, either surgical or medical.
A remarkable work on anatomy by Charles Estienne (1504-1564) appeared in Paris in 1546.55 This book was the fifth in a series of books on anatomy to be published in Europe, following Berengario da Carpi (two books), Dryander, and Vesalius. Although published 3 years after Andreas Vesalius’ work, the book had actually been completed in 1539, but legal problems delayed publication. This work contains a wealth of beautiful but bizarre anatomical plates with the subjects posed against sumptuous, imaginative Renaissance backgrounds (Fig. 1.24). The anatomical detail clearly lacks the details of Vesalius and the book repeats many of the errors of Galen. The plates on the nervous system are quite graphic but flawed in the anatomical details. A typical plate shows a full anatomical figure with the skull cut to show the brain. Although gross structures like the ventricle and cerebrum are recognizable they do lack solid anatomical details.
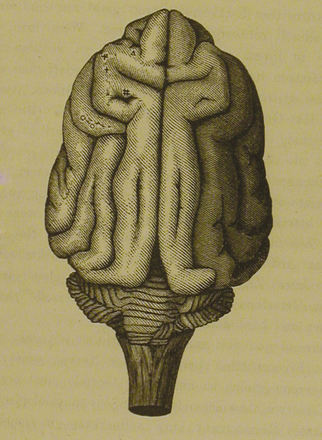
Seventeenth Century: Origins of Neurology
Within this century came the first intense exploration of the human brain. Leading the many investigators was Thomas Willis (1621-1675), after whom the circle of Willis is named (Fig. 1.25). A fashionable London practitioner, educated at Oxford, Willis published his Cerebri Anatome in London in 1664 (Fig. 1.26).56 With its publication we have now the first accurate anatomical study of the human brain. Willis was assisted in this work by Richard Lower (1631-1691). In Chapter VII Lower demonstrates by laboratory experimentation that when parts of the “circle” were tied off, the anastomotic network still provided blood to the brain. Lower noted, “if by chance one or two [of its arteries] should be stopt, there might easily be found another passage instead of them . . .” (see Figure 1a, p. 27).56 The striking brain engravings were drawn and engraved by the prominent London personality, Sir Christopher Wren (1632-1723), who was often present at Willis’ dissections. Most surgeons are not aware that the eponym was not applied to the circle until Albrecht Haller used it in his eighteenth century bibliography on anatomy.57,58
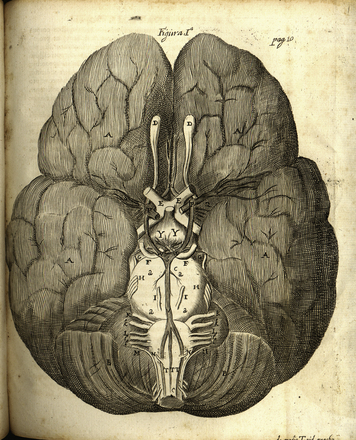
FIGURE 1.26 Thomas Willis’ Cerebri Anatome, published in 1664, showing his depiction of what is now called the circle of Willis. The eponym for the circle of Willis did not appear until the eighteenth century when Albrecht Haller assigned it in his anatomical bibliography.57
(From Willis T. Cerebri Anatome: Cui Accessit Nervorum Descriptio et Usus. London: J. Flesher; 1664.)
To Thomas Willis we owe the introduction of the concept of “neurology,” or the doctrine of neurons, here using the term in a purely anatomical sense. The word neurology did not enter general use until Samuel Johnson defined it in his dictionary of 1765, in which the word neurology now encompassed the entire field of anatomy, function, and physiology. The circle of Willis was also detailed in other anatomical works of this period by Vesling,59 Casserius,60 Fallopius,61 and Humphrey Ridley.62
Another important work on the anatomy of the brain appeared under the authorship of Humphrey Ridley (1653-1708). The book was unique in that it was written in the vernacular (English), not the usual academic Latin, and became widely circulated (Fig. 1.27).62 Ridley was educated at Merton College, Oxford, and at the University of Leiden, where he received his doctorate in medicine in 1679. At the time his work on the brain appeared, many ancient theories of the brain were still prevalent. Shifting away from the earlier cell doctrine theory, seventeenth century anatomists came to recognize the brain as a distinct anatomical entity. Cerebral function, instead of residing within the ventricles, was now known to be a property of the brain parenchyma.
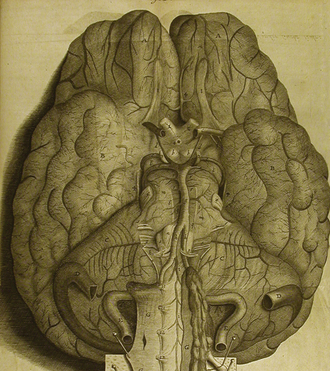
FIGURE 1.27 Circle of Willis as detailed by Ridley in an anatomically more correct rendition than that of Willis.
(From Ridley H. The Anatomy of the Brain, Containing its Mechanisms and Physiology: Together With Some New Discoveries and Corrections of Ancient and Modern Authors Upon That Subject. London: Samuel Smith; 1695.)
Ridley described a number of original observations in this volume on brain anatomy. He ingeniously conducted anatomical studies on freshly executed criminals, most of whom had been hanged. Ridley realized that hanging caused vascular engorgement of the brain and hence allowed easier identification of the anatomy. In reviewing his description of the circle of Willis we find an even more accurate view than Willis’. Ridley added a more complete account of both the posterior cerebral artery and the superior cerebellar artery. The anastomotic principle of this network was even further elucidated with his injection studies of the vessels. His understanding of the deep nuclei and, in particular, the anatomy of the posterior fossa, was superior to that of previous writers including Thomas Willis. The first accurate description of the fornix and its pathways appears in this monograph. Ridley provided an early and accurate description of the arachnoid membrane. Ridley’s book was not totally without error as he argues here in favor of the belief that the rete mirabile exists.
His large work, Observationum et Curationum, included over 600 surgical cases and a number of important and original observations on the brain.63 Congenital malformations, skull fractures, techniques for bullet extraction, and field surgical instruments are all clearly described. He performed operations for intracranial hemorrhage (with cure of insanity), vertebral displacement, congenital hydrocephalus, and occipital tumor (i.e., encephalocele) of the newborn; he also carried out trephinations for abscess and claimed a cure of an old aphasia. To remove a splinter of metal from the eye he used a magnet, a cure that enhanced his reputation.
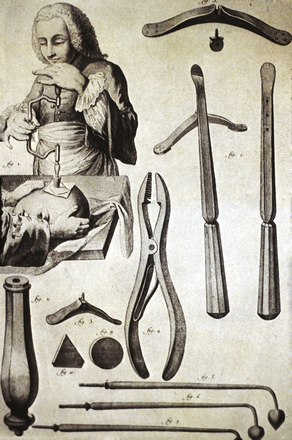
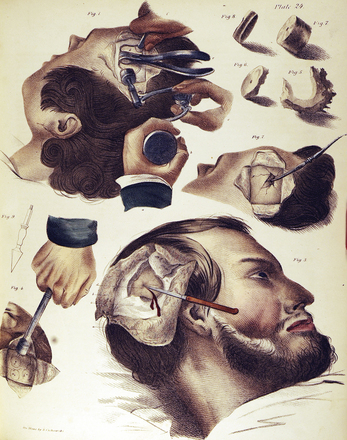
Johann Schultes (Scultetus) of Ulm (1595-1645) provided in his Armamentarium Chirurgicum XLIII the first descriptive details of neurosurgical instruments to appear since those published by Berengario in 1518.64 His book was translated into many languages, influencing surgery throughout Europe. Its importance lies in the exact detail of surgical instrument design and in the presentation of tools from antiquity to the present. Interestingly a number of the instruments illustrated by Scultetus are still in use today. Scultetus details a variety of surgical procedures dealing with injuries of the skull and brain. The text is further enhanced by some of the best seventeenth century illustrations detailing surgical technique (Fig. 1.28).

FIGURE 1.28 Seventeenth century neurosurgical trephination techniques as detailed by Scultetus.
(From Scultetus J. Armamentarium Chirurgicum XLIII. Ulm: Balthasar Kühnen; 1655.)
James Yonge (1646-1721) was among the first since Galen to argue emphatically that “wounds of the brain are curable.” Appropriately enough, Yonge’s remarkable little monograph was entitled Wounds of the Brain Proved Curable.65 Yonge was a Plymouth naval surgeon, remembered mostly for his flap amputation technique. In his monograph Yonge gives a detailed account of a brain operation on a child aged 4 years with extensive compound fractures of the skull from which brain tissue issued forth. The surgery was a success and the child lived. Yonge also included reports on more than 60 cases of brain wounds that he found in the literature, beginning with Galen, which had been cured.
Eighteenth Century: Adventurous Surgeons
The eighteenth century produced some quite clever and adventurous surgeons. Percival Pott (1714-1788) was the greatest English surgeon of the eighteenth century. His list of contributions, several of which apply to neurosurgery, is enormous. His work Remarks on That Kind of Palsy of the Lower Limbs Found to Accompany a Curvature of the Spine describes the condition now known as Pott’s disease.66 His clinical descriptions are excellent, with the gibbous and tuberculous condition of the spine well outlined. Interestingly, he failed to associate the spinal deformity with the paralysis. He also described an osteomyelitic condition of the skull with a collection of pus under the pericranium, now called Pott’s puffy tumor. Pott felt strongly that these lesions should be trephined to remove the pus and decompress the brain.
In the ongoing argument over whether to trephine, Pott was a strong proponent of intervention (Figs. 1.29, 1.30). In his classic work on head injury,67 Pott appreciated that symptoms of head injury were the result of injury of the brain and not of the skull. He made an attempt to differentiate between “compression” and “concussion” injury of the brain.
The reasons for trepanning in these cases are, first, the immediate relief of present symptoms arising from pressure of extravasated fluid; or second, the discharge of matter formed between the skull and dura mater, in consequence of inflammation; or third, the prevention of such mischief, as experience has shown may most probably be expected from such kind of violence offered to the last mentioned membrane. …
In the … mere fracture without depression of bone, or the appearance of such symptoms as indicate commotion, extravasation, or inflammation, it is used as a preventative, and therefore is a matter of choice, more than immediate necessity.67
John Hunter (1728-1793) was one of the most remarkable and talented figures in English surgery and anatomy. His knowledge and skills in anatomy, pathology, and surgery and his dedication to his work allowed him to make a number of important contributions. Hunter received minimal formal education, though Percival Pott was an early teacher and mentor. In his book A Treatise on the Blood, Inflammation, and Gun-Shot Wounds,68 Hunter drew on his years of military experience (he served as a surgeon with the British forces during the Spanish campaign of 1761-1763). Unfortunately, the section on skull fractures took up only one paragraph and offered nothing original. However, his discussion of vascular disorders was quite advanced, with an appreciation of the concept of collateral circulation. His views on this subject grew out of his surgical experimentation on a buck whose carotid artery he tied off; he noted the response to be development of collateral circulation.69
Benjamin Bell (1749-1806) was among the most prominent and successful surgeons in Edinburgh. He was one of the first to emphasize the importance of reducing pain during surgery. His text, A System of Surgery,70 is written with extraordinary clarity and precision, qualities that made it one of the most popular surgical texts in the eighteenth and nineteenth centuries. In the section on head injury there is an interesting and important discussion of the differences between concussion, compression, and inflammation of the brain—each requiring different modes of treatment.70 Bell stressed the importance of relieving compression of the brain, whether it be caused by a depressed skull fracture or pressure caused by pus or blood—a remarkably aggressive approach for this period (Fig. 1.31). Bell was among the first to note that hydrocephalus is often associated with spina bifida. His treatment of a myelomeningocele involved placing a ligature around the base of the myelomeningocele sac and tying it down. The concept of an epidural hematoma and its symptoms were detailed by Bell; he argued for a rapid and prompt evacuation. His discussion of the symptoms of brain compression caused by external trauma is classic:
A great variety of symptoms … indicating a compressed state of the brain [among which] … the most frequent, as well as the most remarkable, are the following: Giddiness; dimness of sight; stupefaction; loss of voluntary motion; vomiting; an apoplectic stertor in the breathing; convulsive tremors in different muscles; a dilated state of the pupils, even when the eyes are exposed to a clear light; paralysis of different parts, especially of the side of the body opposite to the injured part of the head; involuntary evacuation of the urine and faeces; an oppressed, and in many case an irregular pulse … (volume 3, chapter 10, section 3).70
Lorenz Heister (1683-1758) produced another of the most popular surgical textbooks of the eighteenth century. A German surgeon and anatomist (a common combination at the time), he published his Chirurgie in 1718. It was subsequently translated into a number of languages and circulated widely.71 The book’s popularity was due to the wide range of surgical knowledge it communicated and its many valuable surgical illustrations. In the treatment of head injury Heister remained conservative with regard to trephination (Fig. 1.32). In wounds involving only concussion and contusion, he felt trephination to be too dangerous. In this preantiseptic era considering the additional risk of infection and injury to the brain, this was not too far off the mark:
XXVII. But when the Cranium is so depressed, whether in Adults or Infants, as to suffer a Fracture, or Division of its Parts, it must instantly be relieved: the Part depressed, which adheres, after cleaning the Wound, must be restored to its Place, what is separated must be removed, and the extravasated Blood be drawn off through the Aperture … (p. 100).71
Francois-Sauveur Morand (1697-1773) describes one of the earliest operations for abscess of the brain. Morand had a patient, a monk, who developed an otitis media and subsequently mastoiditis with temporal abscess.72 He trephined over the carious bone and discovered pus. He placed a catgut wick within the wound, but it continued to drain. He reopened the wound and this time opened the dura (a very adventurous maneuver for this period) with a cross-shaped incision and found a brain abscess. He explored the abscess with his finger, removing as much of the contents as he could, and then instilled balsam and turpentine into the cavity. He placed a silver tube for drainage, and as the wound healed he slowly withdrew the tube. The abscess healed, and the patient survived.
Domenico Cotugno (1736-1822) was a Neapolitan physician and was the first to provide descriptions of cerebrospinal fluid (CSF) and sciatica73 (Fig. 1.33). He performed a number of experiments on the bodies of some 20 adults. Using the technique of lumbar puncture, he was able to demonstrate the characteristics of CSF. In De Ischiade Nervosa Commentarius he demonstrated the “nervous” origin of sciatica, differentiating it from arthritis, with which it was generally equated at that time. Cotugno discovered the pathways of CSF, showing that it circulates in the pia-arachnoid interstices and flows through the brain and spinal cord via the aqueduct and convexities. He also described the hydrocephalus ex vacuo seen in cerebral atrophy.
In 1709, a small, and now very rare, monograph by Daniel Turner (1667-1741) appeared.74 The book was entitled A Remarkable Case in Surgery: Wherein an Account is given of an uncommon Fracture and Depression of the Skull, in a Child about Six Years old; accompanied with a large Abscess or Aposteme upon the Brain … (Fig. 1.34). This rather poignant piece of writing is perhaps our best view of the treatment of brain injuries in the early eighteenth century.
Louis Sebastian (also listed as Nicolas) Saucerotte (1741-1814) was first surgeon to the King of Poland and later a surgeon in the French Army. As has often been the case in the history of neurosurgery, war provided Saucerotte with training and multiple opportunities to deal with head injury. He reintroduced the concept of the contre-coup injury. In a review of head injury, he described in detail a series of intracranial injuries and their symptoms, including compression of the brain due to blood clot.75 Saucerotte described a classic case of incoordination, including opisthotonos and rolling of the eyes, as a result of a cerebellar lesion. He divided the brain into “areas” of injury, pointing out that areas of severe injury are at the base of the brain, while injuries of the forebrain are the best tolerated.
Nineteenth and Twentieth Centuries: Anesthesia, Antisepsis, and Cerebral Localization
During the nineteenth century three major innovations made possible great advances in surgery. Anesthesia allowed patients freedom from pain during surgery, antisepsis and aseptic technique enabled the surgeon to operate with a greatly reduced risk of postoperative complications caused by infection, and the concept of cerebral localization helped the surgeon make the diagnosis and plan the operative approach.
In the first half of the century, improvements in surgical technique and neuropathology helped prepare the way for these innovations. John Abernethy (1764-1831) succeeded John Hunter at St. Bartholomew’s Hospital and followed his tradition of experimentation and observation. Abernethy’s surgical technique did not differ from that of his predecessors; what is remarkable in his Surgical Observations76 is the thoughtful, very thorough discussion of all the mechanisms of injury to the brain and spinal cord. He performed one of the earliest known procedures for removal of a painful neuroma. The neuroma was resected and the nerve reanastomosed; the pain resolved and sensation returned, proving the efficacy of the anastomosis.
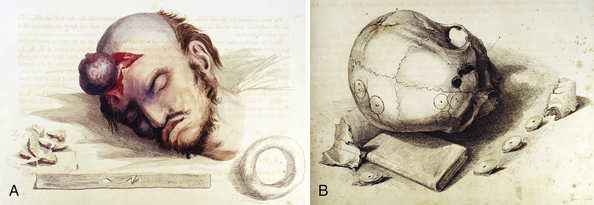
Sir Charles Bell (1774-1842), a Scottish surgeon and anatomist, was a prolific writer. He was educated at the University of Edinburgh and spent most of his professional career in London. He is remembered for many contributions to the neurosciences, including the differentiation of the motor and sensory components of the spinal root. He wrote a number of works on surgery, many of which were beautifully illustrated with his own drawings. These hand-colored illustrations were unrivaled at the time in detail, accuracy, and beauty (Fig. 1.35). In describing a trephination Bell details the technique as he practiced in 1821:
The surgeon will expect the instruments to be handed to him in this succession—the scalpel; the rasparatory; the trephine; the brush, the quill, and probe, from time to time; the elevator, the forceps, the lenticular (p. 6).77
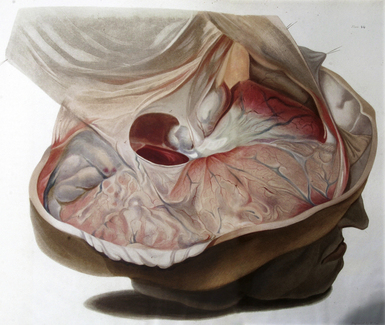
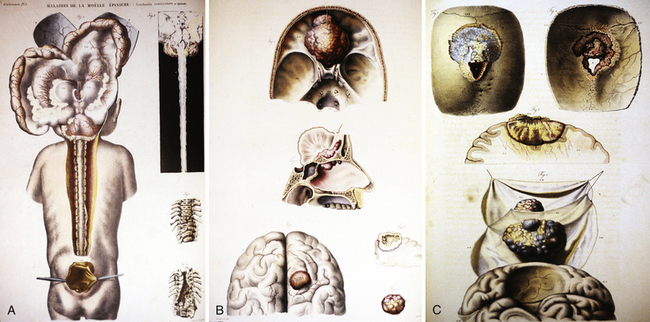
Also in the first half of the nineteenth century, a number of industrious individuals provided the basis for study of neuropathological lesions. Several excellent atlases appeared, beautifully colored and pathologically correct. Among the best known are those of Robert Hooper, Jean Cruveilhier, Robert Carswell, and Richard Bright (Fig. 1.36). Cruveilhier’s atlas is the most dramatic in appearance with illustrations of the brain and spine that were unparalleled for the period.78
Jean Cruveilhier (1791-1874) was the first occupant of a new chair of pathology at the University of Paris. He had at his disposal an enormous collection of autopsy material provided by the dead house at the Salpêtrière and the Musée Dupuytren. Using material from these sources he made a number of original descriptions of pathologies of the nervous system, including spina bifida (Fig. 1.37), spinal cord hemorrhage, cerebellopontine angle tumor, disseminated sclerosis, muscular atrophy, and perhaps the best early description of meningioma. This work was published in a series of fascicles issued over 13 years.79 The detailed descriptions by Cruveilhier and others provided the basis for the later cerebral localization studies. An understanding of tumors and their clinicopathological effects on the brain was critical for the later development of neurosurgery and the neurological examination. Harvey Cushing was the first to call attention to Cruveilhier’s accuracy in pathology and clinical correlation. He used portions of Cruveilhier’s works in his treatise on acoustic neuromas and his classic meningioma monograph.79–81
Antisepsis
Utilizing the recent bacterial concepts developed by Louis Pasteur, Joseph Lister introduced antisepsis in the operating room (Fig. 1.38). For the first time a surgeon, using aseptic technique and a clean operating theater, could operate on the brain with a reasonably small likelihood of infection. The steam sterilizer, the carbolic sprayer, the scrub brush, and Halsted’s rubber gloves truly heralded a revolution in surgery.
Cerebral Localization
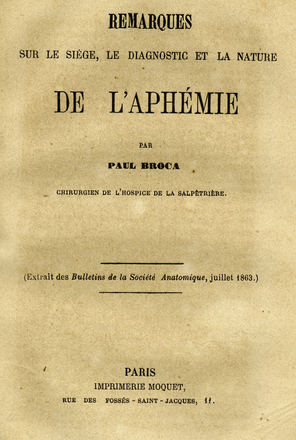
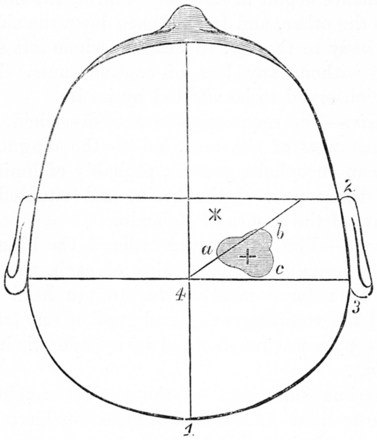
To make a diagnosis of a brain lesion or brain injury was not meaningful until the concept of localization was formulated (Fig. 1.39). During the 1860s several investigators, including G.T. Fritsch and E. Hitzig82 as well as Paul Broca, introduced the concept of cerebral localization, that each part of the brain was responsible for a particular function (Fig. 1.40).
Paul Broca (1824-1880) conceived the idea of speech localization in 1861.83 His studies were based on the work by Ernest Auburtin (1825-1893?), who had as a patient a gentleman who attempted suicide by shooting himself through the frontal region. He survived, but was left with a defect in the left frontal bone. Through this defect Auburtin was able to apply a spatula to the anterior frontal lobe and with pressure abolish speech, which returned when the spatula was removed. Auburtin immediately recognized the clinical implications. Broca further localized speech in an epileptic patient who was aphasic and could only emit the utterance “tan,” for which the patient became named. At autopsy, Broca found softening of the third left frontal convolution, and from this he postulated the cerebral localization of speech.83,84 Later, Karl Wernicke (1848-1904) identified a different area of the brain where speech was associated with conduction defects.85
These studies led to an explosion of research on the localization of brain function, such as the ablation studies by David Ferrier (1843-1928).86 John Hughlings Jackson (1835-1911), the founder of modern neurology, demonstrated important areas of function by means of electrical studies and developed the concept of epilepsy.87 Robert Bartholow (1831-1904), working in Ohio, published a series of three cases of brain tumors in which he correlated the clinical observations with the anatomical findings.88
Bartholow later performed an amazing clinical study correlating these types of pathological findings. In 1874 he took under his care a lady named Mary Rafferty who had developed a large cranial defect from infection, which had in turn exposed portions of each cerebral hemisphere. Through these defects he electrically stimulated the brain; unfortunately she subsequently died of meningitis. Bartholow records that “two needles insulated were introduced into left side until their points were well engaged in the dura mater. When the circuit was closed, distinct muscular contractions occurred in the right arm and leg.”89 Bartholow stimulated a number of different areas, carefully recording his observations. These clinical observations supported his postulated functional localizations in the brain. The ethics of his studies would be called into question today!
Advances in Surgical Techniques
Sir Rickman Godlee (1859-1925) (Fig. 1.41) removed one of the most celebrated brain tumors, the first to be successfully diagnosed by cerebral localization, in 1884.90 The patient, a man by the name of Henderson, had suffered for 3 years from focal motor seizures. They started as focal seizures of the face and proceeded to involve the arm and then the leg. In the 3 months prior to surgery the patient also developed weakness and eventually had to give up his work. A neurologist, Alexander Hughes Bennett (1848-1901), basing his conclusions on the findings of a neurological examination, localized a brain tumor and recommended removal to the surgeon. Godlee made an incision over the rolandic area and removed the tumor through a small cortical incision. The patient survived the surgery with some mild weakness and did well, only to die a month later from infection. Bennett, the physician who had made the diagnosis and localization, along with J. Hughlings Jackson and David Ferrier, two prominent British neurologists, observed this landmark operation. All of these physicians were extremely interested in whether the cerebral localization studies would provide necessary results in the operating theater. The results were good; this operation remains a landmark in the progress of neurosurgery.
Sir William Gowers (1845-1915) was one of an extraordinary group of English neurologists. Using some of the recently developed techniques in physiology and pathology, he made great strides in refining the concept of cerebral localization. Gowers was noted for the clarity and organization of his writing; his neurological writings remain classics.91–93 These investigative studies allowed surgeons to operate on the brain and spine for other than desperate conditions.
Sir Victor Alexander Haden Horsley (1857-1916) was an English general surgeon who furthered the development of neurosurgery during its embryonic period. Horsley began his experimental studies on the brain in the early 1880s, during the height of the cerebral localization controversies. Horsley worked with Sharpey-Schäfer in using faradic stimulation to analyze and localize motor functions in the cerebral cortex, internal capsule, and spinal cord of primates.94–96 In a classic study with Gotch, done in 1891, using a string galvanometer, he showed that electrical currents originate in the brain.97 These experimental studies showed Horsley that cerebral localization was possible and that operations on the brain could be conducted safely using techniques adapted from general surgery. In 1887, working with William Gowers, Horsley performed a laminectomy on Gowers’ patient, Captain Golby, a 45-year-old army officer. Golby was slowly losing function in his legs from a spinal cord tumor. Gowers localized the tumor by examination and indicated to Horsley where to operate; the tumor, a benign “fibromyxoma” of the fourth thoracic root, was successfully removed.98
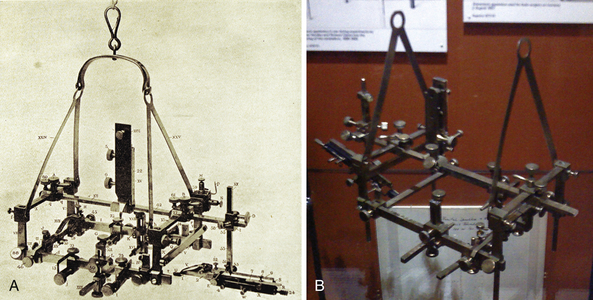
Horsley made a number of technical contributions to neurosurgery, including the use of beeswax to stop bone bleeding. He performed one of the earliest craniectomies for craniostenosis and relief of increased intracranial pressure. For patients with inoperable tumors he developed the decompressive craniectomy. For treatment of trigeminal neuralgia Horsley advocated sectioning the posterior root of the trigeminal nerve for facial pain relief. Using his technical gifts he helped Clarke design the first useful stereotactic unit for brain surgery (Fig. 1.42). Although never used in human surgery, the Horsley-Clarke stereotactic frame inspired all subsequent designs.99
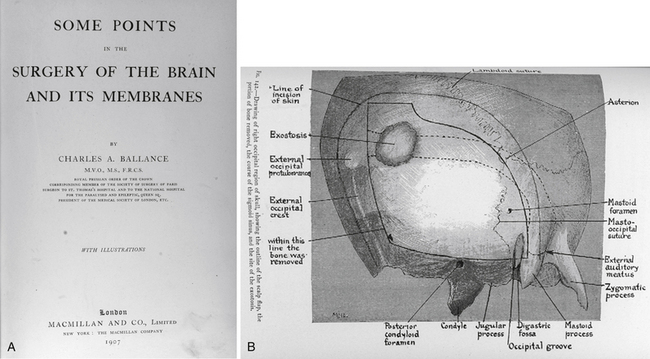
Sir Charles A. Ballance (1856-1936) was an English surgeon who received his medical education at University College, London. Ballance was an early pioneer in neurosurgery, performing the first mastoidectomy with ligation of the jugular vein. Ballance was one of the first to graft and repair the facial nerve. In his monograph on brain surgery Ballance sets forth many ideas that were quite modern.100 The book came from a series of Lettsomian Lectures given in 1906 in which are contained a series of three lectures on cerebral membranes, tumors, and abscesses. Ballance’s treatise recognized and described chronic subdural hematoma with great accuracy and detailed an operative success. Additional successful operations included one for subdural hygroma. Ballance routinely used the recently introduced lumbar puncture for cases of head injury and suppurative meningitis. An interesting and apparent cure of congenital hydrocephalus was recorded by Ballance using a technique that included ligation of both common carotid arteries. In his treatment of brain abscesses Ballance urged evacuation of the abscess with drainage recommended; in some cases he felt that complete enucleation of an abscess was advisable. Ballance devoted 243 pages of his monograph to a discussion of brain tumors and noted a wide operative experience with 400 such lesions. One of his most important cases, and one only recently recognized in the literature, involved a patient who was reported well in 1906 from whom he removed “a fibrosarcoma from the right cerebellar fossa” (i.e., an acoustic neuroma) in 1894; this would appear to be one of the earliest surgeries for an angle tumor100,101 (Fig. 1.43). In a profound comment on surgical operations for tumors Ballance had a hopeful outlook: “… I am convinced that the dawn of a happier day for these terrible cases has come.”
William Macewen (1848-1924), a Scottish surgeon, successfully accomplished a brain operation for tumor on July 29, 1879 (Fig. 1.44). Using meticulous technique and the recently developed neurological examination, he localized and removed a periosteal tumor from over the right eye of a 14-year-old. The patient went on to live for 8 more years, only to die of Bright’s disease; at autopsy no tumor was detected. By 1888, Macewen had operated on 21 neurosurgical cases with only three deaths and 18 successful recoveries, a remarkable change from earlier series. Macewen considered his success to be the result of excellent cerebral localization and good aseptic techniques. Macewen’s monograph on pyogenic infections of the brain and their surgical treatment, published in 1893,102 was the earliest to deal with the successful treatment of brain abscess. His morbidity and mortality statistics are as good as those in any series reported today.
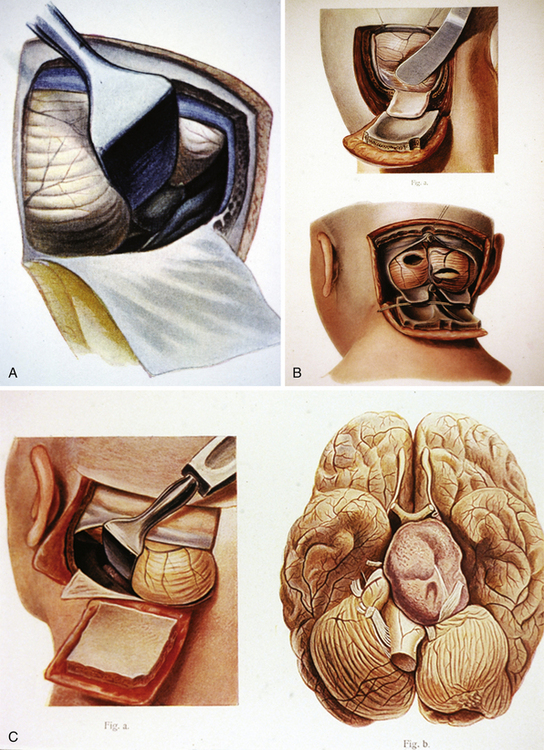
Joseph Pancoast (1805-1882) produced one of the most remarkable nineteenth century American monographs on surgery in the era just before the introduction of antisepsis and anesthesia103 (Fig. 1.45). Pancoast spent his academic career in Philadelphia, Pennsylvania, where he was physician and visiting surgeon to the Philadelphia Hospital. He later became professor of surgery and anatomy at Jefferson’s Medical College in 1838. Pancoast’s Treatise has 80 quarto plates comprising 486 lithographs with striking surgical details. These plates remain some of the most well-executed and graphical illustrations of different surgical techniques. The lithographs are exceedingly graphic, so much so that religious purists often removed numbers 69 and 70 because of their depiction of the female genitalia. The section on head injury and trauma clearly demonstrates the techniques of trephination and the elevation of depressed fractures. Pancoast was one of the first to devise an operation for transecting the fifth cranial nerve for trigeminal neuralgia.
Fedor Krause (1857-1937) was a general surgeon whose keen interest in neurosurgery made him the father of German neurosurgery. His three-volume atlas on neurosurgery, Surgery of the Brain and Spinal Cord, published in 1909-1912, was one of the first to detail the techniques of modern neurosurgery; it has since been through some 60 editions104 (Fig. 1.46). Krause, like William Macewen, was a major proponent of aseptic technique in neurosurgery. His atlas describes a number of interesting techniques. The “digital” extirpation of a meningioma is graphically illustrated. A number of original neurosurgical techniques are reviewed, including resection of scar tissue for treatment of epilepsy. Krause was a pioneer in the extradural approach to the gasserian ganglion for treatment of trigeminal neuralgia. He pioneered the transfrontal craniotomy in addition to transection of the eighth cranial nerve for severe tinnitus. To deal with tumors of the pineal region and posterior third ventricle he pioneered the supra-cerebellar-infratentorial approach. Krause was the first to suggest that tumors of the cerebellopontine angle (e.g., acoustic neuromas) could be operated on safely. Interestingly, Krause retired to Rome, where he gave up neurosurgery and continued his greatest love, playing the piano. When asked what he would most like to be remembered for, it was not as a neurosurgeon but rather as a classical pianist.
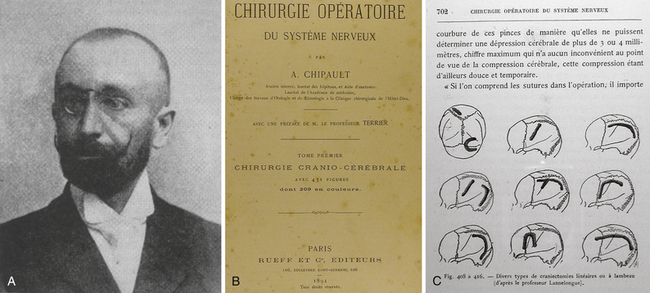
Antony (Antoine) Chipault (1866-1920) has remained an obscure historical figure in neurosurgery yet nevertheless he was one of the pioneers and was once considered the potential father of French neurosurgery. Chipault was named at birth Antonie Maxime Nicolas Chipault on July 16, 1866, in the town of Orleans, France. His father was a surgeon and he began his medical studies in Paris at the age of 18. He initially qualified as a gynecologist but later became interested in neurology. He became initially interested in the anatomy of the spine and published a now rare seminal monograph Etudes de Chirurgie Médullaires.105 In 1891 he began working with Professor Duplay at the Hotel Dieu under whom he became interested in craniocerebral pathology. In 1894 he published his classic work on surgery of the spine and spinal cord. Chipault published a series of papers on the brain and spinal cord including writings on Pott’s disease, osteoplastic craniotomy, spinal trauma, posterior root section for pain, and surgical treatment of brain tumors and hemorrhage, among other subjects. He made a number of technical innovations in neurosurgery, including introducing the removal of the underlying dura in meningiomas, a new laminectomy technique, plus development of small clamps for closing a scalp incision. He treated hydrocephalus by tapping the ventricles through a burr hole, and proposed a scheme of craniectomies for treatment of craniosynostosis (Fig. 1.47). He pioneered the use of wires and steel splints in the stabilization of the spine in trauma and deformities. In 1894 his surgical masterpiece appeared Chirurgie Opératoire du Systéme Nerveux, an extremely popular work that was translated into English, Spanish, Italian, German, Romanian, and Serbo-Croatian.106 He also introduced one of the first journals devoted to surgery of the spine and brain—Les Travaux de Neurologie Chirurgicale. Despite this illustrious career he dropped out of sight in 1905 ceasing all writing and works in neurosurgery. The cause is thought to be the onset of paraplegia, the etiology of which remains unknown. Chipault moved with his family to the Jura mountains near Orchamps. He died in 1920 at the age of 54 in total obscurity, a state in which he remains.
All carpets and unnecessary furniture were removed from the patient’s room. The walls and ceiling were carefully cleaned the day before operation, and the woodwork, floors, and remaining furniture were scrubbed with carbolic solution. This solution was also sprayed in the room on the morning preceding but not during the operation. On the day before operation, the patient’s head was shaved, scrubbed with soap, water, and ether, and covered with a wet corrosive sublimate dressing until the operation, then ether and mercuric chloride washings were repeated. The surgical instruments were boiled in water for 2 hours, and new deep-sea sponges (elephant ears) were treated with carbolic and sublimate solutions before usage. The surgeon’s hands were cleaned and disinfected using soap and water, alcohol, and sublimate solution (pp. 1001-1002).107
One of the earliest American monographs on neurosurgery, Linear Craniotomy, was prepared by Keen.108 He described the difficult differentiation between microcephalus and craniosynostosis. He then performed, in 1890, one of the first operations for craniostenosis in America. He developed a technique for treatment of spastic torticollis by division of the spinal accessory nerve and the posterior roots of the first, second, and third spinal nerves.109 He was also responsible for introducing the Gigli saw, first described in Europe in 1897, into American surgery in 1898.110,111
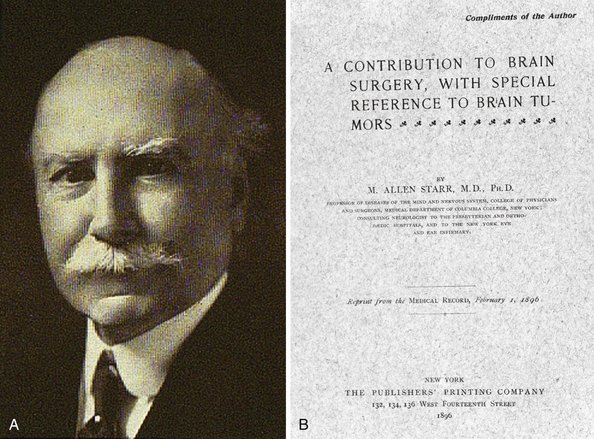
The first American monograph devoted to brain surgery was written not by a neurosurgeon but by the New York neurologist Allen Starr (1854-1932) (Fig. 1.48).112,113 Starr was Professor of Nervous Diseases at Columbia University and an American leader in neurology. He trained in Europe, working in the laboratories of Erb, Schultze, Meynert, and Nothnagle, experiences that gave him a strong foundation in neurological diagnosis. Working closely with Charles McBurney (1845-1913), a general surgeon, he came to the realization that brain surgery not only could be done safely but was necessary in the treatment of certain neurological problems (Fig. 1.49).114 He summarized his views in the preface:
Brain surgery is at present a subject both novel and interesting. It is within the past five years only that operations for the relief of epilepsy and of imbecility, for the removal of clots from the brain, for the opening of abscesses, for the excision of tumors, and the relief of intra-cranial pressure have been generally attempted … It is the object of this book to state clearly those facts regarding the essential features of brain disease which will enable the reader to determine in any case both the nature and situation of the pathological process in progress, to settle the question whether the disease can be removed by surgical interference, and to estimate the safety and probability of success by operation.112
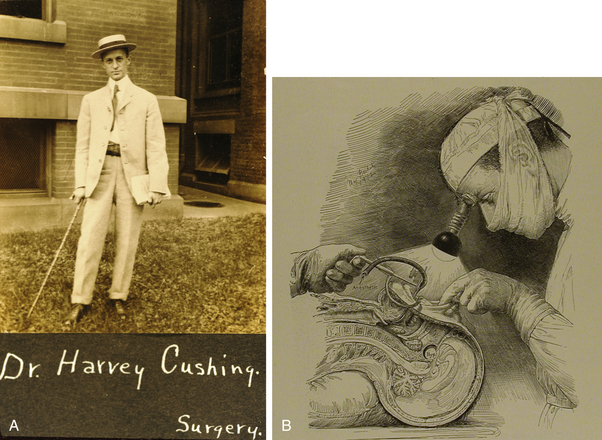
In 1923 Harvey Cushing, reviewing one of his own cases, commented about Allen Starr:
I am confident that if Allen Starr, in view of his position in neurology and his interest in surgical matters, had taken to the scalpel rather than the pen we would now be thirty years ahead in these matters, and I am sure his fingers must many times have itched when he stood alongside an operating table and saw the operator he was coaching hopelessly fumble with the brain.115
Harvey William Cushing (1869-1939) is considered the father of American neurosurgery (see Fig. 1.49). Educated at Johns Hopkins under one of the premier general surgeons, William Halsted (1852-1922), Cushing learned meticulous surgical technique from his mentor. As was standard then, Cushing spent time in Europe; he worked in the laboratories of Theodore Kocher in Bern, investigating the physiology of CSF. These studies led to his important monograph in 1926 on the third circulation.116 It was during this period of experimentation that the cerebral phenomenon of increased intracranial pressure in association with hypertension and bradycardia was defined; it is now called the “Cushing phenomenon.” While traveling through Europe he met several important surgical personalities involved in neurosurgery, including Macewen and Horsley. They provided the impetus for him to consider neurosurgery as a full-time endeavor (Fig. 1.50).
Cushing’s contributions to the literature of neurosurgery are too extensive to be listed in this brief chapter. Among his most significant work is a monograph on pituitary surgery published in 1912.117 This monograph inaugurated a prolific career in pituitary studies. Cushing syndrome was defined in his final monograph on the pituitary published in 1932.118 In a classic monograph, written with Percival Bailey in 1926, Cushing brought a rational approach to the classification of brain tumors.119 His monograph on meningiomas, written with Louise Eisenhardt in 1938, remains a classic.120
Cushing retired as Moseley Professor of Surgery at Harvard in 1932. By the time he completed his 2000th brain tumor operation,121 he had unquestionably made some preeminent contributions to neurosurgery, based on meticulous, innovative surgical techniques and the effort to understand brain function from both physiological and pathological perspectives. An ardent bibliophile, Cushing spent his final years in retirement as Stirling Professor of Neurology at Yale, where he put together his extraordinary monograph on the writings of Andreas Vesalius.122 Cushing’s life has been faithfully recorded by his close friend and colleague John F. Fulton.123
Walter Dandy (1886-1946), who trained under Cushing at Johns Hopkins, made a number of important contributions to neurosurgery. Based on Luckett’s serendipitous finding of air in the ventricles after a skull fracture,124 Dandy developed the technique of pneumoencephalography (Fig. 1.51).125–127 This technique provided the neurosurgeon with the opportunity to localize the tumor by analyzing the displacement of air in the ventricles.127 A Philadelphia neurosurgeon, Charles Frazier, commented in 1935 on the importance of pneumoencephalography and the difference it made in the practice of neurosurgery:
Only too often, after the most careful evaluation of the available neurologic evidence, no tumor would be revealed by exploration, the extreme intracranial tension would result in cerebral herniation to such an extent that sacrifice of the bone flap became necessary, and subsequently the skin sutures would give way before the persistent pressure, with cerebral fungus and meningitis as inevitable consequences. But injection of air has done away with all these horrors. The neurologist has been forced to recognize its important place in correct intracranial localization and frequently demands its use by the neurosurgeon.128
Dandy was an innovative neurosurgeon, far more aggressive in style and technique than Cushing. He was the first to show that acoustic neuromas could be totally removed.129,130 He devoted a great deal of effort to the treatment of hydrocephalus.131–133 He introduced the endoscopic technique of removing the choroid plexus to reduce the production of CSF.134 He was among the first to treat cerebral aneurysms by obliterating them using snare ligatures or metal clips.135 His monograph on the third ventricle and its anatomy remains a standard to this day, with anatomical illustrations that are among the best ever produced.136
In the field of spinal surgery, two important American figures appeared in the first quarter of the twentieth century: Charles Elsberg (1871-1948), Professor of Neurosurgery at the New York Neurological Institute, and Charles Frazier (1870-1936), Professor of Surgery at the University of Pennsylvania. Toward the end of the nineteenth century studies on the spine had been initiated by J. L. Corning, who had shown that lumbar puncture could be performed safely for diagnosis.137 H. Quincke went on to popularize this procedure; these early studies encouraged the development of spinal surgery.138,139
From a surgical experience developed during World War I Charles Frazier decided on a career in neurosurgery. Charles Frazier’s 1918 textbook on spinal surgery was the most comprehensive work on the subject available140; he summarized much of the existing literature and established that spinal surgery could be performed safely.
From New York City came Charles Elsberg, another pioneer in spinal surgery. Elsberg’s techniques were impeccable and led to excellent results. By 1912 he had reported on a series of 43 laminectomies and by 1916 he had published the first of what were to be three monographs on surgery of the spine.141,142 In the treatment of intramedullary spinal tumors Elsberg introduced the technique of a first-stage myelotomy. By waiting some time afterward, this allowed the intramedullary tumor to deliver itself, so then, at a second-stage procedure, the tumor was resected143 (Fig. 1.52). He worked with a fierce intensity and was always looking for new techniques. Working with Cornelius Dyke, a neuroradiologist at the New York Neurological Institute, he treated spinal glioblastomas with directed radiation in the operating room after the tumor had been exposed! These procedures were performed with the patients receiving only local anesthesia. During the half-hour therapy, while the radiation was being delivered, the surgeon and assistants stood off in the distance behind a glass shield.144
Leo Davidoff (1898-1975) was one of the prodigies of twentieth century neurosurgery (Fig. 1.53). Starting from humble origins in Lithuania, the son of a cobbler, he immigrated to the United States with his eight siblings. As a teen Davidoff worked in a factory to support his family; the factory’s manager admired his skill and dedication and sponsored his education, leading to his graduation from Harvard University in 1916. He completed his medical degree at Harvard in 1922 as an AOA (the national honor society for graduating medical students) member. Davidoff trained under Harvey Cushing and became one of his most popular students, not always an easy achievement with Cushing’s personality. When Cushing was once asked who he would allow to operate on him for a brain tumor his response was “Well I guess I would have Davey [Davidoff] do it.” Davidoff initially joined the staff of the New York Neurological Institute with Charles Elsberg in 1929. Here he began his seminal studies on the normal anatomy seen in pneumoencephalograms utilizing the hundreds of pneumoencephalograms performed at the Neurological Institute. In 1937 he issued a classic monograph with Cornelius Dyke (1900-1943), The Normal Encephalogram.145 This work, and a later publication with Bernard Epstein (1908-1978), The Abnormal Encephalogram (1950),146 became two of the most important neuroradiological texts, remaining influential for over 30 years. Davidoff’s meticulous and detailed studies led him to be called the father of neuroradiology. He left the Neurological Institute in 1937 when Bryon Stookey became chief, moving on to Brooklyn to the Jewish Hospital. Davidoff became chief of neurosurgery at Montefiore Hospital in 1945, working with two contemporary giants, Houston Merritt in neurology and Harry Zimmerman in neuropathology. Davidoff later became instrumental in the founding of the Albert Einstein College of Medicine, becoming the first chairman of neurosurgery in 1955. Davidoff was a charter member of the Harvey Cushing Society and served as president of the American Association of Neurological Surgeons from 1956 to 1957. Davidoff was described by his staff as a hard taskmaster, punctual, demanding, and critical. His operating room was meticulous and organized, with no unnecessary sound or speech allowed. Never one to raise his voice, a mere look, even behind a surgical mask, could be a chilling experience for the new house officer or scrub nurse. His legacy remains in over 200 scientific publications, his pioneering work in neuroradiology, and his total commitment to the highest standards in patient care and resident training.
Besides the pioneering techniques of Dandy, Cushing, and others, a number of diagnostic techniques were introduced whereby the neurosurgeon could localize lesions less haphazardly, thereby shifting the emphasis from the neurologist to the neurosurgeon. One such technique, myelography using opaque substances, was brought forward by Jean Athanase Sicard (1872-1929).147 With the use of a radiopaque iodized oil, the spinal cord and its elements could be outlined on x-ray. Antonio Caetano de Egas Moniz (1874-1955), Professor of Neurology at Lisbon, perfected arterial catheterization techniques and the cerebral angiogram in animal studies. This work required that a number of iodine compounds be studied, many of which caused convulsions and paralysis in laboratory animals. However, his ideas were sound and by 1927 angiography, used in combination with pneumoencephalography, offered the neurosurgeon the first detailed view of the intracranial contents.148,149 Ironically Moniz was later awarded the Nobel Prize in medicine in 1949 for his work in psychosurgery and not for his work in cerebral angiography.
In 1929, Alexander Fleming (1881-1955) published a report on the first observation of a substance that appeared to block the growth of a bacterium. This substance, identified as penicillin, heralded a new era of medicine and surgery.150 With World War II, antibiotics were perfected in the treatment of bacterial infection, reducing even further the risk of infection during craniotomy.
A defining moment in operative neurosurgery came with the Nobel Prize–winning work of an engineer by the name of Sir Godfrey Newbold Hounsfield and his design of the computer-assisted tomography (CAT).151 For the first time a neurosurgeon was able to visualize intracranial pathology by a noninvasive technique. The original images were poor quality grainy images on Polaroid film, whereas in a mere 40 some years the neurosurgeon now has elegant, high-resolution three-dimensional images with multimodality grids being easily obtained. This pioneer work led to an engineer (not a physician) receiving the first Nobel Prize in medicine in 1979, only 6 years after the publication of his seminal paper in 1973 (Fig. 1.54).
Conclusion
The first half of the twentieth century brought the formalization of the field of neurosurgery. In the 1920s, Elsberg, Cushing, and Frazier persuaded the American College of Surgeons to designate neurosurgery as a separate specialty. It has taken some 5000 years of constant study and the experience of generations to make neurosurgery what it is today (Fig. 1.55).
In just under 160 years the patient entering a neurosurgical operating room can have a painless operation with minimal risk of infection, and surgery will rarely be in the wrong location. Thanks to magnetic resonance imaging and computed tomography, the localization of neurological problems is hardly an issue. Intraoperative computerized localization of brain pathology is rapidly becoming the standard throughout the world. Some provocative forward thinkers feel that the neurosurgeon of the 2020s will be mere data engineers inputting into a computerized operation room with robots and in-place scanners. This scenario is a far cry from our Asclepiad fathers, who could only whisper secret incantations, lay on the hands, and provide herbal medicaments that only occasionally worked.
Cushing H. The Pituitary Body and Its Disorders: Clinical States Produced by Disorders of the Hypophysis Cerebri. Philadelphia: JB Lippincott; 1912.
Dandy W.E. Localization or elimination of cerebral tumors by ventriculography. Surg Gynecol Obstet. 1920;30:329-342.
Fulton J.F. Harvey Cushing: A Biography. Springfield, IL: Charles C Thomas; 1946.
Goodrich J.T. Sixteenth century Renaissance art and anatomy: Andreas Vesalius and his great book—a new view. Med Heritage. 1985;1:280-288.
Leonardo da Vinci. Corpus of the Anatomical Studies in the Collection of Her Majesty the Queen at Windsor Castle. K.D. Keele, C. Pedretti. New York: Harcourt Brace Jovanovich; 1979.
Moniz C.E. L’encéphalographie artérielle: son importance dans la localisation des tumeurs cérébrales. Rev Neurol. 1927;2:72-90.
Please go to expertconsult.com to view the complete list of references.
1. Elerick D.V., Tyson R.A. Human Paleopathology and Related Subjects: An International Bibliography. San Diego: San Diego Museum of Man; 1997.
2. Tyson R.A., Dyer Alcauska E.S. Catalogue of the Hrdlicka Paleopathology Collection. San Diego: San Diego Museum of Man; 1980.
3. Stone J.L., Urcid J. Pre-Columbian skull trepanation in North America. In: Arnott R., Finger S., Smith C.U.M., editors. Trepanation History, Discovery, Theory. Lisse, France: Swets & Zeitlinger; 2003:237-249.
4. Clower W.T., Finger S. Discovering trephination: the contribution of Paul Broca. Neurosurgery. 2001;49:1417-1425.
5. Goodrich J.T. Olmec serpentine dwarf. Childs Nerv Syst. 2006;22:1215.
6. Breasted J.H. The Edwin Smith Papyrus. Published in Facsimile and Hieroglyphic Transliteration with Translation and Commentary. Chicago: University of Chicago Press; 1930.
7. Ebers Papyrus. The Papyrus Ebers. The Greatest Egyptian Medical Document. [Ebbell B, Trans.]. Copenhagen: Levin & Munksgard; 1937.
8. Hippocrates. [Foesio A, Trans./Ed.]. Magni Hippocratis Medicorum Omnium Facile Principis, Opera Omnia Quae Extant. Geneva: Samuel Chouet; 1657-1662.
9. . Hippocrates. [Leonicenus N, Laurentianus L, Trans.]. Aphorismi, cum Galeni Commentariis; Praedictiones, cum Galeni Commentariis. Paris: Simon Sylvius; 1527.
10. Clarke E. Apoplexy in the Hippocratic writings. Bull Hist Med. 1963;37:301.
11. Marx K.F.H. Herophilus: ein Beitrag zur Geschichte der Medizin. Karlsruhe und Baden. Verlag der D.R.: Marrschen und Runsthandlung; 1838.
12. Ryff W. Des Aller Furtefflichsten … Erschaffen. Das is des Menchen … Warhafftige Beschreibund oder Anatomi. Strasbourg: Balthassar Beck; 1541.
13. Celsus. Medicinae Libri VIII. Venice: Aedes Aldi et Andreae Asulani Soceri; 1528.
14. Medicae Artis Principes post Hippocratem et Galenum. Geneva: Henri Estienne; 1567.
15. Galen. Omnia Quae Extant Opera in Latinum Sermonem Conversa, 5th ed. Venice: Juntas; 1576-1577.
16. Galen. Experimental section and hemisection of the spinal cord (taken from De locis affectibus). Ann Med Hist. 1917;1:367.
17. Paulus Aeginetes. Opus de Re Medica Nunc Primum Integrum. Köln: Joannes Soter. 1534.
18. . Paulus Aeginetes. [Adams F, Trans.]. The Seven Books of Paulus Aegineta. London: Sydenham Society; 1844-1847.
19. Lascaraltos J.G., Panourias I.G., Saka D.E. Hydrocephalus according to Byzantine writers. Neurosurgery. 2004;53:214-221.
20. Rhazes. Opera Parva. Lyons: Gilbertus de Villiers, Johannis de Ferris; 1511.
21. Avicenna. Liber Canonis, de Medicinis Cordialibus, et Cantica. Basel: Joannes Heruagios; 1556.
22. Aciduman A., Belen D. Hydrocephalus and its management in Avicenna’s Canon of Medicine. J Neurosurg. 2007;105(suppl 6):513-516.
23. Haly Abbas (Abdul-Hasan Ali Ibn Abbas Al Majusi). Liber Totius Medicine necessaria continens quem sapientissimus Haly filius Abbas discipulus Abimeher Muysi filii Sejar editit: regique inscripsit unde et regalis depositionis nomen assumpsit. Et a Stephano philosophie discipulo ex Arabica lingua in Latinam… reductus. Necnon a domino Michaele de Capella… Lugduni. Lyons: Jacobi Myt; 1523.
24. Albucasis. Liber Theoricae Necnon Practicae Alsaharavii. Augsburg: Sigismundus Grimm & Marcus Vuirsung; 1519.
25. Albucasis. [Spink MS, Lewis GL, Trans./Eds.]. Albucasis on Surgery and Instruments. Berkeley: University of California Press; 1973.
26. Al-Rodhan N.R.F., Fox J.L. Al-Zahrawi and Arabian neurosurgery, 936-1013 ad. Surg Neurol. 1986;25:92-95.
27. Sabuncuoglu S. Cerrahiyyetü’l-Haniyye [Imperial Surgery] [translated from Arabic]. Ottoman Empire circa fifteenth century. From a later copied manuscript in the author’s collection, circa 1725. See also Cerrahiyyetü’l-Haniyye. Paris: France: Bibliothéque Nationale; 1465, Suppl Turc No. 693.
28. Elmaci I. Color illustrations and neurosurgical treatments of Serefeddin Sabuncuoglu in the 15th century. Neurosurgery. 2000;47:947-954.
29. Aygen G., Karasu A., Ofluoglu A.E., et al. The first Anatolian contribution to treatment of sciatica by Serefeddin Sabuncuoglu in the 15th century. Surg Neurol. 2009;71:130-133.
30. Aciduman A., Belen D. The earliest document regarding the history of cranioplasty from the Ottoman Era. Surg Neurol. 2007;68:349-353.
31. Constantinus Africanus. Constantini Africani Post Hippocratem et Galenum. Basel: Henricus Petrus; 1536.
32. Roger of Salerno. Practica chirurgiae. In: Guy de Chauliac Cyrurgia … et Cyrurgia Bruni, Teodorici, Rolandi, Lanfranci, Rogerii, Bertapalie. Venice: Bernardinus Venetus de Vitalibus; 1519.
33. Corner G. [Trans.]. In: The Bamberg Surgery. Bull Inst Hist Med. 1937;5:1-32.
34. . Theodoric Bishop of Cervia. [Campbell E, Colton J, Trans.]. The Surgery of Theodoric, ca. AD 1267. New York: Appleton-Century-Crofts; 1955-1966.
35. William of Saliceto. Chirurgia. Venice: F. di Pietro; 1474.
36. Leonard of Bertapalia. Chirurgia. In: Guy de Chauliac Cyrurgia … et Cyrurgia Bruni, Teodorici, Rolandi, Lanfranci, Rogerii, Bertapalie. Venice: Bernardinus Venetus de Vitalibus; 1519.
37. . Leonard of Bertapalia. [Ladenheim JC, Trans.]. On Nerve Injuries and Skull Fractures. Mount Kisco, NY: Futura Publishing; 1989.
38. Lanfranchi of Milan. Chirurgia. In: Guy de Chauliac Cyrurgia … et Cyrurgia Bruni, Teodorici, Rolandi, Lanfranci, Rogerii, Bertapalie. Venice: Bernardinus Venetus de Vitalibus; 1519.
39. Guy de Chauliac. Chirurgia magna. In: Guy de Chauliac Cyrurgia … et Cyrurgia Bruni, Teodorici, Rolandi, Lanfranci, Rogerii, Bertapalie. Venice: Bernardinus Venetus de Vitalibus; 1519.
40. Guy de Chauliac. [Brennan WA, Trans.]. Guy de Chauliac (AD 1363) on Wounds and Fractures. Chicago: published by translator; 1923.
41. Leonardo da Vinci. Quaderni d’Anatomia. Christiania: Jacob Dybwad; 1911-1916.
42. Hopstock H. Leonardo as an anatomist. In: Singer C., editor. Studies in the History of Medicine. Oxford: Clarendon Press, 1921.
43. Leonardo da Vinci. Keele K.D., Pedretti C., editors. Corpus of the Anatomical Studies in the Collection of Her Majesty the Queen at Windsor Castle. New York: Harcourt Brace Jovanovich, 1979.
44. Goodrich J.T. Sixteenth century Renaissance art and anatomy: Andreas Vesalius and his great book – a new view. Med Heritage. 1985;1:280-288.
45. Paré A. Opera. [Guillemeau J, Trans.]. Paris: Jacobus Du Puys; 1582.
46. Paré A. [Johnson T, Trans.]. The Workes of That Famous Chirurgion Ambroise Parey. London: Richard Coates; 1649.
47. Berengario da Carpi J. Tractatus de Fractura Calvae Sive Cranei. Bologna: Hieronymus de Benedictus; 1518.
48. Dryander J. Anatomiae. Marburg: Eucharius Ceruicornus; 1537.
49. Hanigan W.C., Ragen W., Foster R. Dryander of Marburg and the first textbook of neuroanatomy. Neurosurgery. 1990;26:489-498.
50. Coiter V. Externarum et Internarum Principalium Humani Corporis Partium Tabulae Atque Anatomicae Exercitationes Observationesque Variae. Nürnberg: Theodoricus Gerlatzenus; 1573.
51. Croce GA della. Chirurgiae Libri Septem. Venice: Jordanus Zilettus; 1573.
52. Vesalius A. De Humani Corporis Fabrica Libri Septem. Basel: Joannes Oporinus; 1543.
53. Vesalius A. [Singer C, Trans./Ed.]. Vesalius on the Human Brain. London: Oxford University Press; 1952.
54. Vesalius A. De Humani Corporis Fabrica. Basel: Oporinus; 1555.
55. Estienne C. De Dissectione Partium Corporis Humani Libri Tres. Paris: Simon Colinaeus; 1546.
56. Willis T. Cerebri Anatome: Cui Accessit Nervorum Descriptio et Usus. London: J. Flesher; 1664.
57. Haller A. Bibliotheca Anatomica. Qua Scripta ad Anatomen et Physiologiam…. Tiguri, apud Orell, Gessner, Fuessli, et Socc. 1774:475.
58. Lo W.B., Ellis H. The circle of Willis: a historical account of the intracranial anastomosis. Neurosurgery. 2010;66:7-18.
59. Vesling J. Syntagma Anatomicum, 2nd ed. Padua: Paulus Frambottus; 1651.
60. Spiegal A van de, Casserius G. De Humani Corporis Fabrica Libri Decem, Tabulis XCIIX Aeri Incisis Elegantissimis. Venice: Evangelista Deuchinus; 1627.
61. Fallopius G. Observationes Anatomicae. Venice: Marcus Antonius Ulmus; 1561.
62. Ridley H. The Anatomy of the Brain, Containing Its Mechanisms and Physiology: Together With Some New Discoveries and Corrections of Ancient and Modern Authors Upon That Subject. London: Samuel Smith; 1695.
63. Fabry W. Observationum et Curationum Chirurgicarum Centuriae. Lyons: J.A. Huguetan; 1641.
64. Scultetus J. Armamentarium Chirurgicum XLIII. Ulm: Balthasar Kühnen; 1655.
65. Yonge J. Wounds of the Brain Proved Curable, Not Only by the Opinion and Experience of Many (the Best) Authors, but the Remarkable History of a Child Four Years Old Cured of Two Very Large Depressions, With the Loss of a Great Part of the Skull, a Portion of the Brain Also Issuing Thorough a Penetrating Wound of the Dura and Pia Mater. London: Henry Faithorn and John Kersey; 1682.
66. Pott P. Remarks on That Kind of Palsy of the Lower Limbs, Which Is Frequently Found to Accompany a Curvature of the Spine. London: J. Johnson; 1779.
67. Pott P. Observations on the Nature and Consequences of Wounds and Contusions of the Head, Fractures of the Skull, Concussions of the Brain. London: C. Hitch and L. Hawes; 1760.
68. Hunter J. A Treatise on the Blood, Inflammation, and Gun-Shot Wounds. London: J. Richardson; 1794.
69. Stone J.L., Goodrich J.T., Cybulski G.R. John Hunter’s contributions to neuroscience. In Boller F., Finger S., Tyler K., editors: History of Neurology. A Volume in the Handbook of Clinical Neurology Series, 3rd series, St. Louis: Elsevier, 2008.
70. Bell B. A System of Surgery. Edinburgh: C. Elliot; 1783-1788.
71. Heister L. A General System of Surgery in Three Parts. London: W. Innys; 1743.
72. Morand F- S. Opuscules de Chirurgie. Paris: Guillaume Desprez; 1768-1772.
73. Cotugno D. De Ischiade Nervosa Commentarius. Napoli: Fratres Simonii; 1764.
74. Turner D. A Remarkable Case in Surgery: Wherein an Account is Given of an Uncommon Fracture and Depression of the Skull, in a Child About Six Years Old; Accompanied With a Large Abscess or Aposteme Upon the Brain. With Other Practical Observations and Useful Reflections Thereupon. Also an Exact Draught of the Case, Annex’d. And for the Entertainment of the Senior, but Instruction of the Junior Practitioners, Communicated. London: R. Parker; 1709.
75. Saucerotte N. Mélanges de Chirurgie. Paris: Gay; 1801.
76. Abernethy J. Surgical Observations. London: Longman, Rees, Orme, Brown, and Greene; 1809-1810.
77. Bell C. Illustrations of the Great Operations of Surgery. London: Longman, Rees, Orme, Brown, and Greene; 1821.
78. Bright R. Report of Medical Cases. London: Longman, Rees, Orme, Brown, and Greene; 1827.
79. Cruveilhier J. Anatomie Pathologique du Corps Humain. Paris: J.-B. Baillière; 1829-1842.
80. Flamm E.S. The neurology of Jean Cruveilhier. Med Hist. 1973;17:343-353.
81. Bakay L. Historical vignette: Cruveilhier on meningiomas (1829-1842). Surg Neurol. 1989;32:159-164.
82. Fritsch G.T., Hitzig E. Über die elektrische Erregbarkeit des Grosshirns. Arch Anat Physiol Wiss Med. 1870:300-332.
83. Broca P. Remarques sur le siège de la faculté du language articulé suivie d’une observation d’aphémie (perte de la parole). Bull Soc Anat Paris. 1861;36:330-357.
84. Broca P. Perte de la parole: ramollissement chronique et destruction partielle du lobe antérieur gauche du cerveau. Bull Soc Anthropol Paris. 1861;2:235-238.
85. Wernicke C. Der aphasische Symptomenkomplex. Breslau: M. Cohn & Weigert; 1874.
86. Ferrier D. The Functions of the Brain. London: Smith, Elder and Co; 1876.
87. Taylor J., editor. Selected Writings of John Hughlings Jackson. New York: Basic Books, 1958.
88. Bartholow R. Tumours of the brain: clinical history and comments. Am J Med Sci. 1868;110(ns):339-359.
89. Bartholow R. Experimental investigations into the functions of the human brain. Am J Med Sci. 1874;67:305-313.
90. Bennett A.H., Godlee R.J. Excision of a tumour from the brain. Lancet. 1884;2:1090-1091.
91. Gowers W.R. The Diagnosis of Diseases of the Spinal Cord. London: J. and A. Churchill; 1880.
92. Gowers W.R. Epilepsy and Other Chronic Convulsive Diseases. London: J. and A. Churchill; 1881.
93. Gowers W.R. Lectures on the Diagnosis of Diseases of the Brain. London: J. and A. Churchill; 1886-1888.
94. Horsley V.A.H., Sharpey-Schäfer E.A. A record of experiments upon the functions of the cerebral cortex. Philos Trans R Soc Lond Biol. 1889;179:1-45.
95. Vilensky J.A., Gilman S. Motor cortex extirpation (1886-1950): the influence of Sir Victor Horsley. Neurosurgery. 2002;51:1484-1488.
96. Vilensky J.A., Gilman S. Horsley was the first to use electrical stimulation of the human cortex intraoperatively. Surg Neurol. 2002;58:425-426.
97. Gotch F., Horsley V.A.H. On the mammalian nervous system, its functions, and their localisation determined by an electrical method. Philos Trans R Soc Lond Biol. 1891;182:267-526.
98. Gowers W.R., Horsley V.A.H. A case of tumour of the spinal cord: removal; recovery. Med Chir Trans. 1888;71:377-430.
99. Horsley V.A.H., Clarke R.H. The structure and functions of the cerebellum examined by a new method. Brain. 1908;31:45-124.
100. Ballance C.A. Some Points in the Surgery of the Brain and Its Membranes. London: Macmillan; 1907.
101. Stone J.L. Sir Charles Balance: pioneer British neurological surgeon. Neurosurgery. 1999;44:631-632.
102. Macewen W. Pyogenic Infective Diseases of the Brain and Spinal Cord. Glasgow: J. Maclehose & Sons; 1893.
103. Pancoast J.A. Treatise on Operative Surgery; Comprising a Description of the Various Processes of the Art, Including all the New Operations; Exhibiting the State of Surgical Science in its Present Advanced Condition. Philadelphia: Carey and Hart; 1844.
104. Krause F., Haubold H., Thorek M. [Trans.]. Surgery of the Brain and Spinal Cord Based on Personal Experiences. New York: Rebman Co.; 1909-1912.
105. Chipault A. Etudes de Chirurgie Médullaire. Paris: Felix Alcan; 1894.
106. Chipault A. Chirurgie Opératoire du Systéme Nerveux. Paris: Rueff et Cie; 1894-1895.
107. Stone J.L., Keen W.W. America’s pioneer neurological surgeon. Neurosurgery. 1985;17:997-1110.
108. Keen W.W. Linear Craniotomy. Philadelphia: Lea Bros. and Co.; 1891.
109. Keen W.W. A new operation for spasmodic wry neck, namely, division or exsection of the nerves supplying the posterior rotator muscles of the head. Ann Surg. 1891;13:44-47.
110. Keen W.W. On the use of the Gigli wire saw to obtain access to the brain. Phila Med J. 1898;1:32-33.
111. Bingham W.F.W.W. Keen and the dawn of American neurosurgery. J Neurosurg. 1986;64:705-717.
112. Starr M.A. Brain Surgery. New York: William Wood & Co.; 1893.
113. Starr M.A. Discussion on the present status of the surgery of the brain, 2: a contribution to brain surgery, with special reference to brain tumors. Trans Med Soc NY. 1896:119-134.
114. McBurney C., Starr M.A. A contribution to cerebral surgery: diagnosis, localization and operation for removal of three tumors of the brain, with some comments upon the surgical treatments of brain tumors. Am J Med Sci. 1893;105(ns):361-387.
115. Cushing H. Neurological surgeons, with the report of one case. Arch Neurol Psychiatr. 1923;10:381-390.
116. Cushing H. The Third Circulation: Studies in Intracranial Physiology and Surgery. London: Oxford University Press; 1926.
117. Cushing H. The Pituitary Body and Its Disorders: Clinical States Produced by Disorders of the Hypophysis Cerebri. Philadelphia: JB Lippincott; 1912.
118. Cushing H. Papers Relating to the Pituitary Body, Hypothalamus, and Parasympathetic Nervous System. Springfield, IL: Charles C Thomas; 1932.
119. Bailey P., Cushing H. A Classification of the Tumors of the Glioma Group on a Histogenetic Basis With a Correlated Study of Prognosis. Philadelphia: JB Lippincott; 1926.
120. Cushing H., Eisenhardt L. Meningiomas: Their Classification, Regional Behavior, Life History and Surgical End Results. Springfield, IL: Charles C Thomas; 1938.
121. Cushing H. Intracranial Tumors: Notes Upon a Series of Two Thousand Verified Cases With Surgical Mortality Percentages Pertaining Thereto. Springfield, IL: Charles C Thomas; 1932.
122. Cushing H. A Bio-Bibliography of Andreas Vesalius. New York: Schuman; 1943.
123. Fulton J.F. Harvey Cushing: A Biography. Springfield, IL: Charles C Thomas; 1946.
124. Luckett W.H. Air in the ventricles following a fracture of the skull. Surg Gynaecol Obstet. 1913;17:237-240.
125. Dandy W.E. Ventriculography following the injection of air into the cerebral ventricles. Ann Surg. 1918;68:5-11.
126. Dandy W.E. Röntgenography of the brain after the injection of air into the spinal canal. Ann Surg. 1919;70:397-403.
127. Dandy W.E. Localization or elimination of cerebral tumors by ventriculography. Surg Gynecol Obstet. 1920;30:329-342.
128. Frazier C.H. Fifty years of neurosurgery. Arch Neurol Psychiatr. 1935;34:907-922.
129. Dandy W.E. An operation for the total extirpation of tumors in the cerebellopontine angle: a preliminary report. Bull Johns Hopkins Hosp. 1922;33:344-345.
130. Dandy W.E. An operation for the total removal of cerebello-pontine (acoustic) tumors. Surg Gynecol Obstet. 1925;41:129-148.
131. Dandy W.E., Blackfan D.D. An experimental and clinical study of internal hydrocephalus. JAMA. 1913;61:2216-2217.
132. Dandy W.E., Blackfan D.D. Internal hydrocephalus: an experimental, clinical and pathologic study. Am J Dis Child. 1914;8:406-482.
133. Dandy W.E. Experimental hydrocephalus. Trans Am Surgical Assoc. 1919;37:397-428.
134. Dandy W.E. An operative procedure for hydrocephalus. Bull Johns Hopkins Hosp. 1922;33:189-190.
135. Dandy W.E. Intracranial aneurysm of the internal carotid artery cured by operation. Ann Surg. 1938;107:654-659.
136. Dandy W.E. Benign Tumors of the Third Ventricles. Springfield, IL: Charles C Thomas; 1933.
137. Corning J.L. Spinal anesthesia and local medication of the cord. NY Med J. 1885;42:483-485.
138. Quincke H.I. Die Lumbalpunction des Hydrocephalus. Berl Klin Wochenschr. 1891;28:929-933. 965-968
139. Quincke H.I. Die diagnostische und therapeutische Bedeutung der Lumbalpunction: klinischer Vortrag. Dtsch Med Wochenschr. 1905;31:1825-1828. 1869-1872
140. Frazier C. Surgery of the Spine and Spinal Cord. New York: Appleton; 1918.
141. Elsberg C.A. Surgery of intramedullary affections of the spinal cord: anatomic basis and technic with report of cases. JAMA. 1912;59:1532-1536.
142. Elsberg C.A. Diagnosis and Treatment of Surgical Diseases of the Spinal Cord and Its Membranes. Philadelphia: WB Saunders; 1916.
143. Elsberg C.A. Tumors of the Spinal Cord. New York: Hoeber; 1925:. 381
144. Pool L. The Neurological Institute of New York, 1909-1974, With Personal Anecdotes. Lakeville, CT: Pocket Knife Press; 1975:. 59
145. Davidoff L., Dyke C. The Normal Pneumoencephalogram. Philadelphia: Lea & Febiger; 1937.
146. Davidoff L., Epstein B. The Abnormal Pneumocephalogram. Philadelphia: Lea & Febiger; 1950.
147. Sicard J.A., Forestier J. Méthode radiographique d’exploration de la cavité épidurale par le lipiodol. Rev Neurol. 1921;37:1264-1266.
148. Moniz C.E. L’encéphalographie artérielle: son importance dans la localisation des tumeurs cérébrales. Rev Neurol. 1927;2:72-90.
149. Moniz C.E. Diagnostic des Tumeurs Cérébrales et Épreuve de l’Encéphalographie Artérielle. Paris: Masson & Cie; 1931.
150. Fleming A. On the antibacterial action of cultures of a penicillium, with special reference to their use in the isolation of B. influenzae. Br J Exp Pathol. 1929;10:226-236.
151. Hounsfield G.N. Computerized transverse axial scanning (tomography). Br J Radiol. 1973;46:1016-1022.